Abstract
The roles of aromatase inhibitors (AIs) and luteinizing hormone–releasing hormone (LH–RH) agonists in the management of male breast cancer remain uncertain, with no reports in Japanese men. We report four Japanese male patients with metastatic breast cancer treated with AIs with or without an LH–RH agonist, and consider the relationship between treatment effect and estradiol (E2) concentration. Three patients were initially treated with AI alone after selective estrogen receptor modulators (SERMs), and one received AIs plus an LH–RH agonist after a SERM. Two patients treated with an AI alone responded, one patient with E2 levels below the lower assay limit and the other with levels above the limit. The other treated with an AI alone experienced progression regardless of the E2 levels below the lower assay limit, however, responded after the addition of an LH–RH agonist. E2 concentrations were related to the efficacy of treatment in one patient. The patient initially treated with an AI plus an LH–RH agonist also responded. No grade 3 or 4 adverse events were observed in any of the patients treated with AIs with or without an LH–RH agonist. AIs with or without an LH–RH agonist offer an effective treatment option for hormone receptor-positive metastatic male breast cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Male breast cancer is rare, accounting for only 1 % of all breast cancer diagnoses, and metastases in men with breast cancer are even rarer [1]. The small number of male breast cancer cases has resulted in limited clinical data, and treatment strategies for male breast cancer have therefore been based on the results of clinical trials of female breast cancer. According to the first international consensus guidelines for advanced breast cancer (ABC1), most experts agree that tamoxifen is the preferred option for estrogen receptor (ER)-positive metastatic male breast cancer [2]. Regarding the use of aromatase inhibitors (AIs), the need for a concomitant luteinizing hormone–releasing hormone (LH–RH) agonist or orchiectomy remains controversial. The National Comprehensive Cancer Network guidelines suggest that men with breast cancer should be treated similarly to postmenopausal women, except that AIs are ineffective without concomitant suppression of testicular steroidogenesis [3]. The roles of AIs and LH–RH agonists in the management of male breast cancer need to be clarified. Here, we report on four male metastatic breast cancer patients who were treated with an AI with or without an LH–RH agonist at various stages of their treatments.
Case reports
Case 1
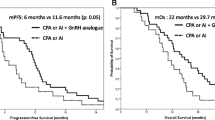
A 40-year-old man presented with coughing, back pain, and a 5.5-cm breast mass. He was diagnosed with invasive ductal carcinoma of the right breast with lung and bone metastases. The breast tumor was ER (Allred score 7) and progesterone receptor (PR) (Allred score 8) positive, but HER2 negative. He was treated with tamoxifen and zoledronic acid (Fig. 1a). Distant metastases were well controlled after 6 months, but the breast mass continued to increase. He underwent simple mastectomy for local control, and continued tamoxifen for a total of 1 year. Because of increased pleural effusion and back pain, he was treated with radiotherapy directed at the thoracic spine, and his hormone therapy was changed to anastrozole and goserelin. He continued treatment with an AI plus LH–RH agonist for a total of 29 months, with partial response. The AIs he used included anastrozole for 21 months, exemestane for 6 months, and letrozole for 2 months. His disease progressed despite treatment with fulvestrant, and chemotherapy was then started. No grade 3 or 4 adverse events were observed in relation to the combined use of an AI and LH–RH agonist.
Case 2
A 53-year-old man presented with back pain and a 2-cm left breast mass. He was diagnosed with invasive ductal carcinoma with multiple bone metastases. The breast tumor was ER (Allred score 7) and PR (Allred score 7) positive and HER2 negative. He was treated with tamoxifen, zoledronic acid, and radiation therapy directed at the lumbar spine and pelvis (Fig. 1b). The number of bone metastases increased after 11 months, and tamoxifen was replaced with letrozole. However, the number of bone metastases increased further over the next 3 months, and goserelin was added to his therapy. His AIs included letrozole for 11 months and exemestane for 3 months. The patient had developed liver metastases at the time of writing and he was scheduled to start treatment with fulvestrant. Estradiol (E2) levels before and during AI treatment, and during treatment with an AI and LH–RH agonist were 27, 10, and ≤10 pg/mL, respectively. No grade 3 or 4 adverse events were observed in relation to the use of AIs with or without an LH–RH agonist.
Case 3
A 72-year-old man with a left breast cancer underwent a mastectomy and axillary lymph node dissection. The tumor was found to be ER (Allred score 8) and PR (Allred score 7) positive, and HER2 positive. Because the patient experienced hemiplegia as a result of brain infarction, he received neither chemotherapy nor trastuzumab. However, he developed liver metastasis during the adjuvant endocrine therapy with tamoxifen 3 years after surgery, and tamoxifen was therefore replaced with letrozole (Fig. 1c). He continued this treatment for 21 months without progression. His E2 levels before and during AI treatment (at progressive disease) were 17 and 10 pg/mL, respectively. No grade 3 or 4 adverse events were observed in relation to the use of an AI.
Case 4
A 72-year-old man with a right breast cancer underwent mastectomy and sentinel lymph node biopsy. The tumor was ER (Allred score 8) and PR (Allred score 5) positive, and HER2 negative. He developed a recurrence on the chest wall during adjuvant endocrine therapy with tamoxifen 2 years after surgery. Resection of the recurrent tumor revealed that it was ER (Allred score 8) and PR (Allred score 5) positive and HER2 positive. Tamoxifen was discontinued and toremifene was started. However, he developed lung metastases 2 years later and toremifene was replaced with letrozole for 6 months (Fig. 1d). The number of the lung metastases increased and goserelin was therefore added. He had continued this treatment for 17 months at the time of writing. His E2 levels during AI, and AI plus LH–RH agonist treatment were 25 and ≤10 pg/mL, respectively. No grade 3 or 4 adverse events were observed in relation to the use of AIs with or without an LH–RH agonist.
Discussion
Male breast cancer is an uncommon disease, and there have been no reports of metastatic male breast cancer treated with AIs with or without an LH–RH agonist in Japanese men. Here, we reported on four men with metastatic breast cancer; three received an AI alone for at least part of their treatment, and three received an AI plus an LH–RH agonist. We also considered the relationship between treatment effect and E2 concentration. Two of three patients achieved partial response with an AI alone (Table 1) but one was resistant, while all patients treated with an AI plus an LH–RH agonist achieved long-term stable disease.
The incidence of male breast carcinoma is increasing [1, 4]. Although breast cancer is similar in men and women, male breast cancer is more frequently hormone receptor positive, and has a higher median age and more advanced stage at diagnosis compared with its female counterpart [4, 5]. Raw data suggest that men have poorer survival than women [4]. However, relative survival rates are similar, after adjusting for older age at diagnosis and poorer life expectancy in men compared with women [4, 6]. Differences in tumor subtypes of male breast cancer exist among different racial/ethnic groups [7], and it is important to examine the efficacies of treatments with respect to these differences.
Most male breast cancer patients are hormone-receptor positive, suggesting an overall good response to endocrine therapy. However, there have been no randomized clinical trials of male breast cancer, and most data come from retrospective series of patients. Treatment strategies are extrapolated from studies of female breast cancer, without evidence to support their suitability in men. Some retrospective data have shown reduced cancer-associated mortality in men with breast cancer treated with tamoxifen, and overall survival was significantly better after adjuvant tamoxifen compared with an AI [8]. Tamoxifen should therefore be considered as the treatment of choice for hormone-receptor-positive male breast cancer in the adjuvant setting. Although approximately 80 % of circulating estrogens in men are derived from peripheral aromatization of androgens, the remaining 20 % are secreted directly by the testes [9, 10], and are therefore unaffected by AIs [11]. Moreover, a trial of AIs in healthy men demonstrated a marked increase in circulating testosterone, with only a 50 % decrease in serum E2 [12]. Based on those data, the National Comprehensive Cancer Network guidelines suggest that men with breast cancer should be treated similarly to postmenopausal women, except that AIs are ineffective without concomitant suppression of testicular steroidogenesis.
Whether AIs alone or in combination with an LH–RH agonist represent the better option for metastatic male breast cancer remains unclear [13–15], and no significant benefit of LH–RH agonist co-administration has so far been demonstrated [14]. The SWOG-S0511 trial evaluated the combination of anastrozole and goserelin in men with hormone-receptor-positive metastatic breast cancer, but was closed prematurely because of poor accrual. Doyen et al. [13] have reported that AIs alone showed activity in male breast cancer patients, and that this activity correlated with significant reductions in E2 concentration. In this study, two of three patients (Cases 2 and 3) had E2 levels below the lower assay limit during AI treatment, while Case 4 had E2 levels below the lower limit during treatment with an AI and an LH–RH agonist. However, although the efficacy of treatment was related to E2 concentrations in Case 3 in the current study, the correlation was poor in Cases 2 and 4. Alternatively, treatment with an LH–RH agonist may have decreased the E2 concentrations in Cases 2 and 4. Further studies are needed to clarify the relation between treatment effect and E2 concentrations.
There have been few reports of endocrine-therapy-related side effects among male breast cancer patients, and AIs regardless of the use of LH–RH agonists have been well tolerated, with no grade 3 or 4 adverse events [14, 15]. Tamoxifen, however, has been associated with toxic effects and a high rate of discontinuation [16, 17], and discontinuation of endocrine therapy remains a problem in both men and women [18–21].
In conclusion, AIs with or without an LH–RH agonist can offer effective treatment options for men with hormone-receptor-positive metastatic breast cancer.
References
White J, Kearins O, Dodwell D, Horgan K, Hanby AM, Speirs V. Male breast carcinoma: increased awareness needed. Breast Cancer Res. 2011;13(5):219.
Cardoso F, Costa A, Norton L, Cameron D, Cufer T, Fallowfield L, et al. 1st International consensus guidelines for advanced breast cancer (ABC 1). Breast. 2012;21(3):242–52.
NCCN Clinical Practice guideline in Oncology: Breast Cancer. 2014. http://www.nccn.org/professionals/physician_gls/f_guidelines.asp.
Giordano SH, Cohen DS, Buzdar AU, Perkins G, Hortobagyi GN. Breast carcinoma in men. Cancer. 2004;101:51–7.
Giordano SH, Buzdar AU, Hortobagyi GN. Breast cancer in men. Ann Intern Med. 2002;137:678–87.
Rushton M, Kwong A, Visram H, Graham N, Petrcich W, Dent S. Treatment outcomes for male breast cancer: a single-center retrospective case control study. Curr Oncol. 2014;21(3):e400–7.
Chavez-Macgregor M, Clarke CA, Lichtensztajn D, Hortobagyi GN, Giordano SH. Male breast cancer according to tumor subtype and race: a population based study. Cancer. 2013;119(9):1611–7.
Eggemann H, Ignatov A, Smith BJ, Altmann U, von Minckwitz G, Röhl FW, et al. Adjuvant therapy with tamoxifen compared to aromatase inhibitors for 257 male breast cancer patients. Breast Cancer Res Treat. 2013;137(2):465–70.
Zumoff B, Fishman J, Cassouto J, Hellman L, Gallagher TF. Estradiol transformation in men with breast cancer. J Clin Endocrinol Metab. 1966;26(9):960–6.
Volm MD. Male breast cancer. Curr Treat Options Oncol. 2003;4(2):159–64.
Harris AL, Dowsett M, Stuart-Harris R, Smith IE. Role of aminoglutethimide in male breast cancer. Br J Cancer. 1986;54(4):657–60.
Mauras N, O’Brien KO, Klein KO, Hayes V. Estrogen suppression in males: metabolic effects. J Clin Endocrinol Metab. 2000;85(7):2370–7.
Doyen J, Italiano A, Largillier R, Ferrero JM, Fontana X, Thyss A. Aromatase inhibition in male breast cancer patients: biological and clinical implications. Ann Oncol. 2010;21(6):1243–5.
Zagouri F, Sergentanis TN, Koutoulidis V, Sparber C, Steger GG, Dubsky P, et al. Aromatase inhibitors with or without gonadotropin-releasing hotmone analogue in metastatic male breast cancer: a case series. Br J Cancer. 2013;108(11):2259–63.
Di Lauro L, Vici P, Del Medico P, Laudadio L, Tomao S, Giannarelli D, et al. Breast Cancer Res Treat. 2013;141(1):119–23.
Visram H, Kanji F, Dent SF. Endocrine therapy for male breast cancer: rates of toxicity and adherence. Curr Oncol. 2010;17(5):17–21.
Pemmaraju N, Munsell MF, Hortobagyi GN, Giordano SH. Retrospective review of male breast cancer patients: analysis of tamoxifen-related side-effects. Ann Oncol. 2012;23(6):1471–4.
Lash TL, Fox MP, Westrup JL, Fink AK, Silliman RA. Adherence to tamoxifen over the five-year course. Breast Cancer Res Treat. 2006;99(2):215–20.
Hershman DL, Kushi LH, Shao T, Buono D, Kershenbaum A, Tsai WY, et al. Early discontinuation and nonadherence to adjuvant hormonal therapy in a cohort of 8,769 early-stage breast cancer patients. J Clin Oncol. 2010;28(27):4120–8.
Taketani K, Tokunaga E, Yamashita N, Tanaka K, Akiyoshi S, Okada S, et al. Early discontinuation of adjuvant hormone therapy is associated with a poor prognosis in Japanese breast cancer patients. Surg Today. 2014;44(10):1841–6.
Kuba S, Ishida M, Nakamura Y, Taguchi K, Ohno S. Persistence and discontinuation of adjuvant endocrine therapy in women with breast cancer. Breast Cancer 2016;23(1):128–33.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
S. Ohno received lecture fees from Chugai and Astrazeneca.
About this article
Cite this article
Kuba, S., Ishida, M., Oikawa, M. et al. Aromatase inhibitors with or without luteinizing hormone–releasing hormone agonist for metastatic male breast cancer: report of four cases and review of the literature. Breast Cancer 23, 945–949 (2016). https://doi.org/10.1007/s12282-016-0679-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12282-016-0679-2