Abstract
Aim
This retrospective study aimed to evaluate surgical outcomes and identify influential factors in pediatric femoral neck fractures.
Materials and methods
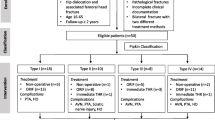
A total of 25 hips from 23 pediatric patients who underwent surgical intervention for femoral neck fractures were included. Data encompassing patient demographics, fracture types, surgical techniques, complications, and follow-up outcomes were analyzed retrospectively. Factors such as fracture displacement, timing of surgery, fixation methods, and reduction quality were assessed concerning postoperative complications.
Results
Falling from a height accounted for 48% of the trauma mechanisms, and avascular necrosis (AVN) was the most prevalent complication (4 hips). Although fracture displacement, bad reduction quality, and delayed surgery were more common among complicated cases, statistical significance was not attained. The study noted an association between presence of avascular necrosis and worse clinical results(rho: 0.428, p: 0.05, CI: 95%).
Conclusion
Surgical treatment yielded favorable clinical outcomes; however, limitations due to the study’s retrospective design, limited sample size, and single-center approach underscore the necessity for larger multicenter studies. Our findings emphasize the need for comprehensive investigations to better understand and manage pediatric femoral neck fractures, especially regarding factors influencing AVN and long-term outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Femoral neck fractures, though relatively rare in the pediatric age group, pose distinct challenges in their management. Comprising merely 1% of all fractures in this demographic [1]. these fractures in children differ significantly from those in elderly patients, commonly resulting from high-energy trauma at an incidence rate of 80–90%, often accompanied by additional traumas [2, 3]. The uniqueness of these fractures in pediatric patients underscores the need for specialized considerations and a comprehensive understanding of the associated complications.
Complications associated with femoral neck fractures in pediatric patients encompass a spectrum of challenges, including avascular necrosis (AVN), coxa vara, delayed union, nonunion, early physeal arrest, and, albeit rarely, infection [3,4,5]. Such complications not only influence the immediate post-injury period but also have implications for the long-term musculoskeletal health and overall well-being of the pediatric patient. Understanding the factors influencing the outcomes of pediatric femoral neck fractures is pivotal for optimizing treatment strategies, enhancing recovery trajectories, and minimizing the risk of complications. However literature lacks on detailed studies including large patient cohors. The scarcity of comprehensive studies addressing the treatment of pediatric proximal femur fractures underscores the urgent need for in-depth research in this domain. Despite the relatively infrequent occurrence of these fractures in the pediatric population, their unique characteristics and complexities necessitate focused investigation. Existing literature reveals a significant gap in our understanding of optimal treatment modalities, long-term outcomes, and factors influencing prognosis in this specific patient demographic [6]. The rarity of manuscripts exploring the nuances of pediatric proximal femur fractures leaves clinicians with limited evidence-based guidelines, highlighting the importance of dedicated research efforts. A more thorough exploration of this area is essential not only for expanding the knowledge base within orthopedics but also for refining clinical practices, ultimately leading to improved treatment protocols and enhanced outcomes for young patients facing these challenging fractures [7].
In light of these considerations, this study seeks to delve into the intricacies of femoral neck fractures in the pediatric age group, particularly focusing on evaluating both the clinical and radiological outcomes of patients who sought treatment at our clinic.
Material and method
After obtaining the ethics committee approval (B.10.1.TKH.4.34.H.GP.0.01/336), the files of patients with pediatric femoral neck fracture who were operated in the same institution between 2010–2022 were retrospectively reviewed. This study was conducted in accordance with principles for human experimentation as defined in the Declaration of Helsinki. Informed consent was obtained from all individuals prior to surgery.
The inclusion criteria were as follows: Patients younger than 15 years of age presenting with traumatic femoral neck fractures and treated surgically, with complete medical records including radiographic images and at least 12 months of follow-up data. Exclusion criteria consisted of the following: having a metabolic bone disease, presenting after a week and/or receiving conservative treatment, undergoing surgery due to complications from a previous surgical procedure, having surgery for a peri-implant fracture, and inadequate medical data with less than 12 months of follow-up. The choice of implant and surgical technique was at the discretion of the operating surgeon. All surgeries were performed by one of thirteen orthopedic trauma surgeons or under the supervision of these surgeons by twelve senior residents.
Health Information Systems (HIS V5), a digital web service, served as the primary resource for acquiring and reviewing patient follow-up data. The evaluation of X-rays involved both authors assessing angular measurements and union time through the employment of the Picture Archive and Communication System (PACS). Any discrepancies were resolved through consensus during discussions between the two senior authors. Each patient's profile included analysis of age, sex, trauma pattern, affected side, presence of associated fractures, fracture characteristics, reduction features, duration between trauma and surgery, type of surgical technique (closed or open reduction), follow-up duration, time to union, identification of complications such as malunion, nonunion, and avascular necrosis (AVN), necessity for implant removal, clinical well-being grading, and radiological alignment during the last follow-up.
The duration between the trauma occurrence and the surgical intervention was assessed by categorizing patients into two groups: those undergoing surgery within the initial 12 h and those operated on more than 12 h later. For fracture classification, the Delbet classification modified by Colonna was employed [2]. Type 1 fractures constituted transepiphyseal fractures, Type 2 fractures were identified as transcervical, Type 3 fractures were categorized as cervicotrochanteric, and Type 4 fractures were extracapsular intertrochanteric fractures. Additionally, the Garden classification was utilized to determine the extent of preoperative displacement [8]. Grade 1 referred to incomplete, nondisplaced fractures, while grade 4 indicated totally displaced fractures. The Ratliff classification facilitated both clinical and radiological evaluations [3]. Patients' clinical well-being was graded as good, moderate, or poor based on factors such as hip range of motion, femoral head sphericity, and the patient's activity level. Avascular necrosis (AVN) detected in the last follow-up radiographs was graded from grade 1 to 3 according to this classification. Furthermore, patients with premature physeal closure were considered as a distinct entity. The postoperative quality of reduction was categorized as good or poor based on the alignment of the femoral neck. Poor alignment was defined as displacement exceeding 5 mm and/or 10º in any plane [9].
Surgery is promptly scheduled upon our patients' arrival at the emergency department, aiming to keep the interval under 12 h. However, due to the high-energy trauma mechanisms involved, the timing of surgery may vary. It could be influenced by observations made by other clinics or due to additional injuries suffered by the patients. Consequently, in some cases, the surgical procedure was conducted beyond the 12-h threshold. Patients underwent surgery either employing an anterior open technique, necessitated by failed closed reduction, or through a closed reduction method. The fixation process utilized a varied assortment of cannulated 4.0 mm and 6.5 mm screws, plates, or K-wires, depending on the fracture type and the surgeon's preference.
All patients underwent follow-up visits at 2, 6, and 10 weeks, as well as at the 3rd, 6th, 12th, and 24th months following surgery. Throughout this period, patients were stabilized with a spica splint, supporting the injured hip for a duration of 4 weeks. Fractures stabilized with K-wires tended to be monitored using spica casts until evidence of union was observed on X-rays. Weight-bearing was permitted upon achieving full clinical union. Full union was deemed attained when patients experienced no hip pain during range of motion tests and weight-bearing, and when there was no evidence of fracture reduction failure after a minimum of 6 weeks of follow-up.
Statistical analyses
Data were analyzed using SPSS software (ver. 22.0; IBM Corp., Armonk, NY, USA). The Chi-square test was used to assess the qualitative parameters. Spearman's correlation coefficient (ρ) was employed to assess the relationship between quantitative variables, while Pearson's correlation coefficient (ρ) was utilized to evaluate associations among categorical variables. A value of ρ (ρ) = 1 signifies a perfect positive correlation, whereas a value of ρ (ρ) = -1 indicates a perfect negative correlation..Quantitative variables are expressed as mean ± standard deviation and minimum and maximum values. Qualitative variables are expressed as frequencies or ratios. P-values < 0.05 were considered to indicate statistical significance.
Results
Between the enrollment dates, a total of 29 hips in 27 patients underwent surgery. Four hips from four patients were excluded from the study: one due to metabolic bone disease, one due to a pathological fracture, and two due to poor follow-up. Consequently, the study included 25 hips from 23 patients. Notably, two patients experienced bilateral femoral neck fractures simultaneously at the time of trauma. The mean age of our patients was 10.8 years (range: 4–15 years), comprising 17 male (%74) and 6 female (%26) patients. Among the included hips, 9 were right-sided, and 16 were left-sided. Falling from a height was the most common trauma mechanism, accounting for 48% of cases. The mean follow-up duration for our patients was 45 months (Table 1).
Among our patients, additional injuries were identified in 5 cases (%22): pelvis fracture in one patient; lung contusion with calcaneus fracture in another patient; lung contusion with supracondylar humerus fracture in one patient; acromioclavicular joint injury in one patient; and in one patient, distal humerus and forearm fractures were present along with a pelvis fracture.
Surgical treatment was conducted within the first 12 h for 11 patients (%44) included in our study, while surgical intervention for the remaining 14 patients (%56) occurred after the initial 12-h timeframe. 8 cases (%32) necessitated an open reduction, whereas closed reduction was performed in 17 patients (%68) (Table 2). Screws were utilized as the fixation method in 23 hips (92%) following reduction: 1 screw and 1 K-wire in 1 case (4%), 2 screws in 5 cases (20%), and 3 screws in 17 cases (68%). Plate fixation was applied in 1 patient (4%), while fixation with 2 K-wires was employed in another patient (4%). Patients who underwent a successful closed reduction did not require intracapsular hematoma evacuation.
Out of the total hips, 19 (76%) did not experience any complications, while various complications were observed in 6 hips (24%) (Table 2). These included avascular necrosis (AVN), screw head fracture during the removal of fixation material, revision surgeries due to loss of reduction and nonunion. Notably, the hip that underwent reduction loss was stabilized with 1 K-wire and 1 cannulated screw following closed reduction. It also happened to be the other hip of the same patient that faced nonunion. Postoperatively, the right hip exhibited poor reduction quality, while the left hip showed good reduction quality according to Ratliff's assessment. The patient with a 3 cm shortening is leading a satisfactory life and has declined further surgical intervention (Fig. 1).
Case 17 depicts the only patient treated using K-wires with closed reduction. a The case involves a 10-year-old girl who suffered Type 2 fracture on the right and Type 3 fracture on the left femur neck after being hit by a car as a pedestrian. b Initial surgery occurred at the 3rd hour post-trauma, employing K-wires for the left side and a hybrid method for the right fracture. Loss of reduction on the right side was observed at the 2nd week after surgery. c Subsequent revision on the right side involved K-wire application following reduction loss. d By the 4th postoperative month, union was achieved on the right side while nonunion persisted on the left hip. e The left side underwent open reduction, autologous bone grafting, and fixation with two 4.0 mm cannulated screws using an anterior approach. f Full union was achieved on the right side, but premature physeal closure resulted in 3 cm shortening on the left side by the 11th postoperative year
Specifically, AVN types were categorized as follows: Type 1 AVN occurred in 1 hip, Type 2 AVN in 2 hips, and Type 3 AVN in 1 hip. Furthermore, premature physeal closure leading to a 3 cm shortening ensued in the hip that underwent open grafting and screw fixation eight months post-trauma due to nonunion. The patient with Type 1 AVN, aged 13, had a Delbet Type 1 fracture (traumatic slipped capital femoral epiphysis) and a Garden Type 4 displaced fracture resulting from a traffic accident. The patient arrived from an external center on the 3rd day and underwent surgery upon arrival. Despite achieving good postoperative reduction, this patient developed AVN with diffuse epiphyseal involvement (Table 2).
Based on Rattlif's clinical and radiological assessments, 80% of patients (20 hips) achieved good results, while 8% (2 hips) showed moderate results, and 12% (3 hips) exhibited poor outcomes. Throughout the patients' follow-up, complications other than AVN emerged, including screw head fracture during screw removal in one patient, revision due to reduction loss in one hip, and revision due to nonunion in another hip. A total of 18 hips (%72) experienced recovery without any complications. The average time for fracture union was 12.5 weeks (Table 2).
There was no observed statistical correlation between the extent of fracture displacement and complications (p = 0.905). The highest complication rate of 28.6% was evident in Garden Type 4 fractures. As per the Delbet classification, no statistically significant relationship was discerned between fracture type and complications (p = 0.33). However, the complication rate was 50% higher in Delbet Type 1 fractures. Likewise, no statistically significant correlation was found between the timing of the operation and complications (p = 0.734) (Table 3).
Upon examining the relationship between open-closed reduction, the number of screws, K-wires, and complications, no statistically significant difference was observed (p = 0.13). Furthermore, investigating the relationship between Ratliff's clinical evaluation scores and the occurrence of complications revealed a statistically moderate and mild correlation in patients within the Ratliff moderate and bad groups (rho: 0.428, p: 0.05, CI: 95%).
Discussion
In this study, we evaluate the outcomes of surgical treatments for pediatric femur neck fractures and the various influential factors affecting these results. Our cohort comprised 23 patients (25 hips), where surgical interventions were administered for fixation of fractures. Noteworthy observations include bilateral femur neck fractures in two patients following trauma and a mean patient age of 10.8 years (range: 4–15 years), predominantly male (17) (%74) with 6 female (%26) patients. The most frequent trauma mechanism identified was falling from a height, occurring in 48% of cases. Additional injuries were present in 5 cases (%22), ranging from pelvis fractures to lung contusions and supracondylar humerus fractures. Surgical intervention within the initial 12 h was executed for 11 patients (%44), while the remaining 14 (%56) underwent surgery post the 12-h timeframe. Complications such as avascular necrosis, screw head fractures, and revisions due to reduction loss or nonunion were identified in 7 hips (%28). Our study did not reveal any significant correlations between fracture types, timing of surgery, methods of reduction, and the presence of complications, thus making it challenging to determine their impact on the final outcomes. However, patients experiencing AVN, nonunion, and premature physeal closure tended to exhibit poorer clinical results.
In our study, femoral neck fractures among pediatric patients were notably infrequent, aligning with findings in the literature. However, the number of hips included in the study was relatively high compared to the limited numbers reported in previous studies. Typically, these fractures occur more commonly between the ages of 10 and 13, with our study indicating a mean age of 10.8 years [3, 10, 11]. Unlike adult cases, high-energy trauma often precipitates pediatric femoral neck fractures, as observed in our study where falling from a height accounted for 48% of cases [12, 13]. In contrast, only two patients in our study suffered femoral neck fractures due to low-energy trauma. The peculiar blood flow in the femoral neck of children makes it particularly vulnerable to damage during hip fractures, rendering AVN a prevalent complication, often posing a high risk of femoral head collapse within the initial year [13, 14]. Similarly, AVN emerged as the most frequent complication in our study.
Several factors, including fracture location according to the Delbet classification and the degree of displacement based on the Garden classification, have been linked to AVN rates in literature [15, 16]. However, our study failed to establish a statistically significant correlation between fracture displacement, location, and complications. The highest complication rate observed in our study was in Garden Type 4 fractures, indicating a 50% higher complication rate in Delbet Type 1 fractures. Consistent with Ratliff's assertion, our study also indicated that patients experiencing AVN often had moderate to poor outcomes [3]. Intriguingly, Leung and Lam suggested substantial changes in clinical and radiological results over a few years for pediatric femoral neck fractures [17]. Notably, in our study, a patient who underwent bilateral femoral neck fracture surgery experienced reduction loss in one hip and nonunion in the other. Although AVN wasn't detected in the affected hip, premature physeal closure was evident in the latter. Despite this, the Ratlif assessment categorized the patient's follow-up results as good, with the patient opting against further surgery.
Numerous factors are associated with AVN development, such as patient age, vessel damage during trauma, fracture location, and displacement degree. Moon et al.'s meta-analysis and Pandey et al.'s findings emphasize fracture type and patient age as key AVN risk factors [3,4,5, 16, 18, 19]. However, conflicting reports exist, with some studies demonstrating positive outcomes and low AVN rates in displaced fractures [20, 21]. Moreover, the risk of AVN appears to increase with age, as indicated by Mitchell et al. and corroborated in our study [18, 22].
Early surgical intervention within the first 12 h has been suggested to reduce AVN risk [7]. yet controversy persists regarding the precise benefit of expedited surgery [13]. While several studies advocate for early surgical intervention, others emphasize the significance of direct trauma-induced vessel damage as the primary factor in AVN development [3, 6, 18].While Ratliff et al. discourage surgery at midnight, as no clear advantages have been established, Bukwa et al. argue in favor of emergency surgery within 12 h to mitigate AVN chances [3, 7]. Pandey et al. suggested early surgical intervention as logistically feasible, albeit controversial in benefitting clinical outcomes [13]. Similarly, our clinic aims for surgery within the first 12 h, prioritizing cases that stay overnight as the first surgeries the next day.
Regarding reduction techniques, closed reduction attempts, followed by open reduction if necessary, have been recommended [4, 20, 23]. Correspondingly, our clinic employs similar procedures, resorting to open reduction for unreduced fractures. Notably, 17 patients underwent closed reduction, while 8 had fixation post-open reduction in our study. The role of decompression, specifically capsulotomy or joint aspiration, in AVN remains debatable. While some studies indicate better outcomes with open reduction and decompression, others show no notable difference in AVN rates with or without capsulotomy [21, 23,24,25]. There are also studies that did not detect any difference in the rate of osteonecrosis with or without capsultomy [4, 6, 26]. In our series, intracapsular hematoma drainage wasn't conducted in any patients subjected to closed reduction. Thus, it is impossible to discuss the benefit of decompression in our series.
Selection of implant type in pediatric femoral neck fractures lacks consensus, with studies suggesting individualized choices based on factors like age, BMI, and fracture type [13]. Similarly, our fixation methods primarily used cannulated screws, with variations in some cases using k-wires or plate and screw implants. However, we do not recommend or use K wires solely for fixation as a stable fixation can not be obtained with K wires. It is noteworthy that osteosynthesis solely employing K-wires, or coupled with essential supplementary immobilization, is not advocated based on contemporary insights. Furthermore, contemporary literature strongly advocates for anatomical reduction and stable fixation [27].
Premature physeal closure's wide-ranging reported incidence in the literature (20% to 62%) echoes the uncertainty surrounding this complication [3, 11, 17, 28]. In our study, one patient experienced premature physeal closure, resulting in 3 cm shortening, yet Rattlif's assessment deemed the patient's results satisfactory without requiring further surgery.
While postoperative infections in pediatric hip fractures are rare, constituting up to 5.2% of cases in literature, our study didn't encounter any infections [17, 28, 29].
The timing of implant removal remains unclear, with suggestions ranging from adequate union after 12 to 22 months of fixation to cautionary notes about associated risks, such as screw site fractures [21, 30,31,32]. In our study, 12 patients had their fixation materials removed, with one patient encountering a screw head fracture during the removal procedure. None of our patients experienced screw site fractures after fixative material removal.
Our study showcased a mean union time of 12.5 weeks, with only one patient achieving union after 12 months. Surgical treatment emerges as a significant factor in achieving favorable clinical outcomes for these fracture cases, yet more extensive multicenter studies are essential due to the rarity of pediatric femoral neck fractures. The limited data in literature emphasize the need for robust studies to unravel the intricacies of these fractures.
Several limitations should be considered in interpreting our study findings. Firstly, our study's retrospective nature and single-center design may limit the generalizability of the results to broader populations. The relatively small sample size and the rarity of pediatric femoral neck fractures constrained the statistical power, potentially impacting the identification of significant associations. Furthermore, despite efforts to encompass various factors, there might exist unmeasured or unexplored variables that could influence fracture outcomes. These limitations advocate for further multicenter prospective studies with larger cohorts to validate and expand upon our observations.
Conclussion
Surgical intervention plays a crucial role in achieving favorable clinical outcomes for these patients despite the potential for complications. Although statistical evidence was lacking, complications seemed to correlate with factors such as the extent of fracture displacement, inadequate reduction, and delayed surgical procedures. Thus, we recommend obtaining anatomical reduction and stable fixation, even if the results shown do not support this in a relatively small number of cases. Osteosynthesis using only K-wires or with necessary additional immobilization is not recommended according to current knowledge. Considering the rarity of pediatric femoral neck fractures, even at our major trauma center, accessing a substantial number of patients for 10-year follow-ups remains a challenge. Hence, conducting multicenter studies becomes imperative to garner more comprehensive insights into these fractures.
Data availability
The data is available if requested directly from corresponding author.
References
Beaty JH. Fractures of the hip in children. Orthop Clin North Am. 2006;37(2):223–32. https://doi.org/10.1016/j.ocl.2005.11.003.
Colonna PC. Fractures of the neck of the femur in children. Am J Surg. 1928;6:793. https://doi.org/10.1016/S0002-9610(29)90726-1.
Ratlif AH. Fractures of the neck of the femur in children. J Bone Joint Surg Br. 1962;44–B:528–42. https://doi.org/10.1302/0301-620X.44B3.528.
Spence D, DiMauro JP, Miller PE, Glotzbecker MP, Hedequist DJ, Shore BJ. Osteonecrosis after femoral Neck fractures in children and adolescents: analysis of risk factors. J Pediatr Orthop. 2016;36(2):111–6. https://doi.org/10.1097/BPO.0000000000000424.
Morsy HA. Complications of fracture of the neck of the femur in children. A long-term follow-up study. Injury. 2001;32(1):45–51. https://doi.org/10.1016/s0020-1383(00)00109-1.
Inan U, Köse N, Omeroğlu H. Pediatric femur neck fractures: a retrospective analysis of 39 hips. J Child Orthop. 2009;3(4):259–64. https://doi.org/10.1007/s11832-009-0180-y.
Bukva B, Abramović D, Vrgoč G, Marinović M, Bakota B, Dučić S, Miškulin M, Brdar R, Čoklo M, Gulan G. Femoral neck fractures in children and the role of early hip decompression in final outcome. Injury. 2015;Suppl 6:S44-7. https://doi.org/10.1016/j.injury.2015.10.059.
Garden R. Low-angle fixation in fractures of the femoral neck. J Bone Joint Surg Br. 1961;43:647–63.
Dhar SA, Ali MF, Dar TA, Sultan A, Butt MF, Kawoosa AA, Mir MR. Delayed fixation of the transcervical fracture of the neck of the femur in the pediatric population: results and complications. J Child Orthop. 2009;3(6):473–7. https://doi.org/10.1007/s11832-009-0209-2.
Mirdad T. Fractures of the neck of femur in children: an experience at the Aseer Central Hospital, Abha, Saudi Arabia. Injury. 2002;33(9):823–7. https://doi.org/10.1016/s0020-1383(02)00013-x.
Azouz EM, Karamitsos C, Reed MH, Baker L, Kozlowski K, Hoeffel JC. Types and complications of femoral neck fractures in children. Pediatr Radiol. 1993;23(6):415–20. https://doi.org/10.1007/BF02012436.
Pring M, Rang M, Wenger D. Pelvis and hip. In: Rang M, Pring M, Wenger DR, editors. Rang’s children’s fractures. 3rd ed. Philadelphia: Lippincott Williams & Wilkins; 2005. pp. 165–79.
Pandey RA, John B. Current controversies in management of fracture neck femur in children: a review. J Clin Orthop Trauma. 2020;32999559(Suppl 5):S799–806. https://doi.org/10.1016/j.jcot.2020.05.029.
Maeda S, Kita A, Fujii G, Funayama K, Yamada N, Kokubun S. Avascular necrosis associated with fractures of the femoral neck in children: histological evaluation of core biopsies of the femoral head. Injury. 2003;34(4):283–6. https://doi.org/10.1016/s0020-1383(02)00281-4.
Riley PM Jr, Morscher MA, Gothard MD, Riley PM Sr. Earlier time to reduction did not reduce rates of femoral head osteonecrosis in pediatric hip fractures. J Orthop Trauma. 2015;29(5):231–8. https://doi.org/10.1097/BOT.0000000000000226.
Moon ES, Mehlman CT. Risk factors for avascular necrosis after femoral neck fractures in children: 25 Cincinnati cases and meta-analysis of 360 cases. J Orthop Trauma. 2006;20(5):323–9. https://doi.org/10.1097/00005131-200605000-00005.
Leung PC, Lam SF. Long-term follow-up of children with femoral neck fractures. J Bone Joint Surg Br. 1986;68(4):537–40. https://doi.org/10.1302/0301-620X.68B4.3733826.
Astur Dda C, Arliani GG, Nascimento CL, Blumetti FC, Fonseca MJ, Dobashi ET, Pinto JA, Ishida A. Correlation between avascular necrosis and early stabilization of proximal femoral fractures in childhood. Rev Bras Ortop. 2015;17(4):426–32. https://doi.org/10.1016/S2255-4971(15)30392-X.
Bali K, Sudesh P, Patel S, Kumar V, Saini U, Dhillon MS. Pediatric femoral neck fractures: our 10 years of experience. Clin Orthop Surg. 2011;3(4):302–8. https://doi.org/10.4055/cios.2011.3.4.302.
Dendane MA, Amrani A, El Alami ZF, El Medhi T, Gourinda H. Displaced femoral neck fractures in children: are complications predictable? Orthop Traumatol Surg Res. 2010;96(2):161–5. https://doi.org/10.1016/j.rcot.2010.02.004.
Qi B, Yu A, Zhang G, Yu G, Shi Y, Zhu S, Pan Z. The treatment of displaced femoral neck fractures with vascularized great trochanter periosteal flap transposition in children. Microsurgery. 2008;28(1):21–4. https://doi.org/10.1002/micr.20439.
Mitchell JI. Fracture of the neck of the femur in children. J Am Med Assoc. 1936;107:1603e1606.
Song KS. Displaced fracture of the femoral neck in children: open versus closed reduction. J Bone Joint Surg [Br]. 2010;92–B:1148e1151.
Ju L, Jiang B, Lou Y, Zheng P. Delayed treatment of femoral neck fractures in 58 children: open reduction internal fixation versus closed reduction internal fixation. J Pediatr Orthop B. 2016;25(5):459–65. https://doi.org/10.1097/BPB.0000000000000339.
Stone JD, Hill MK, Pan Z, Novais EN. Open reduction of Pediatric femoral Neck fractures reduces osteonecrosis risk. Orthopedics. 2015;38(11):e983–90. https://doi.org/10.3928/01477447-20151020-06.
Varshney MK, Kumar A, Khan SA, Rastogi S. Functional and radiological outcome after delayed fixation of femoral neck fractures in pediatric patients. J Orthop Traumatol. 2009;10(4):211–6. https://doi.org/10.1007/s10195-009-0072-4.
Sankar WN, Mehlman CT. The Community Orthopaedic Surgeon taking trauma call: Pediatric femoral Neck fracture pearls and pitfalls. J Orthop Trauma. 2019;33(Suppl 8):S22–6. https://doi.org/10.1097/BOT.0000000000001541.
Davison BL, Weinstein SL. Hip fractures in children: a long-term follow-up study. J Pediatr Orthop. 1992;12(3):355–8. https://doi.org/10.1097/01241398-199205000-00014.
Yeranosian M, Horneff JG, Baldwin K, Hosalkar HS. Factors affecting the outcome of fractures of the femoral neck in children and adolescents: a systematic review. Bone Joint J. 2013;95–B(1):135–42. https://doi.org/10.1302/0301-620X.95B1.30161.
Flynn JM, Wong KL, Yeh GL, Meyer JS, Davidson RS. Displaced fractures of the hip in children: management by early operation and immobilisation in a hip spica cast. J Bone Joint Surg. 2002;ve 84-B:108e112.
Kovar FM, Strasser E, Jaindl M, Endler G, Oberleitner G. Complications following implant removal in patients with proximal femur fractures - an observational study over 16 years. Orthop Traumatol Surg Res. 2015;101(7):785–9. https://doi.org/10.1016/j.otsr.2015.07.021.
Song KS, Lee SW. Subtrochanteric femur fracture after removal of screws for femoral neck fracture in a child. Am J Orthop (Belle Mead NJ). 2015;44(1):40–2.
Funding
No funding has been received for this study.
Author information
Authors and Affiliations
Contributions
MSS, MT: design of the study, statistical analysis, development of checklists, interpretation of data, writing of the article, drafting and revision of the article. FB: acquisition of data, co-writing of the article.BK: contributed to the acquisition and analysis of the data, MSS, MT; contributed to the interpretation of the data and design of the research. All authors critically revised the manuscript, agree to be fully accountable for ensuring the integrity and accuracy of the work, and read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This study was conducted in accordance with the Declaration of Helsinki and received approval from local Instutional Review Board. (B.10.1.TKH.4.34.H.GP.0.01/336).
Guarantor
MT.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Taşcı, M., Başak, F., Kemah, B. et al. Analysis of influential factors on surgical outcomes in pediatric femur neck fractures: a single-institution retrospective study. Eur J Trauma Emerg Surg (2024). https://doi.org/10.1007/s00068-024-02584-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00068-024-02584-x