Abstract
Although several studies have shown the efficacy of third-generation aromatase inhibitors (AIs) in women with breast cancer, the role of such molecules remains elusive in male breast cancer patients. It is also unknown whether the addition of gonadotropin-releasing hormone (GnRH) analogues to AIs would be a superior strategy or not. This pooled analysis was conducted in accordance with the PRISMA guidelines. All studies that examined the efficacy of AIs in metastatic male breast cancer were considered eligible. Overall, 15 studies (105 cases) were eligible for this pooled analysis. The mean age of the study sample was 62.8 years. ER status was positive in all eligible cases. AI was given as first line in 61.5 % of cases. GnRH analogue was co-administered with AI in 37.1 % of cases (n = 39). CR, PR, SD and PD were achieved in 5.7, 23.8, 37.2 and 33.3 % of cases, respectively. The median PFS and OS were equal to 10.0 and 39.0 months, respectively. Co-administration of GnRH analogues was associated with more than threefold increase in rates of clinical benefit (OR = 3.37, 95 % CI 1.30–8.73) but did not seem to correlate with better PFS or OS. No statistically significant associations between the examined outcomes and the other parameters were noted. Available data suggest that AIs may potentially play a promising role in the optimal therapeutic strategy for metastatic male breast cancer patients. Especially, co-administration of AI with a GnRH analogue seems to increase the rate of clinical benefit and could be more effective, warranting further consideration.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Male breast cancer is an uncommon malignancy, with an occurrence of one case per 100,000 people in Europe and comprises less than 1 % of all breast cancers [1, 2]. Due to the rarity of this neoplasm, it is hard to conduct prospective clinical trials; therefore, the management strategies are based on limited retrospective studies and clinical management of female breast cancer. According to ESMO and NCCN guidelines, tamoxifen is the gold-standard adjuvant endocrine therapy in male breast cancer and plays an important role in the metastatic setting [3–5]. On the other hand, little is known about other endocrine therapies in patients who were already exposed to tamoxifen.
Aromatase inhibitors (AIs) prevent the conversion of androstendione to 17β-estradiol and are extensively used for the treatment of hormone receptor (HR)-positive, postmenopausal women with breast cancer [3–6]. Although the superiority of third-generation AIs (exemestane, anastrozole and letrozole) over tamoxifen in women has been documented in several studies [7–9], the role of such molecules remains elusive in male breast cancer patients. It is also unknown whether the addition of gonadotropin-releasing hormone (GnRH) analogues to AI would be a superior strategy or not. GnRH are known to desensitize the pituitary GnRH receptors resulting in a reduction of luteinizing hormone (LH) and follicle-stimulating hormone (FSH) as well as a fall in testicular testosterone and estrogens, while the remaining estrogens, produced through peripheral aromatization, may be blocked with AIs. Hence, the combination strategy of AIs with GnRH analogues hold promise—at least in theory—to improve clinical outcomes in metastatic male breast cancer patients but this remains to be demonstrated [10–14].
In this manuscript, we report the first pooled analysis of the literature synthesizing all available data coming from case reports/case series and evaluating the efficacy and safety of aromatase inhibitors in male breast cancer.
Materials and methods
Selection of studies and data abstraction
This pooled analysis was conducted according to the PRISMA guidelines [15]. The protocol of this analysis has been approved by the Institutional Review Board of Alexandra Hospital, Medical School, National University of Athens, Greece and is available upon request. Eligible articles were sought in PUBMED from 1 January 1980 to 15 October 2014. The search strategy included the following keywords: breast[ti] AND (neoplasms OR neoplasm OR cancer OR cancers OR carcinoma OR carcinomas) AND (“aromatase inhibitors” OR anastrozole OR letrozole OR exemestane) AND (male[ti] OR men[ti]).
All reports or studies that examined the efficacy (response and/or survival) of third-generation AIs (anastrozole, letrozole, exemestane) in metastatic male breast cancer and reported data regarding efficacy, regardless of sample size, were eligible for this pooled analysis. Studies with AIs administration in male breast cancer patients without reporting any data on efficacy were excluded from this analysis. In this pooled analysis, in case of administration of AI in different lines of treatments, only the first administration of AI was considered eligible. Moreover, the first time of co-administration of AI and GnRH analogues, was considered eligible for this analysis, irrespectively of administration of GnRH analogues or AI in a previous line of treatment; in that case, the subjects were censored at the moment of transition to the second treatment (regarding the first treatment). Moreover, cases with co-administration of AI with other chemotherapeutic agents or hormonal manipulations other than GnRH analogues were excluded from this analysis.
Only articles in English, German, Spanish and French were considered eligible for this pooled analysis. Two investigators (FZ and DC), working independently and blindly to each other, searched the literature and performed data abstraction. Reviews were not eligible, while all prospective and retrospective studies, as well as case reports, were eligible for this pooled analysis. In addition, in a “snowball” procedure we evaluated all references in relevant reviews and eligible articles retrieved by our search strategy, in an attempt to identify additional studies and conference abstracts.
The following data were collected: first author, year of publication, type of aromatase inhibitor, co-administration of GnRH analogues, characteristics of patient population (pathological type, initial stage, grade, ER, PR and HER2 status, ki-67), age (years), previous treatments (hormonal treatment, chemotherapy), line of treatment, response [complete response (CR), partial response (PR), stabilization of the disease (SD), progression of the disease (PD)], type of metastases (visceral, bone) median overall survival (OS) in months, median progression-free survival (PFS) in months and complications.
Quantitative synthesis and statistics
Regarding the quantitative synthesis (pooled analysis) of the published studies, two sets of calculations were performed. First, the descriptive statistics were calculated. Kaplan–Meier survival curves were estimated for PFS and OS, separately by the co-administration GnRH analogues or not, for the graphical presentation of results. Second, factors potentially associated with i. clinical benefit, as defined by each eligible study (CR, PR and SD grouped together, versus PD), and ii. PFS and iii. OS were evaluated; to this end, univariate logistic regression analyses and univariate Cox regression analyses were performed, respectively. The potentially prognostic factors that were examined were the following: co-administration of GnRH analogues, type of AI (exemestane vs. anastrozole/letrozole), age at AI administration, lines of treatment, grade, initial stage at diagnosis, HER2 status, PR status, adjuvant hormonal treatment, adjuvant chemotherapy, visceral metastases and bone metastases. In case of not estimable odds ratios, due to the presence of a zero cell in the corresponding 2 × 2 table, the p values were derived from Fisher’s exact test. In case of not estimable hazard ratios, due to the occurrence of zero events in an examined subgroup, the p-values were derived from log-rank test, as appropriate.
The statistical analysis should be deemed explorative given the questionable comparability of cases among the various studies. Statistical analysis was performed with STATA/SE 13 statistical software (StataCorp, College Station, TX, USA).
Results
The search strategy retrieved 39 articles. Among them, five were irrelevant, 13 were reviews, eight were excluded due to various reasons [2, 16–22] (language restrictions [16], AI administered in the adjuvant setting [2, 17], lack of data pertaining to efficacy [18–21], aromatase inhibitors other than these of the third generation [22] ) and 13 were eligible [10, 11, 23–33] ). The “snowball” procedure yielded two additional conference abstracts/articles that were included [34, 35]. Of note, the case by Baumgärtner et al. [36], retrieved through the references of eligible articles, was excluded from our analysis due to reporting reasons as OS and PFS were not provided, while best response was not clearly defined. Overall, 15 studies (105 cases, 102 patients individuals as three patients were included both at the AI group and AI plus analogue group) were eligible for this pooled analysis (Suppl Tables 1, 2). The aforementioned steps are illustrated in detail in Fig. 1.
The mean age of the study sample was 62.8 years (SD 10.0, median 63). The majority of cases (86.5 %) presented with IDC, whereas 13.5 % presented with ILC. Stage at initial diagnosis was as follows: stage I 13.5 %, II 32.4 %, III 37.9 % and IV 16.2 %. Half of the cases had a grade 3 carcinoma (50 %), followed by grade 2 (44 %) and grade 1 (6 %). ER was positive in all eligible cases, PR was positive in the vast majority of cases (94.7 %) and HER2 was negative in 97.0 % of male breast cancer cases; the mean ki-67 positivity percentage was 31.0 % (SD 13.5, median 30.0). Adjuvant hormonal treatment was administered in 67.2 % of cases where this information was provided. As far as previously given adjuvant chemotherapy, 26.1 % of cases had received anthracycline- and taxane-based chemotherapy; 18.5 % had received anthracycline-based chemotherapy; 4.6 % had received taxane-based chemotherapy; 16.9 % had received other regimens, whereas the majority of cases (33.9 %) had not received any adjuvant chemotherapy. In one case, trastuzumab was co-administered with anastrozole as maintenance therapy.
AI was given as first line therapy for metastatic disease in 61.5 % of cases, as second line in 25.3 %, while as third line or beyond in 13.2 % of cases. 77.8 % of cases at AI administration had visceral metastases, whereas in 40.7 % of them bone metastases existed; of note, in 12.3 % of the total cases only bone metastases were present without the presence of visceral metastases. Anastrozole or letrozole was given in 85.2 % of cases, whereas exemestane was administered in 14.8 %. Of note, GnRH analogue was co-administered with aromatase inhibitor in 37.1 % of cases (n = 39).
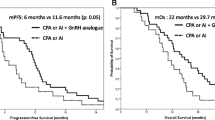
Regarding best response, in 5.7 % of cases CR was achieved, in 23.8 % PR was noted, in 37.2 % of cases SD was recorded, whereas in 33.3 % PD was observed. The median PFS was equal to 10.0 months, while the median OS was equal to 39.0 months. Kaplan–Meier survival estimate regarding progression-free survival and overall survival is depicted in Figs. 2, 3, and 4.
Table 1 presents the results of univariate logistic regression and univariate Cox regression analyses regarding clinical benefit, PFS and OS, respectively. Co-administration of GnRH analogues was associated with more than threefold increase in rates of clinical benefit (OR = 3.37, 95 % CI 1.30–8.73, versus no administration of GnRH analogues, Fig. 5) but did not seem to correlate with better PFS (HR = 0.89, p = 0.740) or OS (HR = 0.75, p = 0.563). No statistically significant associations between the examined outcomes and type of AI, age at administration of AI, lines of treatment, grade, initial stage at diagnosis, HER2 status, PR status, adjuvant hormonal treatment, adjuvant chemotherapy, visceral metastases or bone metastases were noted.
Discussion
Our results indicate that AIs represent an effective and safe treatment option for HR-positive metastatic male breast cancer patients, with a median progression-free survival equal to 10 months. We found that co-administration of GnRH analogues was associated with more than threefold increase in clinical benefit rate, suggesting that this combination seems to be potentially more effective than AIs alone in metastatic male breast cancer patients; a finding that has never been previously reported in the literature.
In preclinical models, administration of AIs correlated with significant increase in the levels of FSH and testosterone, but not estradiol (E2) [13, 26]. However, in healthy men, administration of AIs resulted in a significant reduction in E2 levels, along with an increase in FSH, LH, and testosterone levels [14, 26]. Consequently, this increase in testosterone levels may overcome aromatase inhibition, limiting the efficacy of AIs [2, 18]. Therefore, it seems that the combination treatment of AIs with GnRH analogues may maximize the effect of aromatase inhibition. In our analysis, despite the threefold increase in rates of clinical benefit, no significance difference in OS and PFS was observed between cases of AIs and cases with co-administration of GnRH analogues; the lack of statistical significance was due to the limited number of cases with data regarding PFS and OS as only a subset of eligible studies reported on survival.
Of note, hormonal treatment seems to represent the cornerstone of therapy for metastatic male breast cancer, taking into consideration that breast cancer in men exhibit a high rate of hormone receptor positivity. According to our pooled analysis, it is interesting enough that AIs seem to remain a reliable treatment option for male patients beyond the first line. Currently, tamoxifen is the most extensively used hormonal therapy for male breast cancer, despite the fact that results stem from relatively small retrospective studies [18, 37]; other medical hormonal manipulations are androgens, steroids, antiandrogens, progestins and estrogens [38–40]. Moreover, the use of fulvestrant in male breast cancer is safe, with promising efficacy data; however, further clinical and pharmacokinetic investigations are warranted before its use becomes a common practice [41, 42].
Concerning the limitations of this study, one cannot ignore that this pooled analysis was confined to case series/case reports, a fact that might have biassed our findings. More specifically, case series are often not published unless there is an adverse event or an interesting outcome that is surprising to the clinician; hence, a firm conclusion cannot be drawn. Therefore, expanding beyond the 105 reported cases of AIs administration that were included in our study, so as to look on a larger scale, seems to be important. Of note, a large registry project currently ongoing by the EORTC is gathering medical information and tumour samples from male breast cancer patients (www.clinicaltrials.gov; ID: NCT01101425). Moreover, prospective investigation of this treatment option is needed to draw definitive conclusions; the data of a phase II trial in metastatic male breast cancer patients, in which goserelin is given in combination with anastrozole, are awaited with interest (SWOG-S0511 trial; www.clinicaltrilas.gov; ID: NCT00217659).
In conclusion, available data suggest that AIs may potentially play a promising role in the optimal therapeutic strategy for metastatic male patients with breast cancer diagnosis. Especially, co-administration of AI with a GnRH analogue seems to increase the rate of clinical benefit and could be more effective, warranting further consideration.
References
Brinton LA, Richesson DA, Gierach GL, Lacey JV Jr, Park Y, Hollenbeck AR, Schatzkin A (2008) Prospective evaluation of risk factors for male breast cancer. J Natl Cancer Inst 100:1477–1481
Eggemann H, Ignatov A, Smith BJ, Altmann U, von Minckwitz G, Röhl FW, Jahn M, Costa SD (2013) Adjuvant therapy with tamoxifen compared to aromatase inhibitors for 257 male breast cancer patients. Breast Cancer Res Treat 137:465–470
NCCN Clinical Practice Guidelines in Oncology. Breast Cancer. Version 3.2014. Available at www.nccn.com
Cardoso F, Costa A, Norton L, Senkus E, Aapro M, André F, Barrios CH, Bergh J, Biganzoli L, Blackwell KL, Cardoso MJ, Cufer T, El Saghir N, Fallowfield L, Fenech D, Francis P, Gelmon K, Giordano SH, Gligorov J, Goldhirsch A, Harbeck N, Houssami N, Hudis C, Kaufman B, Krop I, Kyriakides S, Lin UN, Mayer M, Merjaver SD, Nordström EB, Pagani O, Partridge A, Penault-Llorca F, Piccart MJ, Rugo H, Sledge G, Thomssen C, Van’t Veer L, Vorobiof D, Vrieling C, West N, Xu B, Winer E (2014) ESO-ESMO 2nd international consensus guidelines for advanced breast cancer (ABC2). Ann Oncol 25:1871–1888
Cardoso F, Costa A, Norton L, Senkus E, Aapro M, André F, Barrios CH, Bergh J, Biganzoli L, Blackwell KL, Cardoso MJ, Cufer T, El Saghir N, Fallowfield L, Fenech D, Francis P, Gelmon K, Giordano SH, Gligorov J, Goldhirsch A, Harbeck N, Houssami N, Hudis C, Kaufman B, Krop I, Kyriakides S, Lin UN, Mayer M, Merjaver SD, Nordström EB, Pagani O, Partridge A, Penault-Llorca F, Piccart MJ, Rugo H, Sledge G, Thomssen C, Van’t Veer L, Vorobiof D, Vrieling C, West N, Xu B, Winer E (2014) ESO-ESMO 2nd international consensus guidelines for advanced breast cancer (ABC2). Breast 23:489–502
Jordan VC, Obiorah I, Fan P, Kim HR, Ariazi E, Cunliffe H, Brauch H (2011) The St. Gallen Prize evolution of long-term adjuvant anti-hormone therapy: consequences and opportunities. Breast 20(Suppl 3):S1–S11
Regan MM, Neven P, Giobbie-Hurder A, Goldhirsch A, Ejlertsen B, Mauriac L, Forbes JF, Smith I, Láng I, Wardley A, Rabaglio M, Price KN, Gelber RD, Coates AS, Thürlimann B, BIG 1–98 Collaborative Group; International Breast Cancer Study Group (IBCSG) (2011) Assessment of letrozole and tamoxifen alone and in sequence for postmenopausal women with steroid hormone receptor-positive breast cancer: the BIG 1–98 randomised clinical trial at 8.1 years median follow-up. Lancet Oncol 12:1101–1108
Cuzick J, Sestak I, Baum M, Buzdar A, Howell A, Dowsett M, Forbes JF, ATAC, LATTE investigators (2011) Effect of anastrozole and tamoxifen as adjuvant treatment for early-stage breast cancer: 10-year analysis of the ATAC trial. Lancet Oncol 11:1135–1141
Bliss JM, Kilburn LS, Coleman RE, Forbes JF, Coates AS, Jones SE, Jassem J, Delozier T, Andersen J, Paridaens R, van de Velde CJ, Lønning PE, Morden J, Reise J, Cisar L, Menschik T, Coombes RC (2012) Disease-related outcomes with long-term follow-up: an updated analysis of the intergroup exemestane study. J Clin Oncol 30:709–717
Soon Wong N, Seong Ooi W, Pritchard KI (2007) Role of gonadotropin-releasing hormone analog in the management of male metastatic breast cancer is uncertain. J Clin Oncol 25:3787
Giordano SH, Hortobagyi GN (2006) Leuprolide acetate plus aromatase inhibition for male breast cancer. J Clin Oncol 24:e42–e43
Onami S, Ozaki M, Mortimer JE, Pal SK (2010) Male breast cancer: an update in diagnosis, treatment and molecular profiling. Maturitas 65:308–314
Turner KJ, Morley M, Atanassova N, Swanston ID, Sharpe RM (2000) Effect of chronic administration of an aromatase inhibitor to adult male rats on pituitary and testicular function and fertility. J Endocrinol 164:225–238
Mauras N, O’Brien KO, Klein KO, Hayes V (2000) Estrogen suppression in males: metabolic effects. J Clin Endocrinol Metab 85:2370–2377
Liberati A, Altman DG, Tetzlaff J (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol 62:e1–e34
Katayama K, Yamagishi J, Kashiwagi B (2013) A case of male breast cancer for which mTOR inhibitor was effective with advanced renal cancer. Gan To Kagaku Ryoho 40:365–369
Chen F, Qiu L (2014) Biological and clinical implications of aromatase inhibitors in early male breast cancer patients. Zhonghua Yi Xue Za Zhi 94:273–275
White J, Kearins O, Dodwell D, Horgan K, Hanby AM, Speirs V (2011) Male breast carcinoma: increased awareness needed. Breast Cancer Res 13:219
Visram H, Kanji F, Dent SF (2010) Endocrine therapy for male breast cancer: rates of toxicity and adherence. Curr Oncol 17:17–21
Harlan LC, Zujewski JA, Goodman MT, Stevens JL (2010) Breast cancer in men in the United States: a population-based study of diagnosis, treatment, and survival. Cancer 116:3558–3568
Cutuli B, Le-Nir CC, Serin D, Kirova Y, Gaci Z, Lemanski C, De Lafontan B, Zoubir M, Maingon P, Mignotte H, de Lara CT, Edeline J, Penault-Llorca F, Romestaing P, Delva C, Comet B, Belkacemi Y (2010) Male breast cancer. Evolution of treatment and prognostic factors. Analysis of 489 cases. Crit Rev Oncol Hematol 73:246–254
Horimoto Y, Hino M, Saito M, Arakawa A, Matsumoto T, Kasumi F (2008) Bilateral nonsynchronous male breast cancer: two case reports. Breast Care (Basel) 3:51–53
Bradley KL, Tyldesley S, Speers CH, Woods R, Villa D (2014) Contemporary systemic therapy for male breast cancer. Clin Breast Cancer 14:31–39
Di Lauro L, Vici P, Del Medico P, Laudadio L, Tomao S, Giannarelli D, Pizzuti L, Sergi D, Barba M, Maugeri-Saccà M (2013) Letrozole combined with gonadotropin-releasing hormone analog for metastatic male breast cancer. Breast Cancer Res Treat 141:119–123
Zagouri F, Sergentanis TN, Koutoulidis V, Sparber C, Steger GG, Dubsky P, Zografos GC, Psaltopoulou T, Gnant M, Dimopoulos MA, Bartsch R (2013) Aromatase inhibitors with or without gonadotropin-releasing hormone analogue in metastatic male breast cancer: a case series. Br J Cancer 108:2259–2263
Bighin C, Lunardi G, Del Mastro L, Marroni P, Taveggia P, Levaggi A, Giraudi S, Pronzato P (2010) Estrone sulphate, FSH, and testosterone levels in two male breast cancer patients treated with aromatase inhibitors. Oncologist 15:1270–1272
Montero AJ, Talebi TN, Zhu Y, Branch KD, Goldsberry GT, Baker MK, Gluck S (2011) Successful use of biweekly gemcitabine plus nab-paclitaxel in two male patients with stage iv breast cancer: case reports and review of the literature. Am J Ther 18:e12–e18
Doyen J, Italiano A, Largillier R, Ferrero JM, Fontana X, Thyss A (2010) Aromatase inhibition in male breast cancer patients: biological and clinical implications. Ann Oncol 21:1243–1245
Fontana S, Ghilardi R, Barbaglio A, Amaddeo P, Faldi F, Pericotti S (2007) Male breast cancer with mandibular metastasis. A case reports. Minerva Stomatol 56:225–230
Arriola E, Hui E, Dowsett M, Smith IE (2007) Aromatase inhibitors and male breast cancer. Clin Transl Oncol 9:192–194
Carmona-Bayonas A (2007) Potential benefit of maintenance trastuzumab and anastrozole therapy in male advanced breast cancer. Breast 16:323–325
Zabolotny BP, Zalai CV, Meterissian SH (2005) Successful use of letrozole in male breast cancer: a case report and review of hormonal therapy for male breast cancer. J Surg Oncol 90:26–30
Giordano SH, Valero V, Buzdar AU, Hortobagyi GN (2002) Efficacy of anastrozole in male breast cancer. Am J Clin Oncol 25:235–237
Italiano A, Largillier R, Marcy PY, Foa C, Ferrero JM, Hartmann MT, Namer M (2004) Complete remission obtained with letrozole in a man with metastatic breast cancer. Rev Med Interne 25:323–324
Arrighi G, Cresti N, Donati S, Ricci S, Michelotti A, Ospedaliera A, Pisana U, Aromatase inhibitos in male breast cancer (2005) Abstract A17. 7TH National Congrss of Medical Oncology. Naples, Italy. Ann Oncol 16(Suppl. 7):vii 11
Baumgärtner AK, Schnelzer AC, Harbeck N, Kiechle M, von Steinburg SP (2007) Endocrine combination therapy for prostate and metastatic breast cancer in a male patient. Breast Care 2:37–39
Kantarjian H, Yap HY, Hortobagyi G, Buzdar A, Blumenschein G (1983) Hormonal therapy for metastatic male breast cancer. Arch Intern Med 143:237–240
Doberauer C, Niederle N, Schmidt CG (1988) Advanced male breast cancer treatment with the LH-RH analogue buserelin alone or in combination with the antiandrogen flutamide. Cancer 62:474–478
Labrie F, Dupont A, Bélanger A, Lacourcière Y, Béland L, Cusan L, Lachance R (1990) Complete response to combination therapy with an LHRH agonist and flutamide in metastatic male breast cancer: a case report. Clin Invest Med 13:275–278
Kogire M, Yoshida A, Noda H, Asano M, Yamada T, Kitamura O, Matsumoto M (1985) A case of advanced male breast cancer treated effectively with estrogen. Gan No Rinsho 31:865–869
Zagouri F, Sergentanis TN, Chrysikos D, Zografos E, Rudas M, Steger G, Zografos G, Bartsch R (2013) Fulvestrant and male breast cancer: a case series. Ann Oncol 24:265–266
Zagouri F, Sergentanis TN, Chrysikos D, Dimopoulos MA, Psaltopoulou T (2015) Fulvestrant and male breast cancer: a pooled analysis. Breast Cancer Res Treat 149:269–275
Conflict of interest
The authors have declared no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below are the links to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Zagouri, F., Sergentanis, T.N., Azim, H.A. et al. Aromatase inhibitors in male breast cancer: a pooled analysis. Breast Cancer Res Treat 151, 141–147 (2015). https://doi.org/10.1007/s10549-015-3356-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-015-3356-9