Abstract
Invasive aspergillosis (IA) is a feared opportunistic infection for many immuncompromised children resulting in significant morbidity and mortality. Timely diagnosis based on traditional testing modalities and clinical evaluation has proven to be challenging. Assays designed to measure IA biomarkers such as galactomannan (GM) and beta-D-glucan (BG) represent a potential significant improvement in the ability to diagnose pediatric IA. However, as with any new diagnostic tool, clinicians need to be aware of the operating characteristics of these assays in order to apply them in the appropriate settings. Published adult and pediatric data regarding GM and BG testing are reviewed and guidance regarding the appropriate utility of these assays in children is offered.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The list of pediatric conditions resulting in immunocompromised states continues to grow. These immunocompromised states include both primary immune deficiencies such as chronic granulomatous disease as well as acquired immune deficiency secondary to HIV. Additionally, there are those immune deficient states resulting from chemotherapeutic exposures for various malignancies and from life saving measures such as solid organ and hematopoietic stem cell transplantation (HCT). Finally, there is an ever-expanding population of patients receiving immune modulating therapies for autoimmune conditions.
Although the type and degree of immune dysfunction varies across each of these patient groups, for many of these immunocompromised children invasive aspergillosis (IA) is a feared opportunistic infection resulting in significant increases in healthcare expenditures and ending in mortality for more than half of those infected [1•, 2]. The reason for the high mortality rate is multifactorial including delays in diagnosis, limited therapeutic options and the difficulty of resolving these infections in children with compromised immune systems. Although limited, previous data suggest that outcomes for IA can be improved with initiation of therapeutic interventions at the earliest possible time point [3, 4].
However, making a timely diagnosis of IA can be challenging. In 2002, a cooperative group of the European Organization for Research and Treatment of Cancer (EORTC) along with the Mycoses Study Group (MSG) published consensus recommendations for defining an invasive fungal infection (IFI) inclusive of IA [5]. Their definitions for proven or probable IA included various host factors, specific radiographic information (e.g., halo sign or air-crescent sign), clinical findings, and microbiologic data. The latter focused mostly on culture or histopathology data from biopsy specimens obtained via invasive procedures. Although presence of Aspergillus antigen in broncoalveolar lavage or blood specimens was included as supportive microbiologic evidence for an IA diagnosis, the cooperative group recognized that the availability of these antigen assays and clinical data supporting their use were sparse at the time.
In the ensuing years a number of large-scale adult prospective clinical observational studies were completed resulting in the FDA approval of two indirect assays, the galactomannan (GM) enzyme immunoassay (EIA) and (1 → 3) Beta-D-Glucan assay (BG), for diagnosing IFI and specifically of IA [6–10, 11••]. Not only did the data from these adult trials support the diagnostic capabilities of these assays, they also revealed the potential to shorten the window of time between onset and detection of IA [8, 9]. Based on these and other studies, the revised EORTC/MSG definitions for all IFI and specifically IA incorporated GM and BG positive results as mycological criteria supportive of a probable diagnosis [12].
While the benefits of these indirect diagnostic tools are multiple (e.g., less invasive testing, earlier time to diagnosis) clinicians caring for immunocompromised pediatric patients at risk for IA must be careful in extrapolating the adult data as the kinetics of these tests can vary by age and patient population. The pediatric specific data for each of these assays will be reviewed and recommendations on appropriate testing will be offered.
Galactomannan Testing
History of Galactomannan
In 1978 Lehmann and Reiss created a rabbit model of IA with a goal of devising a test capable of detecting a circulating antigen from Aspergillus [13]. They were successful at raising an anti-serum from these rabbits that was specific to a certain carbohydrate antigenic moiety. In subsequent studies they identified this antigen as GM [14]. Their efforts established a foundation for development of various assays to detect GM antigenemia. Galactomannan is a polysaccharide composed of a mannose backbone with galactose side groups, which compromises a major component of the cell wall of Aspergillus spp. During an IA infection, GM is released resulting in the potential for detection of this antigen in the serum or other body fluids of an infected patient. In the decades after the isolation of GM antigen, a number of techniques were explored to accurately detect BM from human specimens [15, 16]. A sandwich ELISA assay using the monoclonal antibody, EB-A2, emerged as the leading technique as it was able to detect lower amounts of circulating GM [17, 18]. The commercially manufactured Platelia™ Aspergillus EIA kit from Bio-Rad Laboratories has made this sandwich ELISA assay technique for detecting GM available for routine clinical use.
Adult Data on Galactomannan Testing
It has been over two decades since the first large prospective trial evaluated the use of serial serum GM testing to detect the onset of IA in adult patients with prolonged neutropenia using the EORTC/MSG IFI definitions as the gold standard [9]. Considering a GM index of 1.0 or greater as positive, this testing strategy resulted in 72.9 % sensitivity, 94.7 % specificity, 61.3 % PPV, and 96.8 % NPV for detection of IA. Results were improved when data from autopsy findings were included. Detection of GM preceded the time of definitive IA diagnosis in 96 % of the proven IA cases by a median of 17 days (range of 2-110 days). Since this sentinel publication a number of similar studies have evaluated GM surveillance testing in various adult immunocompromised cohorts. These studies have been summarized in two separate meta-analyses each of which highlight the variable performance of GM testing across different patient types [10, 11••]. The meta-analysis by Pfeiffer et al., suggested that the GM assay was likely most useful in a population of hematologic malignancy patients or HCT recipients [10]. Importantly, the meta-analysis from the Cochrane Collaboration suggested that the sensitivity of the assay improved from 64 % to 78 % when the threshold for positivity was decreased from a GM index of 1.5 to 0.5. This decrease in the threshold to optimize sensitivity did compromise specificity from 95 % to 81 % [11••]. Based on these data the manufacturer recommendation for a positive result is a galactomannan index of ≥0.5.
Pediatric Data on Galactomannan Testing
As is typical with many diagnostic tests, extrapolating results from primarily adult studies to pediatric patients can be misleading. Fortunately, there have been a number of prospective observational studies that inform the use of serum GM testing in children (Table 1) [19–24]. Taken collectively the operating characteristics are reassuring for the use of GM testing in children, however, as with any diagnostic test there needs to be caution when applying study results to specific clinical scenarios. Notably two studies [24, 25] reported a 0 % sensitivity mainly because only one proven or probable case of IA was identified in these cohorts. Although each of these cohorts included patients considered at high risk for IFI, ultimately few patients developed IA limiting the potential number of true positive patients. This reinforces the fact that GM testing should not be applied to scenarios where there is a low likelihood of IA.
Galactomannan Testing Approach
Although the operating characteristics of GM in high-risk populations seem reasonable, a number of questions still remain as to what time is ideal to initiate testing. Recently, the first published pediatric specific guideline for fever and neutropenia supported the implementation of twice-weekly GM testing in children with fever and neutropenia at high-risk for IFI [26••]. This approach is reasonable as arguably the pre-test probability of IA in a febrile neutropenic patient is higher than that of a patient with just neutropenia. It is important to note that the recommendation for GM testing was graded as weak based on moderate-quality evidence.
Certainly, additional data in various patient settings are necessary to refine the optimal testing window. For instance, receipt of prophylactic antifungal therapy has been shown to reduce the sensitivity of GM testing in predominantly adult cohorts [6, 27]. The reduction in sensitivity while on antifungals is less pronounced when the threshold GM index of 0.5 is applied. Additionally, the vast majority of pediatric data are derived from populations of children with neutropenia secondary to chemotherapy for malignancy or conditioning for HCT.
Galactomannan Testing in Non-Neutropenic Populations
As noted previously, there are a number of additional populations at risk for IA. However, data are limited on the utility of GM testing in immuncompromised patients that are not neutropenic. Multiple case reports have documented repeatedly negative GM assays in patients with chronic granulomatous disease and proven IA suggesting limited utility in this patient group [28–30]. Furthermore, data from solid organ transplant recipients suggest variable effectiveness of serum GM testing in this population during active IA [31–35].
Galactomannan Testing on Non-Serum Specimens
There have been a number of published reports evaluating the diagnostic utility of detecting GM in other body fluids. An adult report including 99 patients with hematologic disorders suggested that GM testing of specimens obtained at the time of a bronchoalveolar lavage fluid (BAL) was diagnostically useful [36]. A similar pediatric study retrospectively reported on GM testing of BAL specimens from children with immunocompetent and compromised conditions. The latter included primary immune deficiencies, various malignancies and HCT and solid organ transplant recipients. Among these immuncompromised patients, GM testing of BAL specimens seemed to be useful with sensitivity, specificity, positive and negative predictive values of 78 %, 100 %, 58 %, and 96 %, respectively [37]. Serum GM testing has been found to be less useful for solid organ transplant recipients. Some reports have noted improvement in the diagnostic capabilities of the assay when applied to BAL specimens in this patient population [38–40]. These data should be interpreted with some caution as these studies were dominated by adult patients. Additionally, there is a real risk for false positive results in this setting especially among lung transplant patients where Aspergillus pulmonary colonization is known to exist.
The evidence to support GM testing on cerebral spinal fluid (CSF) is limited to case reports and case series that included patients where the suspicion of an IA infection was high [41, 42]. At this time, GM testing on BAL and CSF specimens should be limited to patients where suspicion for an active IA infection is high and routine testing on all obtained BAL and CSF should be discouraged as false positive results can be misleading and result in unnecessary additional investigations. Finally, Fisher et al., recently reported on the simultaneous surveillance of serum and urine GM levels in children with prolonged neutropenia [20]. The results were promising and suggested that urine may be a reasonable specimen for early detection of GM. However, the increased number of false positive results dictates refinement of the assay with urine specific thresholds for positivity before it can be endorsed in this manner.
Galactomannan Levels to Monitor Response to Therapy
Recent publications have investigated the predictive value of baseline GM levels for IA outcomes and also evaluated the utility of following serum GM testing to monitor effectiveness of antifungal therapy in patients with IA [43–45]. Bergeron et al., showed that baseline elevation of the GM index was associated with mortality at 60 days (Hazard ratio of 1.25 (95 % CI: 1.1. to 1.43) per one unit increase in the GM index) and that follow-up GM levels after initiating therapy were accurately correlated with both improvement and lack of improvement of IA [44]. Nouer et al., compared two definitions for successful antifungal therapy in 115 adults with IA. The first definition was based on GM testing results and the second definition relied on EORTC criteria for establishing improvement [43]. They found a 91 % agreement for successful response to antifungal therapy for the two definitions. Finally, Chai et al., focused on the kinetics of GM assay results in the first two weeks after initiation of IA treatment in 202 patients [45]. A GM index reduction of >35 % predicted a good response to therapy by week 12, likewise an increase in the GM index from negative to positive within 2 weeks of starting antifungal therapy predicted a poor response. The majority of patients in each of these trials were adults and thus the generalizability of these results to children is not clear. However, it is reasonable to consider follow-up GM assay results as an adjunctive measure to monitoring the effectiveness of IA therapy in children.
Beta-D-Glucan Testing
History of Beta-D-Glucan
Beta glucans are a group of heterogeneous glucose polysaccharides linked by beta glycosidic bonds. Contrary to GM, BG is found in the cell wall of various pathogenic fungi including but not limited to species of Aspergillus, Candida, Fusarium, and Scedosporium. It should be noted that BG is also found in Pneumocystis jiroveci but notably absent from Cryptococci and organisms of the Mucorales family (such as Absidia, Mucor and Rhizopus) [46].
The detection of BG is based on the use of factor G prepared from the amebocytes of either Limulus polyphemus (American horseshoe crab) or Tachypleus tridentatus (Japanese horseshoe crab) [46]. The discovery of this horseshoe crab lysate extract dates back to 1968, when Levin and Bang first reported on the ability to detect bacterial endotoxin using horseshoe crabs amebocytes. Their original assay required the activation of the ambocytes’ factor C by bacterial endotoxin resulting in activation of a clotting cascade [47]. It was eleven years later that Lehmann and Reiss isolated both GM and BG from the serum of rabbits infected with Aspergillus fumigatus [13]. Beta glucan was found to be non-antigenic in these early animal studies and thus not initially pursued as a biomarker. A short time later Morita et al., discovered that BG interacted with factor G that triggered the coagulation cascade of the horseshoe crab amebocytes but via an alternate pathway to that of bacterial endotoxin [48]. Obayashi et al., subsequently created lysate from the amebocytes that retained factor G but was lacking in factor C establishing an assay for the detection of BG that did not also respond to bacterial endotoxin [49].
There are currently two commercially made BG assay kits, the Fungitec G Test MK® manufactured by the Japanese company Seikagaku Biobusiness Corporation and the Fungitell® Assay (formerly Glucatell) from the Associates of Cape Cod, Inc. Each kit relies on the use of amebocyte lysate from either Japanese or American horseshoe crabs. The Fungitell® Assay has received FDA approval and thus will be the focus of the remainder of this section. It should be noted that the two kits have been shown to be comparable in the identification of BG and do not cross react with other non-(1 → 3) beta-D-glucans [7].
Adult Data on Beta-D-Glucan Testing
The operating characteristics of the BG assay for identifying all IFI were initially elucidated in two adult cohorts. The first included twice weekly testing during the neutropenic periods of 283 adult patients with newly diagnosed AML or myelodysplastic syndrome undergoing initial induction chemotherapy and receiving fungal prophylaxis with either caspofungin or itraconazole [7]. The resultant sensitivity, specificity, PPV and NPV for diagnosing proven or probable IFI of 100 %, 90 %, 43 %, and 100 %, respectively. Only four of the IFI events were specifically IA. For all four IA cases the BG result was positive and for 3 of the 4 it became positive before IA was clinically apparent.
The second study evaluated 95 adult patients with fever and neutropenia down to 16 years of age [8]. Thirty-eight patients with proven, probable or possible IFI were identified, 24 of which were thought to have possible or probable IA. The resultant sensitivity, specificity, PPV and NPV were 97.4 %, 28.6 %, 55.2 %, and 92.3 %. Likely the specificity reported was reduced because of inclusion of patients with a “possible” IFI designation as this designation is much less definitive. Operating characteristics specific to IA could not be elucidated given the data published.
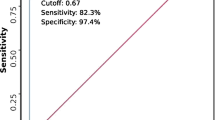
Although the Fungitell® Assay can detect BG levels down to 1 pg/mL the manufacturer recommended cutoff for a positive value is >80 pg/mL with an indeterminate range of 60-79 pg/mL and a negative result being <60 pg/mL. The indeterminate range was created to account for normal human serum levels of BG ranging from 10-40 pg/mL. These baseline human levels are thought to result from the presence of yeast in the normal flora of the alimentary and gastrointestinal tract.
Pediatric Data on Beta-D-Glucan Testing
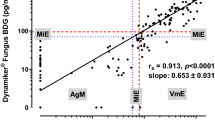
A study evaluating this BG assay in children without risk for IFI was performed to establish pediatric baseline BG levels. The results suggested that children can have substantially elevated levels of BG in the absence of IFI resulting in significant concern in how to interpret BG assay results in children [50•]. To date, there are limited data regarding BG testing in at-risk pediatric immunocompromised patients [51, 52] making it impossible to make any recommendations for employing BG testing for detection of IA in children. Fortunately, large pediatric prospective studies in both the United States and Europe are currently ongoing. The results of these studies in the coming years should help to inform the utility or lack thereof for BG testing in children.
Sources of False Positivity
Clinicians utilizing either the GM or BG assays should be aware of factors that have been sighted as possible sources for false positive results. Table 2 denotes a number of medications, medical interventions, and other organisms that have been suggested as possible causes of false positive results for BG and GM testing [46, 53, 54]. Concomitant piperacillin-tazobactam exposure has often been cited as a possible cause of a false positive GM result.[24] This is concerning for institutions where this medication is used in the setting of fever and neutropenia. However, recent data has suggested that false positive results secondary to piperacillin-tazobactam are not specific to the antibiotic but rather the manufacturer of the antibiotic [55•, 56]. Similarly, recent studies have exonerated other beta lactam antibiotics such as ampicillin-sulbactam as a cause of false positive GM or BG testing [57]. Pneumocystis jiroveci is also listed as a cause of a “false positive” BG test. Technically this is not a true false positive as the BG assay is detecting beta glucan from the cell wall of Pneumocystis jiroveci as it would for other fungal infections. The BG assay has been successfully used to identify Pneumocystis jiroveci in various immunocompromised populations [58]. However, in this instance the implications for therapeutic management would of course be different.
Galactomannan and Beta-D-Glucan Assays as Adjunctive Tools
Most of the studies evaluating the effectiveness of GM and BG testing for detecting IA have done so in isolation during a specific clinical scenario such as neutropenia or neutropenia with fever. Alternatively, the results of these assays can be used as adjuncts to clinical and radiographic results to guide clinicians not just in the diagnosis of IA but also in the appropriate time to initiate antifungal therapy. Cordonnier et al., took this approach and compared the use of GM testing in conjunction with other clinical and radiographic findings to guide pre-emptive initiation of antifungal therapy versus empiric antifungal therapy in adults with persistent fever and neutropenia despite broad-spectrum antibiotics [59•]. Although IFI was ultimately diagnosed more frequently in the pre-emptive arm, there was no difference in IFI-related mortality and there was a noted reduction in antifungal use. Based on these and other similar studies, the 2010 IDSA update for IA endorsed this pre-emptive approach that leverages non-invasive biomarkers in conjunction with clinical and radiographic data as an alternative option to routine empiric antifungal therapy for prolonged fever and neutropenia [60]. Subsequent to the release of the IDSA guidelines Pagano et al., published a prospective adult observational trial that revealed an increased rate of IFI and attributable mortality in patients managed in a pre-emptive approach resulting in questions regarding the safety of pre-emptive therapy [61]. Thus far no such study has been performed in a pediatric specific cohort. Pediatric studies that combine data from these biomarkers with data from clinical, radiographic and other traditional laboratory results to guide both the diagnosis of IA and guidance on initiating antifungal therapy are urgently needed. Until such studies are completed, it is difficult to endorse such approaches in children.
Conclusion
For many decades researchers and clinicians have yearned for diagnostic tools that would improve upon the abilities of traditional diagnostic testing to identify IA. The primary goal of improved diagnostic modalities is to identify the presence of IA at its earliest point of onset so that important therapeutic measures can be enacted and thus better outcomes achieved. Galactomannan, and BG assays are two non-invasive biomarkers that are bringing us closer to this goal. However, in isolation none of these laboratory tools are perfect for detecting IA. Based on the reviewed data it is reasonable to employ serum GM testing in at risk pediatric patients. Although the data are less convincing, GM testing in BAL or CSF specimens is reasonable in patients with a high suspicion for IA. Comparatively, the data for BG testing in pediatric patients are much less and the lack of information on an appropriate threshold for this assay in children should limit its application in pediatric patients until further evidence is available.
To date, both GM and BG assays have received the most attention in the medical literature as biomarkers for the diagnoses of IA. The time from initial discovery of these two biomarkers to their application in clinical settings required multiple decades of investigation. Fortunately, other testing modalities for early detection of IA are in development or are on the horizon. Aspergillus PCR testing of the blood has received significant attention in recent years [62]. Most recently, Badiee et al., reported reassuring operating characteristics of a commercially available nested-PCR for Aspergillus in 62 pediatric patients with hematologic disorders [63]. Although the results of PCR testing were favorable, it should be noted that the incidence rate of IA was extremely high in this cohort (27.4 %) and thus the results may not be generalizable. Before routine use of an Aspergillus PCR can be supported in children, there needs to be further investigations to better define the operating characteristics in at risk populations, to establish optimal testing strategies, and to standardize testing processes. In addition to PCR testing, various novel proteomic techniques have been employed to more efficiently identify a number of candidate proteins that may not only serve as new biomarkers to aide in the diagnosis of IA but that also have the potential to correlate with Aspergillus pathogenicity and stage of infection [64, 65].
Pediatric clinicians electing to employ these diagnostic modalities need to do so judiciously in clinical scenarios where the pre-test probability for detecting IA is relatively high. Indiscriminate use of these tests will result in unnecessary medical expenditures and the potential to misinterpret their results. Researchers need to continue to establish the operating characteristics of each of these tests across various patient cohorts and under various clinical conditions. As noted previously fungal biomarkers present the possibility of identifying the presence of IA many days before clinical symptoms are apparent. While it is reasonable to theorize that an earlier diagnosis could translate into improved outcomes, no study to date has shown that biomarker testing has the ability to reduce the morbidity and mortality of IA. Therefore, additional efforts need to focus not just on determining the operating characteristics of novel fungal biomarkers but also to define their ability to reduce the morbidity and mortality of IA. Ultimately, it is likely that integrating these and similar future diagnostic tests with other clinical and traditional diagnostic data will result in the greatest benefit for identifying IA at its earliest point of onset so that the morbidity and mortality of this feared infection can be reduced.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
• Burgos A, Zaoutis TE, Dvorak CC, et al. Pediatric invasive aspergillosis: a multicenter retrospective analysis of 139 contemporary cases. Pediatrics. 2008;121:e1286–94. This manuscript represents one of the largest collections of pediatric patients with invasive aspergillosis and describes important case characteristics and their outcomes.
Zaoutis TE, Heydon K, Chu JH, Walsh TJ, Steinbach WJ. Epidemiology, outcomes, and costs of invasive aspergillosis in immunocompromised children in the United States, 2000. Pediatrics. 2006;117:e711–6.
Denning DW. Therapeutic outcome in invasive aspergillosis. Clin Infect Dis. 1996;23:608–15.
von Eiff M, Roos N, Schulten R, Hesse M, Zühlsdorf M, van de Loo J. Pulmonary aspergillosis: early diagnosis improves survival. Respiration. 1995;62:341–7.
Ascioglu S, Rex JH, De Pauw B, et al. Defining opportunistic invasive fungal infections in immunocompromised patients with cancer and hematopoietic stem cell transplants: an international consensus. Clin Infect Dis. 2002;34:7–14.
Marr KA, Balajee SA, McLaughlin L, Tabouret M, Bentsen C, Walsh TJ. Detection of galactomannan antigenemia by enzyme immunoassay for the diagnosis of invasive aspergillosis: variables that affect performance. J Infect Dis. 2004;190:641–9.
Odabasi Z, Mattiuzzi G, Estey E, et al. Beta-D-glucan as a diagnostic adjunct for invasive fungal infections: validation, cutoff development, and performance in patients with acute myelogenous leukemia and myelodysplastic syndrome. Clin Infect Dis. 2004;39:199–205.
Ellis M, Al-Ramadi B, Finkelman M, et al. Assessment of the clinical utility of serial beta-D-glucan concentrations in patients with persistent neutropenic fever. J Med Microbiol. 2008;57:287–95.
Maertens J, Verhaegen J, Lagrou K, Van Eldere J, Boogaerts M. Screening for circulating galactomannan as a noninvasive diagnostic tool for invasive aspergillosis in prolonged neutropenic patients and stem cell transplantation recipients: a prospective validation. Blood. 2001;97:1604–10.
Pfeiffer CD, Fine JP, Safdar N. Diagnosis of invasive aspergillosis using a galactomannan assay: a meta-analysis. Clin Infect Dis. 2006;42:1417–27.
•• Leeflang MM, Debets-Ossenkopp YJ, Visser CE, et al. Galactomannan detection for invasive aspergillosis in immunocompromized patients. Cochrane Database Syst Rev. 2008; CD007394. This is a meta-analysis of the studies investigating galactomannan testing in immunocompromised patients. Importantly this publication represents mostly adult patient populations.
De Pauw B, Walsh TJ, Donnelly JP, et al. Revised definitions of invasive fungal disease from the European Organization for Research and Treatment of Cancer/Invasive Fungal Infections Cooperative Group and the National Institute of Allergy and Infectious Diseases Mycoses Study Group (EORTC/MSG) Consensus Group. Clin Infect Dis. 2008;46:1813–21.
Lehmann PF, Reiss E. Invasive aspergillosis: antiserum for circulating antigen produced after immunization with serum from infected rabbits. Infect Immun. 1978;20:570–2.
Reiss E, Lehmann PF. Galactomannan antigenemia in invasive aspergillosis. Infect Immun. 1979;25:357–65.
Kurup VP, Kumar A. Immunodiagnosis of aspergillosis. Clin Microbiol Rev. 1991;4:439–56.
Stynen D, Sarfati J, Goris A, et al. Rat monoclonal antibodies against Aspergillus galactomannan. Infect Immun. 1992;60:2237–45.
Stynen D, Goris A, Sarfati J, Latge JP. A new sensitive sandwich enzyme-linked immunosorbent assay to detect galactofuran in patients with invasive aspergillosis. J Clin Microbiol. 1995;33:497–500.
Verweij PE, Stynen D, Rijs AJ, de Pauw BE, Hoogkamp-Korstanje JA, Meis JF. Sandwich enzyme-linked immunosorbent assay compared with Pastorex latex agglutination test for diagnosing invasive aspergillosis in immunocompromised patients. J Clin Microbiol. 1995;33:1912–4.
Armenian SH, Nash KA, Kapoor N, et al. Prospective monitoring for invasive aspergillosis using galactomannan and polymerase chain reaction in high risk pediatric patients. J Pediatr Hematol Oncol. 2009;31:920–6.
Fisher BT, Zaoutis TE, Park JR, et al. Galactomannan Antigen Testing for Diagnosis of Invasive Aspergillosis in Pediatric Hematology Patients. Journal of the Pediatric Infectious Diseases Society. 2012;1:103–11.
Rohrlich P, Sarfati J, Mariani P, et al. Prospective sandwich enzyme-linked immunosorbent assay for serum galactomannan: early predictive value and clinical use in invasive aspergillosis. Pediatr Infect Dis J. 1996;15:232–7.
Sulahian A, Boutboul F, Ribaud P, Leblanc T, Lacroix C, Derouin F. Value of antigen detection using an enzyme immunoassay in the diagnosis and prediction of invasive aspergillosis in two adult and pediatric hematology units during a 4-year prospective study. Cancer. 2001;91:311–8.
Hovi L, Saxen H, Saarinen-Pihkala UM, Vettenranta K, Meri T, Richardson M. Prevention and monitoring of invasive fungal infections in pediatric patients with cancer and hematologic disorders. Pediatr Blood Cancer. 2007;48:28–34.
Steinbach WJ, Addison RM, McLaughlin L, et al. Prospective Aspergillus galactomannan antigen testing in pediatric hematopoietic stem cell transplant recipients. Pediatr Infect Dis J. 2007;26:558–64.
Fisher BT, Harris T, Torp K, et al. Establishment of an 11-Year Cohort of 8733 Pediatric Patients Hospitalized at United States Free-standing Children's Hospitals With De Novo Acute Lymphoblastic Leukemia From Health Care Administrative Data. Med Care 2012; epub ahead of print.
•• Lehrnbecher T, Phillips R, Alexander S, et al. Guideline for the Management of Fever and Neutropenia in Children With Cancer and/or Undergoing Hematopoietic Stem-Cell Transplantation. Journal of Clinical Oncology. 2012; epub ahead of print. This manuscript is the first pediatric fever and neutropenia guideline. It summarizes the impact of both galactomannan and beta glucan testing in children.
Marr KA, Laverdiere M, Gugel A, Leisenring W. Antifungal therapy decreases sensitivity of the Aspergillus galactomannan enzyme immunoassay. Clin Infect Dis. 2005;40:1762–9.
Verweij PE, Weemaes CM, Curfs JH, Bretagne S, Meis JF. Failure to detect circulating Aspergillus markers in a patient with chronic granulomatous disease and invasive aspergillosis. J Clin Microbiol. 2000;38:3900–1.
Mortensen KL, Knudsen JB, Jensen-Fangel S, Stausbøl-Grøn B, Arendrup MC, Petersen E. Successful management of invasive aspergillosis presenting as pericarditis in an adult patient with chronic granulomatous disease. Mycoses. 2011;54:e233–6.
Falcone EL, Holland SM. Invasive fungal infection in chronic granulomatous disease: insights into pathogenesis and management. Curr Opin Infect Dis. 2012;25:658–69.
Husain S, Kwak EJ, Obman A, et al. Prospective assessment of Platelia™ Aspergillus galactomannan antigen for the diagnosis of invasive aspergillosis in lung transplant recipients. Am J Transplant. 2004;4:796–802.
Kwak EJ, Husain S, Obman A, et al. Efficacy of galactomannan antigen in the Platelia™ Aspergillus enzyme immunoassay for diagnosis of invasive aspergillosis in liver transplant recipients. J Clin Microbiol. 2004;42:435–8.
Fortún J, Martín-Dávila P, Moreno S, et al. Risk factors for invasive aspergillosis in liver transplant recipients. Liver Transpl. 2002;8:1065–70.
Cornet M, Mallat H, Somme D, et al. Fulminant invasive pulmonary aspergillosis in immunocompetent patients–a two-case report. Clin Microbiol Infect. 2003;9:1224–7.
Gangneux JP, Camus C, Philippe B. Epidemiology of invasive aspergillosis and risk factors in non neutropaenic patients. Rev Mal Respir. 2010;27:e34–46.
Maertens J, Maertens V, Theunissen K, et al. Bronchoalveolar lavage fluid galactomannan for the diagnosis of invasive pulmonary aspergillosis in patients with hematologic diseases. Clin Infect Dis. 2009;49:1688–93.
Desai R, Ross LA, Hoffman JA. The role of bronchoalveolar lavage galactomannan in the diagnosis of pediatric invasive aspergillosis. Pediatr Infect Dis J. 2009;28:283–6.
Tabarsi P, Soraghi A, Marjani M, et al. Comparison of serum and bronchoalveolar lavage galactomannan in diagnosing invasive aspergillosis in solid-organ transplant recipients. Exp Clin Transplant. 2012;10:278–81.
Husain S, Paterson DL, Studer SM, et al. Aspergillus galactomannan antigen in the bronchoalveolar lavage fluid for the diagnosis of invasive aspergillosis in lung transplant recipients. Transplantation. 2007;83:1330–6.
Clancy CJ, Jaber RA, Leather HL, et al. Bronchoalveolar lavage galactomannan in diagnosis of invasive pulmonary aspergillosis among solid-organ transplant recipients. J Clin Microbiol. 2007;45:1759–65.
Viscoli C, Machetti M, Gazzola P, et al. Aspergillus galactomannan antigen in the cerebrospinal fluid of bone marrow transplant recipients with probable cerebral aspergillosis. J Clin Microbiol. 2002;40:1496–9.
Roilides E, Pavlidou E, Papadopoulos F, et al. Cerebral aspergillosis in an infant with corticosteroid-resistant nephrotic syndrome. Pediatr Nephrol. 2003;18:450–3.
Nouér SA, Nucci M, Kumar NS, Grazziutti M, Barlogie B, Anaissie E. Earlier response assessment in invasive aspergillosis based on the kinetics of serum Aspergillus galactomannan: proposal for a new definition. Clin Infect Dis. 2011;53:671–6.
Bergeron A, Porcher R, Menotti J, et al. Prospective evaluation of clinical and biological markers to predict the outcome of invasive pulmonary aspergillosis in hematological patients. J Clin Microbiol. 2012;50:823–30.
Chai LYA, Kullberg BJ, Johnson EM, et al. Early serum galactomannan trend as a predictor of outcome of invasive aspergillosis. J Clin Microbiol. 2012;50:2330–6.
Marty FM, Koo S. Role of (1–>3)-beta-D-glucan in the diagnosis of invasive aspergillosis. Med Mycol. 2009;47 Suppl 1:S233–40.
Levin J, Bang FB. Clottable protein in Limulus; its localization and kinetics of its coagulation by endotoxin. Thrombosis et diathesis haemorrhagica. 1968;19:186–97.
Morita T, Tanaka S, Nakamura T, Iwanaga S. A new (1-3)-b-D-glucan-mediated coagulation pathway found inLimulusamebocytes. FEBS Lett. 1981;129:318–21.
Obayashi T, Tamura H, Tanaka S, et al. A new chromogenic endotoxin-specific assay using recombined limulus coagulation enzymes and its clinical applications. Clinica chimica acta; international journal of clinical chemistry. 1985;149:55–65.
• Smith PB, Benjamin DK, Alexander BD, Johnson MD, Finkelman MA, Steinbach WJ. Quantification of 1,3-beta-D-glucan levels in children: preliminary data for diagnostic use of the beta-glucan assay in a pediatric setting. Clin Vaccine Immunol. 2007;14:924–5. This manuscript questions the appropriate threshold level for beta glucan testing in children.
Zhao L, Tang J-Y, Wang Y, et al. Value of plasma beta-Glucan in early diagnosis of invasive fungal infection in children. Chin J Contemp Pediatr. 2009;11:905–8.
Mularoni A, Furfaro E, Faraci M, et al. High Levels of beta-D-glucan in immunocompromised children with proven invasive fungal disease. Clin Vaccine Immunol. 2010;17:882–3.
Marty FM, Lowry CM, Lempitski SJ, Kubiak DW, Finkelman MA, Baden LR. Reactivity of (1–>3)-beta-d-glucan assay with commonly used intravenous antimicrobials. Antimicrob Agents Chemother. 2006;50:3450–3.
Wheat LJ, Walsh TJ. Diagnosis of invasive aspergillosis by galactomannan antigenemia detection using an enzyme immunoassay. Eur J Clin Microbiol Infect Dis. 2008;27:245–51.
• Mikulska M, Furfaro E, Del Bono V, et al. Piperacillin/tazobactam (Tazocin™) seems to be no longer responsible for false-positive results of the galactomannan assay. J Antimicrob Chemother. 2012;67:1746–8. This manuscript presents data that exonerates piperacillin/tazobactam as a cause for false positive galactomannan testing. This is important as piperacillin/tazobactam has long been implicated as a contributor to false positivity.
Gerlinger MP, Rousselot P, Rigaudeau S, et al. False positive galactomannan Platelia due to piperacillin-tazobactam. Med Mal Infect. 2012;42:10–4.
Metan G, Agkus C, Nedret Koc A, Elmali F, Finkelman MA. Does ampicillin-sulbactam cause false positivity of (1,3)-beta-D-glucan assay? A prospective evaluation of 15 patients without invasive fungal infections. Mycoses. 2012;55:366–71.
Karageorgopoulos DE, Vouloumanou EK, Ntziora F, Michalopoulos A, Rafailidis PI, Falagas ME. β-D-glucan assay for the diagnosis of invasive fungal infections: a meta-analysis. Clin Infect Dis. 2011;52:750–70.
• Cordonnier C, Pautas C, Maury S, et al. Empirical versus Preemptive Antifungal Therapy for High–Risk, Febrile, Neutropenic Patients: A Randomized, Controlled Trial. Clin Infect Dis. 2009;48:1042–51. This manuscript presents a controlled comparison of two therapeutic options for antifungal therapy in patients with fever and neutropenia.
Freifeld AG, Bow EJ, Sepkowitz KA, et al. Clinical practice guideline for the use of antimicrobial agents in neutropenic patients with cancer: 2010 Update by the Infectious Diseases Society of America. Clin Infect Dis. 2011;52:427–31.
Pagano L, Caira M, Nosari A, et al. The use and efficacy of empirical versus pre-emptive therapy in the management of fungal infections: the HEMA e-Chart Project. Haematologica. 2011;96:1366–70.
Klingspor L, Loeffler J. Aspergillus PCR formidable challenges and progress. Med Mycol. 2009;47 Suppl 1:S241–7.
Badiee P, Alborzi A, Karimi M, et al. Diagnostic potential of nested PCR, galactomannan EIA, and beta-D-glucan for invasive aspergillosis in pediatric patients. J Infect Dev Ctries. 2012;6:352–7.
Teutschbein J, Albrecht D, Pötsch M, et al. Proteome profiling and functional classification of intracellular proteins from conidia of the human-pathogenic mold Aspergillus fumigatus. J Proteome Res. 2010;9:3427–42.
Kniemeyer O, Lessing F, Brakhage AA. Proteome analysis for pathogenicity and new diagnostic markers for Aspergillus fumigatus. Med Mycol. 2009;47 Suppl 1:S248–54.
Disclosure
The author has received grants from NIH and Pfizer Pharmaceuticals.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fisher, B.T. The Role of Biomarkers for Diagnosis of and Therapeutic Decisions Related to Invasive Aspergillosis in Children. Curr Fungal Infect Rep 7, 7–14 (2013). https://doi.org/10.1007/s12281-012-0127-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12281-012-0127-5