Abstract
Purpose of Review
To provide an overview of the diagnostic tests available to identify invasive fungal disease (IFD) in children with a primary immunodeficiency and to evaluate the relative strengths and weaknesses of those tests.
Recent Findings
Novel tools to aid the diagnosis of IFD, such as fungal PCRs and lateral flow devices (for Aspergillus spp.), are emerging. However, the paucity of high-quality, multicentre clinical trials evaluating the performance of these diagnostic tools, particularly in the paediatric cohort of interest, remains a challenge. Children with primary immunodeficiencies are seldom referenced in existing studies.
Summary
It is difficult to provide recommendations for the majority of fungal diagnostic tests, with the exception of histopathology, microscopy, culture, and imaging modalities, due to their poorly studied and largely unvalidated nature. Moving forward, multicentre trials considering the role of these tools in the investigation of children with probable IFD and a primary immunodeficiency are strongly encouraged.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In the current era of innovative medical science, it is anticipated that most children born with a primary immunodeficiency will enjoy a near-normal life expectancy. To achieve this, early diagnosis of infection is crucial. Invasive fungal disease (IFD) is more frequently encountered in children with a primary immunodeficiency than in the general paediatric population: 85% of children with STAT3 deficiency and hyper-IgE syndrome present with chronic mucocutaneous candidiasis and CARD9 deficiency predisposes to aspergillosis and deep dermatophytosis [1, 2]. Table 1 provides an overview of, some of the more frequently encountered, primary immunodeficiencies and the fungal pathogens which can opportunistically cause infection in these conditions.
The clinical relevance of fungal infection, particularly in immunodeficient patients, is increasingly appreciated by paediatricians. Yet, diagnosing these infections is more challenging than one might think. This is because there are many diagnostic tools and procedures that are not ‘child-friendly’ and sample volumes obtained from children are often much smaller, limiting the number of tests available. Additionally, many novel diagnostic methods, such as molecular markers, are not validated for paediatric patients and must be interpreted with caution.
As has been the case for many years, identification of a fungal pathogen either on biopsy of the affected organ, termed ‘histopathological diagnosis’, or on microscopy and culture of blood/bodily fluid remains gold standard [10•]. Alongside these more ‘conventional’ diagnostic tools, we might also consider imaging modalities such as computed tomography (CT). CT imaging has consistently been proven to be of value in the diagnosis of invasive fungal disease (IFD), particularly aspergillosis [11].
Over the last decade, novel molecular tools such as the biomarkers 1,3-β-d-glucan, Candida mannan and galactomannan, and species-specific and pan-fungal PCRs have emerged in paediatric mycology practice. These have been employed in an effort to expedite the diagnostic process. However, clinician confidence in the interpretation of results yielded from molecular tools, and the usefulness of these results, differs in paediatric patients when compared with adults.
Regardless of the diagnostic tools employed, the presence of either direct (positive culture or histopathology) or indirect (positive biomarker) evidence of mycological infection is sufficient to escalate classification from ‘possible’ to ‘probable’ fungal disease [10•]. This is as per the European Organization for Research and Treatment of Cancer/Invasive Fungal Infections Cooperative Group (EORTC) guideline which comprehensively defines IFD [10•].
The purpose of this review article is to provide the reader with an up-to-date account of recent developments in the field of fungal diagnostics, whilst also acknowledging the benefits of more conventional methods of isolating fungal pathogens. The reader should gain an understanding of how best to approach and investigate a child with primary immunodeficiency and suspected fungal infection. Reference will be made to relevant paediatric guidelines, namely, but not exclusively, those endorsed by the European Society of Clinical Microbiology and Infectious Diseases (ESCMID).
Conventional Diagnostic Tools
Culture and Histopathology
The 2017 ESCMID-ECMM-ERS document, not principally a paediatric-focused guideline but inclusive of recommendations for children, states that for patients at risk of invasive aspergillosis (IA), microscopy and culture, and/or histopathological examination, should be attempted on appropriate clinical specimens [12••]. Appropriate clinical specimens would include blood, albeit Aspergillus spp. are seldom isolated from blood culture and may be considered contaminants, bronchoaleveolar lavage fluid, and tissue samples from deep sites. If hyphae are observed under direct microscopy of deep site samples, this is indicative of ‘proven’ fungal infection. Sensitivity of direct microscopy for IA is poor, at around 50–70%, but use of calcofluor white (note this is not Aspergillus specific) and staining with periodic acid-Schiff or Gomori’s methenamine silver enhances sensitivity [12••, 13].
For candidiasis, blood culture currently remains a central component of the diagnostic work-up [14]. The sample volume is important. ESCMID suggests that three serial blood cultures of between 2 ml, for children weighing < 2 kg, and 6 ml, for those > 2kg, increases culture sensitivity from 25–30% to 50–75% [15•]. In clinical practice, obtaining blood culture samples of the ESCMID-advised volume from paediatric patients is challenging. It is also true that in deep-seated candida infection, blood cultures will often be negative.
One does encounter more unusual fungal pathogens when managing children with primary immunodeficiencies [16]. Helpfully, many of these, such as the Mucorales, Scedosporium spp., Trichocomaceae spp., and Fusarium spp., can be identified on histopathological examination and culture, provided appropriate specimens are obtained.
Understandably, the prospect of bronchoscopy, bronchoalveolar lavage (BAL) or image-guided biopsy to obtain deep-site tissue samples, in order to facilitate histopathology and culture, from a child is daunting. This practice continues to be advised as it has been shown that, provided experienced interventionalists are available, the benefits of confirming the causative fungal pathogen, particularly in IA, and initiating targeted therapy more often outweigh the risks [17,18,19]. It is, of course, acknowledged that there will be instances when a child is too severely unwell to undergo invasive sampling and alternative means of diagnosis must be sought.
More innovative approaches to obtaining samples for culture are emerging. Fujita et al. report on a 2-month-old boy with chronic granulomatous disease (CGD) who was diagnosed with Rasamsonia piperina fungal pneumonia using gastric aspirate culture, a relatively non-invasive procedure [20•]. Although only a single case report, the authors suggest culture of gastric aspirate provides a means of diagnosing fungal infection in infants with respiratory symptoms and primary immunodeficiency without the need for bronchoscopy.
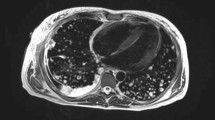
Imaging
The role of computed tomography (CT) in the diagnosis of IA, or indeed any mould that causes infection localised to the lungs, is well established. The ESCMID-ECMM-ERS guideline advises ‘thin-section’ chest CT as the imaging modality of choice for patients at risk of IA and with clinical signs suggestive of the same [12••]. Where this is not feasible, pulmonary MRI has been suggested as an alternative [21, 22]. Given the atypical presentation pattern of invasive mould infection in immunodeficient children, it would be prudent to also include the paranasal sinuses in any scheduled chest imaging study [23•].
On chest CT, the classical features of halo sign (in the early phases of infection), reverse halo sign, nodules of > 1 cm diameter, alveolar consolidation, air-crescent sign, and centrilobular nodules with tree-in-bud appearance should be observed in IA and may be observed with other invasive moulds [24,25,26]. Unfortunately, in children, many of these features are not observed and it has long been proposed that any new CT changes should prompt the clinician to consider IFD and initiate antifungal treatment [11].
For select patient groups in whom IFD is considered probable rather than possible, for example those with a severe inherited primary immunodeficiency (CGD or severe combined immunodeficiency SCID), clinical features of IFD and/or who meet specific mycological criteria such as positive biomarkers, it might also be reasonable to consider CT or MRI brain [10•]. This is particularly important in the setting of mould-active prophylaxis which can encourage the emergence of indolent and atypical fungal pathogens [27,28,29]. Mould-active prophylaxis has become increasingly commonplace in the management of children with primary immunodeficiency, specifically CGD. Haidar et al. describe a young man with X-linked CGD, taking prophylactic posaconazole, who presented with disseminated Phellinus tropicalis of the lungs and brain [29]. De Ravin et al. outline a similar case involving a 10-year-old boy with CGD, prescribed prophylactic itraconazole, who subsequently developed a paraspinal fungal mass attributed to Phellinus spp. [30•]. Thus, whilst central nervous system (CNS) imaging is not mandated in any published guideline, unless localising signs are present, it is important to remember that CNS manifestations of fungal disease occur more frequently in vulnerable patients. Early diagnosis improves outcome and clinicians should remain vigilant in their diagnostic efforts to exclude fungal CNS disease.
Selective imaging is important for invasive yeast infections too. According to the Infectious Diseases Society of America, the diagnostic work-up for neonates with invasive candidiasis should include ultrasound or CT imaging of the GI tract, liver, and spleen, particularly in cases with persistent blood culture positivity [31].
Both the ESCMID and the European Conference on Infections in Leukaemia (ECIL-4) guidelines advise all paediatric patients, not exclusively neonates, with proven candidaemia should be imaged looking for deep sites of infection [15•, 32••, 33•]. Their preferred imaging modality is not stated. Whilst the ECIL-4 guideline considers children with an underlying malignancy, not a primary immunodeficiency, the degree of concordance across published European mycology guidelines is important to highlight. It reflects clinician awareness that difficult to treat, deep-seated, Candida infections are more common in children. Most paediatricians would consider, in line with ESCMID, that deep site infection should be actively excluded in children with candidiasis, by employing appropriate imaging modalities such as CT, MRI, or ultrasound.
Novel Diagnostic Tools
The advantage of these tools is that they require minimally invasive procedures to obtain a test specimen. Most can be measured on peripheral blood and are routinely incorporated into clinical practice in adult medicine. They are promising adjuncts in the field of paediatric mycology.
Biomarkers
Table 2 outlines the fungal pathogens that can be detected using the current armoury of biomarkers.
β-d-glucan
1,3-β-d-glucan is present as a cell-wall component in most clinically relevant, pathogenic fungi including Pneumocystis jiroveci, Aspergillus spp., and Candida spp [10•, 39]. It should, however, be remembered that it is not present in the cell wall of certain, more uncommon but equally pathogenic, fungal species such as Cryptococcus spp. or zygomycetes.
In adult patients, there is consensus opinion that detection of β-d-glucan in the serum is an effective screening test for IFD. The EORTC recommends its use in immunodeficient adults [10•]. Conversely, paediatric guidelines regarding β-d-glucan are lacking and opinions on the usefulness of the test are varied [10•, 31, 40]. There are no published guidelines which advocate the use of β-d-glucan as a screening or diagnostic tool for fungal infection in children with primary immunodeficiency. The ECIL-4 guideline mentions β-d-glucan but suggests one should not base clinical decisions upon the test result [33•].
The appropriate cutoff for a positive assay is also debated. The adult cutoff of 80 pg/ml is considered inappropriate for paediatric patients as children unaffected by IFD have baseline serum β-d-glucan levels up to one-third higher than adults [41].
Calitri et al. evaluated β-d-glucan performance in a tertiary paediatric Italian hospital [42••]. All screened patients had risk factors for IFD, including primary immunodeficiency, and clinical features suggestive of IFD, although decision to screen was at the discretion of the consulting clinician. A total of 1577 samples from 255 patients were analysed. The authors found that β-d-glucan sensitivity was always < 0.80 and that specificity only reached > 0.90 if higher cutoff values for positivity, a level of > 200 pg/ml, were employed [42••]. A corresponding increase in specificity with an increase in the pg/ml cutoff for positivity has been observed in previous studies [43•]. This highlights the importance of interpreting positive β-d-glucan results in the context of the cutoff value chosen by local laboratories.
In the Calitri study, negative predictive value was high at > 0.90 but positive predictive value was only 0.50. It is reasonable, therefore, to suggest that a negative β-d-glucan test is of value, caution surrounds this statement as low overall incidence of IFD impacts the relevance of high negative predictive values, but that a positive test is of lesser significance [42••].
Dependent on the β-d-glucan assay employed, false-positive results may be observed due to blood product transfusion, haemodialysis, and antibiotics including piperacillin-tazobactam, mucositis, and surgical gauze [7, 43•]. Further, the time frame in which β-d-glucan levels may fall after treatment of IFD is largely unknown and studies have reported elevated levels despite evidenced clearance of infection [44].
The reported difficulties surrounding the interpretation of β-d-glucan should not be ignored but it must be stressed that much of the data to date has arisen from single-centre studies and case reports. Multicentre studies are ongoing and will give further insight into the performance of β-d-glucan on a wider scale: the Fungal Biomarkers for Diagnosis and Response to Therapy for Paediatric Candidemia (BIOPIC) is one such study. Due to the current lack of available evidence, it is not possible to recommend the use of β-d-glucan as a marker of IFD in children with a primary immunodeficiency.
Galactomannan and Aspergillus Antigen
The galactomannan (GM) immunoassay was designed to facilitate early diagnosis of IA and is considered to be more sensitive than culture. It is not as broadly useful at detecting other fungi as β-d-glucan but can be elevated, to a degree, in the presence of specific pathogens such as Histoplasma and Cryptococcus spp. [45]. Threshold for a positive result in paediatric patients is an optical density of ≥0.5, similar to that in adults [10•, 45, 46].
Specificity of serum GM is > 87% and sensitivity can be > 90% if use is limited to neutropenic children with proven or probable IA [47•]. In children with a primary immunodeficiency the GM assay is unvalidated as, for reasons that are unclear, GM is less sensitive in this patient population [46, 48]. Walsh et al. considered 16 children with CGD or hyper-IgE syndrome and proven/probable IA and found that only 25% of these children had a detectable serum GM [48].
Until recently, all published guidelines that directed GM use, and bore relevance to paediatric patients, were written specifically for children with malignancy or post-haematopoietic stem cell transplant [32, 49]. The 2019 ESCMIDD-ECMM guideline considers the usefulness of GM for diagnosis of IA in all paediatric patients [50••]. The authors acknowledge that GM is not validated in non-neutropenic patients but do not dismiss its usefulness altogether, they suggest GM testing be reserved for patients at high-risk for IA or for those with imaging findings and clinical signs suggestive of evolving IA [50••].
Adult studies have found that GM assay results from BAL specimens perform more reliably, with sensitivity increased relative to serum testing, even in non-neutropenic patients [12••, 51]. Limited paediatric studies would suggest this might also be true for BAL samples from children [50••].
It is worth mentioning that the use of GM as a serial screening tool for IA, in patients on mould-active prophylaxis, is not advised by any published study or guideline [52].
The Aspergillus antigen lateral flow device is discussed briefly here because, although promising, there is a limited amount of clinical experience using the technology to date, particularly in paediatric practice. It is a device designed to allow rapid, bed-side diagnosis of IA by employing a monoclonal antibody specific for an antigen released by Aspergillus spp. during phases of growth and invasion [53]. Small retrospective studies in adults have yielded some encouraging results: if Aspergillus antigen testing is used in conjunction with GM on BAL fluid, then sensitivity for IA has been shown to reach 94% [54]. If Aspergillus antigen testing is used alongside an Aspergillus-specific PCR, on serum samples, a sensitivity and specificity of 100% have been achieved in a single adult study which used this combinatorial approach to differentiate probable IA from non-IA [55]. Similar data for paediatric patients is not yet available.
Essentially, GM is a biomarker which remains unvalidated for use in children with primary immunodeficiency. If employed, it is best reserved for children in whom IA is probable and not as a screening tool for all children, with primary immunodeficiency, in whom uncharacterized fungal infection is possible. The clinical specimen sent for GM assay should be carefully considered and, based on available data, it is suggested that a BAL sample is preferable. The Aspergillus antigen lateral flow device should prove a valuable diagnostic tool in the future but, as yet, is not widely commercially available or validated for use in paediatric patients with primary immunodeficiencies.
Candida Mannan Antigen and Anti-mannan Antibody
Mannan antigen circulates during infection with Candida spp., mannan being a small component of the Candida cell wall. In adult studies, mannan antigen and anti-mannan antibody are analysed in combination. This results in sensitivity and specificity, for invasive candidiasis, of 83% and 86% respectively [56].
In paediatric medicine, most interest in the utility of mannan assays has emerged from the neonatal community. As a result, it is difficult to find studies which do not exclusively focus on preterm infants, the majority of whom do not have a primary immunodeficiency. These neonatal-focused studies suggest mannan assays perform relatively well. Oliveri et al. considered 184 neonates, employing a cutoff mannan level of > 0.5 ng/ml for a positive result, and demonstrated mannan assay sensitivity of 92% [57]. The authors also determined that a positive result was available between 4 and 18 days ahead of blood cultures [57].
One could be tempted to infer that similar findings might be observed in large-scale studies of older children but this has not been evidenced to date. Certainly, in 63 paediatric oncology patients known to be colonized with Candida spp., confirmed on culture of rectal/groin/oropharyngeal swabs, Candida mannan was not significantly elevated relative to non-colonized patients [58•]. Further, of two patients who subsequently developed candidaemia, only one developed a positive mannan result [58•].
There have also been concerns that, as the assay was originally derived against C. albicans, it does not detect other Candida species [59]. This is most probably due to the reduced amount of mannan produced by these species [59].
Currently, there are no studies considering the use of Candida mannan or anti-mannan in children with a primary immunodeficiency but, given the poor performance of the assays in oncology patients rendered immunodeficient secondary to anti-cancer treatment, caution is advised. It is not possible, in view of the available literature, to be certain of the contribution mannan assays bring to the field of paediatric fungal diagnostics.
Fungal PCR
PCR-based methods identify species-specific or pan-fungal ribosomal DNA sequences and can help in the diagnosis of a wide range of fungal pathogens. Broadly speaking, fungal PCR can be performed on serum, BAL, CSF, and deep-site tissue samples. For certain fungi, sensitivity and specificity are known to be affected by sample type; many commercially available Aspergillus PCR tests, for example, demonstrate greater specificity with BAL samples but greater sensitivity with serum [60].
A significant benefit of PCR is that it can yield results within 24 h, a time gain of up to 5 days compared with microscopy and culture [61]. This inevitably results in earlier initiation of targeted treatment, crucial when managing immunodeficient paediatric patients. Limitations and challenges are, as one might expect, that the high degree of homology between human and fungal DNA can complicate interpretation of results, that differentiating between patient colonisation and invasive infection is not always possible, and that risk of environmental contamination of the sample is greater than with conventional diagnostic tools [62, 63].
For Aspergillus infection, the 2017 ESCMID-ECMM-ERS guideline proposes that, at present, Aspergillus-specific PCR be employed only in combination with another fungal biomarker, namely GM, to improve diagnostic accuracy and not as a standalone investigation [12••]. This combinatorial approach is associated with earlier diagnosis of IA and enhanced diagnostic certainty: in adults, the specificity, sensitivity, and positive predictive value of GM and Aspergillus PCR is 97%, 85%, and 94% respectively [12••, 64•]. Considering paediatric patients, studies have shown conflicting results regarding the specificity and sensitivity of Aspergillus-specific PCR but, similar to in adults, the test is thought to have a role alongside GM [65, 66]. Vrioni et al. considered 156 children with possible IA, admitted to a tertiary hospital in Greece, their cohort included patients with primary immunodeficiency [67•]. The authors concluded that the combination of GM and Aspergillus-specific PCR heightened diagnostic accuracy for IA, across the entire study population, and that agreement between the two tests was 97.5% in the subgroup with primary immunodeficiency [67•].
Data supporting the use of Candida PCRs in children is scarce. Taira et al. considered a multiplex nested PCR approach to detect Candida species in the bloodstream of critically ill children in an intensive care setting, none of whom suffered from a confirmed primary immunodeficiency [68]. Their sample size was small (54 patients) and, whilst results showed that PCR sensitivity was 24% compared with culture sensitivity of 14.8%, this difference was not statistically significant [68]. Septifast is a commercially available multiplex Candida PCR assay with a 61% sensitivity and 99% specificity for Candida spp. [69]. Septifast has been shown to yield a statistically significant (due to a large number of study participants) increase in positive results compared with culture: 14.6% vs 10.3% respectively, but, one should consider that a 4.3% difference, whilst statistically significant, is of debatable clinical significance [69]. Again, all participants in this study appeared to be absent of a primary immunodeficiency, although such patients were not actively excluded.
The T2Candida panel combines PCR techniques with magnetic resonance–based biosensing to detect, to species level within 3–5 h, five pathogenic Candida spp. [70•]. Multicentre trials have recently assessed performance of this technology in adult patients: the 2015 DIRECT trial determined T2Candida panel sensitivity and specificity to be 91% and 98% respectively [71]. Further, from a clinical standpoint, studies have shown a reduction in the mean duration of empirical antifungal treatment when T2Candida testing is combined with blood culture and both are negative [72]. Only one study, designed by Humala et al., has attempted T2Candida testing, using smaller samples than those advised by the T2Candida instrument, on a cohort of paediatric patients [73]. Fifteen children at the Children’s Hospital of Philadelphia, all of whom also had blood drawn for culture, participated; the authors found 100% concordance with blood culture results and advised that subsequent, large-scale, paediatric studies be designed to confirm their findings [73]. As the underlying diagnoses of the patient cohort were not disclosed within the paper, it is unclear if any suffered from a primary immunodeficiency [73].
Based on currently available data, the view of the mycology community as a whole, is that PCR-based methods of identifying Candida spp. cannot offer species-specific information reliably or rapidly enough to offset the cost of routinely employing these techniques [69, 74, 75].
Further research, principally more multicentre trials, are needed before the use of species-specific/pan-fungal PCR can be advised, as routine practice, in paediatric patients with a primary immunodeficiency, although the promising nature of studies to date is acknowledged.
What Might the Future of Fungal Diagnostics Look Like?
Pan-fungal/fungi-specific PCRs and rapid diagnostic test kits, such as the Aspergillus antigen lateral flow device and the T2Candida panel, are exciting novel tools which, once validated for paediatric patients, could dramatically alter the landscape of fungal diagnostics. Given the importance of early diagnosis of fungal infection in children with primary immunodeficiency tests such as these, with a rapid turnaround time, are appealing.
New imaging modalities are in development, such as 18F-FDG positron emission tomography (PET)/CT. Leroy-Freschini et al. considered 51 immunocompromised patients with a diagnosis of IFD and performed 18F-FDG PET/CTs on 29/51 patients, all of whom were treatment-naïve [76•]. They found that sensitivity, specificity, and positive and negative predictive values for IFD were 93%, 81%, 95%, and 72% respectively. Also, as there was enhanced definition of extent of infection in scanned patients, they noted that treatment increases, treatment withdrawal, and any other diagnostic procedures were more appropriately scheduled [76•]. An identifiable weakness of 18F-FDG PET/CT is that it is not specific for any single fungal organism, nor can it differentiate between them. Our proficiency in differentiating between fungal species, using labelled radionuclides for example, is evolving as our understanding of fungal pathogen survival within the human host advances. Whilst not yet commercially available, labelled siderophores have been proposed by Petrik et al. as a means of positively identifying IA on PET scan, providing clinicians with a differentiating imaging tool [77].
Conclusion
The field of fungal diagnostics is rapidly evolving but there are many challenges to be overcome. This is particularly true when it comes to our knowledge of how novel fungal diagnostic tools perform in immunodeficient paediatric patients. All children are dissimilar to adults in terms of the epidemiology of IFD. An additional layer of complexity is added when one considers the heterogeneity of disease within the small paediatric cohort classed as having primary immunodeficiency. At present, we do not have the evidence base to direct the use of many fungal diagnostic tests, excepting histopathology, microscopy, and culture and diagnostic imaging, in this vulnerable cohort.
Of the limited number of studies available for review, many were weakened by their small sample sizes, exclusion of potentially relevant patient groups, and variability of specimens chosen for testing, both in type (serum vs BAL) and in sampling nature (repeat testing vs single specimen analysis).
From the relevant body of literature that was available, we could determine that, when IFD is suspected, samples should be obtained for microscopy, culture, and/or histopathology. It is also advised that imaging be carefully considered, with due thought to the extent of imaging and appropriateness of modality, acknowledging the potential for deep site infection and/or CNS involvement in children, especially in those with a primary immunodeficiency.
Galactomannan remains unvalidated in paediatric patients with a primary immunodeficiency but, on review of studies performed to date, it is evident that an increasing number are supportive of the GM assay provided this test is employed judiciously, i.e., only to assist in the diagnosis of IA for appropriately selected high-risk patients. GM assays are particularly encouraged when a BAL sample is available for testing following bronchoscopy.
In light of the currently published literature, Candida mannan assays and β-d-glucan are not routinely advised. Recommendations as to how clinicians should interpret results of these tests, if they are run, cannot be given due to the lack of supporting evidence. Fungal PCRs, specifically Aspergillus PCRs with their relatively high positive predictive value, are promising but, a poor evidence base means they should be used and interpreted with caution, unless as a component of an ongoing clinical trial.
One of the most significant challenges in the diagnostic work-up of children with a primary immunodeficiency may be the increasing use of mould-active prophylaxis. Prophylaxis not only encourages growth of atypical fungal pathogens but also complicates the interpretation of many diagnostic tests, including GM. This should be considered when evaluating any immunodeficient child for IFD.
This review has identified that our knowledge of fungal diagnostic test performance in immunodeficient children is suboptimal. Moving forward, children with primary immunodeficiency should be actively included in multicentre trials evaluating non-culture-based fungal diagnostic tools. It is important that communication and collaborative working is fostered between tertiary centres in order to best facilitate this.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Chandesris MO, Melki I, Natividad A, Puel A, Fieschi C, Yun L, et al. Autosomal dominant STAT3 deficiency and hyper-IgE syndrome: molecular, cellular, and clinical features from a French national survey. Medicine (Baltimore). 2012;91:e1–19. https://doi.org/10.1097/MD.0b013e31825f95b9.
Garraffo A, Pilmis B, Toubiana J, Puel A, Mahlaoui N, Blanche O, et al. Invasive fungal infection in primary immunodeficiencies other than chronic granulomatous disease. Current Fungal Infection Reports. 2017;11:25–34. https://doi.org/10.1007/s12281-017-0273-x.
Beauté J, Obenga G, Le Mignot L, Mahlaoui N, Bougnoux ME, Mouy R, et al. Epidemiology and outcome of invasive fungal diseases in patients with chronic granulomatous disease: a multicenter study in France. Pediatric Infectious Diseases Journal. 2011;30:57–62. https://doi.org/10.1097/INF.0b013e3181f13b23.
Lanternier F, Cypowyj S, Picard C, Bustamante J, Lortholary O, Casanova JL, et al. Primary immunodeficiencies underlying fungal infections. Current Opinions in Pediatrics. 2013;25:736–47. https://doi.org/10.1097/MOP.0000000000000031.
Antachopoulos C. Invasive fungal infections in congenital immunodeficiencies. Clinical Microbiology and Infection. 2010;16(9):1335–42. https://doi.org/10.1111/j.1469-0691.2010.03289.x.
Odio CD, Milligan KL, McGowan K, Rudman Spergel AK, Bishop R, Boris L, et al. Endemic mycoses in patients with STAT3-mutated hyper-IgE (Job) syndrome. Journal of Allergy and Clinical Immunology. 2015;136:1411–3. https://doi.org/10.1016/j.jaci.2015.07.003.
Pana ZD, Roilides E, Warris A, Groll AH, Zaoutis T. Epidemiology of Invasive Fungal Disease in Children. Journal of Pediatric Infectious Diseases Society. 2017;6(1):S3–S11. https://doi.org/10.1093/jpids/pix046.
Jones N, Garcez T, Newman W, Denning D. Endogenous Candida endophthalmitis and osteomyelitis associated with CARD9 deficiency. BMJ Case Reports. 2016;3:2016. https://doi.org/10.1136/bcr-2015-214117.
Drewniak A, Gazendam RP, Tool AT, Van Houdt M, Jansen MH, Van Hamme J. Invasive fungal infection and impaired neutrophil killing in human CARD9 deficiency. Blood. 2013;121:2385–92. https://doi.org/10.1182/blood-2012-08-450551.
• De Pauw B, Walsh TJ, Donnelly JP, Stevens DA, Edwards JE, Calandra T, et al. Revised definitions of invasive fungal disease from the European Organization for Research and Treatment of cancer/invasive fungal infections cooperative group and the National Institute of Allergy and Infectious Diseases mycoses study group (EORTC/MSG) consensus group. Clinical Infectious Diseases. 2008;46:1813–21. https://doi.org/10.1086/588660Provides the reader with clear definitions, and guidelines for the diagnosis of, possible, probable and proven IFD.
Thomas KE, Owens CM, Veys PA, Novelli V, Costoli V. The radiological spectrum of invasive aspergillosis in children: a 10-year review. Pediatric Radiology. 2003;33:453–60. https://doi.org/10.1007/s00247-003-0919-4.
•• Ullmann AJ, Aguado JM, Arikan-Akdagli S, Denning DW, Groll AH, Lagrou K, et al. Diagnosis and management of Aspergillus diseases: executive summary of the 2017 ESCMID-ECMM-ERS guideline. Clinical Microbiology and Infection. 2018;24:e1–e38. https://doi.org/10.1016/j.cmi.2018.01.002Useful overview of the investigative work-up for patients with suspected IPA.
Rüchel R, Schaffrinski M. Versatile fluorescent staining of fungi in clinical specimens by using the optical brightener blankophor. Journal of Clinical Microbiology. 1999;37:2694–6.
Clancy CJ, Nguyen MH. Finding the "missing 50%" of invasive candidiasis: how non-culture diagnostics will improve understanding of disease spectrum and transform patient care. Clinical Infectious Diseases. 2013;56:1284–92. https://doi.org/10.1093/cid/cit006.
•Cuenca-Estrella M, Verweij PE, Arendrup MC, Arikan-Akdagli S, Bille J, Donnelly JP, et al. ESCMID* guideline for the diagnosis and management of Candida diseases 2012: diagnostic procedures. Clinical Microbiology and Infection 2012:18(S7):9–18. Doi: https://doi.org/10.1111/1469-0691.12038. Useful inclusion of recommendations for paediatric patients.
Parta M, Hilligoss D, Kelly C, Kwatemaa N, Theobald N, Malech H, et al. Haploidentical Hematopoietic Cell Transplantation with Post-Transplant Cyclophosphamide in a Patient with Chronic Granulomatous Disease and Active Infection: A First Report. Journal of Clinical Immunology. 2015;35(7):675–80. https://doi.org/10.1007/s10875-015-0204-y.
Liss B, Vehreschild JJ, Bangard C, Maintz D, Frank K, Gronke D, et al. Our 2015 approach to invasive pulmonary aspergillosis. Mycoses. 2016;58:375–82. https://doi.org/10.1111/myc.12319.
Sisli E, Ozdemir Sahan Y, Ayik MF, Nart D, Atay Y. A rare complication of chronic granulomatous disease in a child: constrictive aspergillus pericarditis. Archives of the Turkish Society of Cardiology. 2017;45(7):660–3. https://doi.org/10.5543/-tkda.2017.52284.
Maaloul I, Ameur SB, Chabchoub I, Kolsi R, Bahloul M, Kamoun T, et al. Fulminant mulch pneumonitis in a previously healthy child. Archives de Pediatrie. 2018;25(8):495–6. https://doi.org/10.1016/j.arcped.2018.09.003.
• Fujita Y, Ishiwada N, Takei H, Suwabe SI, Yarita K, Ohkusu M, et al. Usefulness of Gastric Aspirate Culture for Diagnosing Congenital Immunodeficiency in an Infant with Fungal Pneumonia Caused by Rasamsonia piperina. The Tohoku Journal of Experimental Medicine. 2019;247(4):265–9. https://doi.org/10.1620/tjem.247.265Authors present a novel means of obtaining tissue for fungal culture, of interest given the challenges this can provide in paediatric practice.
Sodhi KS, Khandelwal N, Saxena AK, Singh M, Agarwal R, Bhatia A, et al. Rapid lung MRI in children with pulmonary infections: time to change our diagnostic algorithms. Journal of Magnetic Resonance Imaging. 2016;43:1196–206. https://doi.org/10.1002/jmri.25082.
Maschmeyer G, Carratala J, Buchheidt D, Hamprecht A, Heussel CP, Kahl C, et al. Diagnosis and antimicrobial therapy of lung infiltrates in febrile neutropenic patients (allogeneic SCT excluded): updated guidelines of the infectious diseases working party (AGIHO) of the German Society of Hematology and Medical Oncology (DGHO). Annals of Oncology. 2015;26:21–33. https://doi.org/10.1093/annonc/mdu192.
• Davies BW, Gonzalez MO, Vaughn RC, Allen GC, Durairaj VD. Dacryocystitis as the initial presentation of invasive fungal sinusitis in immunocompromised children. Ophthalmic plastic and reconstructive surgery. 2016;32(4):e79–81. https://doi.org/10.1097/IOP.-0000000000000252Highlights the atypical presentation of IFD observed in vulnerable paediatric patients.
Bruno C, Minniti S, Vassanelli A, Pozzi-Mucelli R. Comparison of CT features of Aspergillus and bacterial pneumonia in severely neutropenic patients. Journal of Thoracic Imaging. 2007;22:160–5. https://doi.org/10.1097/RTI.0b013e31805f6a42.
Franquet T, Gimenez A, Hidalgo A. Imaging of opportunistic fungal infections in immunocompromised patient. European Journal of Radiologyl. 2004;51(2):130–8. https://doi.org/10.1016/j.ejrad.2004.03.007.
Althoff Souza C, Muller NL, Marchiori E, Escuissato DL, Franquet T. Pulmonary invasive aspergillosis and candidiasis in immunocompromised patients: a comparative study of the high-resolution CT findings. Journal of Thoracic Imaging. 2006;21:184–9. https://doi.org/10.1097/01.rti.0000213552.16011.ad.
Dotis J, Pana ZD, Roilides E. Non-Aspergillus fungal infections in chronic granulomatous disease. Mycoses. 2013;56:449–62. https://doi.org/10.1111/myc.12049.
Vinh DC, Shea YR, Jones PA, Freeman AF, Zelazny A, Holland SM. Chronic invasive aspergillosis caused by Aspergillus viridinutans. Emerging Infectious Diseases. 2009;15:1292–4. https://doi.org/10.3201/-eid1508.090251.
Haidar G, Zerbe CS, Cheng M, Zelazny AM, Holland SM, Sheridan KR. Phellinus species: An emerging cause of refractory fungal infections in patients with X-linked chronic granulomatous disease. Mycoses. 2017;60(3):155–60. https://doi.org/10.1111/myc.12573.
• De Ravin SS, Parta M, Sutton DA, Wickes BL, Thompson EH, Wiederhold NP, et al. Paravertebral mushroom: identification of a novel species of Phellinus as a human pathogen in chronic granulomatous disease. Journal of Clinical Microbiology. 2014;52:2726–9. https://doi.org/10.1128/JCM.00667-14Important reminder that growth of indolent organisms can be encouraged by prophylactic prescription.
Pappas PG, Kauffman CA, Andes D, Clancy CJ, Marr K, Ostrosky-Zeichner L, et al. Clinical Practice Guideline for the Management of Candidiasis: 2016 Update by the Infectious Diseases Society of America. Clinical Infectious Diseases. 2016;62(4):e1–e50. https://doi.org/10.1093/cid/civ933.
•• Hope WW, Castagnola E, Groll AH, Roilides E, Akova M, Arendrup MC, et al. ESCMID* guideline for the diagnosis and management of Candida diseases 2012: prevention and management of invasive infections in neonates and children caused by Candida spp. Clinical Microbiology and Infection. 2012;18:38–52. https://doi.org/10.1111/1469-0691.12040Guideline for the management of candidiasis, specifically in children.
• Groll AH, Castagnola E, Cesaro S, Dalle JH, Engelhard D, Hope W, et al. Fourth European Conference on Infections in Leukaemia(ECIL-4): guidelines for diagnosis, prevention, and treatment of invasive fungal diseases in paediatric patients with cancer or allogeneic haemopoietic stem-cell transplantation. Lancet Oncology. 2014;15(8):e327–40. https://doi.org/10.1016/S1470-2045(14)70017-8Although largely pertaining to management of paediatric haemoncology patients, this paper provides an excellent overview of fungal diagnostic tools and was the first guideline devised for children with cancer and an IFD.
• Huppler AR, Fisher BT, Lehrnbecher T, Walsh TJ, Steinbach WJ. Role of Molecular Biomarkers in the Diagnosis of Invasive Fungal Diseases in Children. Journal of the Pediatric Infectious Disease Society. 2017;6(1):32–44. https://doi.org/10.1093/jpids/pix054Excellent overview of fungal biomarkers and their role in the diagnosis of IFD.
Theel E, Doern C. β-D-glucan testing is important for diagnosis of invasive fungal infections. Journal of Clinical Microbiology. 2013;51(11):3478–83. https://doi.org/10.1128/JCM.01737-13.
Tran T, Beal S. Application of the 1,3-β-d-Glucan (Fungitell) Assay in the Diagnosis of Invasive Fungal Infections. Archives of Pathology and Laboratory Medicine. 2016;140(2):181–5. https://doi.org/10.5858/arpa.2014-0230-RS.
Fontana C, Gaziano R, Favaro M, Ia C, Pistoia E, Di Francesco P. (1-3)-β-D-Glucan vs Galactomannan Antigen in Diagnosing Invasive Fungal Infections (IFIs). Open Microbiology Journal. 2012;6:70–3. https://doi.org/10.2174/1874285801206010070.
Bernabé F, Chumpitazi F, Lebeau B, Faure-Cognet O, Hamidfar-Roy R, Timsit JF, et al. Characteristic and clinical relevance of Candida mannan test in the diagnosis of probable invasive candidiasis. Medical Mycology. 2014;52(5):462–71. https://doi.org/10.1093/mmy/myu018.
Del Bono V, Delfino E, Furfaro E, Mikulska M, Nicco E, Bruzzi P, et al. Clinical performance of the (1, 3)-Beta-D-glucan assay in early diagnosis of nosocomial Candida bloodstream infections. Clinical and Vaccine Immunology. 2011;18(12):2113–7. https://doi.org/10.1128/CVI.05408-11.
He S, Hang JP, Zhang L, Wang F, Zhang DC, Gong FH. A systematic review and meta-analysis of diagnostic accuracy of serum 1,3-beta-D-glucan for invasive fungal infections: focus on cutoff levels. Journal of Microbiology, Immunology and Infection. 2015;48(4):351–61. https://doi.org/10.1016/j.jmii.-2014.06.009.
Smith PB, Benjamin DK Jr, Alexander BD, Johnson MD, Finkleman MA, Steinbavh WJ. Quantification of 1,3-beta-d-glucan levels in children: preliminary data for diagnostic use of the beta-glucan assay in a pediatric setting. Clinical and Vaccine Immunology. 2007;14(7):924–5. https://doi.org/10.1128/CVI.00025-07.
•• Calitri C, Caviglia I, Cangemi G, Furfaro E, Bandettini R, Fioredda F, et al. Performance of 1,3-β-D-glucan for diagnosing invasive fungal diseases in children. Mycoses. 2017;60(12):789–95. https://doi.org/10.1111/myc.12664Interesting study that questions the performance of 1,3-β-D-glucan in the paediatric cohort.
• Salvatore CM, Petraitiene R, Sitaras L, Hammad H, Leimena P, Toussi S, et al. Prospective study and analytical performance of serum (1->3)-β-d-glucan in pediatric patients. New Orleans, LA: Program and Abstracts of ID Week. Open Forum Infectious Diseases. 2016;3(1):1570. https://doi.org/10.1093/ofid/ofw172.1270Further explores the utility of 1,3-β-D-glucan in paediatric practice.
Naselli A, Faraci M, Lanino E, Morreale G, Cangemi G, Bandettini R, et al. Persistence of high-level (1,3)-β-d-glucan after candidemia following autologous peripheral SCT in a pediatric patient. Bone Marrow Transplant. 2015;50:137–8.
Roilides E, Pana ZD. Application of diagnostic markers to invasive aspergillosis in children. Annals of the New York Academy of Sciences. 2012;1272:1–8. https://doi.org/10.1111/j.1749-6632.2012.06828.x.
Fisher BT. The role of biomarkers for diagnosis of and therapeutic decisions related to invasive aspergillosis in children. Current Fungal Infection Reports. 2013;7(1):7–14. https://doi.org/10.1007/s12281-012-0127-5.
• Henriet S, Verweij PE, Holland SM, Warris A. Invasive fungal infections in patients with chronic granulomatous disease. Advances in Experimental Medicine and Biology. 2013;764:27–55. https://doi.org/10.1007/978-1-4614-4726-9_3Particular focus on CGD: a disease process which has taught much about IFD and the relative merits of the available diagnostic tests.
Walsh TJ, Schaufele RL, Sein T. Gea-Banacloche J, Bishop M, Young N, et al. Reduced expression of galactomannan antigenemia in patients with invasive aspergillosis and chronic granulomatous disease or Job’s syndrome. Program and Abstracts of the 40th Annual Meeting of the Infectious Diseases Society of America; 24–27 October 2002; Chicago, IL.
Lehrnbecher T, Robinson P, Fisher B, Alexander S, Ammann RA, Beauchemin M, et al. Guideline for the management of fever and neutropenia in children with cancer and hematopoietic stem cell transplantation recipients: 2017 update. Journal of Clinical Oncology. 2017;35:2082–94. https://doi.org/10.1200/JCO.2016.71.7017.
•• Warris A, Lehrnbecher T, Roilides E, Castagnola E, Bruggemann RJM, Groll AH. Escmid-ecmm guideline: diagnosis and management of invasive aspergillosis in neonates and children. Clinical Microbiology and Infection. 2019. https://doi.org/10.1016/j.cmi.2019.05.019One of the key paediatric guidelines directing management of children with IA.
D'Haese J, Theunissen K, Vermeulen E, Schoemans H, De Vlieger G, Lammertijn L, et al. Detection of galactomannan in bronchoalveolar lavage fluid samples of patients at risk for invasive pulmonary aspergillosis: analytical and clinical validity. Journal of Clinical Microbiology. 2012;50(4):1258–63. https://doi.org/10.1128/JCM.06423-11.
Duarte R, Sánchez-Ortega I, Cuesta I, Arnan M, Patiño B, Fernández de Sevilla A, et al. Serum galactomannan–based early detection of invasive Aspergillosis in hematology patients receiving effective anti-mold prophylaxis. Clinical Infectious Diseases. 2014;59(12):1696–702. https://doi.org/10.1093/cid/ciu673.
Thornton CR. Development of an immunochromatographic lateral flow device for rapid serodiagnosis of invasive aspergillosis. Clinical Vaccine Immunology. 2008;15(7):1095–105. https://doi.org/10.1128/CVI.00068-08.
Hoenigl M, Prattes J, Spiess B, Wagner J, Prueller F, Raggam RB, et al. Performance of galactomannan, beta-d-glucan, Aspergillus lateral-flow device, conventional culture, and PCR tests with bronchoalveolar lavage fluid for diagnosis of invasive pulmonary aspergillosis. Journal of Clinical Microbiology. 2014;52(6):2039–45. https://doi.org/10.1128/JCM.00467-14.
White PL, Parr C, Thornton C, Barnes RA. Evaluation of real-time PCR, galactomannan enzyme-linked immunosorbent assay (ELISA) and a novel lateral flow device for diagnosis of invasive Aspergillosis. Journal of Clinical Microbiology. 2013;51(5):1510–6. https://doi.org/10.1128/JCM.03189-12.
Marchetti O, Lamoth F, Mikulska M, Viscoli C, Verweij P, Bretagne S, et al. ECIL recommendations for the use of biological markers for the diagnosis of invasive fungal diseases in leukemic patients and hematopoietic SCT recipients. Bone Marrow Transplant. 2012;47(6):846–54. https://doi.org/10.1038/bmt.2011.178.
Oliveri S, Trovato L, Betta P, Romeo MG, Nicoletti G. Experience with the Platelia Candida ELISA for the diagnosis of invasive candidosis in neonatal patients. Clinical Microbiology and Infection. 2008;14(4):391–3. https://doi.org/10.1111/j.1469-0691.2007.01938.x.
• Mokaddas E, Burhamah MH, Khan ZU, Ahmad S. Levels of (1→3)-β-D-glucan, Candida mannan and Candida DNA in serum samples of pediatric cancer patients colonized with Candida species. BMC Infectious Diseases. 2010;10:292. https://doi.org/10.1186/1471-2334-10-292Highlights weaknesses of theCandidamannan assay when it is employed to as a diagnostic tool in paediatric patients.
Mikulska M, Calandra T, Sanguinetti M, Poulain D, Viscoli C. Third European Conference on Infections in Leukemia Group. The use of mannan antigen and anti-mannan antibodies in the diagnosis of invasive candidiasis: recommendations from the Third European Conference on Infections in Leukemia. Critical Care. 2010;14(6):222. https://doi.org/10.1186/cc9365.
White PL, Wingard JR, Bretagne S, Loffler J, Patterson TF, Slavin MA, et al. Aspergillus polymerase chain reaction: systematic review of evidence for clinical use in comparison with antigen testing. Clinical Infectious Diseases. 2015;61:1293–303. https://doi.org/10.1093/cid/civ507.
Hadir A, El-Mahallawy H, Shaker Hala A, Tarek M, Razak A. Evaluation of pan-fungal PCR assay and Aspergillus antigen detection in the diagnosis of invasive fungal infections in high risk paediatric cancer patients. Medical Mycology. 2006;44(8):733–9. https://doi.org/10.1080/13693780600939955.
Arendrup MC, Fisher BT, Zaoutis TE. Invasive fungal infections in the paediatric and neonatal population: diagnostics and management issues. Clinical Microbiology and Infection. 2009;15(7):613–24. https://doi.org/10.1111/j.1469-0691.2009.02909.x.
Frank-Michael C, Muller E, Trusen A, Weig M. Clinical Manifestations and diagnosis of invasive aspergillosis in immunocompromised children. European Journal of Paediatrics. 2002;161(11):563–74. https://doi.org/10.1007/s00431-002-1041-6.
• Boch T, Spiess B, Vehreschild JJ, Rath PM, Steinmann J, Heinz WJ, et al. Diagnosis of invasive fungal infections in haematological patients by combined use of galactomannan, 1,3-β-D-glucan, Aspergillus PCR, multifungal DNA-microarray, and Aspergillus azole resistance PCRs in blood and bronchoalveolar lavage samples: results of a prospective multicentre study. Clinical Microbiology and Infection. 2016;22(10):862–8. https://doi.org/10.1016/j.cmi.2016.06.021Interesting data: BAL vs serum testing.
Reinwald M, Konietzka CA, Kolve H, Uhlenbrock S, Ahike E, Hummel M, et al. Assessment of Aspergillus-specific PCR as a screening method for invasive aspergillosis in paediatric cancer patients and allogeneic haematopoietic stem cell recipients with suspected infections. Mycoses. 2014;57:537–43. https://doi.org/10.1111/myc.12192.
Hummel M, Spiess B, Roder J, van Komorowski G, Kürken M, Kentouche K, et al. Detection of Aspergillus DNA by a nested PCR assay is able to improve the diagnosis of invasive aspergillosis in paediatric patients. Journal of Medical Microbiology. 2009;58:1291–7. https://doi.org/10.1099/jmm.0.007393-0.
• Vrioni G, Theodoridou K, Tsiamis C, Mavrouli M, Kapsimali V, Rigopoulos D, et al. Use of Galactomannan antigen and Aspergillus DNA real time polymerase chain reaction as routine methods for invasive aspergillosis in immunosuppressed children in Greece. Clinical Therapeutics. 2018;40(6):918–24. https://doi.org/10.1016/j.clinthera.2018.05.002Supportive evidence for combining GM andAspergillusPCR, in the clinical setting.
Taira CL, Okay TS, Delgado AF, Ceccon ME, de Almeida MT, Del Negro GM. A multiplex nested PCR for the detection and identification of Candida species in blood samples of critically ill paediatric patients. BMC Infectious Diseases. 2014;14:406–2334. https://doi.org/10.1186/1471-2334-14-406.
Lucignano B, Ranno S, Liesenfeld O, Pizzorno B, Putignani L, Bernaschi P, et al. Multiplex PCR allows rapid and accurate diagnosis of bloodstream infections in newborns and children with suspected sepsis. Journal of Clinical Microbiology. 2011;49:2252–8. https://doi.org/10.1128/JCM.02460-10.
• Clancy C, Nguyen M. T2 magnetic resonance for the diagnosis of bloodstream infections:charting a path forward. Journal of Antimicrobial Chemotherapy. 2018;73(4):2–5. https://doi.org/10.1093/jac/dky050Exciting prospect, moving forward, to consider MR technology facilitating more rapid turnaround of PCR based methods.
Mylonakis E, Clancy CJ, Ostrosky-Zeichner L. T2 magnetic resonance assay for the rapid diagnosis of candidemia in whole blood: a clinical trial. Clinical Infectious Diseases. 2015;60:892–9.
Patch ME, Weisz E, Cubillos A. Impact of rapid, culture independent diagnosis of candidemia and invasive candidiasis in a community health system. Journal of Antimicrobial Chemotherapy. 2018;73(4):27–30.
Hamula C, Hughes K, Fisher B, Zaoutis T, Singh I, Velegraki A, et al. T2Candida provides rapid and accurate species identification in pediatric cases of candidemia. American Journal of Clinical Pathology. 2016;145(6):858–61. https://doi.org/10.1093/ajcp/aqw063.
Wellinghausen N, Siegel D, Winter J, Gebert S. Rapid diagnosis of candidemia by real-time PCR detection of Candida DNA in blood samples. Journal of Medical Microbiology. 2009;58:1106–11. https://doi.org/10.1099/jmm.0.007906-0.
Ao W, Klonoski J, Berlinghoff E, Jensen J, Afroz T, Munns D, et al. Rapid Detection and Differentiation of Clinically Relevant Candida Species Simultaneously from Blood Culture by Use of a Novel Signal Amplification Approach. Journal of clinical microbiology. 2017;56(1):e00982–17. https://doi.org/10.1128/JCM.00982-17.
• Leroy-Freschini B, Treglia G, Argemi X, Bund C, Kessler R, Herbrecht R, et al. 18F-FDG PET/CT for invasive fungal infection in immunocompromised patients. QJM. 2018;111(9):613–22. https://doi.org/10.1093/qjmed/hcy128Study suggesting that an alternative approach to imaging could offer a means of treatment planning and more detailed definition of fungal disease.
Petrik M, Haas H, Laverman P, Schrettl M, Franssen GM, Blatzer M, et al. 68Ga-triacetylfusarinine C and 68Ga-ferrioxamine E for Aspergillus infection imaging: uptake specificity in various micro-organisms. Molecular Imaging and Biology. 2014;16(1):102–8. https://doi.org/10.1007/s11307-013-0654-7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Catherine Mark and Claire McGinn declare no conflicts of interest relevant to this manuscript.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Pediatric Fungal Infections
Rights and permissions
About this article
Cite this article
Mark, C., McGinn, C. From Culture to Fungal Biomarkers: the Diagnostic Route of Fungal Infections in Children with Primary Immunodeficiencies. Curr Fungal Infect Rep 13, 211–220 (2019). https://doi.org/10.1007/s12281-019-00356-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12281-019-00356-4