Abstract
Background
Transient ischemic dilation (TID) in the setting of an abnormal SPECT radionuclide myocardial perfusion imaging (MPI) study is considered a marker of severe and extensive coronary artery disease (CAD). However, the clinical significance of TID and its association with CAD in patients with an otherwise normal MPI study is unclear.
Methods
From a database of patients who underwent MPI over a 9-year period, 96 without known cardiac history who had normal image perfusion patterns, and who underwent coronary angiography within 6 months, were identified. TID quantitative values were derived. To adjust for varying stress and image protocols, a TID index based on published threshold values was derived for each patient, with >1 considered as TID. We examined the relationship of TID to the presence/extent of CAD, and to a CAD prognostic index. TID was also correlated with patient survival. To address referral bias, survival in a separate cohort of 3,691 patients with a normal perfusion MPI who did not undergo angiography in the 6-month interval was correlated with the presence and severity of TID.
Results
For 28 (29.2%) patients with normal MPI perfusion patterns but with TID, there was no increased incidence of CAD, multivessel or left main disease, or a higher prognostic index compared with no TID. In addition, there was no increased mortality associated with TID in both the angiography cohort and in the patients who did not undergo immediate angiography.
Conclusions
TID in patients with an otherwise normal SPECT MPI study does not increase the likelihood of CAD, its extent or severity, and is not associated with worsened patient survival.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Transient ischemic dilation (TID) of the left ventricle on a stress single-photon emission computed tomography (SPECT) radionuclide myocardial perfusion imaging (MPI) study is thought to reflect myocardial ischemia that is sufficiently severe and extensive to cause visually apparent LV enlargement on the post-stress relative to the post-rest images. Several pathophysiologic mechanisms have been proposed, including actual stress-induced transient cavity dilation,1 a lack of subendocardial tracer uptake in the setting of extensive subendocardial ischemia without true anatomic cavity enlargement,2 a stress induced decrease in LV systolic function from stunning that appears as TID in the summed SPECT images,3,4 or perhaps various combinations of these. Regardless of the mechanism of the phenomenon, the presence of TID in patients with an abnormal MPI study has been shown to be a marker of severe and extensive CAD,1,5-7 and in a few studies to confer increased risk for cardiovascular events.8-10
Nevertheless, the significance of TID in patients with otherwise normal MPI images is not well understood as such patients have typically been excluded from investigative studies. One study did find an increased likelihood of a cardiac event in these patients, but most events were revascularization procedures rather than hard cardiac events, with therefore a potential bias from the image findings leading to the events rather than there being true increased patient risk.11
Therefore, it remains unclear how best to approach patients with TID and otherwise normal SPECT images. While many people consider TID and normal SPECT to indicate a significant likelihood of balanced ischemia from multivessel coronary artery disease (CAD), to our knowledge there are no published manuscripts correlating TID as an isolated finding with the anatomic extent and severity of CAD. A recent editorial states that the finding of isolated TID is usually not associated with severe CAD and that it would not be appropriate to perform invasive coronary angiography on the basis of this observation alone, but then also suggests that in some clinical instances isolated TID could indicate high risk “balanced” ischemia.12
Therefore, to further investigate the significance of isolated TID on SPECT MPI, i.e., to specifically assess whether this SPECT image finding increases the likelihood of balanced ischemia from multivessel disease, we queried our nuclear cardiology database to find patients with normal perfusion images who underwent cardiac catheterization. We examined the relationship of the presence/absence and quantitative severity of TID to the extent/severity of CAD on coronary angiography and to patient survival. In addition, to account to some extent for catheterization referral bias, we assessed the survival of patients with normal perfusion images who did not undergo cardiac catheterization in relation to the presence/absence and quantitative severity of TID, with the reasoning being that the absence of a worsened prognosis suggests that balanced ischemia/multivessel disease was infrequent.
Methods
Study Population
The study patient selection process is detailed in Figure 1. To summarize, following IRB expedited review and approval, we reviewed a prospectively created database of over 20,000 consecutive patients who underwent stress radionuclide MPI at our institution between 2000 and 2009. We identified all patients without previously known cardiac history (no myocardial infarction, no coronary revascularization, no cardiomyopathy) who had normal or probably normal perfusion images on initial clinical read, and for whom a TID value had been entered into the database, approximately 6,000 patients. From these we chose patients who underwent cardiac catheterization within 180 days of nuclear testing, without intervening intervention or cardiac event, yielding 168 patients. Images of these patients were retrieved and reprocessed to assure that the images were truly normal in terms of perfusion (summed stress score (SSS) < 4).13 All patients with equivocal findings, those with probable cardiomyopathy, left bundle branch block or pacemaker perfusion patterns, and doubles (for those who had numerous tests during the time interval, only the first test was used) were excluded, resulting in the 96 patients who comprise the main cohort of the study (Cohort 1). For these patients the TID score was based on the reprocessed value rather than that obtained at the initial clinical read.6,14
Study patient selection process. CABG, coronary artery bypass grafting; CHF, congestive heart failure; DCM, dilated cardiomyopathy; LBBB, left bundle branch block; MPI, myocardial perfusion imaging; PCI, percutaneous coronary intervention; PPM, permanent pacemaker; pts, patients; cath., catheterization; SSS, summed stress score
To take into account the confounding influence of catheterization referral bias, a separate cohort of patients without previous cardiac history who did not undergo cardiac catheterization within 6 months of SPECT imaging, with a TID value entered in the database, and with a clinical read data entry of normal perfusion (SSS < 4; images in this cohort were not reprocessed nor re-reviewed) but who had not undergone cardiac catheterization within 180 days were identified, yielding 3691 patients (Cohort 2).
Stress Testing and Imaging
Patients had undergone stress radionuclide single-photon emission computed tomography (SPECT) myocardial perfusion imaging using standard techniques.15 Radiopharmaceutical dosing, image acquisition, and processing were performed as per published guidelines.16 At the time the patients in this study underwent testing, dual isotope imaging was standard in many institutions, and was thus used for the majority of our patients.
Image Interpretation
SPECT images had been visually interpreted during a standard clinical read by experienced readers blinded to catheterization data, but with all other clinical data available to make a final clinical interpretation. All SPECT images were scored semiquantitatively using the standard 17-segment scoring method, generating a summed stress score (SSS), summed rest score (SRS), and summed difference score (SDS) for each patient.16 During the clinical read, each image had been interpreted globally as normal, probably normal, equivocal, probably abnormal, or abnormal. ECG-gated SPECT acquisition was performed in all cases, with the RR segments divided into 16 intervals.
Measurement of TID
TID values were calculated from the summed SPECT images using a commercially available automated program (QPS = quantitative perfusion score, Cedars-Sinai, Los Angeles, California) which allows manual operator interaction if required. The TID ratio is derived from rest and stress endocardial volumes bounded by endocardial surface and valve plane.6 To adjust for known varying TID values and normal thresholds of the different stresses and imaging protocols, we derived a TID index, dividing the raw QPS-derived TID values by published normal thresholds. A TID index > 1 was considered to be TID “positive” (“TID +”), TID ≤ 1 was designated “TID−.” For the entire population of patients studied (Cohorts 1 and 2), the mean TID index was 0.87 ± 0.15, with a median of 0.86. The patients were divided into TID quartiles based on the distribution of these patients, with the groupings as follows—Quartile I: 0.31-0.77 (976 total patients); Quartile II: 0.78 = 0.86 (938 total patients); Quartile III: 0.87 = 0.95 (908 total patients); Quartile IV: 0.96-1.88 (965 total patients).
Angiographic Analysis
Angiographic data were obtained from cardiac catheterization reports, composed of independent angiographers at the time of the procedure. Significant coronary artery disease (CAD) was defined as luminal coronary diameter stenosis of ≥70% in at least one major coronary artery distribution: left anterior descending (LAD), left circumflex artery (LCx), or right coronary artery (RCA). Significant left main (LM) disease was defined as luminal diameter stenosis of ≥50%. Multi-vessel CAD was defined as either significant left main disease, or two-vessel or triple-vessel CAD. To more precisely characterize the extent and severity of CAD, a CAD prognostic index based on the description by Mark et al.18 was derived for our patients based on the number of vessels diseased as well as the location, given higher weight to lesion in proximal segments of larger vessels. The presence and extent of coronary artery disease were correlated with the presence and the severity of TID.
Survival Analysis
Data for Cohorts 1 and 2 were uploaded into Montefiore Medical Center’s Clinical Looking Glass™ (CLG), an interactive software application system developed at our institution for the evaluation of health care quality, effectiveness, and efficiency.19-21 Among other functions, CLG can merge patient information with the national Social Security Death Registry to generate survival analysis curves. We analyzed all-cause mortality of patients from both cohorts to determine the relation of TID presence or severity with patient survival (note that the Social Security Death Registry does not provide the cause of death).
Statistical Analysis
Continuous variables were expressed as the means ± standard deviation, and categorical variables were expressed as percentages (%). The Student’s t test was used for analysis of continuous data, and the χ2 test was used to compare differences between proportions of categorical variables. The extent and severity of CAD between subjects with various degrees of TID were analyzed using ANOVA. Univariate analysis was performed to determine how a variety of key variables (age, gender, pharmacologic stress, diabetes mellitus, hypertension, baseline abnormal ECG, ECG ischemia during stress) compared with the presence of TID in terms of the presence of CAD or MVD/LM, and if any these variable correlated with CAD or MVD/LM in the patients who had TID. Survival analysis was depicted using Kaplan-Meier curves, and differences in the event occurrence rate between the two groups were analyzed using a log-rank Mantel-Haenszel test. For all analyses, P values <.05 were considered statistically significant.
Results
Patient Characteristics
Cohort 1 comprised a total of 96 patients. While one cannot say exactly why these patients with normal SPECT perfusion images were referred for cardiac catheterization within 6 months of nuclear testing, compared with the Cohort 2 patients who did not undergo cardiac catheterization in such close proximity to SPECT, the Cohort 1 patients more often had various clinical factors consistent with increased cardiac risk. These included a higher Diamond/Forrester pre-test likelihood of CAD.22 (47.5% ± 28.3% vs 38.9% ± 27.5%, P < .01), and were often taking cardiac medications at the time of testing (β-blockers: 51% vs 35%, P < .01; nitrates: 10% vs 3%, P < .001; angiotensin converting enzymes inhibitors: 44% vs 31%, P < .05; aspirin: 60% vs 44%, P < .005), suggesting that they may have been more symptomatic. They also more frequently had hypertension (78% vs 71%, P < .05), were more often referred for pharmacologic stress (78% vs 62%, P < .05), more frequently had an abnormal baseline ECG (73% vs 62%, P < .05), and had a lower LV ejection fraction (61% ± 15% vs 70% ± 10%, P < .001). Cohort 1 patients were also more often men (51% vs 29%, P < .001).
Of these 96 patients, 28 were “TID+” and 68 “TID−”. As in Table 1, the mean age was lower for “TID+” than for “TID−” patients. There were no significant differences in the type of chest pain/angina, the prevalence of hypertension or diabetes mellitus, cardiac medications taken, the method of the stress or imaging, the baseline or stress ECG results, or the LV ejection fraction.
In terms of TID quartiles, 12 patients (12.5%) were in quartile I, 13 (13.5%) were in quartile II, 30 (31.3%) were in quartile III, and 41 (42.7%) were in quartile IV. Thus, when considering the entire study population (Cohorts 1 and 2) patients in higher TID quartiles were more likely to undergo cardiac catheterization—1.2% (12/976) for quartile I, 1.4% (13/938) for Quartile II, 3.3% (30/908) for quartile III, and 4.2% (41/965) for quartile IV (P < .001).
TID and Coronary Angiography
The interval between the SPECT study and coronary angiography was 26 ± 49 days. CAD results were similar in “TID+” and “TID−” patients, shown in Table 2. In particular, the two groups were similar with regard to the presence of CAD, the number of vessels with significant stenoses, or the CAD prognostic index. For example, although “TID+” is often considered to have a high correlation with multivessel or left main disease, such disease was present in only 11% of patients with “TID+” compared with 16% of those with “TID−” (P = NS).
The distribution of the number of vessels with a significant coronary stenosis was similar in patient with and without TID, depicted in Figure 2. As illustrated in Figure 3, the distributions of CAD prognostic indices were similar across the four TID index quartiles, without the presence of more extensive or severe coronary disease in the higher TID groups.
None of the variables assessed by univariate analysis correlated with the presence of CAD, or the presence of multivessel or left main disease (MVD/LM). Of the 28 patient with TID+, the presence of diabetes did increase the likelihood of CAD compared with patients who did not have diabetes—60% (6/10) vs 11% (2/18) (P = −.11), respectively, but did not significantly increase the likelihood of MVD/LM.
TID and All Cause Mortality
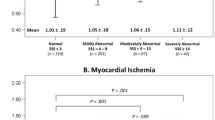
Patients in Cohort 1 were followed for 3.5 ± 2.2 years (98% follow-up). The mortality in patients with “TID+” was not increased compared with “TID−” patients, 3.7% vs 6.0%, respectively (P = NS), with survival curves shown in Figure 4.
Characteristics of Cohort 2 patients are shown in Table 3. For these patients, those who were TID+ were less often male, had more non-anginal or no chest pain at the time presentation for stress SPECT testing, were more often taking aspirin, more often underwent pharmacologic stress, had more stress ECG ischemia, and had a lower LVEF. Cohort 2 patients were followed for 3.6 ± 1.9 years (95% follow-up), and despite the aforementioned somewhat worsened clinical characteristics of the TID+ subgroup, again there was a similar mortality in “TID+” and “TID−” patients (8.4% vs 6.0%, respectively, P = NS), with survival curves (Figure 5) that essentially superimposed.
Sub-group analysis for both cohorts showed no difference in survival among the various TID quartiles, illustrated in Figure 6 for Cohort 2 (for Cohort 1, subgroup quartile analysis yielded too few patients for meaningful analysis).
Discussion
The presence of TID in patients with an abnormal SPECT MPI study is considered to be a marker of severe and extensive CAD that confers increased risk for cardiovascular events.1,5-10 Such patients are therefore often referred for cardiac catheterization with intent to revascularize. However, despite the absence of clear data, such an approach is often extrapolated to patients who have TID in the presence of an otherwise normal MPI study, with these patients commonly also referred for cardiac catheterization out of concern for the possible presence of multivessel disease and balanced ischemia. Nevertheless, our study of close to 100 patients with normal perfusion images who underwent cardiac catheterization within 6 months of SPECT found no TID associated increase in the presence of CAD, the presence of multivessel or left main disease, or in the CAD prognostic index. Patients who had TID had no worsened survival compared with patients who did not. Similarly, for a much larger group of over 3,000 patients with normal (perfusion pattern) SPECT images who did not (within 6 months) undergo cardiac catheterization, the presence of TID also did not increase mortality, or was there any increase in mortality as the extent of TID increased.
Thus, our findings indicate that in the setting of an otherwise normal SPECT perfusion image study, TID infrequently indicates balanced ischemia, and in this instance is not useful as a marker for severe or extensive CAD. In addition, there is no increased mortality compared with patients who do not have TID.
Previous Reports
To our knowledge there are no published manuscripts on the correlation of TID with the anatomic extent and severity of CAD in patients with an otherwise normal MPI study. Studies that have addressed the relation of TID to coronary anatomy have excluded patients with normal SPECT MPI.1,5-7
There are several studies reporting prognostic implications of TID in patients with otherwise normal SPECT images. Abidov et al. studied a group of 1,560 patients with no perfusion defects, and a second group of 2,037 patients with SPECT scans considered normal by the institution’s standard definition (SSS ≤ 3) that therefore also included patients with minimal defects considered too small to be called abnormal.11 In follow-up of slightly over a mean of 2 years, the annual hard event rate (cardiac death and non-fatal MI) was extremely low in both the groups (<0.5%), but the patients in the highest TID quartile in both groups had a significantly higher total event (cardiac death, non-fatal MI, and revascularization 60 days after SPECT) rate than patients in the lower three quartiles. In the first cohort the highest TID quartile was an independent predictor (with diabetes, age, and typical angina) of total events, having a hazard ratio of 2.3. In that study, though, it is unclear how the presence of TID might have biased the decision to proceed to revascularization and thereby increase the total event rate.
Several other studies reported no increased cardiac event rate associated with TID in the presence of otherwise normal perfusion images. Baddi et al23 followed 1,200 patients with normal perfusion images for approximately 4 years, and for the 25 patients who had TID there were no deaths, no cardiac events or hospitalizations, and the patients were symptom free. More recently, Hakeem et al. found that of 1,003 patients with normal MPI (SSS < 4), for the 3.8% of patients with TID followed for about 2 years, there was no increase in all cause mortality, although there was a trend toward increased cardiac events (21% vs 10%, P = .06).24
Mechanisms
The mechanism of TID is not entirely clear. Initial papers by Stolzenberg and by Weiss et al.1,25 measured an area derived from tracing the epicardial border of planar images that therefore would appear to represent true stress-induced cardiac enlargement. However with SPECT imaging, TID represents a change in the inner cavity dimension that is both apparent visually and quantitatively measurable by standard software programs which calculate the change in area or volume circumscribed by software determined endocardial border. As TID is customarily derived from summed (systolic and diastolic) SPECT images, this inner cavity dimension represents a complex interplay between left ventricular systolic functional changes with stress, and perfusion tracer uptake in the myocardial subendocardium, with likely a component of true anatomic cavity dilation as well.2-4,26 Given the likely complex mechanism of the TID phenomenon, it is not be surprising that it occurs in association with pathophysiology other than extensive coronary disease. For example, there are several reports of TID associated with hypertension and left ventricular hypertrophy.27,28 Smelly et al29 reported an independent association of TID with a hypertensive response to exercise in patients with otherwise normal perfusion images. Hypertensive and hypertrophic conditions may result in stress-induced subendocardial ischemia because of a greater reduction in subendocardial than in transmural perfusion, thereby accounting for the TID.30 Likewise, diabetes has been associated with TID independent of the severity of CAD, perhaps also accounted for by subendocardial ischemia, possibly related to flow reserve abnormalities in microvessels.31 Nevertheless, in both of our patient cohorts, those with TID did not have more frequent hypertension or diabetes.
Of course, in some cases computer measured TID may be the result of technical errors related to limits of the computer software’s ability to detect the endocardial border or the myocardial valve plane, or from errors in slice matching between the stress and rest images.32 In addition, in patients with small left ventricles, small statistically random changes in cavity size between stress and rest images can yield high ratios.6,26
Clinical Implications
Contrary to the significance of TID in patients with concomitant MPI perfusion defect(s), the significance of TID as an isolated finding in MPI does not appear to increase the likelihood of severe CAD or convey increased mortality. Thus, our results show no evidence that TID alone should be used to guide decisions regarding further invasive testing, such as coronary angiography, or for risk stratification beyond conventional cardiac risk factors.
Limitations
There are several limitations to this study. The reported findings are based on data obtained from a nuclear cardiology database of a single center with unique characteristics, and thus may not be applicable to other centers. Corroboration of our findings in other settings and with larger patient populations is needed.
In addition, the catheterization referral bias that results in few referrals of patients with normal perfusion pattern images for invasive coronary angiography skews the data. While we did not find a worsened survival in the patients with TID who were not immediately (<6 months) referred for catheterization, it is still possible that many had severe and extensive CAD, doing well in terms of survival because of the protective effects of current aggressive medical therapies (although our results therefore do suggest that avoiding an invasive approach does no harm in this regard). Perhaps, the widespread availability of noninvasive cardiac CTA may allow accumulation of larger patient cohorts in which the concepts considered here can be explored further, although results from such analyses would still be affected to some degree by referral bias to cardiac CTA.
In addition, due to the retrospective nature of our study, specific cardiac event data are not available. As we only analyzed all-cause mortality, we cannot know if the patients with TID had a higher cardiac mortality that was off-set by a higher non-cardiac mortality in patients without TID, although this would be unlikely, especially as no differences in all-cause mortality were seen for any of the multiple survival analyses performed. As discussed above, at least one group reports a trend toward a higher non-revascularization cardiac event rate in association with TID despite there being no survival decrease.24 Certainly in the current era aggressive approaches to acute coronary syndromes have significantly improved survival, making it more difficult to show mortality differences, particularly over shorter follow-up times. At the same time, there is no evidence that an invasive approach to otherwise stable coronary disease prevents acute coronary syndrome, again arguing that avoiding cardiac catheterization in clinically stable patients with TID but otherwise normal perfusion images is a an appropriate management approach.
Conclusions
The presence of TID in our cohort of patients with otherwise normal SPECT myocardial perfusion images did not predict extensive and severe CAD. In addition, the presence of TID in these patients did not increase the mortality risk when compared with those who did not have TID. Thus, the presence of TID as an isolated finding in stable patients with an otherwise normal SPECT MPI studies does not appear to indicate a need for invasive coronary angiography.
References
Weiss AT, Berman DS, Lew AS, Nielsen J, Potkin B, Swan HJ, et al. Transient ischemic dilation of the left ventricle on stress thallium-201 scintigraphy: A marker of severe and extensive coronary artery disease. J Am Coll Cardiol 1987;9:752-9.
Iskandrian AS, Heo J, Nguyen T, Lyons E, Paugh E. Left ventricular dilatation and pulmonary thallium uptake after single-photon emission computer tomography using thallium-201 during adenosine-induced coronary hyperemia. Am J Cardiol 1990;66:807-11.
Heston TF, Sigg DM. Quantifying transient ischemic dilation using gated SPECT. J Nucl Med 2005;46:1990-6.
Hung GU, Lee KW, Chen CP, Lin WY, Yang KT. Relationship of transient ischemic dilation in dipyridamole myocardial perfusion imaging and stress-induced changes of functional parameters evaluated by Tl-201 gated SPECT. J Nucl Cardiol 2005;12:268-75.
Takeishi Y, Tono-oka I, Ikeda K, Komatani A, Tsuiki K, Yasui S. Dilatation of the left ventricular cavity on dipyridamole thallium-201 imaging: A new marker of triple-vessel disease. Am Heart J 1991;121:466-73.
Mazzanti M, Germano G, Kiat H, Kavanagh PB, Alexanderson E, Friedman JD, et al. Identification of severe and extensive coronary artery disease by automatic measurement of transient ischemic dilation of the left ventricle in dual-isotope myocardial perfusion SPECT. J Am Coll Cardiol 1996;27:1612-20.
Abidov A, Bax JJ, Hayes SW, Cohen I, Nishina H, Yoda S, et al. Integration of automatically measured transient ischemic dilation ratio into interpretation of adenosine stress myocardial perfusion SPECT for detection of severe and extensive CAD. J Nucl Med 2004;45:1999-2007.
McClellan JR, Travin MI, Herman SD, Baron JI, Golub RJ, Gallagher JJ, et al. Prognostic importance of scintigraphic left ventricular cavity dilation during intravenous dipyridamole technetium-99m sestamibi myocardial tomographic imaging in predicting coronary events. Am J Cardiol 1997;79:600-5.
Lette J, Bertrand C, Gossard D, Ruscito O, Cerino M, McNamara D, et al. Long-term risk stratification with dipyridamole imaging. Am Heart J 1995;129:880-6.
Veilleux M, Lette J, Mansur A, et al. Prognostic implications of transient left ventricular cavitary dilation during exercise and dipyridamole-thallium imaging. Can J Cardiol 1994;10:259-62.
Abidov A, Bax JJ, Hayes SW, Hachamovitch R, Cohen I, Gerlach J, Kang X, et al. Transient ischemic dilation ratio of the left ventricle is a significant predictor of future cardiac events in patients with otherwise normal myocardial perfusion SPECT. J Am Coll Cardiol 2003;42:1818-25.
Abidov A, Germano G, Berman DS. Transient ischemic dilation ratio: A universal high-risk diagnostic marker in myocardial perfusion imaging. J Nucl Cardiol 2007;14:497-500.
Berman DS, Hachamovitch R, Kiat H, Cohen I, Cabico JA, Wang FP, et al. Incremental value of prognostic testing in patients with known or suspected heart disease: A basis for optimal utilization of exercise technetium-99 m sestamibi myocardial perfusion single-photon emission computed tomography. J Am Coll Cardiol 1995;26:639-47.
Germano G, Kiat H, Kavanagh PB, Moriel M, Mazzanti M, Su H, et al. Automatic quantification of ejection fraction from gated myocardial perfusion SPECT. J Nucl Med 1995;36:2138-47.
Henzlova MJ, Cerqueira MD, Hansen CL, Taillefer R, Yao SS. Stress protocols and tracers. J Nucl Cardiol 2009. doi:10.1007/s12350-009-9062-4 (http://www.asnc.org/imageuploads/ImagingGuidelinesStressProtocols021109.pdf, accessed 8/17/2010).
Holly TA, Abbott BG, Al-Mallah M, Calnon DA, Cohen MC, DiFilippo FP, Ficaro EP, Freeman MR, Hendel RC, Jain D, Leonard SM, Nichols KJ, Polk DM, Soman P. Single photon-emission computed tomography. J Nucl Cardiol 2010; published on line June 15, 2010. doi:10.1007/s12350-010-9246-y. (http://www.asnc.org/imageuploads/ImagingGuidelineSPECTJune2010.pdf, accessed 8/17/10).
Berman DS, Shaw LJ, Hachamovitch R, Friedman JD, Polk DM, Hayes SW, et al. Comparative use of radionuclide stress testing, coronary artery calcium scanning, and noninvasive coronary angiography for diagnostic and prognostic cardiac assessment. Semin Nucl Med 2007;37:2-16.
Mark DB, Nelson CL, Califf RM, Harrell FE Jr, Lee KL, Jones RH, et al. Continuing evolution of therapy for coronary artery disease. Initial results from the era of coronary angioplasty. Circulation 1994;89:2015-25.
Yoon AJ, Melduni RM, Duncan SA, Ostfeld RJ, Travin MI. The effect of beta-blockers on the diagnostic accuracy of vasodilator pharmacologic SPECT myocardial perfusion imaging. J Nucl Cardiol 2009;16:358-67.
http://www.emerginghealthit.com/body.cfm?id=23. Last access date: August 17, 2010.
http://www.montefiore.org/guide/lookingglass/. Last access date: August 17, 2010.
Diamond GA, Forrester JS. Analysis of probability as an aid in the clinical diagnosis of coronary-artery disease. N Engl J Med. 1979;300:1350-8.
Baddi A, Bhatt M, Leonard SM, Hendel RC. Significance of transient ischemic left ventricular dilation in the absence of SPECT perfusion defects. Circulation 2002;106:II-618 (abstract).
Hakeem A, Bhatti S, Cook JR, Chang SM. Isolated transient ischemic dilation and the risk of adverse cardiac events in a cohort of high risk individuals undergoing myocardial perfusion SPECT imaging. J Am Coll Cardiol 2010; 55:A90.E854 (abstract).
Stolzenberg J. Dilatation of left ventricular cavity on stress thallium scan as an indicator of ischemic disease. Clin Nucl Med 1980;5:289-91.
McLaughlin MG, Danias PG. Transient ischemic dilation: A powerful diagnostic and prognostic finding of stress myocardial perfusion imaging. J Nucl Cardiol 2002;9:663-7.
Sugihara H, Shiga K, Umamoto I, Harada Y, Katahira T, Nakagawa T, et al. Assessment of transient dilation of the left ventricular cavity in patients with hypertrophic cardiomyopathy by exercise thallium-0201 scintigraphy [in Japanese]. Kaku Igaku 1990;27:1281-9.
Robinson VJ, Corley JH, Marks DS, Eberhardt LW, Eubig C, Burke GJ, et al. Causes of transient dilatation of the left ventricle during myocardial perfusion imaging. Am J Roentgenol 2000;174:1349-52.
Smelley MP, Virnich DE, Williams KA, Ward RP. A hypertensive response to exercise is associated with transient ischemic dilation on myocardial perfusion SPECT imaging. J Nucl Cardiol 2007;14:537-43.
Lin DA, Harb TS, Yoder SR, Mackin ML, Schwartz RG. Transient ischemic dilation without angiographically detectable coronary artery disease is associated with left ventricular hypertrophy and low mortality. J Nucl Cardiol 2003;10:S46 (abstract).
Emmett L, Magee M, Freedman SB, Van der Wall H, Bush V, Trieu J, et al. The role of left ventricular hypertrophy and diabetes in the presence of transient ischemic dilation of the left ventricle on myocardial perfusion SPECT images. J Nucl Med 2005;46:1596-601.
Hansen CL, Sangrigoli R, Nkadi E, Kramer M. Comparison of pulmonary uptake with transient cavity dilation after exercise thallium-201 perfusion imaging. J Am Coll Cardiol 1999;33:1323-7.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Valdiviezo, C., Motivala, A.A., Hachamovitch, R. et al. The significance of transient ischemic dilation in the setting of otherwise normal SPECT radionuclide myocardial perfusion images. J. Nucl. Cardiol. 18, 220–229 (2011). https://doi.org/10.1007/s12350-011-9343-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12350-011-9343-6