Abstract
Background
Although triple-negative breast cancer (TNBC) with epidermal growth factor receptor (EGFR) expression has been extensively studied, few studies have simultaneously examined EGFR expression and EGFR gene amplification. Here, we examined the correlations of EGFR expression with EGFR gene amplification, EGFR-activating mutations, and the expression of components of the Akt pathway.
Methods
Tumor tissues were obtained from 84 patients with TNBC. We analyzed the expression of EGFR, phosphorylated Akt (p-Akt), phosphorylated mammalian target of rapamycin (p-mTOR), and other relevant proteins using immunohistochemistry. We also analyzed EGFR gene and chromosome 7 copy numbers by dual-color in situ hybridization. DNA was extracted from formalin-fixed paraffin-embedded samples. Analysis of EGFR gene-activating mutations was performed using the smart amplification process version 2 assay.
Results
Most TNBCs expressing EGFR are non-specialized invasive ductal carcinomas, whereas others are likely to be rare specialized carcinomas, such as typical medullary carcinoma, apocrine carcinoma, metaplastic carcinoma, and adenoid cystic carcinoma. EGFR was expressed in samples from 28 of 84 (33.3 %) patients, but the EGFR gene was not amplified in any of the 84 samples. There were significant correlations between EGFR expression and the number of polysomic cells and the presence of high polysomy of chromosome 7. However, EGFR expression was not correlated with p-Akt or p-mTOR expression, nor with the other clinicopathological factors recorded in this study. We found no evidence of EGFR gene-activating mutations.
Conclusions
EGFR gene amplification and EGFR-activating mutations might not be the mechanisms leading to the constitutive activation of EGFR in TNBC. Further investigation is needed to clarify the other molecular mechanisms for oncogenic activation of EGFR in TNBC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Triple-negative breast cancer (TNBC) is defined by the lack of estrogen receptor (ER) and progesterone receptor (PgR) expression on immunohistochemistry, and by the lack of human epidermal growth factor type 2 (HER2) overexpression or gene amplification detected by immunohistochemistry or in situ hybridization. TNBCs represent a group of tumors with poor prognosis and poor sensitivity to currently available therapies targeting endocrine receptors or HER2.
Epidermal growth factor receptor (EGFR) is expressed in 13–52 % of TNBCs [1]. EGFR expression is associated with poor clinical outcome and aggressive biological properties of TNBC [2]. Therefore, elucidating the role of EGFR expression on the cell membrane is critical for implementing successful anti-EGFR therapy. However, the mechanism responsible for EGFR expression in TNBC is still poorly understood.
The EGFR gene is located on the arm of chromosome 7. The gene codes a transmembrane protein consisting of an extracellular EGF binding domain, a short transmembrane region, and an intracellular domain with ligand-activated tyrosine kinase activity. Activation of the EGFR through its tyrosine kinase domain leads to the recruitment of downstream effectors and the activation of proliferative and cell survival signaling pathways [3, 4]. The Ras–Raf mitogen-activated protein kinase pathway and the Akt pathway are the major proliferative and cell survival signaling pathways activated by the EGFR [5–7].
EGFR gene mutations, which cause ligand-independent receptor tyrosine kinase activity or EGFR overexpression, are responsible for constitutional activation of proliferative and cell survival signaling pathways [3, 5–7]. Constitutional activation of these signaling pathways can lead to aberrant activity of many cellular processes, resulting in malignant transformation of cells.
EGFR is now widely considered as a molecular therapeutic target in colorectal cancer, non-small cell lung cancer (NSCLC), and squamous cell carcinoma of the head and neck. Patients with NSCLC with EGFR gene mutations and increased EGFR copy numbers are particularly sensitive to anti-EGFR therapies [8–10]. Although EGFR is frequently expressed in TNBC, and several clinical trials of anti-EGFR drugs have been conducted [1, 11], the practical use of anti-EGFR drugs is still controversial.
Interestingly, several recent studies have found that there are no EGFR-activating mutations in TNBC [12–15]. To our knowledge, only one report [16] has identified such mutations; 11.4 % of their patients had mutations, but these mutations were independent of EGFR expression determined by immunohistochemistry. Notably, 1.6–21 % of breast cancers showing EGFR expression had increased EGFR gene copy numbers [12, 15, 17–19]. Moreover, Gumuskaya et al. [19] reported that cell membrane EGFR expression is associated with increased gene copy number.
Although TNBCs expressing EGFR have been extensively studied, few studies have simultaneously examined EGFR expression and EGFR gene amplification. Therefore, the aim of this study was to examine correlations of EGFR expression with EGFR gene amplification, EGFR-activating mutations, and the expression of components of the Akt pathway.
Materials and methods
Patients and tissues
One hundred and fifteen TNBC specimens were obtained from patients who underwent surgery at Gunma University Hospital (Maebashi, Gunma) and Tone Chuou Hospital (Numata, Gunma) between January 1997 and December 2010. The tissues were 10 % formalin-fixed and paraffin-embedded (FFPE). All hematoxylin and eosin-stained and immunohistochemically stained FFPE sections were reviewed to confirm their morphological and immunohistochemical parameters. Patients who received neoadjuvant chemotherapy at initial diagnosis were excluded and also tissues which were not well preserved and could not provide enough material for immunostaining were excluded from this study. A total of 84 out of those 115 TNBC samples were obtained for this study. Informed consent was obtained before surgery. The Committee for Clinical Studies, Gunma University Faculty of Medicine reviewed and approved this study (17 February 2011, No. 10-25). The clinicopathological features of the patients are shown in Table 1.
Pathologic investigations
Tumors were histologically classified according to the general rules of clinical and pathological recording of breast cancer (16th edition) of the Japanese Breast Cancer Society [20]. However, two further histological subclassifications were included for TNBC, as described by Ishikawa et al. [21]. One was atypical medullary carcinoma (classified as type A) defined as high nuclear grade carcinoma composed of a syncytial arrangement of tumor cells, marked stromal lymphocytic infiltration, a pushing border of invasion, and a ribbon-like architecture with massive necrosis [22, 23]. The other type was invasive ductal carcinoma (IDC) with a central acellular zone (classified as type B), as described by Tsuda et al. [23, 24]. Conventional IDCs, other than types A and B, were classified as type C (conventional IDC), whereas specialized types were classified as type D.
Immunohistochemistry and evaluation of immunostaining
We cut 4-μm-thick sections from FFPE tumor tissues. Immunostaining for ER, PgR, HER2, EGFR, CK5/6, and Ki67 was performed using the Ventana XT system (Ventana Japan, Tokyo, Japan) with the antibodies listed in Table 2. Immunostaining for phosphorylated Akt (p-Akt) and phosphorylated mammalian target of rapamycin (p-mTOR) was performed using the polymer detection method (Simple Stein MAX-PO, Nichirei, Tokyo, Japan) with the antibodies listed in Table 2. For all other antigens, the epitopes were retrieved by boiling the sections in citrate buffer at pH 6.0 for 30 min.
Tissue samples with nuclear staining for ER or PgR in at least 10 % of the tumor cells were classified as ER or PgR positive. HER2 was defined as positive when the tumor was scored 3+ or 2+ and the HER2 gene/chromosome 17 centromere ratio was greater than 2.2 on in situ hybridization. EGFR (Fig. 1a) was scored as follows: 0, no immunostaining or membrane staining of less than 10 % of tumor cells; 1+, weak and incomplete membrane staining in more than 10 % of tumor cells; 2+, uniform weak membrane staining in at least 10 % of tumor cells or uniform intense membrane staining in 10–30 % of tumor cells; 3+, uniform intense membrane staining in at least 30 % of tumor cells. EGFR was defined as positive when it was scored as 1+, 2+, or 3+. Tumors were defined as CK5/6 and p-mTOR (Fig. 1b) positive when at least 5 % of cells showed membrane staining for these proteins. The Ki67 labeling index was calculated as the nuclear staining rate of approximately 1000 cells. p-Akt (Fig. 1c) expression was semiquantitatively determined as the histochemical score (H score), which was calculated as staining intensity (scored as 0–3) × percentage of stained cells (0–100 %). Tumors were defined as p-Akt positive when the H score was greater than 50 [25].
Immunohistochemical staining of EGFR, p-mTOR (Ser 2448), and p-Akt (Ser 473) (×400). a A sample showing uniform intense membrane EGFR staining in more than 80 % of tumor cells. Immunohistochemical score is 3+. b A sample showing strong membrane and cytoplasmic p-mTOR (Ser 2448) staining in more than 50 % of tumor cells. c A sample showing strong cytoplasmic p-Akt (Ser 473) expression. H score is 150 (intensity is 3 × percentage of stained cells is 50)
Dual-color in situ hybridization
The dual-color in situ hybridization (DISH) assay for EGFR gene expression was performed using the Ventana XT system (Ventana Japan) with a DNP-labeled EGFR DNA probe (Ventana Japan) and a DNP-labeled chromosome 7 centromere oligoprobe (Ventana Japan) via the one-step fully automated protocol, as previously described [26].
The DISH results were observed under an Olympus BX50 microscope equipped with a Nikon digital camera (DS-Fi1) with a ×40 objective lens. We counted at least 50 nuclei (mean 66.4) as DISH signals in each samples using Image Processing and Analysis in Java (National Institutes of Health). In each nucleus, the numbers of EGFR gene signals and chromosome 7 centromere signals were independently counted. Tumor cells were classified according to the number of copies of the chromosome 7 centromeres as follows: (1) normal cell, no more than 2 copies/nucleus; (2) trisomic cells, 3 copies/nucleus; and (3) polysomic cell, at least 4 copies/nucleus. We also classified tumors according to the criteria reported by Cappuzzo et al. [9] (Table 3).
DNA extraction
FFPE samples with the greatest tumor area were selected and sliced into three 10-μm-thick sections. The tumor area of each section was macro dissected and DNA was extracted using a DNA FFPE tissue kit (Qiagen, Tokyo, Japan). We added RNase during DNA extraction, although this was an optional step according to the manufacturer’s protocol. The resulting DNA concentrations were at least 40 ng/μL in all of the extracted solutions.
Smart amplification process version 2 assay
The smart amplification process version 2 (SmartAmp2) assay EGFR mutation detection kit (DNAFORM, Japan) was used to determine the mutational status of EGFR in each sample [27–29]. This kit can detect some EGFR deletions of exon 19 and a point mutation of exon 21 (L858R). In accordance with the manufacturer’s instructions, the SmartAmp2 reactions were prepared on ice, and then incubated at 60 °C for 60 min. The Mx3000P system (Stratagene/Agilent Technologies, USA) was used to maintain isothermal conditions and monitor the transition in fluorescence intensity of the intercalating SYBR Green I during the reactions.
Statistical analysis
Correlations of EGFR expression with clinicopathologic characteristics, histopathologic features, and the expression of CK5/6, p-Akt, and p-mTOR were analyzed using χ 2 tests or Fisher’s exact test. We examined the correlations of EGFR expression with the Ki67 labeling index, and the numbers of normal cells, trisomic cells, and polysomic cells using the Mann–Whitney U test as these data were non-normally distributed according to the Shapiro–Wilk test. All analyses were conducted using SPSS software version 19 (SPSS Japan, Tokyo, Japan). Values of p less than 0.05 were regarded as statistically significant.
Results
EGFR expression and clinicopathologic characteristics
We compared the histological features of EGFR-positive and EGFR-negative TNBCs. Both groups of TNBCs had similar histological features, including the proportion of types A and B TNBCs (Table 4), high nuclear grade (p = 0.17), markedly elevated mitotic index (p = 0.19) and severe stromal lymphocytic response (p = 0.30). However, some histological differences were apparent among EGFR-positive and EGFR-negative TNBCs. Of note, EGFR-positive TNBCs were more frequently of type D, whereas EGFR-negative were more frequently of type C (Table 4). We found no differences in other clinicopathological factors, such as age (p = 0.80), tumor size (p = 0.45), and lymph node metastasis (p = 0.44).
EGFR expression and results of immunohistochemistry
EGFR expression was not correlated with CK5/6 expression (p = 0.53) or Ki67 labeling index (p = 0.90). Although p-Akt expression and p-mTOR expression were well correlated (p = 0.003), neither p-Akt (p = 0.20) nor p-mTOR (p = 0.20) was correlated with EGFR expression.
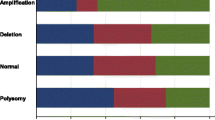
DISH analysis of EGFR gene
Representative images of DISH assays for FFPE TNBC samples are shown in Fig. 2. Single copies of the EGFR gene signal are indicated as individual black dots in the nuclei. Single copies of the chromosome 7 centromere are indicated as red dots that are slightly larger than the black dots corresponding to the EGFR gene in the nuclei. We successfully analyzed all 84 samples and the quality of the in situ hybridization was good.
Representative dual-color in situ hybridization (DISH) assays (bright field microscopy, ×1000 oil immersion) showing normal cells (a cells with black arrow), trisomic cells (b cells with black arrow), and polysomic cells (c cells with black arrow). Single copies of the chromosome 7 centromere are indicated as red dots (pointed to by red arrow) that are slightly larger than the black dots (pointed to by white arrow) corresponding to the EGFR gene in the nuclei. (Color figure online)
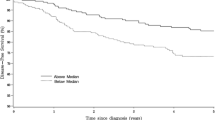
The EGFR gene was not amplified in any of the 84 samples. Among the 84 samples, disomy was detected in 28 (33.3 %), low trisomy in 30 (35.7 %), high trisomy in 2 (2.4 %), low polysomy in 18 (21.4 %), and high polysomy in 6 (7.1 %) (Table 5). EGFR expression was correlated with high polysomy (p = 0.014). We also analyzed correlations between EGFR expression and the numbers of normal cells, trisomic cells, and polysomic cells (Fig. 3). This analysis showed that EGFR expression was correlated with the number of polysomic cells (p = 0.009), but not with the number of trisomic cells (p = 0.19). The median number of polysomic cells was 4 % (range 0–88 %). If we limited the positive score based on the number of polysomic cells to at least 4 %, this parameter showed a strong correlation with EGFR expression (p = 0.005). EGFR expression was also negatively correlated with the number of normal cells (p = 0.029).
EGFR mutational analysis
Genomic DNA was extracted from 76 of 84 (90.5 %) TNBCs. Unfortunately, we could not macro dissect eight FFPE samples because we had difficulty obtaining three 10-μm-thick sections with a large tumor area. The SmartAmp2 assay and sequencing were successfully performed in 55 samples. Overall, our analysis showed that there were no mutations in these 55 samples.
Discussion
The present study demonstrated the following findings for TNBC tissues. First, EGFR expression was strongly correlated with the specialized type of breast cancer. Second, there was no EGFR gene amplification. Third, there were no EGFR-activating mutations. Fourth, EGFR expression was not correlated with p-Akt and p-mTOR expression. We discuss below each finding in detail.
In terms of EGFR expression in breast cancer, several studies have examined the clinical and pathological outcomes of EGFR expression in sporadic breast cancer and in TNBC. For example, Rimawi et al. [30] reported that EGFR expression is associated with lower hormone receptor levels, greater proliferation, genomic instability, and HER2 overexpression, and is correlated with increased risk of relapse in patients receiving adjuvant chemotherapy. Viale et al. [2] also reported that the extent of EGFR immunoreactivity is significantly correlated with prognosis of TNBC. Although some of the clinical features of TNBC expressing EGFR have already been described [2, 30], only a few studies have provided a complete description of the pathological features of these cancers. In this study, we found few differences between EGFR-positive and EGFR-negative TNBC in terms of clinicopathological and immunohistochemical characteristics. However, we found that TNBCs expressing EGFR were more likely to be of type D than of type C. These results indicate that, even though the pathological features of TNBCs expressing EGFR include certain types of TNBC (e.g., typical medullary carcinoma, metaplastic carcinoma, and adenoid cystic carcinoma), it is difficult to classify most TNBCs as EGFR-positive or -negative on the basis of clinical and histological findings.
We determined EGFR gene copy number in these TNBCs using DISH assays. Overall, 33 % of the TNBCs expressed EGFR. However, none of the tissue samples showed EGFR gene amplification. According to previous studies [12, 15, 17–19], EGFR gene amplification occurs in 1.6–21 % of TNBCs, which differs from our results. This contradiction may be due to differences in gene amplification methods, EGFR gene probes, and sample sizes between the earlier studies and our study. In our study, we used automated DISH assays, because the manual procedures used in the previous studies [12, 15, 17–19] show some limitations in terms of reproducibility in the analytical phase. Indeed, the new automated DISH assay may further improve reproducibility [26, 31, 32]. In addition, using the automated DISH assay, we could easily and accurately determine the chromosome 7 copy numbers. Measurement of numerical abnormalities in chromosome 7 may be important because they were found in several types of malignancy, including malignant mesothelioma, colorectal cancer, and NSCLC [33–35]. To date, however, few studies have examined the correlations between chromosome 7 copy numbers and the characteristics of breast cancer. In this study, we found that EGFR expression was significantly correlated with the number of polysomic cells and the presence of high polysomy of chromosome 7. This indicates that chromosome 7 polysomy frequently occurs in TNBC cells expressing EGFR. Although EGFR expression is statistically correlated with the number of chromosome 7 polysomic cells, we could not determine the one-to-one relationship between these factors in individual cells on continuous tissue sections under microscopic observation. Consequently, our DISH assay results suggest that EGFR might be expressed in the absence of gene amplification in TNBC and, therefore, there might be other molecular mechanisms. Zandi et al. [36] introduced in their review some of the mechanisms for EGFR expression, which include increased activity of the EGFR promoter or deregulation at the translational and post-translational levels. For example, p53 proteins have been shown to directly activate EGFR transcription by binding to a specific response site in the promotor. Ishikawa et al. [21] reported that p53 was expressed in 49.5 % of TNBC. Therefore, p53 may lead to continuous activation of the EGFR promoter in TNBC and thus receptor expression.
EGFR mutations occur in 5–40 % of all NSCLCs. Exon 19 deletions and the L858R mutation in exon 21 account for 85–90 % of all mutations in NSCLC [10]. These mutations exist around the ATP binding pocket of the EGFR tyrosine kinase domain [8] and mutations cause ligand-independent activation and increased activation duration of EGFR. Previous reports of sporadic breast cancer, metaplastic breast carcinoma, and Japanese TNBC [12–15] found no EGFR mutations in breast cancer. Similarly, we found no EGFR mutations in our series of TNBCs. To our knowledge, only one study has shown evidence of such mutations: in the study by Teng et al. [16], EGFR mutations were present in 11.8 % of TNBCs. However, as described in their report, differences in patient ethnicity and background characteristics may contribute to the differences in results among studies.
The Akt pathway regulates many different biological functions, including cellular proliferation, survival, and motility. Bose et al. [37] reported that there was no correlation between p-Akt expression and the expression of ER, PgR, and HER2, but p-Akt expression was correlated with p-mTOR expression. On the other hand, Aleskandarany et al. [38] reported that p-Akt expression was associated with ER expression, but not with EGFR expression. We found a rather significant correlation between p-Akt expression and p-mTOR expression, similar to that reported by Bose et al. [37], and found no correlation between p-Akt and EGFR, as reported by Aleskandarany et al. [38]. Our results suggest that the Akt pathway may regulate the biological functions of TNBCs, but activation of EGFR is not solely responsible for activation of the Akt–mTOR signaling pathway in TNBCs.
In conclusion, the present study showed that there were no EGFR gene amplification, no EGFR-activating mutation, and no correlation between EGFR expression and expression of components of the Akt pathway in TNBC expressing EGFR. EGFR gene amplification and EGFR-activating mutations might not be the mechanisms leading to the constitutive activation of EGFR in TNBC. Further investigation is needed to clarify the other molecular mechanisms for oncogenic activation of EGFR in TNBC.
References
Carey L, Winer E, Viale G, Cameron D, Gianni L. Triple-negative breast cancer: disease entity or title of convenience? Nat Rev Clin Oncol. 2010;7:683–92.
Viale G, Rotmensz N, Maisonneuve P, Bottiglieri L, Montagna E, Luini A, et al. Invasive ductal carcinoma of the breast with the “triple-negative” phenotype: prognostic implications of EGFR immunoreactivity. Breast Cancer Res Treat. 2009;116:317–28.
Alroy I, Yarden Y. The ErbB signaling network in embryogenesis and oncogenesis: signal diversification through combinatorial ligand–receptor interactions. FEBS Lett. 1997;410:83–6.
Liu W, Li J, Roth RA. Heregulin regulation of Akt/protein kinase B I breast cancer cells. Biochem Biophys Res Commun. 1999;261:897–903.
Roberts PJ, Der CJ. Targeting the Raf-MEK-ERK mitogen-activated protein kinase cascade for the treatment of cancer. Oncogene. 2007;26:3291–310.
McCubrey JA, Steelman LS, Chappel WH, Abrams SL, Wong EWT, Chang F, et al. Roles of the Raf/MEK/ERK pathway in cell growth, malignant transformation and drug resistance. Biochim Biophys Acta. 2007;1773:1263–84.
Altomare DA, Testa JR. Perturbations of the AKT signaling pathway in human cancer. Oncogene. 2005;24:7455–64.
Lynch TJ, Bell DW, Sordella R, Gurubhagavatula S, Okimoto RA, Brannigan BW, et al. Activating mutations in the epidermal growth factor receptor underlying responsiveness of non-small-cell lung cancer to gefitinib. N Engl J Med. 2004;350:2129–39.
Cappuzzo F, Hirsch FR, Rossi E, Bartolini S, Ceresoli GL, Bemis L, et al. Epidermal growth factor receptor gene and protein and gefitinib sensitivity in non-small-cell lung cancer. J Natl Cancer Inst. 2005;97:643–55.
John T, Liu G, Tsao MS. Overview of molecular testing in non-small-cell lung cancer: mutational analysis, gene copy number, protein expression and other biomarkers of EGFR for the prediction of response to tyrosine kinase inhibitors. Oncogene. 2009;28:S14–23.
Pal SK, Childs BH, Pegram M. Triple negative breast cancer: unmet medical needs. Breast Cancer Res Treat. 2011;125:627–36. doi:10.1007/s10549-010-1293-1.
Bhargava R, Gerald WL, Li AR, Pan Q, Lal P, Ladanyi M, et al. EGFR gene amplification in breast cancer: correlation with epidermal growth factor receptor mRNA and protein expression and HER-2 status and absence of EGFR-activating mutations. Mod Pathol. 2005;18:1027–33.
Reis-Filho JS, Pinheiro C, Lambros MB, Milanezi F, Carvalho S, Savage K, et al. EGFR amplification and lack of activating mutations in metaplastic breast carcinomas. J Pathol. 2006;209:445–53.
Generali D, Leek R, Fox SB, Moore JW, Taylor C, Chambers P, et al. EGFR mutations in exons 18–21 in sporadic breast cancer. Ann Oncol. 2007;18:203–5.
Toyama T, Yamashita H, Kondo N, Okuda K, Takahashi S, Sasaki H, et al. Frequently increased epidermal growth factor receptor (EGFR) copy numbers and decreased BRCA1 mRNA expression in Japanese triple-negative breast cancers. BMC Cancer. 2008;8:309.
Teng YH, Tan WJ, Thike AA, Cheok PY, Tse GM, Wong NS, et al. Mutations in the epidermal growth factor receptor (EGFR) gene in triple negative breast cancer: possible implications for targeted therapy. Breast Cancer Res. 2011;13:R35. doi:10.1186/bcr2857.
Kersting C, Tidow N, Schmidt H, Liedtke C, Neumann J, Boecker W, et al. Gene dosage PCR and fluorescence in situ hybridization reveal low frequency of egfr amplifications despite protein overexpression in invasive breast carcinoma. Lab Invest. 2004;84:582–7.
Park K, Han S, Shin E, Kim HJ, Kim JY. EGFR gene and protein expression in breast cancers. Eur J Surg Oncol. 2007;33:956–60.
Gumuskaya B, Alper M, Hucumenoglu S, Altundag K, Uner A, Guler G. EGFR expression and gene copy number in triple-negative breast carcinoma. Cancer Genet Cytogenet. 2010;203:222–9.
The Japanese Breast Cancer Society. Histological classification of breast tumor. In: General rules for clinical and pathological recording of breast cancer. 16th ed. Tokyo: Kanehara; 2008; p. 18–24.
Ishikawa Y, Horiguchi J, Toya H, Nakajima H, Hayashi M, Tagaya N, et al. Triple-negative breast cancer: histological subtypes and immunohistochemical and clinicopathological features. Cancer Sci. 2011;102:656–62. doi:10.1111/j.1349-7006.2011.01858.x.
Livasy CA, Karaca G, Nanda R, Tretiakova MS, Olopade OI, Moore DT, et al. Phenotypic evaluation of the basal-like subtype of invasive breast carcinoma. Mod Pathol. 2006;19:264–71.
Sasaki Y, Tsuda H. Clinicopathological characteristics of triple-negative breast cancers. Breast Cancer. 2009;16:254–9.
Tsuda H, Takarabe T, Hasegawa T, Murata T, Hirohashi S. Myoepithelial differentiation in high-grade invasive ductal carcinomas with large central acellular zones. Hum Pathol. 1999;30:1134–9.
Shousha S. Oestrogen receptor status of breast carcinoma: Allred/H score conversion table. Histopathology. 2008;53:346–7.
Nitta H, Hauss-Wegrzyniak B, Lehrkamp M, Murillo AE, Gaire F, Farrell M. Development of automated brightfield double in situ hybridization (BDISH) application for HER2 gene and chromosome 17 centromere (CEN 17) for breast carcinomas and an assay performance comparison to manual dual color HER2 fluorescence in situ hybridization (FISH). Diagn Pathol. 2008;3:41.
Mitani Y, Lezhava A, Kawai Y, Kikuchi T, Oguchi-Katayama A, Kogo Y, et al. Rapid SNP diagnostics using asymmetric isothermal amplification and a new mismatch-suppression technology. Nat Methods. 2007;4:257–62.
Hoshi K, Takakura H, Mitani Y, Tatsumi K, Momiyama N, Ichikawa Y, et al. Rapid detection of epidermal growth factor receptor mutations in lung cancer by the SMart-amplification process. Clin Cancer Res. 2007;13:4974–83.
Kawai Y, Kikuchi T, Mitani Y, Kogo Y, Itoh M, Usui K, et al. Sensitive detection of EGFR mutations using a competitive probe to suppress background in the SMart amplification process. Biologicals. 2008;36:234–8.
Rimawi MF, Shetty PB, Weiss HL, Schiff R, Osborne CK, Chamness GC, et al. Epidermal growth factor receptor expression in breast cancer association with biologic phenotype and clinical outcomes. Cancer. 2010;116:1234–42.
Francis GD, Jones MA, Beadle GF, Stein SR. Bright-field in situ hybridization for HER2 gene amplification in breast cancer using tissue microarrays: correlation between chromogenic (CISH) and automated silver-enhanced (SISH) methods with patient outcome. Diagn Mol Pathol. 2009;18:88–95.
García-García E, Gómez-Martín C, Angulo B, Conde E, Suárez-Gauthier A, Adrados M, et al. Hybridization for human epidermal growth factor receptor 2 testing in gastric carcinoma: a comparison of fluorescence in-situ hybridization with a novel fully automated dual-colour silver in-situ hybridization method. Histopathology. 2011;59:8–17. doi:10.1111/j.1365-2559.2011.03894.x.
Shin HJ, Shin DM, Tarco E, Sneige N. Detection of numerical aberrations of chromosomes 7 and 9 in cytologic specimens of pleural malignant mesothelioma. Cancer. 2003;99:233–9.
Li YH, Wang F, Shen L, Deng YM, Shao Q, Feng F, et al. EGFR fluorescence in situ hybridization pattern of chromosome 7 disomy predicts resistance to cetuximab in KRAS wild-type metastatic colorectal cancer patients. Clin Cancer Res. 2011;15(17):382–90. doi:10.1158/1078-0432.CCR-10-0208.
Buckingham LE, Coon JS, Morrison LE, Jacobson KK, Jewell SS, Kaiser KA, et al. The prognostic value of chromosome 7 polysomy in non-small cell lung cancer patients treated with gefitinib. J Thorac Oncol. 2007;2:414–22.
Zandi R, Larsen AB, Andersen P, Stockhausen MT, Poulsen HS. Mechanisms for oncogenic activation of the epidermal growth factor receptor. Cell Signal. 2007;19:2013–23.
Bose S, Chandran S, Mirocha JM, Bose N. The Akt pathway in human breast cancer: a tissue-array-based analysis. Mod Pathol. 2006;19:238–45.
Aleskandarany MA, Rakha EA, Ahmed MA, Powe DG, Ellis IO, Green AR. Clinicopathologic and molecular significance of phospho-Akt expression in early invasive breast cancer. Breast Cancer Res Treat. 2011;127:407–16. doi:10.1007/s10549-010-1012-y.
Acknowledgments
We thank Ms. A. Katayama (MD-PhD course student, Gunma University Faculty of Medicine), Dr. T. Hikino, Dr. M.Saito, and Mr. F. Hara (Department of Diagnostic Pathology, Gunma University Graduate School of Medicine) for their excellent technical assistance.
Conflict of interest
The authors have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Nakajima, H., Ishikawa, Y., Furuya, M. et al. Protein expression, gene amplification, and mutational analysis of EGFR in triple-negative breast cancer. Breast Cancer 21, 66–74 (2014). https://doi.org/10.1007/s12282-012-0354-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12282-012-0354-1