Abstract
The clinical spectrum of spinocerebellar ataxia type 2 includes motor manifestations and cognitive disturbances in executive functions, memory, and visuoconstructive skills. The relationships between severity of motor disturbances and altered cognition are poorly known. In this study, we assessed patients with spinocerebellar ataxia type 2 and age- and sex-matched healthy control subjects by a test battery including the Mini-mental State Examination, the Wisconsin Card Sorting test, and the Wechsler Memory Scale-Revised. The correlation between severity of motor ataxia (as assessed by a validated and widely used severity scale, the SARA scale, and by an objective automated computerized system of gait analysis) and altered cognition was then evaluated by Spearman correlation analysis. Patients performed worse than healthy controls in almost all administered neuropsychological tests. Nevertheless, only global intellectual abilities and executive functions significantly correlated with the overall severity of ataxia as assessed by the SARA scale, and impaired executive functions alone correlated with performance on several spatio-temporal gait analysis parameters. Our findings would probably suggest a prominent influence of executive functions on motor abilities in patients with spinocerebellar ataxia type 2 and raise the possibility that cognitive pharmaceutical or rehabilitative interventions may be of benefit in the management of motor problems in these patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Spinocerebellar ataxia type 2 (SCA2) is one of the most common forms of SCAs worldwide and the most frequent subtype in southern Italy [1]. This dominantly inherited degenerative disorder is due to an expanded CAG trinucleotide repeat in the ATXN2 gene coding for the protein ataxin [2]. Ataxic gait, impaired balance and speech, dysmetria, and slow eye movements [3,4,5,6] are typical motor manifestations of SCA2; the clinical spectrum of SCA2 may also include an altered cognitive profile characterized by disturbances in fronto-executive functions, memory, and visuoconstructive skills [7,8,9,10,11,12,13,14]. Although the patho-anatomical basis of neuropsychological impairment in SCA2 remains to be fully elucidated, recent anatomical and functional magnetic resonance imaging studies have revealed abnormalities in the cerebellar network as well as in non-cerebellar regions, such as orbitofrontal cortex, the middle frontal region, the primary sensorimotor cortex, and temporomesial and insular cortices that are known to be functionally connected to the cerebellum [15,16,17,18,19,20,21,22]. Cognitive profile of SCA2 patients meets the features of the cerebellar cognitive affective syndrome (CCAS) or Schmahmann’s syndrome that characterize the disturbances of higher function in patients with cerebellar injury across different disease types and ages [23].
Over the last two decades, an accumulating body of evidence showed that motor processes should no longer be considered as mere automated activities but as complex tasks also requiring cognitive abilities [24]. It is therefore likely that certain cognitive functions contribute to motor control [24, 25]. Nevertheless, studies addressing the relationships between severity of motor disturbances and cognition in SCA2 provided inconsistent results [11, 13, 14, 26,27,28,29,30].
The present study was designed to explore the relationships between the severity of motor ataxia (as assessed by a validated and widely used clinical severity scale and by an objective automated computerized system of gait analysis) and the burden of cognitive impairment in global intellectual abilities, general executive functions, and short- and long-term verbal and visuospatial memory in SCA2 patients.
Materials and Methods
Study Subjects
Case patients were recruited among outpatients with genetically confirmed SCA2 who attended the outpatient movement disorders clinic of the Neurology Unit “Amaducci,” “Aldo Moro” University of Bari, Italy, from September 2016 to July 2017. Patients who were able to walk without support were included in the study whereas patients who could not walk without support because of ataxia or patients who complained of neuro-otological, orthopaedic, or visual disorders, or were under drugs possibly affecting ataxic manifestations were excluded. Sex- and age- (± 5 years) matched healthy control subjects were recruited among relatives of non-ataxic outpatients. All participants provided a written informed consent and study procedures were approved by the local ethics committee (“Aldo Moro” University of Bari, Italy).
Study Procedures
Case and control individuals were asked to participate in a study on cognition and movement approved by the ethics committee. A trained interviewer, not blinded to the case/control status but unaware of the study hypotheses, collected relevant demographic and clinical information. Severity of ataxia was rated by the validated clinical “scale for the assessment and rating of ataxia” (SARA) that measures eight domains (stance, gait, sitting, speech, finger chase, nose–finger, fast alternating hand movements, heel-shin slide) and provides a total score (SARA-TOT) ranging from 0 to 40, with 0 indicating absence of ataxia and 40 the most severe degree of ataxia [31]. We also tested the SARA-gait subscore for possible correlations.
A neuropsychological test battery was administered by an experienced neuropsychologist (who was blinded to the results of motor assessments) to both case and control subjects one to four days after motor assessment. The test battery included the Mini-mental State Examination (MMSE), the Wisconsin Card Sorting Test (WCST), and the Wechsler Memory Scale-Revised (WMS). MMSE provided a global assessment of cognitive functions [32]. The WCST [33] is a well-established measure of general executive function evaluating several “frontal” lobe properties, including strategic planning, organized searching, utilizing environmental feedback to shift cognitive sets, directing behaviour toward achieving a goal, and modulating impulsive responding. The test uses stimulus and response cards (64-card scoring version) characterized by various forms, colors, and numbers [33]. The participant is told to match the cards, but not how to match them; however, the subject is told whether a particular match is right or wrong. As the test progresses, there are unannounced shifts in the sorting principle which require the subject to alter her/his approach. Performance is recorded as number of correct categories (W-CA), total number of corrected responses (W-CORRECT), and number of perseverative errors (W-PERRORS). The WMS measures different memory functions by several subtests, including information on general knowledge, orientation in time and place, mental control (testing the ability to repeat sequences such as the alphabet), logical memory (immediate repetition of short stories presented orally), digits forwards and digits reversed (the conventional digit span tests), visual reproduction (drawing reproduction of three simple designs, each presented individually for 10 s), and associate learning (the patient is given three trials to learn 10 pairs of words, with six pairs having a logical match and four pairs having no logical connection). The Beck depression Inventory (BDI) was used to assess depressive symptoms [34].
Spatio-temporal parameters of gait were assessed in SCA2 patients by a motion capture system (SMART-E, BTS Bioengineering, Milan, Italy) equipped with a set of 8 infrared cameras [35]. After acquisition of data on height, weight, anterior superior iliac spine (ASIS) distance, pelvis thickness, knee and ankle width, and leg length (distance between ASIS and medial malleolus), 22 retro-reflective spherical markers for the lower-body segments were placed on anatomical landmarks in accordance with Davis model [36]. Kinetic data were collected using 2 piezoelectric force platforms (Kistler Instruments, Winterthur, Switzerland; 400 × 64 cm) embedded in a walkway. Patients were asked to walk over the walkway at their comfortable, preferred speed; each trial started 2 m in front of the mat and continued for 2 m beyond it in order to consider only stationary conditions (i.e., constant speed) discarding acceleration and deceleration phases. After a familiarization phase, each participant performed at least six walking trials. The raw kinematic data were then processed to calculate the following spatio-temporal parameters: gait speed, step length, step width, cadence, stance, and double support phase duration (expressed as percentage of the gait cycle). As intra-subject variability of gait parameters has been reported as a relevant feature of ataxic gait, we also calculated for each parameter the coefficient of variation (CV) using the formula: CV = standard deviation × 100/mean.
Statistical Analysis
Statistical analysis was performed by Stata 11.0 package (Stata Corporation, College Station, TX, USA). Data were expressed as mean and standard deviation (SD) unless otherwise indicated. Differences between study groups were assessed by the chi-square test and the Student’s two-tailed t tests, as appropriate. p values from multiple case-control comparisons were adjusted by the Bonferroni correction. Correlations between study variables were checked by Spearman’s rank correlation analysis. Sex was categorized as 0 for men and 1 for women. Statistical significance was set at the 0.05 level.
Results
Demographics and Clinical Features of SCA2 Patients and Controls
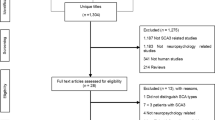
Twenty-two right-handed SCA2 patients were seen during the study period. Two subjects were however excluded from the study, one because of severe visual impairment due to diabetes mellitus, the other one because of severe spinal disc herniation-related pain. The remaining 20 patients who met eligibility criteria were 11 women and 9 men from 11 families. The SCA2 group and the healthy control group were matched for sex and did not significantly differ for age (53.4 ± 13.3 vs. 49.6 ± 2.7 years, p = 0.11) and years of schooling (9.5 ± 3.4 vs. 10.7 ± 4.4, p = 0.2).
SCA2 patients carried a heterozygous CAG triplet expansion with 37.6 ± 2.9 repeats (range, 35 to 47) in the coding ATXN2 region. The normal alleles contained 22 repeats in all case patients. Mean age at disease onset was 39.7 years (SD, 13.6; range, 10–62) and mean disease duration was 13.8 years (SD, 10.6; range, 1–37). There was a negative correlation between number of repeats in the expanded allele and age at disease onset (Spearman rho = − 0.56, p = 0.01). No patient was under riluzole therapy.
SARA-TOT score was 10.4 ± 4.5 (range, 2.5 to 17.5). There was no significant correlation between SARA-TOT score and age (Spearman rho = − 0.15, p = 0.5) or gender (Spearman rho = 0.08, p = 0.7), whereas non-significant trends were observed for a correlation between SARA-TOT score and age at disease onset (Spearman rho, − 0.43, p = 0.06), disease duration (Spearman rho = 0.31, p = 0.07), and number of triplets (Spearman rho, 0.43, p = 0.06). No significant correlation was found between SARA-TOT score and years of schooling (Spearman rho, − 0.12, p = 0.62).
Neuropsychological Testing
Neuropsychological assessment showed that SCA2 patients significantly differed from healthy controls for MMSE, W-PERRORS, and total WMS score (Table 1). BDI was comparable in case and control subjects (Table 1). All subitems from WMS except WMS-orientation and WMS-digits forwards were significantly lower in case patients (p values ranging between < 0.04 and < 0.0001 after Bonferroni correction orientation). No SCA2 patient could be diagnosed with dementia according to DSM-V criteria, even though 35% of them scored ≤ 23 on MMSE. Of note, WCST and WMS were impaired in both patients who scored < 23 on MMSE and patients yielding MMSE score in the non-demented range (data not shown).
In the SCA2 group, there was no significant correlation between demographic variables (age, sex, years of schooling, age at disease onset, disease duration, and number of triplets) and most cognitive tests (data not shown): the only significant correlation was observed between number of triplets and W-CORRECT score (rho = − 0.55, p = 0.01); moreover, male gender was associated with higher BDI score (rho = − 0.46, p = 0.04).
Spearman analysis revealed significant correlations between the overall severity of ataxia as assessed by the SARA scale and performance on MMSE and WCST (Table 2). These findings were confirmed even when analysis was restricted to the gait parameter from SARA (SARA-gait vs. MMSE: rho = − 0.61, p = 0.004; SARA-gait vs. W-CORRECT score: rho = − 0.68, p = 0.004). By contrast, no significant correlation emerged between SARA-TOT score and performance on BDI, WMS total score (Table 2) or any subtest of the WMS (data not shown).
Gait Analysis
The results of gait analysis in the 20 SCA2 patients are in Table 3. Higher SARA-TOT and SARA-gait scores significantly correlated to worse performances on gait analysis (Table 4). Analyzing the relationships between demographic variables (age, number of repeats, age of disease onset, disease duration, and schooling) and gait analysis parameters on Spearman correlation, the only significant correlations were found between disease duration and stance phase duration (rho = 0.61, p = 0.01), double support (rho = 0.51, p = 0.04), step length (rho = − 0.57, p = 0.02), and gait speed (rho = − 0.69, p = 0.003).
Significant correlations also emerged between cognitive performance on the WCST and stance phase, double support subphase, step width, gait speed, or step length (Table 5). No significant correlation was observed between gait parameters and MMSE, BDI, WMS (Table 5), or any subtest of the WMS (data not shown). Finally, there was no significant correlation between CV of the examined gait parameters and any neuropsychological test (data not shown).
Discussion
Our psychometric evaluation showed that SCA2 patients performed worse than age- and sex-matched healthy controls of comparable level of schooling on a neuropsychological test battery assessing global intellectual abilities, general executive functions, and short- and long-term verbal and visuospatial memory. Overall, these findings confirmed previous observations in SCA2 patients [7, 10,11,12,13,14, 17, 19, 27, 29]. The 35% frequency of SCA2 patients scoring ≤ 23 on MMSE was comparable to the frequency of altered general cognitive status reported in SCA2 patients [7,8,9,10,11,12,13,14]. None of our patients could be diagnosed with dementia according with DSM-V criteria, which was consistent with the low rate of dementia characterizing most SCA2 pedigrees [7,8,9,10,11,12,13,14, 22, 27, 29].
Although SCA2 patients showed a poorer performance in almost all administered tests, only global intellectual abilities and executive functions significantly correlated with the overall severity of ataxia as assessed by the SARA scale; and impaired executive functions alone correlated with performance on several spatio-temporal gait analysis parameters. These findings would probably suggest a prominent influence of executive functions on motor abilities in SCA2 patients. Supporting the specificity of the findings, there was no correlation between cognitive performance and age, gender, disease duration, years of schooling, or repeat length.
Several studies dealt with the relationships between motor abilities and cognition in patients with heredodegenerative ataxia [11, 13, 14, 26,27,28,29,30] but results were inconsistent. In 18 SCA2 patients, La Pira et al. reported a significant correlation between ataxia severity and a few items of the California Verbal Learning Test, a neuropsychological tool that measures verbal memory and learning strategies [13]. By contrast, Burk et al. [11] did not find any significant relationships between motor performance (evaluated using a severity scale for limb ataxia and dysarthria only) and cognitive impairment in 17 SCA2 patients by MMSE, WCST, and WMS. Using different clinical and electrophysiological approaches, significant inverse relationships emerged between severity of motor disturbances and performance in cognitive domains in large series of SCA2 patients [27,28,29,30]. In particular, higher SARA score was associated with greater impairment in phonemic verbal fluency [27], error-based visuomotor learning [28], attention [29, 30], visual memory, spatial planning and motor control [29], and working memory [30]. Two further studies assessing genetically heterogeneous samples of SCA patients found significant correlations between severity of ataxia, measured by the SARA scale [26] and the ataxia clinical rating scale [14], and cognitive performances assessed by MMSE, WCST, and WMS [26] in one study, by MMSE, Raven PM, phonemic fluency, semantic fluency, and attentional matrices in the other study [14]. However, both studies did not provide separate data on SCA2 subgroup, probably because of the small sample size and the low statistical power. Finally, in the study for the development of the cerebellar cognitive affective/Schmahmann syndrome scale [23], Hoche et al. did not find any strong correlation between the Brief Ataxia Rating Scale and cognitive performance in various domains in both exploratory and validation cohorts, each consisting of various forms of acquired or inherited conditions. The heterogeneity of cerebellar diseases and the very small number of SCA2 patients included in the study (there were 5 SCA2 patients in the exploratory cohort, only one SCA2 patient in the validation cohort) may explain the discrepancy between our and Hoche study.
At variance with previous studies that used a variety of tools to assess motor activity and cognition [11, 13, 14, 26], in the present work, we used widely validated and suitable clinical tools to ascertain both motor and cognitive abilities in a homogeneous group of SCA2 patients [22, 31]. This makes the results of our study probably valid and accurate. The use of an objective system to measure ataxic gait also distinguished the present study from previous works [11, 13, 14, 23, 26,27,28,29,30] and corroborated the validity of our findings. Further supporting the validity of our methods, we observed an obvious correlation between SARA scores and gait analysis parameters.
The pathophysiological basis underlying the relationships between ataxia and executive dysfunction in SCA2 patients remains to be fully elucidated. As revealed by neuropathological and voxel-based morphometry studies, patients affected by SCA2 show a pattern of both olivo-ponto-cerebellar and supratentorial damage [15,16,17,18,19,20,21]; moreover, functional magnetic resonance imaging studies in SCA2 have shown a connection between posterior regions in the cerebellum and regions in the cerebral cortex related to cognition [16, 21]. Although it is now well accepted that cerebellum plays a role in both motor and cognitive tasks, including executive functions [15, 22, 37,38,39,40], it remains unclear whether the association between ataxia and executive dysfunction reflects a prominent cerebellar involvement or a concomitant neural degeneration in extra-cerebellar structures leading to a disconnection in the fronto-ponto-cerebello-thalamo-cortical circuits [2, 9, 10, 37, 41]. The cerebellar cognitive affective/Schmahmann syndrome has also been described in patients with isolated cerebellar pathology [23, 37]. However, it could not rule out the possibility that the pathological alterations in non-cerebellar structures may play a determinant role in the positive association between ataxia and cognitive disturbances emerged in patients with complex cerebrocerebellar pathologies [13, 22, 23, 27,28,29,30]. In keeping with this view, in patients with SCA2, cognitive disfunctions has been found to correlate with both cerebellar [19, 20] and cerebral [17] structural damage using the voxel-based morphometry and diffusion tensor imaging. Various degrees of cognitive impairment have been described in different dominantly inherited ataxias with isolated cerebellar or complex cerebrocerebellar pathology [22, 42,43,44,45,46], but only few studies evaluated the relationship between motor abilities and cognitive state, showing either the presence [42, 43] or the absence [44,45,46] of a correlation. The inconsistency in neuropsychological tests selection and other potential confounding factors including the use of tests unsuitable to explore specific cognitive domains in patients with ataxias due to their visual, speech, and motor disturbances may explain discrepancies across studies [22].
Regardless of the diffusion of neural damage to extra-cerebellar structures, the loss of the cerebellar contribution to the cerebrocerebellar circuitry has been argued to serve as the basis for the cognitive impairments in patients with cerebellar pathology, a concept embedded within the dysmetria of thought theory [37]. Studies based on pathological examination as well as longitudinal and functional neuroimaging studies could better investigate whether the correlation between motor functions and cognition emerged in different ataxic disorders relies on the cerebellar damage alone or on the diffusion of the neurodegeneration process to extra-cerebellar structures.
It has been postulated that executive functions may play an important role in the assessment, planning, response to a given situation, and choice of the gait pattern [47, 48] and there is emerging evidence indicating that cognitive interventions may improve motor activity in several conditions [49]. Different studies were designed to investigate the effect on motor abilities of either cognitive-enhancing medications or cognitive training interventions [49]. Though providing preliminary findings with different methodologic limitations, most of these studies showed that improvement in executive functions could result in good outcomes in gait, balance, risk of falls, and dual-task performances in series of patients with Parkinson’s disease [50,51,52], mild-to-moderate dementia [53, 54], and in healthy older adults [55,56,57,58]. Although studies on this issue are lacking in heredodegenerative ataxia, the relationship between ataxia and executive functions we found may support the idea that cognitive pharmaceutical and rehabilitative interventions can be of benefit in the management of motor problems in SCA2 patients.
Our study has strengths and limitations. First, this was not a population-based study, but recruiting criteria yielded a case series resembling the general population of cases in both demographic and clinical features. The significant correlations we found between the number of CAG repeats and age at disease onset and between SARA scores and disease duration were in agreement with data from previous SCA2 series, [11, 13, 30, 59] thus supporting the representativeness of our sample. Second, technical difficulties linked to motor impairment due to ataxia might have contributed to the poorer cognitive performance showed by SCA2 patients, at least in some cases. However, we took care to exclude tests that could have been influenced by manual and speech abilities. In particular, the WCST avoids the pitfalls of performance speed pressure and do not place a premium on motor or visual speed and accuracy. Influence of depression mood on the differences in cognition between groups was also unlikely because of the comparable BDI scores showed by patients and healthy subjects. Using a clinical tool to assess motor severity might have provided inconsistent results. However, the results obtained using a validated and widely used clinical scale (the SARA scale) were corroborated by the findings from an objective computer-assisted system measuring gait performance. Third, in our gait analysis, we did not use a control group, but we referred to the normative data provided by the motion capture system manufacturer (BTS Bioengineering, Milan, Italy); supporting the validity of our observation, our findings are comparable with pathological values of ataxic patients from a study that used the same gait analysis system and also provided a control group. [60]. Finally, our case and control groups are relatively small and we cannot exclude the possibility that non-significant results reflect, at least in part, lack of statistical power. Further studies investigating the relationship between motor control and cognition in larger series of cases and healthy subjects are therefore necessary.
Despite the foregoing limitations, our analysis confirmed the poor performance of SCA2 patients in several cognitive domains and provided new information suggesting a specific correlation between ataxia and executive dysfunction. Information from this study may help to clarify the relationships between motor and cognitive performance in SCA2 patients and also to identify new targets for rehabilitative and pharmacological intervention.
References
Brusco A, Gellera C, Cagnoli C, Saluto A, Castucci A, Michielotto C, et al. Molecular genetics of hereditary spinocerebellar ataxia: mutation analysis of spinocerebellar ataxia genes and CAG/CTG repeat expansion detection in 225 Italian families. Arch Neurol. 2004;61(5):727–33.
Lastres-Becker I, Rüb U, Auburger G. Spinocerebellar ataxia 2 (SCA2). Cerebellum. 2008;7(2):115–24. https://doi.org/10.1007/s12311-008-0019-y Review.
Durr A. Autosomal dominant cerebellar ataxias: polyglutamine expansions and beyond. Lancet Neurol. 2010;9(9):885–94. https://doi.org/10.1016/S1474-4422(10)70183-6.
Velázquez-Pérez L, Rodríguez-Labrada R, García-Rodríguez JC, Almaguer-Mederos LE, Cruz-Mariño T, Laffita-Mesa JM. A comprehensive review of spinocerebellar ataxia type 2 in Cuba. Cerebellum. 2011;10(2):184–98. https://doi.org/10.1007/s12311-011-0265-2.
Auburger GWJ. Spinocerebellar ataxia type 2. Handb Clin Neurol. 2012;103:423–36.
Manto M-U. The wide spectrum of spinocerebellar ataxias (SCAs). Cerebellum. 2005;4:2–6.
Bürk K, Stevanin G, Didierjean O, Cancel G, Trottier Y, Skalej M, et al. Clinical and genetic analysis of three German kindreds with autosomal dominant cerebellar ataxia type I linked to the SCA2 locus. J Neurol. 1997;244(4):256–61.
Cancel G, Dürr A, Didierjean O, Imbert G, Bürk K, Lezin A, et al. Molecular and clinical correlations in spinocerebellar ataxia 2: a study of 32 families. Hum Mol Genet. 1997;6(5):709–15.
Dürr A, Smadja D, Cancel G, Lezin A, Stevanin G, Mikol J, et al. Autosomal dominant cerebellar ataxia type I in Martinique (French West Indies). Clinical and neuropathological analysis of 53 patients from three unrelated SCA2 families. Brain. 1995;118(Pt 6):1573–81.
Storey E, Forrest SM, Shaw JH, Mitchell P, Gardner RJ. Spinocerebellar ataxia type 2: clinical features of a pedigree displaying prominent frontal-executive dysfunction. Arch Neurol. 1999;56(1):43–50.
Bürk K, Globas C, Bösch S, Gräber S, Abele M, Brice A, et al. Cognitive deficits in spinocerebellar ataxia 2. Brain. 1999;122(Pt 4):769–77.
Gambardella A, Annesi G, Bono F, Spadafora P, Valentino P, Pasqua AA, et al. CAG repeat length and clinical features in three Italian families with spinocerebellar ataxia type 2 (SCA2): early impairment of Wisconsin Card Sorting Test and saccade velocity. J Neurol. 1998;245(10):647–52.
Le Pira F, Zappalà G, Saponara R, Domina E, Restivo D, Reggio E, et al. Cognitive findings in spinocerebellar ataxia type 2: relationship to genetic and clinical variables. J Neurol Sci. 2002;201:53–7.
Fancellu R, Paridi D, Tomasello C, Panzeri M, Castaldo A, Genitrini S, et al. Longitudinal study of cognitive and psychiatric functions in spinocerebellar ataxia types 1 and 2. J Neurol. 2013;260(12):3134–43.
Buckner RL. The cerebellum and cognitive function: 25 years of insight from anatomy and neuroimaging. Neuron. 2013;80(3):807–15. https://doi.org/10.1016/j.neuron.2013.10.044 Review.
Hernandez-Castillo CR, Galvez V, Mercadillo RE, Díaz R, Yescas P, Martinez L, et al. Functional connectivity changes related to cognitive and motor performance in spinocerebellar ataxia type 2. Mov Disord. 2015;30(10):1391–9. https://doi.org/10.1002/mds.26320 Epub 2015 Aug 8.
Hernandez-Castillo CR, Vaca-Palomares I, Galvez V, Campos-Romo A, Diaz R, Fernandez-Ruiz J. Cognitive deficits correlate with white matter deterioration in spinocerebellar ataxia type 2. J Int Neuropsychol Soc. 2016;22(4):486–91. https://doi.org/10.1017/S1355617716000084 Epub 2016 Feb 18.
Mercadillo RE, Galvez V, Díaz R, Hernández-Castillo CR, Campos-Romo A, Boll MC, et al. Parahippocampal gray matter alterations in spinocerebellar ataxia type 2 identified by voxel based morphometry. J Neurol Sci. 2014;347(1-2):50–8. https://doi.org/10.1016/j.jns.2014.09.018 Epub 2014 Sep 19.
Olivito G, Lupo M, Iacobacci C, Clausi S, Romano S, Masciullo M, et al. Structural cerebellar correlates of cognitive functions in spinocerebellar ataxia type 2. J Neurol. 2018;265(3):597–606. https://doi.org/10.1007/s00415-018-8738-6 Epub 2018 Jan 22.
Olivito G, Lupo M, Iacobacci C, Clausi S, Romano S, Masciullo M, et al. Microstructural MRI basis of the cognitive functions in patients with spinocerebellar ataxia type 2. Neuroscience. 2017;366:44–53. https://doi.org/10.1016/j.neuroscience.2017.10.007 Epub 2017 Oct 12.
Olivito G, Cercignani M, Lupo M, Iacobacci C, Clausi S, Romano S, et al. Neural substrates of motor and cognitive dysfunctions in SCA2 patients: a network based statistics analysis. Neuroimage Clin. 2017;14:719–25. https://doi.org/10.1016/j.nicl.2017.03.009 eCollection 2017.
Lindsay E, Storey E. Cognitive changes in the spinocerebellar ataxias due to expanded polyglutamine tracts: a survey of the literature. Brain Sci. 2017;14:7(7).
Hoche F, Guell X, Vangel MG, Sherman JC, Schmahmann JD. The cerebellar cognitive affective/Schmahmann syndrome scale. Brain. 2018;141(1):248–70. https://doi.org/10.1093/brain/awx317.
Amboni M, Barone P, Hausdorff JM. Cognitive contributions to gait and falls: evidence and implications. Mov Disord. 2013;28(11):1520–33. https://doi.org/10.1002/mds.25674 Review.
Morris R, Lord S, Bunce J, Burn D, Rochester L. Gait and cognition: mapping the global and discrete relationships in ageing and neurodegenerative disease. Neurosci Biobehav Rev. 2016;64:326–45. https://doi.org/10.1016/j.neubiorev.2016.02.012 Epub 2016 Feb 23.
Kish SJ, el-Awar M, Stuss D, Nobrega J, Currier R, Aita JF, et al. Neuropsychological test performance in patients with dominantly inherited spinocerebellar ataxia: relationship to ataxia severity. Neurology. 1994;44(9):1738–46.
Rodríguez-Labrada R, Velázquez-Pérez L, Aguilera-Rodríguez R, Seifried-Oberschmidt C, Peña-Acosta A, Canales-Ochoa N, et al. Executive deficit in spinocerebellar ataxia type 2 is related to expanded CAG repeats: evidence from antisaccadic eye movements. Brain Cogn. 2014;91:28–34. https://doi.org/10.1016/j.bandc.2014.07.007 Epub 2014 Sep 3.
Vaca-Palomares I, Díaz R, Rodríguez-Labrada R, Medrano-Montero J, Vázquez-Mojena Y, Velázquez-Pérez L, et al. Spinocerebellar ataxia type 2 neurodegeneration differentially affects error-based and strategic-based visuomotor learning. Cerebellum. 2013;12(6):848–55. https://doi.org/10.1007/s12311-013-0496-5.
Vaca-Palomares I, Díaz R, Rodríguez-Labrada R, Medrano-Montero J, Aguilera-Rodríguez R, Vázquez-Mojena Y, et al. Strategy use, planning, and rule acquisition deficits in spinocerebellar ataxia type 2 patients. J Int Neuropsychol Soc. 2015;21(3):214–20. https://doi.org/10.1017/S1355617715000132 Epub 2015 Mar 23.
Rodríguez-Labrada R, Velázquez-Pérez L, Ortega-Sánchez R, Peña-Acosta A, Vázquez-Mojena Y, Canales-Ochoa N, et al. Insights into cognitive decline in spinocerebellar ataxia type 2: a P300 event-related brain potential study. Cerebellum Ataxias. 2019;6:3. https://doi.org/10.1186/s40673-019-0097-2 eCollection 2019.
Schmitz-Hübsch T, du Montcel ST, Baliko L, Berciano J, Boesch S, Depondt C, et al. Scale for the assessment and rating of ataxia: development of a new clinical scale. Neurology. 2006;66:1717–20.
Folstein MF, Folstein SE, McHugh PR (1975) “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12:189–198
Heaton RK, Chelune GJ, Talley JL, Kay GG, Curtiss G. Wisconsin card sorting test (WCST) CV-64. Psychological Assessment Resources: Odessa Fla; 1993.
Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561–71.
Ferrigno G, Pedotti A. ELITE: a digital dedicated hardware system for movement analysis via real-time TV signal processing. IEEE Trans Biomed Eng. 1985;32:943–50.
Davis RB, Ounpuu S, Tyburski D, Gage JR. A gait analysis data collection and reduction technique. Hum Mov Sci. 1991;10:575–87.
Schmahmann JD. The role of the cerebellum in cognition and emotion: personal reflections since 1982 on the dysmetria of thought hypothesis, and its historical evolution from theory to therapy. Neuropsychol Rev. 2010;20(3):236–60. https://doi.org/10.1007/s11065-010-9142-x. Epub 2010 Sep 7 Review.
Stoodley CJ, Schmahmann JD. Evidence for topographic organization in the cerebellum of motor control versus cognitive and affective processing. Cortex. 2010;46(7):831–44. https://doi.org/10.1016/j.cortex.2009.11.008 Epub 2010 Jan 11.
Ilg W, Timmann D. Gait ataxia--specific cerebellar influences and their rehabilitation. Mov Disord. 2013;28(11):1566–75. https://doi.org/10.1002/mds.25558.
Bodranghien F, Bastian A, Casali C, Hallett M, Louis ED, Manto M, et al. Consensus paper: revisiting the symptoms and signs of cerebellar syndrome. Cerebellum. 2016;15(3):369–91. https://doi.org/10.1007/s12311-015-0687-3 Review.
Estrada R, Galarraga J, Orozco G, Nodarse A, Auburger G. Spinocerebellar ataxia 2 (SCA2): morphometric analyses in 11 autopsies. Acta Neuropathol. 1999;97:306–10.
Feng L, Chen DB, Hou L, Huang LH, Lu SY, Liang XL. etal. Cognitive impairment in native Chinese with spinocerebellar ataxia type 3. Eur Neurol. 2014;71(5-6):262–70. https://doi.org/10.1159/000357404 Epub 2014 Feb 12.
Cooper FE, Grube M, Elsegood KJ, Welch JL, Kelly TP, Chinnery PF, et al. The contribution of the cerebellum to cognition in spinocerebellar ataxia type 6. Behav Neurol. 2010;23(1-2):3–15. https://doi.org/10.3233/BEN-2010-0265.
Roeske S, Filla I, Heim S, Amunts K, Helmstaedter C, Wüllner U, et al. Progressive cognitive dysfunction in spinocerebellar ataxia type 3. Mov Disord. 2013;28(10):1435–8. https://doi.org/10.1002/mds.25512 Epub 2013 Jun 4.
Chirino A, Hernandez-Castillo CR, Galvez V, Contreras A, Diaz R, Beltran-Parrazal L, et al. Motor and cognitive impairments in spinocerebellar ataxia type 7 and its correlations with cortical volumes. Eur J Neurosci. 2018;48(10):3199–211. https://doi.org/10.1111/ejn.14148 Epub 2018 Sep 26.
Moro A, Teive HAG. Cognitive impairment in spinocerebellar ataxia type 10. Dement Neuropsychol. 2016;10(4):310–4. https://doi.org/10.1590/s1980-5764-2016dn1004009.
van Iersel MB, Kessels RP, Bloem BR, Verbeek AL, Olde Rikkert MG. Executive functions are associated with gait and balance in community-living elderly people. J Gerontol A Biol Sci Med Sci. 2008;63(12):1344–9.
Liu-Ambrose T, Ahamed Y, Graf P, Feldman F, Robinovitch SN. Older fallers with poor working memory overestimate their postural limits. Arch Phys Med Rehabil. 2008;89(7):1335–40. https://doi.org/10.1016/j.apmr.2007.11.052.
Segev-Jacubovski O, Herman T, Yogev-Seligmann G, Mirelman A, Giladi N, Hausdorff JM. The interplay between gait, falls and cognition: can cognitive therapy reduce fall risk? Expert Rev Neurother. 2011;11(7):1057–75. https://doi.org/10.1586/ern.11.69 Review.
Auriel E, Hausdorff JM, Herman T, Simon ES, Giladi N. Effects of methylphenidate on cognitive function and gait in patients with Parkinson’s disease: a pilot study. Clin Neuropharmacol. 2006;29:15–7 PubMed: 16518128.
Litvinenko IV, Odinak MM, Mogil’naya VI, Emelin AY. Efficacy and safety of galantamine (reminyl) for dementia in patients with Parkinson’s disease (an open controlled trial). Neurosci Behav Physiol. 2008;38:937–45 PubMed: 18975103.
Mirelman A, Maidan I, Herman T, Deutsch JE, Giladi N, Hausdorff JM. Virtual reality for gait training: can it induce motor learning to enhance complex walking and reduce fall risk in patients with Parkinson’s disease? J Gerontol A Biol Sci Med Sci. 2011;66:234–40 PubMed: 21106702.
Assal F, Allali G, Kressig RW, Herrmann FR, Beauchet O. Galantamine improves gait performance in patients with Alzheimer’s disease. J Am Geriatr Soc. 2008;56:946–7 PubMed: 18454755.
Schwenk M, Zieschang T, Oster P, Hauer K. Dual-task performances can be improved in patients with dementia: a randomized controlled trial. Neurology. 2010;74:1961–8. Largest study to date that examined the effects of dual-task training on gait. The results provide Class II evidence of its utility among patients with mild-to-moderate dementia PubMed: 20445152.
Ben-Itzhak R, Giladi N, Gruendlinger L, Hausdorff JM. Can methylphenidate reduce fall risk in community-living older adults? A double-blind, single-dose cross-over study. J Am Geriatr Soc. 2008;56:695–700. The positive effects of an attention-enhancing drug are documented in this study among older adults PubMed: 18266665.
Silsupadol P, Lugade V, Shumway-Cook A, et al. Training-related changes in dual-task walking performance of elderly persons with balance impairment: a double-blind, randomized controlled trial. Gait Posture. 2009;29:634–9 PubMed: 19201610.
Li KZ, Roudaia E, Lussier M, Bherer L, Leroux A, McKinley PA. Benefits of cognitive dual-task training on balance performance in healthy older adults. J Gerontol A Biol Sci Med Sci. 2010;65:1344–52 PubMed: 20837662.
Verghese J, Mahoney J, Ambrose AF, Wang C, Holtzer R. Effect of cognitive remediation on gait in sedentary seniors. J Gerontol A Biol Sci Med Sci. 2010;65:1338–43 PubMed: 20643703.
Geschwind DH, Perlman S, Figueroa CP, Treiman LJ, Pulst SM. The prevalence and wide clinical spectrum of the spinocerebellar ataxia type 2 trinucleotide repeat in patients with autosomal dominant cerebellar ataxia. Am J Hum Genet. 1997;60(4):842–50.
Serrao M, Pierelli F, Ranavolo A, Draicchio F, Conte C, Don R, et al. Gait pattern in inherited cerebellar ataxias. Cerebellum. 2012;11(1):194–211. https://doi.org/10.1007/s12311-011-0296-8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gigante, A.F., Lelli, G., Romano, R. et al. The Relationships Between Ataxia and Cognition in Spinocerebellar Ataxia Type 2. Cerebellum 19, 40–47 (2020). https://doi.org/10.1007/s12311-019-01079-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12311-019-01079-5