Abstract
In spinocerebellar ataxia type 6 (SCA6), the vestibular dysfunction and its correlation with other clinical parameters require further exploration. We determined vestibular responses over a broad range of stimulus acceleration in 11 patients with SCA6 (six men, age range=33–72 years, mean age±SD=59±12 years) using bithermal caloric irrigations, rotary chair, and head impulse tests. Correlations were also pursued among disability scores, as measured using the International Cooperative Ataxia Rating Scale, disease duration, age at onset, cytosine-adenine-guanine (CAG) repeat length, and the gain of the vestibulo-ocular reflex (VOR). In response to relatively low-acceleration, low-frequency rotational and bithermal caloric stimuli, the VOR gains were normal or increased regardless of the severity of disease. On the other hand, with relatively high-acceleration, high-frequency head impulses, there was a relative increase in gain in the mildly affected patients and a decrease in gain in the more severely affected patients and gains were negatively correlated with the severity of disease (Spearman correlation, R=−0.927, p<0.001). Selective decrease of the vestibular responses during high-acceleration, high-frequency stimuli may be ascribed to degeneration of either the flocculus or vestibular nuclei. The performance of the VOR during high-acceleration, high-frequency head impulses may be a quantitative indicator of clinical decline in SCA6.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Spinocerebellar ataxia type 6 (SCA6) is a relatively pure cerebellar form of spinocerebellar ataxia (SCA) due to a small cytosine-adenine-guanine (CAG) repeat expansion in the CACNA1A gene [1]. Ocular motor abnormalities of SCA6 include spontaneous, gaze-evoked, head-shaking, and positional downbeat nystagmus; saccadic dysmetria; impaired smooth pursuit (SP); and impaired cancellation of the vestibulo-ocular reflex (VOR) with fixation suppression [1–6]. In contrast, the gain of the VOR has been reported to be normal [2, 7], decreased [8, 9], or increased [1]. These discrepancies may stem from the different frequencies or accelerations of the stimuli used to evaluate the VOR in these studies. VOR abnormalities that differ depending on characteristics of the stimulus have also been observed in patients with central vestibular lesions [10, 11]. Recently, a selective reduction in VOR gain during head impulses has been reported in a patient with an isolated floccular infarction [11]. In SCA6, the flocculus is more severely affected compared to the cerebellum or pons [12]. The disease severity may also have contributed to the discrepancies in VOR gain in SCA6. Indeed, ocular motor abnormalities correlate with the clinical parameters, CAG repeat length, or disease severity, in SCA2, SCA3, and SCA17 [13–16]. However, correlations among the ocular motor impairments and clinical parameters have rarely been reported in SCA6 [6].
Therefore, we sought to determine the vestibular dysfunction in patients with SCA6 using a broad range of stimuli including bithermal caloric, rotary chair, and head impulse tests. We also correlated vestibular responses with clinical parameters including the age at onset, disease duration and severity, and CAG repeat length.
Methods
Subjects
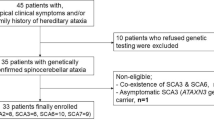
We prospectively studied 11 patients with genetically confirmed SCA6 (six men, age range=33–72 years, mean age±SD=59±12 years). Patients had neither a history of peripheral vestibular diseases nor an exposure to ototoxic medication. Medications that could affect ocular motor and vestibular function were not used during the study. All patients had a full neurological and neuro-otological evaluation by one of the authors (J.S.K.). The International Cooperative Ataxia Rating Scale (ICARS) was applied at the time of their evaluation. Demographic and clinical details of the patients are presented in Table 1. Normative data were obtained from 29 healthy age-matched volunteers (14 men) with the ages ranging from 33 to 73 years (mean±SD=54±11 years).
All experiments complied with the tenets of the Declaration of Helsinki, and informed consent was obtained after the nature and possible consequences of this study had been explained to the participants. The study protocol was also approved by the Institutional Review Board of Seoul National University Bundang Hospital.
Evaluation of the Vestibular Function
The VOR was evaluated using bithermal caloric, rotary chair, and head impulse tests. Caloric stimuli were provided by irrigating the ears for 25 s with 50 mL of cold and hot water (30 and 44 °C, respectively) [17]. Total sum of the peak responses to each caloric stimulus was defined as the caloric response.
The CHARTR® rotary vestibular test system (ICS Medical, Schaumburg, IL, USA) was used to assess the horizontal VOR during sinusoidal harmonic accelerations. Sinusoidal rotation was about a vertical axis at frequencies of 0.02, 0.04, 0.08, 0.16, and 0.32 Hz and a peak angular velocity of 50°/s. Eye position was detected with electrodes placed using standard methods and was digitized at 160 Hz with a frequency response of 0–30 Hz and notch filter at 60 Hz. The velocity of eye movement elicited was compared with the velocity of the stimulus (assumed to be the same as head velocity). The resultant velocity curve was then analyzed using Fourier analysis. At each frequency, gain of the peak slow-phase eye velocity relative to the peak chair velocity was calculated.
To assess the VOR during head impulse testing (HIT), a magnetic search coil technique was adopted using three-dimensional scleral coils. Rotation of the eye and head was recorded in a 70-cm cubic search coil frame (Skalar, Delft, Netherlands). Digitized eye and head position data were analyzed with MATLAB software. For HIT, the patient was instructed to fix on a red target (0.25°) 1.2 m away. The head impulses were passive and unpredictable head rotations with amplitudes of 20–30°, peak velocities of 200–300°/s, and peak accelerations of 3000–5000°/s2. They were delivered in the planes of the both horizontal canals (HCs), left anterior and right posterior canals, and right anterior and left posterior canals while the subjects sat upright. A minimum of five impulses was applied in each direction. The VOR gain was calculated for each trial as the ratio between the peak eye velocity and peak head velocity after excluding the component of covert saccades with a visual inspection of all individual waves by the experienced authors (J.S.K. and H.J.K.). Thus, in the trials with covert saccades, the peak eye velocities were mostly obtained from the maximal eye velocity just before the take-off of covert saccades [11].
International Cooperative Ataxia Rating Scale
Disability was scored according to the ICARS, a semi-quantitative ataxia scale [18]. ICARS is a 100-point scale that is divided into four subscales, consisting of postural and gait disturbance (34 points), limb kinetic function (52 points), speech disorder (8 points), and ocular motor function (6 points). Higher scores indicate worse performance.
Statistical Analysis
Shapiro-Wilk test was used to determine the normality of data. Between the patient and control groups, differences in the parametric variables were analyzed using Student’s t-test. Spearman correlation and Mann-Whitney U test were used for nonparametric data. The level of significance was set at p < 0.05. Normal values for ocular motor parameters were defined as the mean±2SD.
Results
Clinical Characteristics
Detailed demographic and the clinical characteristics of the patients are presented in Table 1. Patients 1 and 6, and patients 2 and 3 were siblings. Fluctuating or episodic symptoms were frequently observed during the early stage of illness (7/11, 64 %). Four patients initially presented with recurrent episodes of dizziness, preceding ataxia or dysarthria. In three patients (patients 1–3), acetazolamide and 3,4-diaminopyridine had been tried with variable subjective improvements, but without a definite effect on ocular motor findings. Nine patients underwent brain MRI that showed variable degrees of cerebellar atrophy.
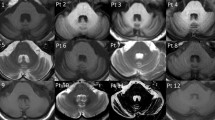
Vestibular Function (Fig. 1 and Supplementary Table)
Vestibular responses in the patients with spinocerebellar ataxia type 6. The VOR gains during head impulse test (HIT) are variously affected, but those during rotary chair and caloric tests were generally increased. In patient 11, VOR gains during HIT were increased only for right horizontal canal, and the mean gain for both horizontal canals was within normal range. Results of rotary chair test are presented for ten patients who had this test. Vestibular responses of individual patient are illustrated as colored dots with a solid line during HIT, rotary chair test (gain at 0.08 Hz), and caloric tests. Gray areas represent the normal range (mean±2SD) of each test. Caloric response indicates the sum of the peak slow-phase velocity of the nystagmus induced in the four stimulus conditions of bithermal caloric tests. HIT-AC head impulse testing in the anterior semicircular canal plane, HIT-HC head impulse testing in the horizontal semicircular canal plane, HIT-PC head impulse testing in the posterior semicircular canal plane
The caloric responses were significantly increased in 10/11 patients (91 %). Rotary chair test was performed in ten patients, and half (5/10) showed increased VOR gains during sinusoidal rotation at more than two stimulation frequencies. The mean VOR gain for each stimulation frequency was symmetric and significantly higher than the normal value except at 0.02 Hz. Small phase leads were observed in five patients.
The VOR responses to head impulses were variously affected in the patients. Most patients (10/11, 91 %) showed abnormal responses to stimulation of at least one semicircular canal (SCC), increased in six and decreased in four. The head impulse VOR gains also varied according to the SCC stimulated. Head impulses in the HC plane showed abnormal gains in eight patients (73 %), increased in four and decreased in four. The gains for anterior canal (AC) were also abnormal in four (36 %), increased in three and decreased in one, while those for the posterior canal (PC) were decreased in two patients (18 %). Even though the head impulse VOR gains did not differ between either side (paired t-test, p > 0.05), five patients showed an abnormal gain in only one of each SCC pair. The VOR responses to head impulses were normal for all six SCCs in only one patient (patient 6) whose functional disability was minimal, whereas those were uniformly decreased for all six SCCs in the most severely affected patient (patient 1, Fig. 2, Video).
Results of the vestibular function tests in patient 1. Caloric test (a). The sum of the peak slow-phase velocity (SPV) of the nystagmus in response to each caloric stimulus is increased at 174°/s (normal range=45–157°/s). Rotary chair test (b). The gains of the vestibulo-ocular reflex (VOR) are normal during sinusoidal horizontal accelerations. Gray areas represent the normal ranges (mean±2SD). Head impulse tests (c). Head impulses in the plane of each semicircular canal (SCC) revealed decreased gain of the VOR for all six semicircular canals with overt catch-up saccades during stimulation of the horizontal and posterior SCCs. The blue lines indicate head velocity, and the red lines represent eye velocity. LAC left anterior SCC, LHC left horizontal SCC, LPC left posterior SCC, RAC right anterior SCC, RHC right horizontal SCC. RPC right posterior SCC
Correlations Among the Ocular Motor Findings and Other Clinical Parameters (Table 2)
Correlations among the vestibular responses and other clinical parameters revealed that the VOR gains during horizontal head impulses inversely correlated with ICARS (R=−0.927, p<0.001, Fig. 3). However, no correlation was found between each clinical parameter (age, age at onset, disease duration, CAG repeat length, ICARS) and other ocular motor parameters (including the head impulse VOR gains of AC and PC, caloric responses, VOR gains during sinusoidal rotation). There was also a positive correlation between ICARS and the disease duration (R=0.706, p=0.015) and a negative correlation between the age at onset and CAG repeat length (R=−0.830, p=0.002).
Correlation between the vestibulo-ocular reflex (VOR) gain during horizontal head impulse test (HIT) and ataxia. VOR gain of the horizontal semicircular canal is negatively correlated with the ataxia score as measured using the International Cooperative Ataxia Rating Scale (ICARS). HIT-HC head impulse testing in the horizontal semicircular canal plane
Discussion
Our study described several new findings in SCA6. (1) Vestibular responses elicited by horizontal head impulses (high-acceleration/high-frequency stimuli) strongly correlated with the disease severity. Gains were relatively increased in patients with milder disability and decreased in more severely affected ones. (2) Vestibular responses during caloric irrigations and sinusoidal rotations (relatively low-acceleration/low-frequency stimuli) were normal or increased regardless of the disease severity. The age at onset was positively correlated with CAG repeat length as described in some previous studies [19].
In this study, the head impulse VOR gains were calculated by dividing the peak eye velocity with the peak head velocity after excluding the covert saccades with a visual inspection of all individual waves [20–22]. Even though several methods have been advanced to calculate the VOR gains during HIT [23], each method has its advantages and disadvantages in calculating the VOR gain. Even when we applied the methods for calculating head impulse VOR gain adopted in other studies, such as the mean of gains (eye velocity/head velocity) at 25, 50, and 75 ms prior to the peak head velocity or the mean eye velocity over mean head velocity during 20 ms around the peak head acceleration [24, 25], the statistics did not change.
Abnormal vestibular responses have also been reported in SCA1, SCA2, and SCA3 [4, 7, 15]. However, responses were generally reduced for all stimulus accelerations and frequencies [7, 15], especially for the lower acceleration stimuli [15]. On the contrary, the vestibular responses in our SCA6 patients differed even in a patient depending on the nature of the stimulus. This finding may account for the discrepancies in the VOR gain abnormalities reported in previous studies in which vestibular responses were elicited with relatively restricted ranges of accelerations and frequencies. We found that patients with milder neurological deficits tended to have increased VOR gains across the range of stimuli including head impulses. In addition, the vestibular response to low-acceleration/low-frequency stimuli remained increased irrespective of the disease severity whereas the horizontal VOR gains at higher acceleration and frequency stimuli using head impulses were more reduced in patients with greater disability. These findings indicate that the horizontal VOR gains to head impulses are increased during the earlier phase and undergo a gradual reduction with disease progression.
The vestibular responses in our patients may be explained based on the cerebellar pathology [1, 12], especially the flocculus that is known to have strong influences on the VOR [26]. The pathogenesis of SCA6 is not fully understood perhaps due to the diverse effects of CACNA1A mutation on the P/Q-type calcium channel [27–29], but deranged calcium signaling in the Purkinje cells may be the key pathogenesis of SCAs [30]. Excess of intracellular calcium due to an abnormal increase in the activity of the mutated calcium channels [27] may trigger cerebellar long-term depression as a protective mechanism against excitotoxicity in the Purkinje cells [31]. Cerebellar long-term depression in turn suppresses glutamatergic synaptic transmission and the Purkinje cell activity, resulting in disinhibition and consequent overactivation of the deep cerebellar nuclei [32] and possibly the portions of the vestibular nuclei that receive direct projections from the vestibulocerebellum including the flocculus. These changes would be responsible for the cerebellar dysfunction as well as increased VOR gain in our SCA6 patients during the early stage when the gross integrity of neural pathways is preserved. Eventually, calcium induced-excitotoxicity leads to a cascade of apoptosis and degeneration of the Purkinje cells [33]. Subsequent degeneration of the flocculus may explain the selective high-acceleration/high-frequency reduction in VOR gain measured with head impulses in our patients with more advanced stage. A recent study also demonstrated that the VOR gains were selectively reduced with high-frequency stimuli in murine CACNA1A mutants whose ocular motor disturbances were compatible with floccular dysfunction [34]. The authors suggested that, despite the inhibitory properties of the Purkinje cells, the modulation phase of the floccular Purkinje cells is appropriate to enhance the VOR gain [35]. In rabbits, the flocculus is known to provide a frequency-dependent signal [36] that normally enhances the VOR gain preferentially during high-acceleration/high-frequency stimuli. Thus, damage to the flocculus may generate a selective deficit in the VOR performance during head impulses. Alternatively, the VOR deficits due to a channelopathy may vary according to stimulus acceleration and frequency. Changes in the VOR gain in the later stage of SCA6 might be also explained based on the response dynamics of the VOR, which can be modeled by two separate pathways, the linear and nonlinear [37]. The linear pathway is responsible for retaining a constant VOR gain at low-acceleration stimuli. The nonlinear pathway accounts for enhancement of the VOR gain with increase of the stimulus acceleration and works at high-acceleration stimuli. These responses are presumed to arise from separate groups of vestibular afferents and may be controlled by distinctive central vestibular networks, such as the vestibular nuclear neurons [38]. Given the neuronal loss with gliosis in the vestibular nuclei observed in SCA6 [39], degeneration in the vestibular nuclei might produce the VOR gain reduction during high-acceleration/high-frequency stimuli and an increased gain during low-acceleration/low-frequency stimuli. Similar patterns of VOR gain changes, a decrease during high-acceleration and normal to increase during low-acceleration stimuli, were also found in animals with experimental cerebellar lesions and human patients with various types of presumably isolated cerebellar pathology [10, 11, 26].
The VOR gains for the vertical canals during head impulses also tended to be lower in patients with severe disability and vice versa, even though this finding did not reach statistical significance. Remarkably, the VOR gains were dissociated among the SCCs even in individual patients. Since the central VOR pathways are segregated for each SCC [40], the dissociated vestibular responses for each SCC could provide additional evidence indicating that abnormal vestibular responses in our patients stem from central rather than peripheral vestibular process.
Finally, we suggest that an impaired VOR during head impulses may be reliable surrogate markers for research on disease modifying therapy as well as for monitoring the progression of disease in SCA6.
References
Gomez CM, Thompson RM, Gammack JT, Perlman SL, Dobyns WB, Truwit CL, et al. Spinocerebellar ataxia type 6: gaze-evoked and vertical nystagmus, Purkinje cell degeneration, and variable age of onset. Ann Neurol. 1997;42:933–50.
Takeichi N, Fukushima K, Sasaki H, Yabe I, Tashiro K, Inuyama Y. Dissociation of smooth pursuit and vestibulo-ocular reflex cancellation in SCA-6. Neurology. 2000;54:860–6.
Yabe I, Sasaki H, Takeichi N, Takei A, Hamada T, Fukushima K, et al. Positional vertigo and macroscopic downbeat positioning nystagmus in spinocerebellar ataxia type 6 (SCA6). J Neurol. 2003;250:440–3.
Buttner N, Geschwind D, Jen JC, Perlman S, Pulst SM, Baloh RW. Oculomotor phenotypes in autosomal dominant ataxias. Arch Neurol. 1998;55:1353–7.
Kim JS, Youn J, Seo DW, Jeong Y, Kang JH, Park JH, et al. Ocular motor characteristics of different subtypes of spinocerebellar ataxia: distinguishing features. Mov Disord. 2013.
Zee DS, Yee RD, Cogan DG, Robinson DA, Engel WK. Ocular motor abnormalities in hereditary cerebellar ataxia. Brain. 1976;99:207–34.
Gordon CR, Joffe V, Vainstein G, Gadoth N. Vestibulo-ocular arreflexia in families with spinocerebellar ataxia type 3 (Machado-Joseph disease). J Neurol Neurosurg Psychiatry. 2003;74:1403–6.
Yu-Wai-Man P, Gorman G, Bateman DE, Leigh RJ, Chinnery PF. Vertigo and vestibular abnormalities in spinocerebellar ataxia type 6. J Neurol. 2009;256:78–82.
Crane BT, Tian JR, Demer JL. Initial vestibulo-ocular reflex during transient angular and linear acceleration in human cerebellar dysfunction. Exp Brain Res. 2000;130:486–96.
Kremmyda O, Kirchner H, Glasauer S, Brandt T, Jahn K, Strupp M. False-positive head-impulse test in cerebellar ataxia. Front Neurol. 2012;3:162.
Park HK, Kim JS, Strupp M, Zee DS. Isolated floccular infarction: impaired vestibular responses to horizontal head impulse. J Neurol. 2013;260:1576–82.
Ying SH, Choi SI, Lee M, Perlman SL, Baloh RW, Toga AW, et al. Relative atrophy of the flocculus and ocular motor dysfunction in SCA2 and SCA6. Ann N Y Acad Sci. 2005;1039:430–5.
Rivaud-Pechoux S, Durr A, Gaymard B, Cancel G, Ploner CJ, Agid Y, et al. Eye movement abnormalities correlate with genotype in autosomal dominant cerebellar ataxia type I. Ann Neurol. 1998;43:297–302.
Velazquez-Perez L, Seifried C, Santos-Falcon N, Abele M, Ziemann U, Almaguer LE, et al. Saccade velocity is controlled by polyglutamine size in spinocerebellar ataxia 2. Ann Neurol. 2004;56:444–7.
Burk K, Fetter M, Abele M, Laccone F, Brice A, Dichgans J, et al. Autosomal dominant cerebellar ataxia type I: oculomotor abnormalities in families with SCA1, SCA2, and SCA3. J Neurol. 1999;246:789–97.
Hubner J, Sprenger A, Klein C, Hagenah J, Rambold H, Zuhlke C, et al. Eye movement abnormalities in spinocerebellar ataxia type 17 (SCA17). Neurology. 2007;69:1160–8.
Huh YE, Kim JS. Patterns of spontaneous and head-shaking nystagmus in cerebellar infarction: imaging correlations. Brain. 2011;134:3662–71.
Saute JA, Donis KC, Serrano-Munuera C, Genis D, Ramirez LT, Mazzetti P, et al. Ataxia rating scales—psychometric profiles, natural history and their application in clinical trials. Cerebellum. 2012;11:488–504.
Takahashi H, Ishikawa K, Tsutsumi T, Fujigasaki H, Kawata A, Okiyama R, et al. A clinical and genetic study in a large cohort of patients with spinocerebellar ataxia type 6. J Hum Genet. 2004;49:256–64.
Fahey MC, Cremer PD, Aw ST, Millist L, Todd MJ, White OB, et al. Vestibular, saccadic and fixation abnormalities in genetically confirmed Friedreich ataxia. Brain. 2008;131:1035–45.
Aw ST, Haslwanter T, Halmagyi GM, Curthoys IS, Yavor RA, Todd MJ. Three-dimensional vector analysis of the human vestibuloocular reflex in response to high-acceleration head rotations. I. Responses in normal subjects. J Neurophysiol. 1996;76:4009–20.
Aw ST, Halmagyi GM, Haslwanter T, Curthoys IS, Yavor RA, Todd MJ. Three-dimensional vector analysis of the human vestibuloocular reflex in response to high-acceleration head rotations. II. Responses in subjects with unilateral vestibular loss and selective semicircular canal occlusion. J Neurophysiol. 1996;76:4021–30.
Halmagyi GM, Weber KP, Aw ST, Todd MJ, Curthoys IS. Impulsive testing of semicircular canal function. Prog Brain Res. 2008;171:187–94.
Cremer PD, Halmagyi GM, Aw ST, Curthoys IS, McGarvie LA, Todd MJ, et al. Semicircular canal plane head impulses detect absent function of individual semicircular canals. Brain. 1998;121(Pt 4):699–716.
Agrawal Y, Schubert MC, Migliaccio AA, Zee DS, Schneider E, Lehnen N, et al. Evaluation of quantitative head impulse testing using search coils versus video-oculography in older individuals. Otol Neurotol. 2014;35:283–8.
Lisberger SG, Miles FA, Zee DS. Signals used to compute errors in monkey vestibuloocular reflex: possible role of flocculus. J Neurophysiol. 1984;52:1140–53.
Piedras-Renteria ES, Watase K, Harata N, Zhuchenko O, Zoghbi HY, Lee CC, et al. Increased expression of alpha 1A Ca2+ channel currents arising from expanded trinucleotide repeats in spinocerebellar ataxia type 6. J Neurosci. 2001;21:9185–93.
Burgess DL, Jones JM, Meisler MH, Noebels JL. Mutation of the Ca2+ channel beta subunit gene Cchb4 is associated with ataxia and seizures in the lethargic (lh) mouse. Cell. 1997;88:385–92.
Tully K, Treistman SN. Distinct intracellular calcium profiles following influx through N- versus L-type calcium channels: role of Ca2 + -induced Ca2+ release. J Neurophysiol. 2004;92:135–43.
Kasumu A, Bezprozvanny I. Deranged calcium signaling in Purkinje cells and pathogenesis in spinocerebellar ataxia 2 (SCA2) and other ataxias. Cerebellum. 2012;11:630–9.
Miyata M, Finch EA, Khiroug L, Hashimoto K, Hayasaka S, Oda SI, et al. Local calcium release in dendritic spines required for long-term synaptic depression. Neuron. 2000;28:233–44.
Shakkottai VG, Chou CH, Oddo S, Sailer CA, Knaus HG, Gutman GA, et al. Enhanced neuronal excitability in the absence of neurodegeneration induces cerebellar ataxia. J Clin Invest. 2004;113:582–90.
Strahlendorf J, Box C, Attridge J, Diertien J, Finckbone V, Henne WM, et al. AMPA-induced dark cell degeneration of cerebellar Purkinje neurons involves activation of caspases and apparent mitochondrial dysfunction. Brain Res. 2003;994:146–59.
Stahl JS, James RA, Oommen BS, Hoebeek FE, De Zeeuw CI. Eye movements of the murine P/Q calcium channel mutant tottering, and the impact of aging. J Neurophysiol. 2006;95:1588–607.
De Zeeuw CI, Wylie DR, Stahl JS, Simpson JI. Phase relations of Purkinje cells in the rabbit flocculus during compensatory eye movements. J Neurophysiol. 1995;74:2051–64.
Stahl JS, Simpson JI. Dynamics of rabbit vestibular nucleus neurons and the influence of the flocculus. J Neurophysiol. 1995;73:1396–413.
Minor LB, Lasker DM, Backous DD, Hullar TE. Horizontal vestibuloocular reflex evoked by high-acceleration rotations in the squirrel monkey. I. Normal responses. J Neurophysiol. 1999;82:1254–70.
Chen-Huang C, McCrea RA, Goldberg JM. Contributions of regularly and irregularly discharging vestibular-nerve inputs to the discharge of central vestibular neurons in the alert squirrel monkey. Exp Brain Res. 1997;114:405–22.
Gierga K, Schelhaas HJ, Brunt ER, Seidel K, Scherzed W, Egensperger R, et al. Spinocerebellar ataxia type 6 (SCA6): neurodegeneration goes beyond the known brain predilection sites. Neuropathol Appl Neurobiol. 2009;35:515–27.
Leigh RJ, Zee DS. The neurology of eye movements. New York: Oxford University Press; 2006.
Acknowledgments
This study was supported by a grant of Korea Medical Device Industrial Cooperative Association.
Conflict of Interest
Drs. Huh, Park, J.M. Kim, and J. W. Cho, and Ms. H.J. Kim report no disclosure.
Dr. J.S. Kim serves as an Associate Editor of Frontiers in Neuro-otology and on the Editorial Boards of the Journal of Korean Society of Clinical Neurophysiology, Research in Vestibular Science, Journal of Clinical Neurology, Frontiers in Neuro-ophthalmology, Journal of Neuro-ophthalmology, and Journal of Vestibular Research and received research support from SK Chemicals, Co. Ltd.
Dr. Jeon has received funding for travel from Novartis Korea and GlaxoSmithKline Korea and has received research support as PI from Norvartis, Boehringer Ingelheim, Ipsen, the Korea Health 21 R&D project, Ministry of Health & Welfare, Republic of Korea (A101273), the National Research Foundation of Korea(NRF), Ministry of Education, Science and Technology (2010-0021653), Advanced Biometric Research Center (ABRC), Korean Science and Engineering Foundation (KOSEF), Seoul National University Hospital, the Mr. Chung Suk-Gyoo and Sinyang Cultural Foundation, and the Song Foundation.
Dr. Zee receives research support from the National Institutes of Health and is an Associate Editor of Frontiers in Neuro-otology and a member of the Editorial Board of the Cerebellum. He received speaker’s honoraria from Abbott and Micromed and from Sun Pharmaceuticals and from the American Academy of Neurology.
Author Contributions
Drs. J.S. Kim and Zee conducted the design and conceptualization of the study, interpretation of the data, and drafting and revising the manuscript. Dr. Huh conducted the design and conceptualization of the study, wrote the manuscript, and analyzed and interpreted the data. Drs. Park, Jeon, J.M. Kim, and Cho contributed to the study concept and design and interpreted the data. Ms. H.J. Kim analyzed and interpreted the data.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Video Head impulse test in patient 1. Bedside head impulse tests were positive in both horizontal directions with corrective saccades. Bedside head impulse tests were performed manually with a rapid rotation of the head in the planes of the horizontal canals. Head impulse test was considered abnormal if a corrective saccade had to be generated to maintain fixation on the target because the slow phase was of the wrong amplitude (MPG 975 kb)
Rights and permissions
About this article
Cite this article
Huh, Y.E., Kim, JS., Kim, HJ. et al. Vestibular Performance During High-Acceleration Stimuli Correlates with Clinical Decline in SCA6. Cerebellum 14, 284–291 (2015). https://doi.org/10.1007/s12311-015-0650-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12311-015-0650-3