Abstract
We describe a patient with a probable diagnosis of idiopathic late-onset cerebellar atrophy who shows improvement of limb coordination, speech, and gait following 21 days of transcranial magnetic stimulation (TMS) applied to scalp regions presumably corresponding to the cerebellum. This case study provides, for the first time, a quantitative assessment of gait improvement in response to TMS therapy in ataxia, as well as neurophysiological evidence in support of modification of cerebellar-cortical interaction that may underlie some of the improvements.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Idiopathic late-onset cerebellar ataxia was coined by Harding in 1981 to refer to sporadic adult onset ataxias of unknown etiology [1]. To date, available therapies primarily offer symptomatic improvements and no curative treatment has been established [2]. Shiga and colleagues explored the efficacy of 21 days of cerebellar TMS in alleviating truncal ataxia in 74 patients with diagnosis of cerebellar atrophy including spinocerebellar ataxia (SCA)1, SCA3, and SCA6 as well as olivopontocerebellar atrophy [3, 4]. Patients were enrolled in a placebo-controlled trial and were clinically evaluated before and after the treatment. Patients who received active treatments exhibited improved gait and increased regional blood flow (rBF) in the cerebellum and pons. Despite positive clinical outcomes, however, no causal relationship was established between rBF changes and clinical improvements. Furthermore, the extent of observed functional improvement was not reported and quantitative assessments of gait and physical function were not performed. Here, we report on the effects of the TMS intervention outlined in Shiga et al. in a clinically and genetically carefully evaluated patient using quantitative movement kinematics and neurophysiological assessments to provide further insight into the therapeutic mechanism of TMS in cerebellar ataxia.
Methods
Subject
A 62-year-old female diabetic patient developed speech and gait difficulties at the age of 37. These symptoms progressed to the point that she now uses a four-wheeled rollator walker for ambulation and requires help with bathing and dressing, but still maintains bowel and bladder control. Clinical examination revealed cervical dystonia, axial and appendicular ataxia, rotatory nystagmus with slow saccadic eye movements, scanning speech with dysarthria, severe truncal ataxia and a wide-based gait. In addition, she exhibits some psychomotor slowing. There is no autonomic dysfunction, hyperreflexia, sexual and sleep disorders, dysphagia, rest tremor, or neuropathy. Brain magnetic resonance imaging (MRI) showed cerebellar atrophy out of proportion to mild diffuse cortical atrophy and no other lesions or abnormalities (Fig. 1). Furthermore, a routine EMG examination was normal, ruling out a peripheral neuropathy. Based upon the patient's clinical characteristics, we performed genetic testing and as a result we were able to exclude the diagnoses of SCA 1, 2, and 3, and Friedreich's Ataxia. The absence of pontine atrophy on MRI rules out olivopontocerebellar atrophy [5]. Moreover, a review of a detailed 4-generation pedigree revealed no family history of ataxia.
Sagittal view of the patient’s brain as depicted by anatomical MRI. Of note, the presented MRI was obtained in 2004, approximately 8 years prior to the present trial. Given the progressive nature of this illness, it is expected that a more recent MRI scan would more accurately illustrate the current structure of the patient’s brain
Treatment Protocol
Daily sessions of TMS were delivered with a Magstim 200 (Magstim, UK) for 21 days at 100 % of maximum stimulator output with a 14-cm circular coil with the handle held upward. As introduced by Shiga et al. [3], each day (at the same time in midmorning), TMS was applied to the following regions in a fixed order: (1) coil centered 4cm lateral to the right of the inion, (2) coil centered on the inion, and (3) coil centered 4-cm lateral to the left of the inion. For each region, five pulses separated by 6 s were first delivered with current flowing counter clockwise followed by five clockwise pulses, for a total of 30 pulses per session.
Quantitative Gait Assessment
Assessments were conducted before (i.e., on day 1) and after (i.e., on day 21) TMS therapy. Functional mobility was assessed by the timed up-and-go test [6]. The patient began seated in an armed chair and was instructed to stand up using the arm rests if needed, walk (with the walker) around a cone placed three meters in front of the chair, return, and sit down as quickly as possible. The time to complete the test was recorded.
Postural control during standing was measured from changes in body sway (i.e., center of pressure) during two, 30-s trials of standing with eyes open on a stationary force platform (AMTI, Watertown, MA). Average postural sway speed (i.e., center-of-pressure path length divided by trial duration) and area (i.e., the area of a confidence ellipse enclosing 95 % of the center-of-pressure signal) were computed and averaged across trials.
Gait was assessed during 90 s of walking at preferred speed along an 80 × 4m indoor hallway. The patient completed one trial of normal walking and one trial of cognitive dual tasking (i.e., walking while naming items found in a supermarket). The timing of each heel and toe ground contact was recorded with footswitches and the activity of lower-leg antagonistic musculature (i.e., tibialis anterior and lateral gastrocnemius) was recorded with standard EMG, using the wireless Noraxon DTS system (Noraxon Inc, Scottsdale, AZ). We computed average gait speed, stride duration variability (i.e., the coefficient of variation about the average stride duration as determined by heel strike to heel strike of the same leg), and double support time (i.e., the average percentage of time of each stride spent with both feet on the ground). The coordination of muscle contraction was examined by computing a co-contraction index between antagonistic muscles [7].
Neurophysiological Assessments
Dual coil-paired pulse TMS was used to examine the cerebellothalamocortical connectivity [8] before (i.e., on day 1) and after the TMS treatment (i.e., on day 21). It has been shown that lateral cerebellar stimulation (e.g., 3-cm lateral to the inion) delivered 5–7 ms prior to a contralateral cortical magnetic stimulation reduces the motor evoked potential (MEP) induced by the cortical stimulation as compared to MEP induced by cortical stimulation delivered alone [8, 9]. TMS-induced cerebellar inhibition (referred to as CBI) was examined according to previously published methods [8]. In short, two Magstim 200 stimulators (The Magstim Company, UK) were connected by a BiStim Module. Surface EMG activity of the left and right first dorsal interosseous (FDI) muscle was recorded (1,280 Hz sampling rate) and filtered (10 Hz – 1 KHz) by PowerLab (ADInstruments, Australia). TMS intensity was determined by placing a figure-of-eight coil over the optimal position in the motor cortex for eliciting MEPs in the FDI muscle, and defined as the intensity that induced average MEPs of about 0.5 mV peak-to-peak in ten trials. The intensity of cerebellar stimulation was set at 5 % less than the active motor threshold for activating the corticospinal tract by placing a double-cone coil over the inion and recording EMG from the FDI muscle. We recorded CBI at three intervals for the right FDI (CBI_5, CBI_6, and CBI_7 ms) and at one interval for the left FDI (CBI_5 ms). A total of ten trials were delivered per each condition. Suppression or facilitation of MEPs was then expressed as the ratio of average MEP size in the paired pulse condition to the MEP size in the single pulse condition.
TMS Maintenance Sessions and Follow-Up Assessment
The patient began receiving maintenance TMS sessions once every week, 45 days after conclusion of the initial TMS intervention. Each maintenance session was similar to those of the initial intervention. Neurophysiological and quantitative functional measures were also reassessed 6 months after completion of the initial intervention.
Results
Clinical Observation
The patient was clinically examined at baseline (i.e., on day 1, prior to TMS treatment) and after each week of treatment. A mild improvement was observed in the patient's speech after the first week as characterized by a louder and clearer voice. The patient exhibited reduced dysmetria and tremor in the finger to nose and the finger-chase tests, as well as improved tracing ability (Fig. 2). The patient’s husband and caregiver reported improvement in the patient's facial expression, a reduction in the weight exerted on the caregiver's arm during assisted walking, and improved and less effortful rhythmicity in pedaling in the patient's routine exercise program on a stationary recumbent bicycle.
Patient performance in a tracing task. The patient's performance was evaluated before (day 1) (a), midway (day 10) (b), and in the last week of the rTMS intervention (day 21) (c). The patient was instructed to draw a line within the figure without touching any edges. It can be observed that the patient committed lesser errors after the intervention
Quantitative Assessment of Physical Function
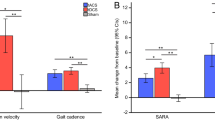
The patient completed the timed up-and-go test 9 % faster (from 34 to 31 s) following the intervention compared to baseline. Noticeable improvements were also observed in standing postural control (Fig. 3a). The average speed and area of postural sway declined from 29 to 22 mm/s and from 2,080 to 1,420 mm2, respectively. The kinematic and electromyographic characteristics of gait also improved. In the normal and cognitive dual task conditions, respectively, gait speed increased 15 and 33 %, stride duration variability decreased 21 and 26 %, and double support time decreased 43 and 47 %. Moreover, visually-apparent changes were observed in lower leg antagonistic co-contraction, such that more rhythmical patterns of muscular coordination were present following the intervention (Fig. 3b). Each of these improvements in mobility, standing postural control, gait kinematics, and muscle coordination were maintained at the 6-month follow-up assessment.
Kinematics and neurophysiological measures acquired before and after the TMS therapy. Panel A demonstrates improvements in standing posture control as evidenced by a reduction in the area of postural sway immediately following TMS therapy (b) as compared to baseline (a). These improvements were preserved 6 months following the trial (c). Panel B demonstrates more rhythmic patterns of lower right leg antagonistic muscle coordination immediately following the TMS therapy (b) and at 6 months after the therapy (c) as compared to baseline (a). Panel C demonstrates reduction of cerebellar inhibition for the interstimulus intervals of 5–7 ms in the right FDI immediately after TMS therapy (white bars), and at 6 months after therapy (black bars, tested at the interstimulus interval of 5 ms) as compared to baseline (gray bars). Error bars indicate the standard error of the mean and asterisks indicate p <0.001
Neurophysiological Assessments
There were significant changes in CBI following the TMS course as compared to baseline (Fig. 3c). Prior to treatment, MEPs were significantly suppressed in the paired pulse conditions in the right FDI (CBI_5 ms = 0.40, p = 0.01; CBI_6 ms = 0.24, p = 0.001; CBI_7 ms = 0.30, p = 0.002) and were moderately suppressed in the left FDI (CBI_5 ms = 0.52, p = 0.14). Following 21 days of treatment, MEPs were significantly facilitated in the paired pulse conditions for the right FDI (CBI_5 ms = 3.74, p = 0.003; CBI_6 ms = 3.38, p = 0.005; CBI_7 ms = 4.69, p = 0.0001) and were moderately facilitated in the left FDI (CBI_5 ms = 1.63, p = 0.1). Finally, in the follow-up assessment, the MEPs were still significantly facilitated in the paired pulse condition in the right FDI (CBI_5 ms = 3.18, p = 0.01).
Discussion
We report functional improvements following 21 days of cerebellar TMS in a patient with probable diagnosis of idiopathic late-onset cerebellar ataxia. Our results extend the findings by Shiga et al. by providing quantitative evidence of gait, and physical function improvements, as well as neurophysiological modifications that may provide insight into the mechanisms of TMS therapy.
Through EMG and kinematics assessments, we objectively documented and quantified improvements in functional mobility, standing postural control, and gait kinematics including rhythmic co-contraction of lower leg antagonistic musculature. These changes were still present 6 months after the initial TMS trial (Fig. 3a–b.) We propose that these improvements may collectively reflect more effective cerebellar control over motor function. The cerebellum regulates motor function by means of its interaction with the primary motor cortex. Specifically, it sends efferent fibers to the motor cortex through the cerebello (dentate nucleus) thalamocortical pathway and receives afferent fibers from the motor cortex through the frontopontocerebellar pathway [10, 11]. This bidirectional connectivity results in a temporospatial precision of motion through the coordination of the agonist and antagonist muscles. Moreover, the cerebellum is believed to play a significant role in corporal equilibrium by processing sensory inputs from the visual, the vestibular, and proprioceptive system (joints, bones, and muscles) regarding the position of the body with respect to the external environment [12].
We assessed the cerebellar-cortical pathway by a dual coil-paired pulse TMS paradigm in which a preceding cerebellar stimulus inhibits the motor response to stimulation of contralateral motor cortex. This TMS-induced CBI is thought to be mediated through activation of the Purkinje cell in the cerebellar cortex and subsequent inhibition of the facilitatory cerebello(dentate nucleus)-thalamic efferent to the contralateral motor cortex in healthy subjects [8]. Following TMS therapy, we observed a significant CBI reduction, which also persisted 6 months after the initial trial (Fig. 3c). Previous studies in healthy subjects have also reported CBI reduction up to 30 min following one session of 1-Hz repetitive TMS applied to the cerebellar hemispheres [13]. These authors suggested that reduction of cerebellar inhibition may be due to transient depletion of cerebellar cortex of neuromediatory mechanisms responsible for suppression of the dentate nucleus [14–18].
While the mechanism of action of TMS remains speculative in patients with cerebellar atrophy, we hypothesize that low-frequency TMS exerts its therapeutic efficacy by reducing the cerebellar cortex inhibitory control over dentate nucleus, thereby potentiating some of dentate nucleus lost activities. In addition, a decreased inhibitory signal from Purkinje cells may enhance the activation of the vestibular nuclei resulting in balance improvement [15]. The Purkinje axons from the vestibular–cerebellum end primarily in parts of the vestibular nuclei that sends ascending fibers to the external ocular muscles through the medial longitudinal fasciculus [19], and to a lesser extent, to the spinal cord. Thus, the vestibular–cerebellum contributes to the control of eye movements and the control of the axial muscles that play pivotal roles in maintaining the postural balance [20].
The observed improvements in speech and dual tasking may also be associated with enhanced cerebellar non-motor function [21]. The patient could name more items found in a supermarket while walking with more ease as evident by a decrease in double support time. This improvement may be a consequence of enhanced motor function and liberating resources for the performance of the concurrent cognitive task. The TMS intervention may also have improved prefrontal function directly thus improving cognitive capacity. Cerebellar nuclei target both motor and prefrontal cortices [22, 23], and previous studies in healthy subjects have shown modification of prefrontal cortex activity and cognitive functions following cerebellar stimulation [24, 25]. It is, therefore, possible that cerebellar stimulation improves both motor and cognitive function through cerebellar projections to both motor and non-motor areas including the prefrontal cortex.
Conclusion
In this case study, we provide further evidence for the efficacy of cerebellar stimulation as a treatment strategy in cerebellar degenerative ataxia. Observed improvements in physical function, gait kinematics, and muscle co-contraction, and cerebellar-cortical interaction are compelling. As this case study lacked both control subjects and control conditions, future controlled trials are warranted to further explore the effects of TMS therapy in these vulnerable patients. Future studies should also include nystagmography to further identify rTMS effect on the abnormal oculomotor control. We envision that a future placebo-controlled trial in patients with genetically confirmed ataxia would permit identifying individuals who would benefit the most from this therapy. Moreover, studies should (1) compare the effect of sham versus active TMS treatment in patients, (2) quantify the effect of 1 day of active versus sham cerebellar TMS in healthy subjects, and (3) compare the efficacy and specificity of TMS treatment with other interventions such as physical therapy. Furthermore, neuroimaging modalities such as diffusion spectrum imaging [26], functional magnetic resonance imaging [27], and electroencephalography [25] might be used to precisely identify the mechanisms of TMS with more efficacy in each patient, and lead to design of more accurate (i.e., neuronavigated), effective and ultimately individually tailored treatment protocols.
References
Harding AE. "Idiopathic" late onset cerebellar ataxia. A clinical and genetic study of 36 cases. J Neurol Sci. 1981;51(2):259–71. Epub 1981/08/01.
Trujillo-Martin MM, Serrano-Aguilar P, Monton-Alvarez F, Carrillo-Fumero R. Effectiveness and safety of treatments for degenerative ataxias: a systematic review. Mov Disord. 2009;24(8):1111–24. Epub 2009/05/05.
Shiga Y, Tsuda T, Itoyama Y, Shimizu H, Miyazawa KI, Jin K, et al. Transcranial magnetic stimulation alleviates truncal ataxia in spinocerebellar degeneration. J Neurol Neurosurg Psychiatry. 2002;72(1):124–6. Epub 2002/01/11.
Shimizu H, Tsuda T, Shiga Y, Miyazawa K, Onodera Y, Matsuzaki M, et al. Therapeutic efficacy of transcranial magnetic stimulation for hereditary spinocerebellar degeneration. Tohoku J Exp Med. 1999;189(3):203–11. Epub 2000/02/16.
Klockgether T, Schroth G, Diener HC, Dichgans J. Idiopathic cerebellar ataxia of late onset: natural history and MRI morphology. J Neurol Neurosurg Psychiatry. 1990;53(4):297–305. Epub 1990/04/01.
Podsiadlo D, Richardson S. The timed "up and go": a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39(2):142–8. Epub 1991/02/01.
Rudolph KS, Axe MJ, Snyder-Mackler L. Dynamic stability after ACL injury: who can hop? Knee Surg Sports Traumatol Arthrosc Off J ESSKA. 2000;8(5):262–9. Epub 2000/11/04.
Ugawa Y, Uesaka Y, Terao Y, Hanajima R, Kanazawa I. Magnetic stimulation over the cerebellum in humans. Ann Neurol. 1995;37(6):703–13. Epub 1995/06/01.
Pinto AD, Chen R. Suppression of the motor cortex by magnetic stimulation of the cerebellum. Exp Brain Res. 2001;140(4):505–10. Epub 2001/10/31.
Groiss SJ, Ugawa Y. Cerebellar stimulation in Ataxia. Cerebellum. 2012;11(2):440–2. doi:10.1007/s12311-011-0329-3.
Schmahmann JD, Smith EE, Eichler FS, Filley CM. Cerebral white matter: neuroanatomy, clinical neurology, and neurobehavioral correlates. Ann N Y Acad Sci. 2008;1142:266–309. Epub 2008/11/08.
Fine EJ, Ionita CC, Lohr L. The history of the development of the cerebellar examination. Semin Neurol. 2002;22(4):375–84. Epub 2003/01/23.
Popa T, Russo M, Meunier S. Long-lasting inhibition of cerebellar output. Brain Stimul. 2010;3(3):161–9. Epub 2010/07/17.
Koeppen AH. The pathogenesis of spinocerebellar ataxia. Cerebellum. 2005;4(1):62–73. Epub 2005/05/18.
Rub U, de Vos RA, Schultz C, Brunt ER, Paulson H, Braak H. Spinocerebellar ataxia type 3 (Machado-Joseph disease): severe destruction of the lateral reticular nucleus. Brain. 2002;125(Pt 9):2115–24. Epub 2002/08/17.
Evert BO, Wullner U, Schulz JB, Weller M, Groscurth P, Trottier Y, et al. High level expression of expanded full-length ataxin-3 in vitro causes cell death and formation of intranuclear inclusions in neuronal cells. Hum Mol Genet. 1999;8(7):1169–76. Epub 1999/06/17.
Durr A, Stevanin G, Cancel G, Duyckaerts C, Abbas N, Didierjean O, et al. Spinocerebellar ataxia 3 and Machado-Joseph disease: clinical, molecular, and neuropathological features. Ann Neurol. 1996;39(4):490–9. Epub 1996/04/01.
Bettencourt C, Lima M. Machado-Joseph Disease: from first descriptions to new perspectives. Orphanet J Rare Dis. 2011;6(35). Epub 2011/06/04.
Zee DS, Yamazaki A, Butler PH, Gucer G. Effects of ablation of flocculus and paraflocculus of eye movements in primate. J Neurophysiol. 1981;46(4):878–99. Epub 1981/10/01.
Shin M, Moghadam SH, Sekirnjak C, Bagnall MW, Kolkman KE, Jacobs R, et al. Multiple types of cerebellar target neurons and their circuitry in the vestibulo-ocular reflex. J Neurosci. 2011;31(30):10776–86. Epub 2011/07/29.
Schmahmann JD. The role of the cerebellum in cognition and emotion: personal reflections since 1982 on the dysmetria of thought hypothesis, and its historical evolution from theory to therapy. Neuropsychol Rev. 2010;20(3):236–60. Epub 2010/09/08.
Schmahmann JD, Pandya DN. The cerebrocerebellar system. Int Rev Neurobiol. 1997;41:31–60. Epub 1997/01/01.
Stoodley CJ, Schmahmann JD. Evidence for topographic organization in the cerebellum of motor control versus cognitive and affective processing. Cortex J Devoted Study Nerv Syst Behav. 2010;46(7):831–44. Epub 2010/02/16.
Oliveri M, Torriero S, Koch G, Salerno S, Petrosini L, Caltagirone C. The role of transcranial magnetic stimulation in the study of cerebellar cognitive function. Cerebellum. 2007;6(1):95–101. Epub 2007/03/17.
Schutter DJ, van Honk J. An electrophysiological link between the cerebellum, cognition and emotion: frontal theta EEG activity to single-pulse cerebellar TMS. NeuroImage. 2006;33(4):1227–31. Epub 2006/10/07.
Granziera C, Schmahmann JD, Hadjikhani N, Meyer H, Meuli R, Wedeen V, et al. Diffusion spectrum imaging shows the structural basis of functional cerebellar circuits in the human cerebellum in vivo. PLoS One. 2009;4(4):e5101. Epub 2009/04/03.
Stoodley CJ, Valera EM, Schmahmann JD. Functional topography of the cerebellum for motor and cognitive tasks: an fMRI study. NeuroImage. 2012;59(2):1560–70. Epub 2011/09/13.
Acknowledgments
FF was supported by Canadian Institute of Health Research (CIHR) fellowship award (201102MFE-246635-181538). This study was supported in part by the Harvard-Thorndike Clinical Research Center at Beth Israel Deaconess Medical Center integrated in the Harvard Clinical and Translational Science Center (grants M01-RR-01066 and UL1 RR025758 from the National Center for Research Resources, National Institutes of Health). YW was supported by Bolsas de Viaje Esteban Martino of Fundacion Marques de Valdecilla (BEM 13/11) and would like to thank Dr. José Luis Fernández Torre for his scientific contribution. BM was supported by a KL2 Medical Research Investigator Training (MeRIT) award (1KL2RR025757-04) from Harvard Catalyst. This work was also in part supported by Sidney Baer Foundation.
Conflict of Interests
FF, YW, BM, EA, ML, VN and PG have no conflict of interest to disclose. APL serves on the scientific advisory boards for Nexstim, Neuronix, starlab Neuroscience, Neosync, and Novavision, and is an inventor on patents and patent applications related to noninvasive brain stimulation and real-time integration of TMS with EEG and fMRI.
Author information
Authors and Affiliations
Corresponding author
Additional information
Faranak Farzan and Yunfen Wu contributed equally to this work.
Rights and permissions
About this article
Cite this article
Farzan, F., Wu, Y., Manor, B. et al. Cerebellar TMS in Treatment of a Patient with Cerebellar Ataxia: Evidence from Clinical, Biomechanics and Neurophysiological Assessments. Cerebellum 12, 707–712 (2013). https://doi.org/10.1007/s12311-013-0485-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12311-013-0485-8