Abstract
Purpose
Avascular necrosis (AVN) of the humeral head is a devastating complication of proximal humeral fracture (PHF) that often results in long-term morbidity for the patient. Rates of AVN depend on the number of fracture fragments and are highly variable. The literature suggests that timely stable and anatomic reduction may decrease the rate at which AVN develops after PHF. To our knowledge, there is no literature published investigating a temporal relationship between the timing of PHF fixation and rates of AVN.
Methods
Operative records of one orthopedic trauma surgeon were used to identify patients that underwent open reduction internal fixation for PHF at our institution between 2007 and 2012. Radiographs at presentation were reviewed and used to classify the fractures into two, three or four parts. Date and time of the initial radiograph were recorded as were the date and time of available intra-operative fluoroscopic images. The time from presentation radiograph to operative fixation was calculated (hours). Available follow-up plain films were then reviewed and evaluated for the presence or absence of humeral head AVN.
Results
Time to surgery (less than or greater than 72 h) and patient age did not correlate with development of AVN after PHF (p > 0.26). Notably, the number of fracture fragments did influence the rate of AVN identified in patients with PHF (p = 0.002).
Conclusion
Early operative intervention does not appear to decrease the rate of development of avascular necrosis after PHF.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Proximal humerus fractures (PHFs) are common, comprising 4–5 % of all fractures presenting for medical evaluation [1]. The minority of these fractures are displaced, and it is this subgroup most at risk for complications [2].
Avascular necrosis (AVN) is a devastating complication of PHF. Development of this complication correlates with displacement and the number of parts created by the fracture lines (as described by Neer) and can range from 3 to 90 % [2, 3]. Patients who develop this complication can face significant long-term disability and few reliable surgical options for treatment [2–6].
A number of risk factors for the development of post-traumatic AVN have been previously reported in the literature. Risk factors include the number of fracture fragments and the degree of fracture fragment displacement [2, 6–8]. These authors have also postulated that operative stabilization promotes revascularization of the humeral head [7, 9].
Traumatic femoral neck fractures in young individuals are treated urgently to reduce the rate of AVN development [10]. Both the femoral head and humeral head are vascularized by retrograde flow, and therefore, a similar relationship between time to open reduction internal fixation (ORIF) and the development of AVN may exist [1, 2].
Presently, there is no literature available describing the relationship between time to ORIF and development of AVN in PHFs. The purpose of this study was to investigate whether time to operative fixation influences incidence of AVN in PHFs.
Patients and methods
Ethics board approval was obtained prior to the commencement of this study. Operative records from one orthopedic surgeon at our institution identified twenty-two patients who underwent ORIF for PHF between 2007 and 2012. Three patients who were treated with ORIF for a nonunion were excluded. ORIF was completed using a combination of the deltopectoral and lateral approaches with fixation achieved using the 3.5-mm LCP proximal humeral plate (Synthes; West Chester, Pennsylvania, USA).
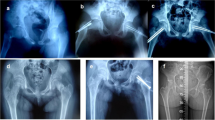
Nineteen patients’ files representing acute PHF were reviewed, and initial (presentation) radiographs and adjuncts (computed tomography (CT) scans, if available) were used to classify the fracture as either two, three or four parts. There were seven two-part, ten three-part and two four-part fractures identified (mode of three parts). The date and time of the initial radiograph and the date and time of intra-operative fluoroscopic images were recorded. Time (hours) between presentation and fixation was then calculated. Determination of time from injury to fixation was not possible based on information available within the patient charts, and therefore, time from presentation to ORIF was used as a surrogate measure. Patients were then divided into less than and greater than 72 h to ORIF to facilitate statistical analysis of the data. On review of the data available in this study, the 72-h mark was an easily identifiable division that permitted sufficient sample size in each group (early versus late ORIF) to facilitate statistical analysis. Final radiographic follow-up films on each patient were then reviewed for the presence or absence of AVN (Table 1).
SPSS 12.0 (SPSS, Chicago, Illinois, 2004) software was used to complete statistical analyses in the form of a binary logistic regression.
Results
Five patients (two two-part and three three-part PHFs, no four-part or four-part valgus-impacted) underwent ORIF within 72 h of presentation (10–51 h; 28 ± 17 h). The mean age of these patients was 53 (range 40–67 years). Follow-up ranged between 90 and 1522 days (729 ± 490 days).
Fourteen patients (five two-part, seven three-part, two four-part displaced, no four-part valgus-impacted PHFs) underwent ORIF 72 h or more after presentation (79–1193 h; 1509 ± 3248 h). The mean age of these patients was 56 (range 19–77 years). Follow-up ranged between 54 and 1249 days (558 ± 387 days).
It should be noted that the groups did not differ significantly in ages as identified by an unpaired Student t test (p = 0.342).
One patient (three-part PHF) treated within 72 h of presentation developed AVN. Two patients (both four-part PHFs) treated after 72 h from presentation developed AVN.
A binary logistic regression analysis was used to determine which variables influenced rate of development of AVN. Only fracture type (two, three or four parts) correlated significantly with the rate of development of AVN (p = 0.002). Time to surgery (either greater or less than 72 h) and age did not correlate significantly with the rate of development of AVN (p > 0.26).
Discussion
PHFs comprise a significant portion (5 %) of traumatic injuries treated by orthopedic surgeons [1]. Complications such as AVN are not uncommon with rates as high as 90 % reported for severe four-part fractures [3].
Established risk factors exist for the development of AVN after fracture. The number and displacement of PHF fragments correlate with rates of AVN [2, 6–8]. Hertel developed predictive criteria for the development of AVN through investigation of one hundred PHFs [7]. Integrity of the medial calcar (lengths < 8 mm) and disruption of the medial hinge most predictably correlated with progression to AVN after fracture [7]. Additionally, Spross et al. [11] found a correlation between fracture dislocations and increased incidence of AVN of the proximal humerus.
The humeral head articular surface has a tenuous blood supply [1, 2]. The arcuate branch of the anterior humeral circumflex artery provides a significant proportion of the flow to the humeral head articular surface in a retrograde fashion. This is akin to the lateral epiphyseal branch of the medial femoral circumflex artery that supplies the femoral head [1, 2]. A temporal relationship between time to ORIF of displaced femoral neck fractures and development of AVN has been established. It follows that the same could be true for the proximal humerus and therefore a shorter time to ORIF may correlate with a smaller incidence of AVN in these fractures.
Several authors have postulated that stable internal fixation promotes revascularization of the humeral head after fracture [7, 9]. Early stabilization of these fractures could therefore be expected to reduce ischemic time for the humeral head and perhaps the rate of AVN.
Impairment resulting from AVN is well documented in the literature, notably chronic pain, severely limited range of motion and poor overall function [2, 6]. Treatment options for young, high-demand patients are limited and outcomes are unreliable; as such, these patients are generally not considered suitable for prosthetic replacement [1, 12–14]. End-stage AVN of the proximal humerus in elderly, low-demand individuals can be treated successfully with hemiarthroplasty; however, hemiarthroplasty for AVN after ORIF is less successful that if hemiarthroplasty is performed as the primary procedure [8, 15]. Identifying those factors that increase the risk of AVN, therefore, is an important pursuit for patients across the age spectrum. At present, there are no studies in the literature that document effective preventative strategies to reduce the incidence of AVN in this population.
The purpose of this study was to investigate the role of time to ORIF in the development of AVN in two-, three- and four-part PHFs. No correlation between time to surgery, either early (less than 72 h) or late (greater than 72 h), and incidence of AVN was identified in the small population studied. However, this study does support the body of evidence correlating the number of fracture fragments with the incidence of AVN.
One explanation for the lack of correlation between time to ORIF and incidence of AVN in PHFs (unlike in the proximal femur) is the number of vessels supplying the humeral head. Apart from the arcuate artery, the humeral head is also supplied by the posterior humeral circumflex and vessels from the greater tuberosity, lesser tuberosity and proximal humeral metaphysis [1, 2]. Parallels for these collateral vessels do not exist in the proximal femur [16].
Of note, this study lends support to the notion that PHFs are not emergent orthopedic cases and as such can be safely performed under semi-elective conditions with a well-rested team versed in the appropriate equipment required. In the era of increasing awareness of surgeon fatigue and related patient complications, such literature is valuable in the determination of after-hours operating room time allocation [17].
Limitations of this study include small sample size (and, therefore, small number of AVN complications) which reduces the available power to detect a correlation between time to ORIF and incidence of AVN. Furthermore, stage one of AVN (according to Cruss) is not detectable on plain film, and as such, the number of cases of AVN identified may underrepresent the true incidence of AVN in this population [13]. Finally, radiographic follow-up varied from 54 to 8627 days; those patients with only short-term follow-up may have developed AVN after final follow-up as reported previously in the literature [8, 18, 19].
Future studies investigating a relationship between time to ORIF for PHFs and incidence of AVN would benefit from a larger sample size and longer follow-up interval. Confirmation of the results presented would certainly contribute to the argument for elective (versus emergent) ORIF of PHFs.
References
Cadet E, Ahmad C (2012) Hemiarthroplasty for three- and four-part proximal humerus fractures. J Am Acad Orthop Surg 20(1):17–27
Schlegel TF, Hawkins RJ (1994) Displaced proximal humeral fractures: evaluation and treatment. J Am Acad Orthop Surg 2:54–66
Neer CS (1970) Displaced proximal humera fractures. II. Treatment of three-part and four-part displacement. J Bone Jt Surg Am 52(6):1090–1103
Carter M, Mikuls T, Nayak S, Fehringer E, Michaud K (2012) Impact of total shoulder arthroplasty on generic and shoulder-specific health-related quality-of-life measures: a systematic literature review and meta-analysis. J Bone Jt Surg Am. 94(17):e127
Besch L, Daniels-Wredenhagen M, Mueller M, Varoga D, Hilgert R-E, Seekamp A (2009) Hemiarthroplasty of the shoulder after four-part fracture of the humeral head: a long-term analysis of 34 cases. J Trauma 66(1):211–214
Gerber C, Hersche O, Berberat C (1998) The clinical relevance of posttraumatic avascular necrosis of the humeral head. J Shoulder Elb Surg. 7(6):586–590
Hertel R, Hempfing A, Stiehler M, Leunig M (2004) Predictors of humeral head ischemia after intracapsular fracture of the proximal humerus. J Shoulder Elb Surg. 13(4):427–433
Harrison AK, Gruson KI, Zmistowski B, Keener J, Galatz L, Williams G et al. (2012) Intermediate outcomes following percutaneous fixation of proximal humeral fractures. J Bone Jt Surg Am 94-A(13):1223–1228
Wijgman A, Roolker W, Patt T, Raaymakers E, Marti R (2002) Open reduction and internal fixation of three and four-part fractures of the proximal part of the humerus. J Bone Jt Surg Am 84-S(11):1919–1925
Browner B, Jupiter J, Levine A, Trafton P, Krettek C (eds) (2008) Skeletal trauma: basic science, management and reconstruction, 4th edn. W.B. Saunders Company, Philadelphia
Spross C, Platz A, Rufibach K, Lattmann T, Forberger J, Dietrich M (2012) The PHILOS plate for proximal humeral fractures—risk factors for complications at one year. J Trauma Acute Care Surg. 72(3):783–792
Soliman OA, Koptan WMT (2013) Four-part fracture dislocations of the proximal humerus in young adults: results of fixation. Int J Care Inj 44(4):442–7
Cushner MA, Friedman RJ (1997) Osteonecrosis of the humeral head. J Am Acad Orthop Surg 5(6):339–346
Mouradian WH (1986) Displaced proximal humerus fractures: seven years’ experience with a modified Zickel supracondylar device. Clin Orthop Relat Res 212:209–218
Tauber M, Karpik S, Matis N, Schwartz M, Resch H (2007) Shoulder arthroplasty for traumatic avascular necrosis. Clin Orthop Relat Res 465:208–214
Grose AW, Gardner MJ, Sussmann PS, Helfet DL, Lorich DG (2008) The surgical anatomy of the blood supply to the femoral head: description of the anastomosis between the medial femoral circumflex and inferior gluteal arteries at the hip. J Bone Joint Surg Br 90(10):1298–1303
Ricci WM, Gallagher B, Brandt A, Schwappach J, Tucker M, Leighton R (2009) Is after-hours orthopaedic surgery associated with adverse outcomes? A prospective comparative study. J Bone Joint Surg Am 91(9):2067–2072
Lee CK, Hansen HR (1981) Post-traumatic avascular necrosis of the humeral head in displaced proximal humeral fractures. J Trauma 21(9):788–791
Greiner S, Kaab M, Haas N, Bail H (2009) Humeral head necrosis rate at mid-term follow-up after open reduction and angular stable plate fixation for proximal humeral fractures. Inj Int J Care Inj. 40:186–191
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No author has declared conflict of interest related to the enclosed manuscript.
Rights and permissions
About this article
Cite this article
Archer, L.A., Furey, A. Rate of avascular necrosis and time to surgery in proximal humerus fractures. Musculoskelet Surg 100, 213–216 (2016). https://doi.org/10.1007/s12306-016-0425-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12306-016-0425-0