Abstract
Background
We aimed to evaluate the application of apparent diffusion coefficient (ADC) values calculated from diffusion-weighted imaging (DWI) (b value = 1500 s/mm2) in the breast imaging reporting and data system (BI-RADS).
Methods
For 104 cases of breast lesions with definitive histology diagnosis (45 benign cases, 59 malignant cases) in which breast magnetic resonance imaging was performed, ADC values were compared between benign and malignant cases, between ductal carcinoma in situ (DCIS) and fibrocystic changes, and between DCIS and ductal hyperplasia (one type of fibrocystic change). Diagnostic accuracy was compared for a total of 101 images and for 34 images including only nine DCIS and 25 fibrocystic changes between BI-RADS alone (with categories 4a, 4b, and 5 defined as malignancies) and BI-RADS plus ADC.
Results
There were significant differences in mean ADC values between malignant and benign cases (p < 0.0001) and between DCIS and fibrocystic changes (p < 0.002), but not between DCIS and ductal hyperplasia. Positive predictive values were significantly greater for BI-RADS plus ADC than for BI-RADS alone in all cases (70.5% for BI-RADS alone, 81.3% for BI-RADS plus ADC) and in cases of DCIS versus fibrocystic changes (40.9% for BI-RADS alone, 64.3% for BI-RADS plus ADC), resulting in a significant improvement in diagnostic accuracy with the addition of ADC.
Conclusion
Adding ADC values calculated from DWI (b value = 1500 s/mm2) to BI-RADS is a useful way to improve differential diagnostic accuracy for malignant tumors and benign lesions, especially for DCIS versus fibrocystic changes, except in cases of ductal hyperplasia.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Many reports on the usefulness of adding diffusion-weighted imaging (DWI) to the results of magnetic resonance imaging (MRI), dynamic curve analysis, and the breast imaging reporting and data system (BI-RADS) [1] in diagnosis of breast cancer have been published [2–10]. However, the b values for DWI used in those studies are not consistent among the reports. Kuroki et al. [9] recommended b values of 0 and 1000 s/mm2, whereas others reported the usefulness of b values of 0 and 1500 s/mm2.
However, there is little study using b values of 0 and 1500 s/mm2. In previous reports using b = 1000 s/mm2 or less, specificity was low as compared with sensitivity, and it is possible that many mastopathies could have caused false positives [2, 3, 5, 6, 8]. On the other hand, because the signal of the surrounding mammary gland tissue decreases at b value of 1500 s/mm2 as compared with b value of 1000 s/mm2 or less [9, 13], b value of 1500 s/mm2 may be useful for excluding mastopathies.
Although a report assessing the combination of BI-RADS and ADC with b value of 1500 s/mm2 was previously published [4], we compare its ability to diagnose ductal carcinoma in situ (DCIS) versus fibrocystic change and DCIS versus ductal hyperplasia in addition to benignity versus malignancy in the present study. It would be especially useful to establish the ability to distinguish between DCIS and mastopathies. In this study we investigate whether adding apparent diffusion coefficient (ADC) values calculated from DWI with b values of 0 and 1500 s/mm2 could improve the diagnostic accuracy of BI-RADS.
Materials and methods
The study included 219 patients who underwent breast MRI in our hospital from May 2009 to April 2010 after breast cancer was suspected based on ultrasonography and/or mammography (MMG). We ensured that MRI was performed preoperatively. Only one case was a recurrence after postoperative chemotherapy. The study subjects included 104 cases of mammary lesions with definitive histology diagnosis (45 benign and 59 malignant cases) in which ADC values were calculable. Forty-five benign lesions indicated high signal intensity on DWI, and pathological diagnosis was decided by US-guided biopsy. Average patient age was 55.3 years (range 13–92 years), and average lesion diameter was 21.1 mm (range 4–87 mm). Based on histological analysis, 45 cases were categorized as benign lesions [two phyllodes tumors, 25 fibrocystic changes (seven cases of ductal hyperplasia, 18 cases of other types of fibrocystic change), three cases of mastitis, four intraductal papillomas, one ductal ectasia, six fibroadenomas, four cases of normal breast tissue (no malignancy findings)] and 59 as malignant [two mucinous carcinomas, one medullary carcinoma, seven invasive lobular carcinomas, six invasive papillary carcinomas, 34 invasive ductal carcinomas, and nine ductal carcinomas in situ (DCIS)] (Tables 1, 2).
All MRI was performed on a Signa HDxt 1.5-T device (GE Healthcare Co. Ltd.) with a 1.5 HD Breast Array coil (8 ch) in the protocol order of diffusion-weighted imaging (DWI, axial), fat-suppressed T2-weighted imaging (FS T2WI, axial), dynamic study (3D, coronal), and contrast-enhanced fat-suppressed T1-weighted imaging (CE FS T1WI, axial) for bilateral breasts. The detailed conditions for each protocol were as follows. DWI: imaging section orientation, axial; TR/TE, 6900/75.5 ms; field of view (FOV), 36 cm; slice thickness, 5 mm; matrix, 128 × 128; gap, 0 mm; NEX, 6; scan duration, 6 min. FS T2WI: imaging section orientation, axial; TR/TE, 3500/82 ms; flip angle, 90°; FOV, 36 cm; slice thickness, 5 mm; matrix, 320 × 192; gap, 2 mm; NEX, 2; scan duration, 2 min. Dynamic study was performed using spoiled gradient recalled acquisition in the steady state (SPGR): imaging section orientation, coronal; TR/TE, 2.3/0.8 ms; flip angle, 10°; FOV, 36 cm; slice thickness, 2.0–3.6 mm; matrix, 256 × 128, precontrast, 40, 80, 120, 180, 300 s; gap, 0 mm; NEX, 2; scan duration, 6.5 min. Dynamic images were acquired at 40 s. For dynamic MRI, meglumine gadopentetate (MEGLUMINE GADOPENTETATE; Taiyo. Co. Ltd., Japan) and gadodiamide hydrate (OMNISCAN; Daiichi-Sankyo. Co. Ltd., Japan) was administered intravenously at rate of 1.5 ml/s (0.2 ml/kg body weight) using automatic injector followed by 40 ml saline flush. CE FS T1WI: imaging section orientation, axial; TR/TE, 450/10.3 ms; flip angle, 90°; FOV, 36 cm; slice thickness, 5 mm; matrix, 320 × 192; gap, 2 mm; NEX, 2; scan duration, 4 min.
In this investigation, the mean ADC value was obtained from three measured sites in the region of interest (ROI) of each lesion except for microlesions (3 mm or less in diameter), excluding cyst components in the lesion except in the case of mucinous carcinoma. The ROI was determined to be as large as 10 mm2 or greater. BI-RADS categories were determined based on the consensus of two certified radiologists. The details of the investigations were as follows. We did not refer to the category of US or MMG, or clinical information, but diagnosed using only MRI (BI-RADS [1]).
The lesion detection capability of DWI (b value = 1500 s/mm2) was compared with results in published reports. ADC values were compared between benign and malignant lesions, between DCIS and fibrocystic changes, and between DCIS and mammary ductal hyperplasia (one type of fibrocystic change). In this investigation, the ADC values for DCIS were obtained from as large an area as possible that demonstrated increased contrast strength and in which ADC values were measurable, although some parts of normal mammary glands and adipose tissues around the lesion might potentially be included. The lesions that we evaluated in the investigation included fibrocystic changes (ductal hyperplasia or other types of fibrocystic change) in which malignancy was originally suspected but for which subsequent biopsy produced a final benign diagnosis. Student’s t test and the Mann–Whitney U test were applied to compare ADC values between benign and malignant cases and between DCIS and fibrocystic changes, respectively.
Comprehensive statistical analysis software, Dr. SPSS II for Windows, was used for statistical analysis.
Results
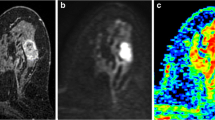
Of the 59 contrast-enhanced (CE) MRI images of the lesions diagnosed histologically as malignant tumors, all were also detectable by DWI. However, some parts of the lesions were undetectable by DWI in cases of invasive lobular carcinoma (Fig. 1) and DCIS (Fig. 2). Four lesions among the benign cases in which biopsy was performed unnecessarily (one fibroadenoma, two diabetic fibrocystic changes, and one fibrocystic change) were undetectable by DWI.
Lobular carcinoma from a female in her 60s. a Contrast-enhanced MRI image: an extensive area with increased contrast strength is shown (arrows). b DWI: signals are diffuse and slightly high, and partially strong signals (arrows) are confirmed. c The ADC map shows a slight decrease in ADC levels in limited areas (arrows). d Histology: lobular carcinoma. The lesion area is 70 × 65 mm2. Invasive carcinoma lesions of various sizes are scattered extensively throughout the tissue. Isolated carcinoma cells with poor cell-to-cell adhesion infiltrate into adipose and stromal tissues (arrow)
DCIS to ductal carcinoma from a female in her 50s. a Contrast-enhanced MRI image: nonsegmental and branched areas of contrast strength are observed (arrows). b DWI: strong signals are confirmed generally, but some areas do not show strong signals (arrows). c The ADC map demonstrates a decrease in ADC levels (arrows). d Histology: DCIS to ductal carcinoma. Atypical cells with condensed nuclei form papillomatous to ductal and solid honeycomb-pattern lesions in the dilated mammary ducts (arrows)
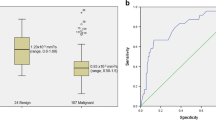
The mean ADC value of malignant lesions was 0.90 ± 0.18 × 10−3 mm2/s, while the mean ADC value of benign lesions was 1.21 ± 0.29 × 10−3 mm2/s (Tables 1, 2), showing a significant difference (p < 0.0001) (Fig. 3). There was also a significant difference in ADC values between DCIS (0.92 ± 0.19 × 10−3 mm2/s) and all fibrocystic changes (1.18 ± 0.29 × 10−3 mm2/s) (p = 0.002). However, there was no significant difference in ADC values between DCIS and only ductal hyperplasia cases among fibrocystic changes (1.05 ± 0.16 × 10−3 mm2/s).
After excluding four outlier cases showing extremely high ADC values (two cases of mucinous carcinoma, one case of invasive lobular carcinoma, and one case of invasive ductal carcinoma observed within fibroadenoma) the highest ADC value among all malignant cases, 1.11 × 10−3 mm2/s, was set as a threshold value for differential diagnosis of malignancies compared with benign cases. When 1.11 × 10−3 mm2/s was set as a threshold, the sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) for differential diagnosis between malignant and benign lesions were 93.2, 55.6, 73.3, and 86.2%, respectively.
Compared with BI-RADS categorization alone (categories 4a, 4b, and 5), adding ADC to BI-RADS (Table 3, I–III) improved the specificity, accuracy, and PPV for both the analysis of all cases (Table 4) and the analysis of DCIS and fibrocystic changes (Table 5). In the nine cases of DCIS, high-grade DCIS accounted for eight of nine and low-grade DCIS for one. In subspecific type, there was much solid, papillary, and cribriform type, with low papillary type in only one case (Table 6).
Discussion
Many reports have demonstrated the usefulness of DWI in breast MRI [2–10]. However, it has been reported that the ranges of ADC values overlap between benign lesions (fibrocystic changes, mastitis, ductal ectasia, and papilloma) and malignant lesions (invasive lobular carcinoma, noninvasive ductal carcinoma, etc.) [5]. In addition, various b values have been used in different facilities. Although Kuroki et al. [9] recommended b values of 0 and 1000 s/mm2, elsewhere b values of 0 and 1500 s/mm2 have been reported to be necessary to suppress strong contrast for some fibrocystic changes. Tozaki et al. [4] reported that eight out of 91 malignant cases were undetectable with b values of 0 and 1500 s/mm2 (detection rate 91.2%; 83 out of 91 cases), and all of these undetectable cases were DCIS. Yabuuchi et al. [3] reported that the detection rate with b values of 0 and 1000 s/mm2 was 94.2%. Nakajima et al. [10] carried out evaluations using b values of 0 and 1000 s/mm2, and the detection rate by DWI was 95% (98 out of 103 cases).
In our study, all 59 malignant cases that were detected by MRI and diagnosed histologically were also detectable by DWI. However, some parts of the lesions were undetectable by DWI in cases of invasive lobular carcinoma (Fig. 1) and DCIS (Fig. 2). On the other hand, CE MRI was able to detect broader lesions. Therefore, our evaluation of DWI with b values of 0 and 1500 s/mm2 demonstrated superior detection capability for breast carcinoma compared with previous reports, but it was not sensitive enough to evaluate the lesion distribution in cases of invasive lobular carcinoma and noninvasive ductal carcinoma.
Van den Bosch et al. [11] reported that fibrocystic changes showed various patterns of morphology and dynamic curves, leading to initial MRI findings suggesting suspected malignancies in five out of 14 cases. Yabuuchi et al. [8] examined 22 non-mass-like enhancement lesions and determined that 15 cases were malignant (including eight noninvasive ductal carcinomas) and that seven were benign (all fibrocystic changes). Five of the seven benign lesions were categorized as BI-RADS American College of Radiology (ACR) category 4. Furthermore, Chen et al. [12] reported that MMG and sonography revealed false-positive results for malignancies in 55% (six out of 11 cases) and 70% (seven out of 10 cases) of focal fibrocystic changes, respectively. In contrast, MRI showed BI-RADS categories 4 or 5 in 82% (nine out of 11 cases) of focal fibrocystic changes (overdiagnosis). Therefore, it is difficult to distinguish fibrocystic changes from noninvasive ductal carcinoma on MRI, resulting in a high rate of false-positive diagnosis of malignancies. Nagasawa et al. [13] reported that the greatest contrast-to-noise ratio between malignant lesions and normal mammary glands was obtained with b values of 0 and 1500 s/mm2 in comparison with b values of 0 and 1000 s/mm2 or less. In cases of DCIS and DCIS primary carcinomas, the intensity in the surrounding normal tissue is expected to decrease with b values of 0 and 1500 s/mm2 more apparently than with b values of 0 and 1000 s/mm2 or less, indicating the superiority of using b values of 0 and 1500 s/mm2. Based on these previous reports, we selected b values of 0 and 1500 s/mm2 and compared the ADC values between DCIS and fibrocystic changes, particularly to distinguish noninvasive ductal carcinomas from fibrocystic changes.
Although most fibrocystic changes do not increase the risk of progression to invasive breast carcinoma, sclerosing adenosis, papilloma, moderate to marked ductal hyperplasia (duct papillomatosis), and mastopathic fibroadenoma have been reported as risk factors for carcinoma (1.5- to 2-fold increase) [14]. In our investigation, there were no cases of sclerosing adenosis or mastopathic fibroadenoma, and few papilloma cases; therefore, we examined ductal hyperplasia associated with the fibrocystic changes and all cases of fibrocystic changes. As a result, there was a statistically significant difference in ADC values between DCIS cases and all cases of fibrocystic change (p = 0.002). In contrast, the ADC values only in the ductal hyperplasia cases were not significantly different from the ADC values in DCIS cases. These results suggest that ADC measurement with b values of 0 and 1500 s/mm2 may be useful for distinguishing DCIS and ductal hyperplasia, which could be risk factors for invasive carcinoma, from other types of fibrocystic changes with no risk of carcinoma.
Partridge et al. [6] reported that applying an ADC threshold of 1.81 × 10−3 mm2/s for 100% sensitivity to DCE MRI (BI-RADS categories 4 or 5) produced PPV of 47% compared with 37% for DCE MRI alone. This addition of ADC thus would have prevented the performance of unnecessary biopsy. In our investigation, in a comparison between fibrocystic changes and DCIS under 100% sensitivity, PPV increased with the addition of the ADC value by 23.4% (64.3% in BI-RADS plus ADC compared with 40.9% in BI-RADS alone) (Table 5). This degree of improvement in PPV was greater than the increase in PPV between benign and malignant lesions in general (10.8% increase; 81.3% compared with 70.5%), indicating the usefulness of including the ADC value, especially for differential diagnosis between fibrocystic change and DCIS. The diagnostic ability of DCIS was high in our study; on histology of nine DCIS (Table 6), high-grade DCIS were dominant and did not correlate with the degree of grade. On the other hand, in subspecific type, there was much solid, papillary, and cribriform type, with low papillary type in only one case. This may be related to the reason why diagnostic ability was high.
For breast MRI, the guideline issued by the European Society of Breast Imaging (EUDOBI) [15] has been recommended in Japan. Although it has not been included in routine medical practice, many reports have indicated that DWI is a promising tool; therefore, establishing a standard procedure for DWI, including the optimal b values, is an important goal.
Conclusions
We evaluated the application of ADC values calculated from DWI with b value of 1500 s/mm2 in BI-RADS for differential diagnosis of breast carcinoma. Adding ADC values to BI-RADS improved the accuracy of differential diagnosis between malignant tumors and benign lesions, especially for DCIS versus fibrocystic changes.
References
American College of Radiology. Breast imaging reporting and data system (BI-RADS). 4th ed. Reston: American College of Radiology; 2003.
Nakashima K, Sugahara T, Ito K, Nakamura S, Baba Y, Saito R. Usefulness of diffusion-weighted imaging in characterizing breast lesions. Jpn J Magn Reson Med. 2008;28(2):154–61.
Yabuuchi H, Matsuo Y, Kamitani T, Setoguchi T, Hatakenaka M, Sakai S, et al. Differential diagnosis capability between benign and malignant breast tumors by the combination of dynamic contrast-enhanced MRI and diffusion-weighted imaging: assessment with ROC analysis. Med Imaging Inf. 2007;39(10):930–5.
Tozaki M, Fukuma E. 1H MR spectroscopy and diffusion-weighted imaging of the breast: are they useful tools for characterizing breast lesions before biopsy? Am J Roentgenol. 2009;193:840–9.
Woodhams R, Marsunaga K, Kan S, Hata H, Ozaki M, Iwabuchi K, et al. ADC mapping of benign and malignant breast tumors. Magn Reson Med Sci. 2005;4(1):35–42.
Partridge SC, De Martini WB, Kurland BF, Eby PR, White SW, Lehman CD. Quantitative diffusion weighted imaging as an adjunct to conventional breast MRI for improved positive predictive value. Am J Roentgenol. 2009;193:1716–24.
Yabuuchi H, Matsuo Y, Okafuji T, Kamitani T, Soeda H, Setoguchi T, et al. Enhanced mass on contrast-enhanced breast MR imaging: lesion characterization using combination of dynamic contrast-enhanced and diffusion-weighted MR dynamic contrast-enhanced and diffusion-weighted MR images. J Magn Reson Imaging. 2008;28(5):1157–65.
Yabuuchi H, Matsuo Y, Kamitani T, Setoguchi T, Okafuji T, Soeda H, et al. Non-mass-like enhancement on contrast-enhanced breast MR imaging: lesion characterization using combination of dynamic contrast-enhanced and diffusion-weighted MR images. Eur J Radiol. 2010;75(1):126–32.
Kuroki Y, Nasu K, Kuroki S, Sekiguchi R. Application of diffusion-weighted imaging to MR mammography: basics. Jpn Dtsch Med Beriche. 2008;53(2):292–6.
Nakajima M, Nitori T, Matsuda M, Fukushima H, Iihara K, Seki Tl. Clinical application of MRI echoplanar diffusion-weighted imaging (EPI-DWI) for breast cancer diagnosis. Jpn J Med Imaging. 2008;27:9–21.
van den Bosch MA, Daniel BL, Mariano MN, Nowels KN, Biedwell RL, Fong KJ, et al. Magnetic resonance imaging characteristics fibrocystic change of the breast. Invest Radiol. 2005;40(7):436–41.
Chen J-H, Nalcioglu O, Su M-Y. Fibrocystic change of the breast presenting as a focal lesion mimicking breast cancer in MR imaging. J Magn Reson Imaging. 2008;28(6):1499–505.
Nagasawa K, Takahashi K, Inaoka T, Yamada A, Hiranuma H, Sakuma A, et al. Investigation of the application of diffusion-weighted imaging with high b-value in breast cancer. Med Imaging Inf. 2007;39(10):940–3.
Tsuchiya S, Akiyama F, Moritani T. Color atlas of pathology in mammary gland. Tokyo: Bunkodo; 2008.
Mann RM, Kuhl CK, Kinkel K, Boestes C. Breast MRI: guideline from the European Society of Breast Imaging. Eur Radiol. 2008;18:1307–18.
Acknowledgments
The authors thank Ms. Miyako Tominaga for her editorial assistance.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Ochi, M., Kuroiwa, T., Sunami, S. et al. Diffusion-weighted imaging (b value = 1500 s/mm2) is useful to decrease false-positive breast cancer cases due to fibrocystic changes. Breast Cancer 20, 137–144 (2013). https://doi.org/10.1007/s12282-011-0319-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12282-011-0319-9