Abstract
Background
We attempted to validate the performance of a fast myocardial perfusion imaging (MPI) protocol in diagnostically challenging patients.
Methods
78 patients with ΒΜΙ > 24.9, LVH or three vessels disease underwent two sequential gated-MPI studies. The first at 15 (Early Imaging, EI) and the second at 45 (Late Imaging, LI) minutes post 99mTc-injection, at both stress and rest. Counts over heart (H), liver (Liv) and subdiaphragmatic space (Sub) and image quality, and myocardial perfusion and function parameters were compared between the two protocols. Coronary angiography was performed within 2 months from MPI, and ROC analysis was used to compare the diagnostic accuracy for the detection of ≥50% diameter luminal stenosis.
Results
Quality was optimal-good in 93% of EI and 98% of LI studies (P = .12), H/Liv and stress H/Sub ratios were similar, but rest H/Sub ratio was lower in EI (P = .009). SSS [10 (0 to 46) vs 9 (0 to 36), P = .006] and SDS [3 (0 to 35) vs 2 (0 to 34), P = .02] were higher in EI protocol. LVEF, motion and thickening scores did not differ between the two protocols. A highly significant (P < .001) linear relationship with clinically negligible mean differences in Bland-Altman analysis was observed for all perfusion and function-related data. Sensitivity (EI 81%, LI 80%) and specificity (65% for both) did not differ (P = .23) between the two protocols.
Conclusion
The fast protocol is technically feasible and diagnostically accurate compared to the established protocol in diagnostically challenging patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Coronary artery disease (CAD) is the leading cause of death worldwide1, and its diagnosis represents the most frequent cause of referral for cardiological testing in developed countries. Among the wide variety of non-invasive modalities available for CAD diagnosis, single-photon emission computed tomography (SPECT) has the lion’s share for this purpose.2 Given the growing use of myocardial perfusion imaging (MPI) for CAD diagnosis and risk stratification in the setting of the limited availability of gamma cameras, there is increasing interest to improve the efficiency of such examinations. A typical MPI study protocol using 99mTc-labeled tracers—which are currently the preferred radiotracers for this purpose3—includes sufficient time for stress, followed by a time lag until the initiation of image acquisition and finally the period of image acquisition. Although some aspects of the imaging protocol are fixed, recent developments have allowed for significant reductions in image acquisition and processing time as well as the time between isotope injection and initiation of imaging. Regarding the latter, the American Society of Nuclear Cardiology recommended,4,5 minimum delays from 99mTc-tetrofosmin injection to image acquisition are 45 minutes for pharmacologic stress, 10 to 15 minutes for exercise stress and 30 minutes for rest. The European Association of Nuclear Medicine6 recommends that imaging should begin at least 30 minutes after injection for exercise stress, with longer delays required for resting images and stress with vasodilators alone. Early imaging has been attempted in various studies dating since 1993.7 However, only one study8 has demonstrated so far the feasibility and diagnostic equivalence of a standardized, complete fast (imaging at 15 minutes post tracer injection at both stress and rest) imaging protocol using 99mTc in comparison to the established protocol, which involves the typical 30 minutes delay and is clinically used in most nuclear medicine laboratories. We aimed at validating these results in a group of diagnostically challenging patients.
Materials and Methods
Patient’s Selection
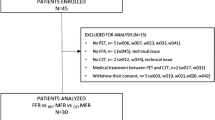
Inclusion criteria were referral for MPI at the nuclear medicine laboratory of Onassis Cardiac Surgery Center, with either exercise or pharmacologic stress for either known or suspected CAD, coronary angiography within 60 days from the imaging study and presence of one or more of the following characteristics: body mass index (BMI) > 24.9 kg/m2, left ventricular hypertrophy (LVH) on a recent echocardiogram (defined as septal and/or posterior wall thickness >9 mm for women or >10 mm for men, according to relevant guidelines9), or angiographically documented triple vessel CAD before imaging. These characteristics were considered by design of the study as difficulty factors for the performance of MPI studies of adequate image quality and diagnostic accuracy, based on existing relative literature.10 – 12 A consecutive series of eligible patients formed the population of this prospective study, as shown in Figure 1. Withdrawal of antianginal medications prior to testing was left at the referring physician’s discretion. The study was approved by the Ethics Committee of our institution and all included patients gave informed consent to participate.
Imaging Protocol
The imaging protocol of the study was as follows (Figure 2): At peak stress, 8 to 10 mCi 99mTc-tetrofosmin (Myoview, GE Healthcare) were administered intravenously through an antecubital vein. Peak stress was defined as the point where 85% of maximum predicted heart rate was achieved for treadmill stress or 3 minutes after initiation of adenosine infusion had elapsed for pharmacologic stress. Immediately after completion of stress, patients had a glass of cold water to accelerate hepatobiliary clearance of the radiotracer and two sequential-gated SPECT image acquisitions took place. The first (Early Stress) at 15 minutes and the second (Late Stress) at 45 minutes post-radiotracer injection. Upon completion of the Late Stress imaging, 20 to 25 mCi 99mTc-tetrofosmin were administered i.v. under resting conditions and Early Rest and Late Rest scans took place, as per stress imaging. All acquisitions were performed using a dual head gamma camera, equipped with a general purpose, low-energy, and high-resolution parallel hole collimator (Millennium VG, GE Medical Systems, Milwaukee, USA). 60 projections were obtained for 20 (rest) to 25 (stress) seconds each, with an 180° rotation extending from the 45° RAO to the 45° LAO projection. Energy discrimination was provided by a 15% window centered at 140 keV x-ray peak, while images were reconstructed using filtered back projection (Butterworth 0.4, order 5 filter) without attenuation or scatter correction. Before the acquisition of tomographic images, static anterior view images were acquired for 5 minutes.
Analysis of Scintigraphic Data
Evaluation of image quality
The overall image quality was evaluated visually, using a semiquantitative 4-point scale by two experienced nuclear medicine physicians (AT, MK). Scoring was performed in the same setting for Early and Late images with readers being blinded to the type of protocol the images belonged to, and disagreements were resolved by consensus. Scores were assigned to each study according to the following criteria: optimal quality = 3, good quality = 2, fair quality = 1, and poor quality = 0.
Analysis of static images
On the anterior raw images, 5 × 5 mm irregular regions of interest were drawn manually over the heart, lungs, liver, and subdiaphragmatic (just below the left ventricle, excluding the liver) areas. The counts measured in each region were normalized via software to the number of pixels, and the mean 99mTc-tetrofosmin activity per pixel was calculated for heart (H), average of the two lungs (L), liver (Liv), and subdiaphragmatic space (Sub) for each protocol in stress and rest images. Subsequently, stress and rest count ratios (H/L, H/Liv and H/Sub) were calculated for each one of the two protocols.
Semiquantitative and quantitative analysis of myocardial perfusion
Semiquantitative perfusion analysis was performed on a 20-segment left ventricular model through an automated, operator-independent analysis where each segment was assigned a specific score according to a 5-point scale (0 = normal, 1 to 3 = mild to severe reduction, and 4 = absence of radioactive uptake). The segmental scores were then summed to produce summed stress (SSS), rest (SRS) and difference scores (SDS). Analysis was performed on a Xeleris workstation v.2.0551 (General Electric, USA) using the Cedars Sinai Quantitative Perfusion SPECT software. Additionally, fully quantitative polar maps were generated and compared against a normal tetrofosmin database provided with the software used. The ischemic myocardium was then calculated as absolute myocardial mass and as a percentage of the total myocardium.
Analysis of global and regional left ventricular function
End-diastolic (LVEDV), end-systolic (LVESV) left ventricular volume, and left ventricle ejection fraction (LVEF) were calculated as surrogate markers of global myocardial function, using the Cedars Sinai Quantitative Gated SPECT software. The software also generated automatically two regional LV function metrics: (a) the summed motion score (SMS), calculated as the sum of regional inner wall motion of all individual LV segments divided by the total number of these segments (scale range 0 to 10 mm) and (b) the summed thickening score (STS), calculated as the sum of regional wall thickening from end-diastole to end-systole of all individual LV segments divided by the total number of these segments (scale range 0% to 100%).
Analysis of Angiographic Data and Diagnostic Accuracy
Quantitative coronary angiography (QCA) was performed in all patients by physicians of our institution, unaware of the protocol of the study and stenosis ≥50% of the luminal diameter was considered significant. Since the study population included patients with previous myocardial infarctions, SSS and total ischemic mass defect (TMD = both reversible and irreversible defect) were used as a criterion of abnormal vs normal myocardial perfusion, with normal SSS cut-off values defined for each protocol through receiver operating characteristics (ROC) curves analysis.
Statistical Analysis
Continuous and normally distributed variables are presented as mean ± SD, while continuous variables with asymmetric distribution are presented as median (min-max) values. The normality assumption for continuous variables was evaluated by the Kolmogorov-Smirnov test. Categorical data are presented as counts and percentages. Pair-wise comparisons of continuous variables were performed with the Student’s pair t test or the Wilcoxon rank sum test, as appropriate. Image quality was compared with the McNemar’s Chi-square test. Differences in scintigraphic variables between patients with and without significant SSS discrepancies were evaluated with the Mann-Whitney test. The relationship and agreement of perfusion and function-related data between the two protocols were evaluated by linear regression and Bland-Altman analysis (BAA). To assess the equivalence of these data, the average measures intraclass correlation coefficient (ICC) for absolute agreement was also assessed. ROC curves analysis was performed, using the Youden’s Index13 (YI) for selection of the optimal SSS and TMD cut-off value of each protocol for identification of ≥50% diameter stenosis and the De Long method14 to compare the respective areas under the curve (AUC). P value for significance was set at 0.05 (two tailed). All analyses were performed with the use of SPSS software, version 17.
Results
Patients’ Characteristics
Characteristics of the study’s population are presented in Table 1. 28 patients had more than one difficulty factor.
Image Quality
Among the 78 patients, in one the fast protocol images were not suitable for analysis, because of significant subdiaphragmatic activity-related artifacts, while the delayed images were characterized as fair quality. This patient was subsequently excluded from all further analyses regarding counts, count ratios, scores, volumes, and mass deficit. In total, 73 (93%) and 77 (98%) of 78 studies were classified as optimal or good quality for Early and Late protocol, respectively (P = .12). Image quality-related parameters of the two protocols are presented in details in Table 2.
Counts and Count Ratios
Counts over heart, lungs, liver, and subdiaphragmatic space with the respective ratios at stress and rest for each protocol, as well as the significance values of their comparison between the two protocols are presented in Table 2. The two protocols demonstrated significant differences in all isolated counts at both stress and rest, with the exception of liver counts at rest. All measured counts were higher for the Early protocol. No significant differences in stress count ratios were observed between the two protocols. At rest, however, although the H/Liv ratio was similar between the two protocols, the H/Sub ratio was significantly lower in the Early imaging protocol.
Myocardial Perfusion Data
Ischemia scores for each protocol are presented in Table 2. The median SSS and SDS values for the Early imaging protocol were significantly higher than the respective Late protocol values, while no significant differences were observed for SRS between the two protocols. Regression analysis demonstrated a highly significant linear relationship between Early and Late SSS, SDS, and SRS (P < .001 in all cases), with ICCs being 0.86, 0.72, and 0.95 for SSS, SDS, and SRS, respectively (see Figure 3). BAA demonstrated a significant (P = .006) shift in the mean value of the SSS difference between the two protocols (SSST1-SSST2) of 2 (0.6 to 3.4, 95% CIs), while the 95% limits of agreement between the two protocols ranged from −10.4 to 14.5. There was also a significant (P = .02) shift in the mean difference of SDS between the two protocols, which according to BAA was 1.6 (0.2 to 2.9, 95% CIs) with −10 to 13.2, 95% limits of agreement. The results of these analyses are graphically presented in Figure 3. As shown in Table 2, total ischemic mass defect as percent (%) of the total myocardium mass (% TMD) was similar between the two protocols. % TMD also demonstrated a significant linear relationship between the two protocols (P < .001) with an ICC value of 0.91 (0.86 to 0.94, 95% CIs) and a mean difference between the two protocols of 1 (−0.1 to 2.2, 95% CIs) in BAA. Regarding patients with 3 vessels disease, one patient had normal images, five patients single, ten patients double and seven patients triple vessel disease pattern of ischemia. Polar maps demonstrating perfusion analysis results in a characteristic patient are presented in Figure 4.
Graphic representation of the relationships of ischemia scores between the two protocols. Upper row results of linear regression analysis. Middle row results of Bland–Altman analysis. Lower row Box-and-Whisker plots of ischemia scores for each protocol with ICC values between the two protocols for each score demonstrated on top. The red central box represents the values from the lower to the upper quartile (25 to 75 percentile). The middle red line represents the median value and the green lines the 95% confidence intervals for the median. A vertical line extends from the minimum to the maximum observed value, excluding outliers. An outlier is defined as a value that is smaller than the lower quartile minus 1.5 times the interquartile range or larger than the upper quartile plus 1.5 times the interquartile range. T1 early imaging, T2 = late imaging
Polar map images of a 52-year-old male with known, stable CAD, LVH, and percutaneous coronary intervention in LCx and LAD 2 years before the MPI study. He underwent treadmill exercise stress testing with the Bruce protocol for 8 minutes and had no symptoms during the test but ECG demonstrated marked horizontal ST depression of 3 mm in leads ΙΙ, ΙΙΙ, aVF, and V4-V6 at peak stress. Results of semiquantitative (SSS and SRS, lower row) and fully quantitative (ischemic mass defect during stress, upper row) perfusion analysis are presented for early (left) and late (right) imaging. Both protocols demonstrated a reversible defect in the inferior and basal inferolateral wall of the LV, but the early imaging protocol demonstrated also a small, reversible defect in the antero-apical region. SSS was 16 for early and 8 for late imaging, while TMD% during stress was 6% according to both imaging protocols. Post-MPI coronary angiogram demonstrated in-stent restenosis of 50% in the LAD, patent stent in LCx and a 80% stenosis in RCA
Global Myocardial Function Data
Volumetric data for each protocol are presented in Table 2. Rest volumes measurements, including LVEF, were similar between the two protocols. Stress volumes measured with the Early imaging protocol were significantly higher, but stress LVEF was again similar between the two protocols. Regression analysis demonstrated a highly significant linear correlation between all volumetric data of the two protocols (P < .001 in all cases) with all ICCs being >0.9 (see Figures 5 and 6), at both stress and rest. The mean difference of LVEF between the two protocols according to BAA was 1.1 (−0.7 to 2.2, 95% CIs) for stress and −0.2 (−1 to 0.7, 95% CIs) for rest, while the 95% limits of agreement between the two protocols ranged from −9 to 11.2 for stress and from −7.9 to 7.5 for rest, respectively (see Figures 5 and 6).
Graphic representation of the relationships of stress volumetric data between the two protocols. Upper row results of linear regression analysis. Middle row results of Bland-Altman analysis. Lower row Box-and-Whisker plots of stress volumetric data for each protocol with ICC values between the two protocols for each volume-related variable demonstrated on top. Characteristics of the Box-and-Whisker plot are the same as for Figure 3. EDV end-diastolic volume, ESV end-systolic volume, EF ejection fraction, ST1 early stress imaging, and ST2 late stress imaging
Graphic representation of the relationships of rest volumetric data between the two protocols. Upper row results of linear regression analysis. Middle row results of Bland-Altman analysis. Lower row Box-and-Whisker plots of rest volumetric data for each protocol with ICC values between the two protocols for each volume-related variable demonstrated on top, as for Figure 4. EDV end-diastolic volume, ESV end-systolic volume, EF ejection fraction, RT1 early rest imaging, and RT2 late rest imaging
MPI Variables Significantly Affected by Type of Stress
Table 3 presents the comparison of image quality-related count ratios and regional LV function metrics between the two protocols by type of stress used. In this subanalysis, it is shown that only rest H/Sub ratio for patients undergoing pharmacologic stress was significantly different between the two protocols. No significant differences were observed for SMS and STS between the two protocols, for patients undergoing either exercise or pharmacologic stress.
Diagnostic Accuracy
ROC curve analysis identified a YI-associated SSS threshold of 6 for both Early (YI = 0.45) and Late imaging (YI = 0.44) as the optimal values for separating patients with from patients without significant CAD. Using these values for classification of a study as normal or abnormal, the agreement between 99mTc-tetrofosmin SPECT and QCA for each of the two protocols is summarized in Table 4. Sensitivity was 81% for the Early and 80% for the Late imaging protocol, specificity was 65% for both protocols, while the AUC was 0.75 (0.64 to 0.84, 95% CIs) and 0.70 (0.59 to 0.80, 95% CIs) for the Early and Late imaging protocol, respectively (P = .23). Performing ROC curve analysis using %TMD instead of SSS, resulted in a %TMD threshold of 3% for both Early (YI = 0.49) and Late (YI = 0.45) imaging as the respective optimal values for patients classification. Using these thresholds, the Early imaging protocol predicted CAD in 48 of 57 patients and the Late imaging protocol in 46 of 57 patients (Early protocol sensitivity = 84%, Late protocol sensitivity = 81%), while both Early and Late imaging protocols excluded CAD in 13 of 20 patients (Early and Late protocol specificity = 65%). With the use of %TMD as a test to detect CAD, AUC was 0.74 (0.63 to 0.83, 95% CIs) for Early imaging and 0.73 (0.62 to 0.82, 95% CIs) for Late imaging (P = .78). ROC curve analysis results are presented in Figure 7.
Patients with Significant Discrepancies Between Early and Late Imaging SSS
Using a tight margin for defining patients with significant discrepancies in MPI findings between the two protocols, 26 patients (33%) were identified who had an absolute difference of SSS between Early and Late imaging larger than 2. Early SSS and SDS were significantly higher than the respective Late scores in these patients [15 (0 to 46) vs 10 (0 to 33), P = .002 for SSS, 4.5 (0 to 35) vs 2.5 (0 to 13), P = .012 for SDS], while a strong linear relationship was still observed for SSS, SRS, SDS, LVEDV, LVESV, and LVEF between the two protocols (P < .001 in all cases). It should be noted that patients with significant SSS discrepancies between the two protocols had significantly higher SSS [15 (0 to 46) vs 8 (0 to 37), P = .007] and SRS [8.5 (0 to 28) vs 4 (0 to 25), P = .006] values by the Early imaging protocol compared to patients with no such discrepancies.
Discussion
Feasibility, Diagnostic Accuracy, and Differences of the Fast Protocol Compared to the Standard Imaging Protocol
As a consequence of the hepatobiliary excretion of 99mTc-tetrofosmin, a significant subdiaphragmatic activity may be seen in the liver and bowel that can affect MPI in several ways,15,16 a phenomenon also known as the “liver-heart artifact.” This is the single most important limiting factor of early myocardial perfusion imaging protocols with 99mTc. Indeed, the initial small studies attempting myocardial perfusion imaging at intervals ranging from 5 to 15 minutes after stress injection reported mixed results.7,17,18 In our study, H/Sub ratio at stress was similar between the two protocols, while the rest H/Sub ratio was compatible with statistically but not clinically significant subdiaphragmatic activity during early imaging at rest, since this difference had no impact in the overall image quality comparison of the two protocols. The latter difference was largely limited to patients undergoing adenosine stress, an observation compatible with the classic knowledge that stress with vasodilators is associated with a higher risk of subdiaphragmatic 99mTc activity compared to exercise. Hence, our findings support the feasibility of early imaging and are in agreement with more recent, non-controlled19,20 and controlled8,21 studies, which have also demonstrated the feasibility of early imaging in terms of image quality appropriate for reliable interpretation. Furthermore, in our study the Early imaging protocol had similar diagnostic accuracy with the Late imaging protocol, demonstrating that early imaging is both technically feasible and diagnostically sufficient compared with the established imaging protocol. All volume and perfusion-related data demonstrated highly significant agreement and linear correlation between the two protocols, while for volumetric data the observed differences, even when statistically significant, should be considered minor from a clinical perspective.
Previous studies
Giorgetti et al8 first documented the feasibility and diagnostic accuracy of this fast protocol in a multicenter study of 120 patients that had a similar design to our single-center study but significant differences in important aspects. Specifically, 30% of patients in that study had no significant CAD and less than 7% triple vessel disease, while no information about BMI or LVH was available. In addition, both same day and 2 days 99mTc imaging protocols were used. The study found absolutely no significant differences in all examined variables. A few years later, Philippe et al21 provided partial validation for the feasibility of this protocol in a study of 194 patients, whose design included two stress (early, late) but only one rest imaging and most important no concomitant QCA. The population of this study was again significantly different compared to our study, as 60% of the patients included had normal MPI findings. According to the authors, this fact may explain in part why the differences between the two protocols were not significant. Furthermore, considerable inhomogeneity in patients available for each variable analysis and the inclusion of patients studied with rest-stress protocols represent additional drawbacks for the interpretation of these results as a sufficient validation of the clinically meaningful (i.e., stress-rest) use of an imaging protocol aiming at reducing total examination time. Finally, Mut et al22 reported recently on the feasibility of exercise stress early imaging in a controlled study of 229 patients with the use of 99mTc-sestamibi, which, however, shared most of the significant limitations of the Philippe et al study. Specifically, 73% of patients in that study had normal scans while its design included two stress and one rest imaging with no concomitant QCA. In addition, there was no evaluation of regional LV function.
The Hypothesis of Enhanced Ischemia Detection
An intriguing theoretical advantage of a fast imaging protocol is the potential for identifying more perfusion defects associated with significant coronary arteries stenosis, as imaging is performed closer to the stressor effect. Indeed, increased SSS in the Early imaging protocol was a uniform finding in all related studies, but it was not translated in a significant difference in diagnostic accuracy in our study, as it was the case with the Giorgetti study.8 Furthermore, in our study, increased Early SSS was not combined with increased %TMD or decreased Early motion scores. The perfusion-motion/thickening scores dissociation was also observed in the Philippe study, while in the Giorgetti study, SMS in Early Stress imaging was paradoxically higher than SMS in Late Stress imaging in patients with significant SDS discrepancies, the only patients in whom SMS data were available. It is conceivable that if Early imaging truly detects more ischemia, increased SSS should be accompanied by worst Early motion and/or thickening scores as a result of the partial volume effect since the larger ischemic burden should be expected to cause more pronounced wall thinning. We did not observe such a relationship in our study, which, however, was not specifically designed to address this issue since it mixed exercise and adenosine stress. The subanalysis performed by stress type, demonstrated non-significantly lower SMS in Early vs Late Stress imaging in patients undergoing exercise stress testing (i.e., the only group in which decreased SMS would be expected based on the differential effects of exercise and vasodilator stress on segmental myocardial function). However, this finding should be considered only as hypothesis generating.
Clinical Implications of the Fast Imaging Protocol
Reduction of the time interval between radiotracer injection and image acquisition contributes to the shortening of the total time required for the completion of a MPI study. The latter has become increasingly important, particularly with the advent of cadmium-zinc-telluride gamma cameras that allow acquisition within a few minutes,23 since it has an obvious and important benefit for both patients (shorter waiting times and increased convenience) and laboratories (performance of more studies per day, increasing efficiency). Beyond this logistic approach, however, Early imaging could have substantial implications in the clinical management of CAD patients as well, if the concept of more ischemia detection with the Early protocol is proved in future studies. The COURAGE24 trial introduced a threshold of 10% ischemic myocardium for deriving benefit from revascularization. Based on this finding, it is conceivable that a small increase in percent ischemic myocardium detected with Early imaging could have a significant impact in the management of the occasional patient in whom the traditional imaging protocol would detect a reversible ischemic defect slightly below 10% of the total myocardium mass.
New Knowledge Gained
This is the first study to evaluate, in a controlled fashion, the feasibility and diagnostic accuracy of a standardized, single-day, stress-rest, 99mTc-tetrofosmin imaging protocol, with a 15-minute delay for initiation of imaging after radioisotope administration, at both stress and rest, and a total duration of maximum 150 minutes. Currently, ASNC guidelines4,5 give the option for the application of a 10 to 15 minutes delay for stress—although much longer delays are usually employed in the real world—but not for rest. The results of this study provide additional support about the potential that fast myocardial perfusion imaging has to be applied in clinical practice.
Limitations
The main limitation of this study is the mixing of exercise and vasodilator stress. Although this mixing does not affect the principal conclusions of the study, regarding feasibility and diagnostic accuracy of the fast protocol, it obscures the elucidation of the pathophysiologic mechanism of the observed results. It is known that stress with vasodilators may alter perfusion without induction of wall motion abnormalities and although no significant differences were observed in regional LV function metrics between the two protocols, either for exercise or for pharmacologic stress, the design of our study did not allow for a statistically robust subanalysis by stressor type. Large-scale studies are still required to comprehensively evaluate the ischemia and motion scores association of the Early imaging protocol and conclude on its true potential for increased sensitivity for CAD diagnosis.
A number of other limitations also apply to this study. First, since the available quantitative perfusion software packages do not include normal reference databases for patients imaged with the fast protocol, early imaging data were compared against the standard normalcy database provided by the software manufacturer, with the potential for false perfusion defects generation. The relatively higher diagnostic accuracy of the Early imaging protocol argues against this possibility; however, before Early imaging is applied normal databases of healthy individuals studied specifically at 15-minute post-tetrofosmin injection must be produced. Second, as this was a validation study, a degree of stenosis ≥50% was chosen as a threshold between significant and non-significant stenosis, in accordance to the Giorgetti study. However, it has been reported25 that blood flow in regions supplied by vessels with 50% to 70% area stenosis showed a similar response to coronary vasodilatation compared to normal subjects and patients with stenosis <50% and even when such reductions in blood flow during stress are present, the corresponding relative count reduction is hard to be detected by a radiotracer such as 99mTc-tetrofosmin, whose kinetic at high flows is largely unsatisfactory. Third, the semiquantitative perfusion analysis performed was computer based and the software employed used a 20-segment LV model. A 17-segment scoring system for SPECT MPI is preferred over the 20-segment system, because it more accurately represents the size of each segment.26 However, since the prognostic implications of the 17- and 20-segment scoring systems have been shown to be equivalent when converted to percent myocardium abnormal27 and myocardial mass was also calculated, the LV segmentation model used had limited effects in the results of the present study. It should be also noted that this study was not appropriate for defining exact figures of sensitivity and specificity of the fast protocol, but only for comparison of its performance to the standard imaging protocol. This stems from the fact that the correlation between coronary angiography and MPI is flawed, because a 50% diameter stenosis was used as a threshold of obstructive CAD, patients with previous revascularization were included and nearly one third of the patients studied had prior MI (i.e., a case with a patent vessel supplying an infarcted area would be falsely classified as false positive). Furthermore, we chose to validate the fast imaging protocol in a population much different than the one used in the Giorgetti study, in order to extent its validity. The assumption in selecting the study’s population is that if the fast protocol performs well in diagnostically challenging patients, it should be at least as good in the general population. However, this concept was not specifically tested.
Finally, some secondary characteristics of the Late imaging protocol used as a reference standard in this study, present minor deviations from the typical values recommended by ASNC. Specifically, the ratio of radioactive doses used at stress and rest (1:2.5) was in accordance with EANM Guidelines6 for Greece, but somewhat lower compared to the one recommended by ASNC Guidelines4,5 (1:3). The stress:rest dose ratio affects predominately the time delay between the two injections (i.e., stress and rest imaging) which according to ACC Guidelines is recommended to be in the range of 30 minutes to 4 hours, assuming a 1:3 ratio. Although this delay in the case of our study was well within the above time range, there are no recommended time delays specifically adjusted for a 1:2.5 ratio, as administered activities stated in the ACC Guidelines are commonly used in the United States but vary in other countries and issues regarding the minimum time interval between the two radiotracer injections are not fully settled.
Abbreviations
- CAD:
-
Coronary artery disease
- SSS:
-
Summed stress score
- SDS:
-
Summed difference score
- SRS:
-
Summed rest score
- LVEDV:
-
LV end-diastolic volume
- LVESV:
-
LV end-systolic volume
- BAA:
-
Bland-Altman analysis
- TMD:
-
Total ischemic mass defect
- ICC:
-
Intraclass correlation coefficient
- QCA:
-
Quantitative coronary angiography
References
WHO. The top ten causes of death. Fact sheet no 310; 2013.
Malvern PAMR. The Myocardial Perfusion Imaging Market Guide (U.S.) Supplement to the U.S. Imaging Market Guide. Inc 2007.
Einstein AJ, Moser KW, Thompson RC, Cerqueira MD, Henzlova MJ. Radiation dose to patients from cardiac diagnostic imaging. Circulation 2007;116:1290-305.
Henzlova MJ, Cerqueira MD, Mahmarian JJ, Yao SS. Stress protocols and tracers. J Nucl Cardiol 2006;13:e80-90.
Holly TA, Abbott BG, Al-Mallah M, Calnon DA, Cohen MC, DiFilippo FP, et al. Single photon-emission computed tomography. J Nucl Cardiol 2010;17:941-73.
Hesse B, Tagil K, Cuocolo A, Anagnostopoulos C, Bardies M, Bax J, Bengel F, Busemann Sokole E, Davies G, Dondi M, Edenbrandt L, Franken P, Kjaer A, Knuuti J, Lassmann M, Ljungberg M, Marcassa C, Marie PY, McKiddie F, O’Connor M, Prvulovich E, Underwood R, van Eck-Smit B. EANM/ESC procedural guidelines for myocardial perfusion imaging in nuclear cardiology. Eur J Nucl Med Mol Imaging 2005;32:855-97.
Jain D, Wackers FJ, Mattera J, McMahon M, Sinusas AJ, Zaret BL. Biokinetics of technetium-99 m-tetrofosmin: myocardial perfusion imaging agent: implications for a one-day imaging protocol. J Nucl Med 1993;34:1254-9.
Giorgetti A, Rossi M, Stanislao M, Valle G, Bertolaccini P, Maneschi A, et al. Feasibility and diagnostic accuracy of a gated SPECT early-imaging protocol: a multicenter study of the Myoview Imaging Optimization Group. J Nucl Med 2007;48:1670-5.
Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging 2015;16:233-70.
Mahajan N, Polavaram L, Vankayala H, Ference B, Wang Y, Ager J, et al. Diagnostic accuracy of myocardial perfusion imaging and stress echocardiography for the diagnosis of left main and triple vessel coronary artery disease: a comparative meta-analysis. Heart 2010;96:956-66.
Burrell S, MacDonald A. Artifacts and pitfalls in myocardial perfusion imaging. J Nucl Med Technol 2006;34:193-211.
Hansen CL, Woodhouse S, Kramer M. Effect of patient obesity on the accuracy of thallium-201 myocardial perfusion imaging. Am J Cardiol 2000;85:749-52.
Youden WJ. Index for rating diagnostic tests. Cancer 1950;3:32-5.
DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics 1988;44:837-45.
Dvorak RA, Brown RK, Corbett JR. Interpretation of SPECT/CT myocardial perfusion images: common artifacts and quality control techniques. Radiographics 2011;31:2041-57.
Nuyts J, Dupont P, Van den Maegdenbergh V, Vleugels S, Suetens P, Mortelmans L. A study of the liver-heart artifact in emission tomography. J Nucl Med 1995;36:133-9.
Matsunari I, Tanishima Y, Taki J, Ono K, Nishide H, Fujino S, et al. Early and delayed technetium-99m-tetrofosmin myocardial SPECT compared in normal volunteers. J Nucl Med 1996;37:1622-6.
Hattori N, Tamaki N, Masuda I, Taniguchi Y, Kitano H, Kudoh T, et al. An ultrashort 1-day protocol of Tc-99m tetrofosmin. Clin Nucl Med 1999;24:85-91.
Tadehara F, Yamamoto H, Tsujiyama S, Hinoi T, Matsuo S, Matsumoto N, et al. Feasibility of a rapid protocol of 1-day single-isotope rest/adenosine stress Tc-99m sestamibi ECG-gated myocardial perfusion imaging. J Nucl Cardiol 2008;15:35-41.
Matsumoto N, Sato Y, Suzuki Y, Yoda S, Kunimasa T, Kato M, et al. Usefulness of rapid low-dose/high-dose 1-day 99mTc-sestamibi ECG-gated myocardial perfusion single-photon emission computed tomography. Circ J 2006;70:1585-9.
Philippe L, Merino B, Blaire T, Bailliez A, Casset-Senon D, Levy M, et al. Tetrofosmin early time gated post-stress single-photon emission computed tomography imaging: feasibility and potential benefits. J Nucl Cardiol 2011;18:62-72.
Mut F, Giubbini R, Vitola J, Lusa L, Sobic-Saranovic D, Peix A, et al. Detection of post-exercise stunning by early gated SPECT myocardial perfusion imaging: results from the IAEA multi-center study. J Nucl Cardiol 2014;21:1168-76.
Miller TD, Askew JW, O’Connor MK. New toys for nuclear cardiologists. Circ Cardiovasc Imaging 2011;4:5-7.
Shaw LJ, Berman DS, Maron DJ, Mancini GB, Hayes SW, Hartigan PM, et al. Optimal medical therapy with or without percutaneous coronary intervention to reduce ischemic burden: results from the Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation (COURAGE) trial nuclear substudy. Circulation 2008;117:1283-91.
Di Carli M, Czernin J, Hoh CK, Gerbaudo VH, Brunken RC, Huang SC, et al. Relation among stenosis severity, myocardial blood flow, and flow reserve in patients with coronary artery disease. Circulation 1995;91:1944-51.
Cerqueira MD, Weissman NJ, Dilsizian V, Jacobs AK, Kaul S, Laskey WK, et al. Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart. A statement for healthcare professionals from the Cardiac Imaging Committee of the Council on Clinical Cardiology of the American Heart Association. J Nucl Cardiol 2002;9:240-5.
Berman DS, Abidov A, Kang X, Hayes SW, Friedman JD, Sciammarella MG, et al. Prognostic validation of a 17-segment score derived from a 20-segment score for myocardial perfusion SPECT interpretation. J Nucl Cardiol 2004;11:414-23.
Disclosure
No relationships with industry or forms of financial support to be disclosed.
Author information
Authors and Affiliations
Corresponding author
Additional information
See related editorial, doi:10.1007/s12350-016-0461-z.
Rights and permissions
About this article
Cite this article
Katsikis, A., Theodorakos, A., Kouzoumi, A. et al. Fast myocardial perfusion imaging with 99mTc in challenging patients using conventional SPECT cameras. J. Nucl. Cardiol. 24, 1314–1327 (2017). https://doi.org/10.1007/s12350-016-0431-5
Received:
Revised:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12350-016-0431-5