Abstract
The U.S. Clinical and Laboratory Standards Institute (CLSI) and the European Committee of Antimicrobial Susceptibility Testing (AFST-EUCAST) have developed broth microdilution methodologies for testing yeasts and filamentous fungi (molds). The mission of these methodologies is to identify in vitro antifungal resistance, which is accomplished by the use of either clinical breakpoints (CBPs), or to a lesser degree, epidemiologic cutoff values (ECVs). The newly adjusted and species-specific CLSI CBPs for Candida spp. versus fluconazole and voriconazole have ameliorated some of the differences between the two methodologies. In the absence of CBPs for mold testing, CLSI ECVs are available for six Aspergillus species versus the triazoles, caspofungin and amphotericin B. Recently, breakpoints were developed by the EUCAST for certain Aspergillus spp. versus amphotercin B, itraconazole and posaconazole, which to some extent are comparable to ECVs. We summarize these latest accomplishments, which have made possible the harmonization of some susceptibility cutoffs, if not methodologies for some agent/species combinations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The incidence and prevalence of invasive fungal infections continue to increase, especially among chemically induced immunosuppressed patients [1–3, 4•]. Such increase prompted the introduction of new systemic antifungal agents, and the development of standardized broth microdilution methods for the in vitro susceptibility testing of yeasts and filamentous fungi (molds) by both the U.S. Clinical and Laboratory Standards Institute (CLSI) [5–7] and the European Committee of Antimicrobial Susceptibility Testing (AFST-EUCAS) [8, 9]. The availability of reliable methodologies made possible the study of mechanisms of resistance and cross-resistance in Candida spp., and more recently in Aspergillus spp. [10•, 11•, 12•, 13•, 14, 15•, 16, 17, 18•, 19]. The association of genetic mutations, high minimum inhibitory concentrations (MICs) and clinical outcome has been also elucidated. Standardization also made possible the definition of clinical breakpoints (CBPs) for the more common Candida spp. (by both CLSI and EUCAST) [20•, 21•, 22•, 23•, 24•, 25•] and some Aspergillus spp. (by EUCAST) [26•], as well as epidemiologic cutoffs (ECVs) for a variety of Aspergillus (by CLSI and EUCAST), Cryptococcus and Candida species (by CLSI) [27•, 28•, 29•, 30•, 31, 32•, 33•, 34•, 35•], and the important antifungal agents (triazoles, echinocandins, amphotericin B and flucytosine) that are currently available for the treatment/prevention of invasive fungal infections [36–38]. This review will focus on the published events that have made possible the comparison not only of testing conditions, but of susceptibility endpoints developed by both CLSI and EUCAST. Because of this, we only discuss testing parameters and cutoffs values when they are available by both organizations.
Antifungal Susceptibility Methods
CLSI and EUCAST Parameters for Testing Candida spp.
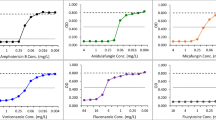
The CLSI and EUCAST broth microdilution standardized methodologies have been discussed in detail elsewhere [10•, 11•, 39, 40], as well in the CLSI (M27-A3) and EUCAST (EDef 7.2) documents [5–9]. The similar testing conditions are (Table 1): RPMI-1640 (RPMI) broth, incubation temperatures (35° and 37° C) and time (24 h), a prominent inhibition of growth (≥50 %) for testing the susceptibilities of Candida spp. to triazoles and echinocandins. The differences are: inoculum densities (0.5 × 103 to 2.5 × 103 CFU/ml and 0.5 × 105 to 2.5 × 105 CFU/ml), the RPMI broth glucose content (0.2 % and 2.0 %), the microdilution wells (round and flat-bottom), and MIC determination (visual and spectrophotometric). Despite these differences, early and recent comparisons of EUCAST and the more practical CLSI 24 h triazole MICs [39–45], as well as of amphotericin B and flucytosine [45], have yielded comparable results regarding both essential, and more importantly, categorical agreement [42, 44].
CLSI and EUCAST Parameters for Testing Cryptococcus spp.
Another area where testing conditions differ between both organizations is for the Cryptoccocus neoformans–C. gattii species complex. As early as the 1990s, the CLSI established that, except for the incubation time (72 h), the standard parameters for this group of fungi were the same as those for Candida spp. [5, 6]. Based on large numbers of isolates of these species (from numerous laboratories) for which MICs were collected during the last 10 to 15 years, ECVs were defined by the CLSI for the Cryptoccocus neoformans–C. gattii species complex versus amphotericin B, flucytosine and the triazoles [33•, 34•]. In 2012, the EUCAST methodology was adopted for the testing of Cryptococcus species, and the plates read when the OD value is above 0.2. In cases with insufficient growth, it is suggested that the test be repeated, but that the trays be incubated at 30 °C [8, 46•]. The comparison with CLSI methodology was complicated, since growth by the CLSI method was insufficient to allow spectrophotometric MIC determination.
CLSI and EUCAST Parameters for Testing Molds
The CLSI M38-A2 document provides guidelines for non-dermatophyte molds with amphotericin B, triazoles and echinocandins [7]. The EUCAST has a similar broth microdilution standard, again except for the sugar content of the RPMI broth (2 % and 0.2 % dextrose), the inoculum concentrations (~105 CFU/ml adjusted by conidial counting and ~104 CFU/ml adjusted by spectrophotometer), and the final DMSO concentration (0.5 % and 1 %) [7, 9]. Both methods recommend the determination of minimal effective concentrations (MECs) when testing echinocandins, instead of the traditional MIC when evaluating other agents [7, 9]. An early comparison of testing conditions for molds demonstrated that the higher EUCAST inoculum size and glucose RPMI concentration did not significantly elevated MICs of amphotericin B and itraconazole [47]. But a recent study reported that voriconazole EUCAST MICs are usually one dilution higher that CLSI values [32•].
Interpretive Guidelines for Candida and Aspergillus Species
CLSI and EUCAST Clinical Breakpoints for Candida spp.
As for any antimicrobial agent, detection of in vitro resistance is an important factor in the treatment of invasive fungal infections (e.g., Candida infections) for which agents have been licensed. For in vitro results to be meaningful, CBPs or ECVs should be available and established using data obtained by standardized methods. During the last two years, CBPs that serve to differentiate an organism as treatable or nontreatable [48•] have been adjusted (lowered) by the CLSI for most of the common Candida spp. versus fluconazole, voriconazole and the three echinocandins (Table 2) [20•, 21•, 22•]. Also, EUCAST breakpoints are available for amphotericin B, anidulafungin, fluconazole, posaconazole, and voriconazole [23•, 24•, 25•].
CBPs for Candida spp. and Fluconazole and Voriconazole
Between 1997 and 2006, the CLSI established susceptible (≤8 μg/ml for fluconazole and 1 μg/ml for voriconazole) and resistant (≥64 μg/ml and ≥4 μg/ml, respectively) CBPs to encompass all Candida spp. During the last three years, the following important factors demanded the adjustment of these CBPs: the CLSI validated the 24 h (when growth permits it) incubation time for testing these agents [41], the need to have species-specific CBPs, and the perception that the original CBPs were not sensitive enough to identify in vitro resistance to these agents, especially when testing C. albicans, C. parapsilosis and C. tropicalis. Therefore, using mutant strains (e.g., due to either target enzyme modifications or reduction of access of the triazole to the target), new pharmacokinetic (PK) and pharmacodynamic (PD) information, MIC distributions, and clinical experience with either mucosal and invasive candidiasis (fluconazole) or with non-neutropenic candidemia patients (voriconazole), CLSI CBPs were adjusted: susceptible (≤ 2 μg/ml for fluconazole and ≤0.125 μg/ml for voriconazole) and resistant (≥ 8 μg/ml and ≥1 μg/ml, respectively) for C. albicans, C. parapsilosis and C. tropicalis [20•, 21•]. No susceptible endpoint was established for C. glabrata and fluconazole. For the combination of voriconazole and C. glabrata, insufficient data that demonstrates a correlation between CLSI MICs and response to therapy precluded the definition of CBPs. These species-specific CBPs would better recognize non-treatable or resistant isolates. Therefore, although both organizations disagree with respect to the resistant endpoint of voriconazole and C. albicans, C. parapsilosis and C. tropicalis (resistant endpoints: EUCAST ≥ 0.25 μg/ml and CLSI ≥ 1 μg/ml), there is complete agreement regarding fluconazole resistant endpoint for these three species (≥8 μg/ml) (Table 2).
CBPs for Candida spp. and the Echinocandins
In 2008, the CLSI established a susceptible CBP (≤2 μg/ml) for echinocandins and all Candida spp. However, using fks1 mutant strains, Garcia-Effron et al. [49, 50] demonstrated that although caspofungin MICs > 2 μg/ml captured almost 100 % of mutant strains, the MICs of anidulafungin and micafungin that captured 95 % of these mutants were lower for C. albicans (>0.5 μg/ml) and C. glabrata (>0.25 μg/ml). More recently, the single susceptible echinocandin CBP was adjusted to species-specific CBPs; susceptible ≤0.25 μg/ml and resistant ≥1 μg/ml for C. albicans, C. krusei and C. tropicalis; lower interpretive endpoints were established for C. glabrata, which also were echinocandin-dependent (Table 2). Since the EUCAST has not established interpretive breakpoints for caspofungin and micafungin, due to insufficient evidence of correlations between in vitro and clinical response, we focus on anidulafungin CBPs (Table 2). EUCAST breakpoints for anidulafungin are based on ECVs, clinical experience and as pharmacokinetic information [24•]. Although both organizations are in agreement regarding the resistant endpoint of anidulafungin and C. parapsilosis (≥8 μg/ml), once more, EUCAST resistant endpoints are lower for C. albicans (≥0.06 μg/ml versus ≥1 μg/ml), and C. glabrata, C. krusei, and C tropicalis (≥0.12 μg/ml versus ≥0.5 μg/ml and ≥1 μg/ml); differences among susceptible endpoints are depicted in Table 2. The reason for these discrepancies could be that although clinical data from three clinical trials were used for the definition of anidulafungin EUCAST endpoints, correlation of EUCAST MICs and clinical response was not possible, since EUCAST in vitro data were not obtained at the time [24•].
Epidemiological Cutoff Values (ECVs) for Candida spp.
In contrast to CBPs, the ECV is the susceptibility endpoint that differentiates between wild type (WT, isolates not harboring resistant mechanisms) from non-WT isolates (harboring one or more resistant markers) [48•, 51]. Among Candida spp., ECVs are usually lower than the CBP. Although an organism with an MIC above the drug ECV (non-WT) shows reduced susceptibility and is less likely to respond to the agent being evaluated as compared to the WT population, it may respond if the MIC is below the breakpoint. CLSI CBPs for Candida spp. versus itraconazole, amphotericin B and flucytosine are not available, due the lack of sufficient clinical and in vitro data to demonstrate correlations. Instead, the CLSI has recently defined ECVs that are based on CLSI MIC data from multiple laboratories [35•]. We focus on the comparison of CLSI amphotericin B ECVs and EUCAST breakpoints for Candida spp. (Table 2), since the latter organization has no interpretive values for either itraconazole or flucytosine; CLSI ECVs for those two latter agents can be found elsewhere [35•, 40].
ECVs and Breakpoints for Candida spp. and Amphotericin B
The EUCAST resistant amphotericin B breakpoints are lower (>1 μg/ml) than the CLSI non-WT endpoints (or isolates with reduced susceptibility to amphotericin B; >2 μg/ml) for the common Candida spp. (Table 2). These differences must be due to testing conditions. Based on peak attainable serum concentrations of 2 μg/ml and the pharmacodynamic correlate of the peak serum concentration-to-MIC ratio of 2 as the predictor of maximal activity, the cutoff of amphotericin B resistance traditionally has been an MIC of ≥1 μg/ml [40]. But so far, attempts to correlate this vitro result (≥1 μg/ml) with clinical outcome in Candida infections have failed [52]. One of the problems is the scarcity of Candida isolates for which the MIC is >2 μg/ml. Therefore, a Candida isolate with such a high MIC should be considered unusual and less likely to respond to amphotericin B therapy.
CLSI and EUCAST ECVs and Breakpoints for Aspergillus spp.
Because recent clinical studies (not designed for correlation purposes) have only provided some insights regarding the potential value of MICs in certain mold–drug combinations, CLSI CBPs are not available for mold testing. For example, during voriconazole clinical trials for aspergillosis, its efficacy data is based on response to treatment of patients infected mostly with WT isolates. However, CLSI ECVs are available for six species of Aspergillus (Aspergillus fumigatus, A. flavus, A. nidulans, A. niger, A. terreus, and A. versicolor) and five antifungal agents (amphotericin B, three triazoles and caspofungin) [28•, 29•, 30•]; Table 3 depicts CLSI ECVs and available EUCAST breakpoints [26•]. As for Candida spp., ECVs could characterize the susceptibility of Aspergillus spp. to antifungal agents and monitor the emergence of strains with mutations and reduced antifungal activity.
ECVs and breakpoints for Aspergillus spp. and Amphotericin B
Although there are available amphotericin B CLSI ECVs for six Aspergillus spp., EUCAST has defined breakpoints only for A. fumigatus and A. niger, and both values are one dilution lower than CLSI ECVs (Table 3) [26•, 30•]. Information is scarce regarding the relationship between resistance mechanisms, high amphotericin MICs and clinical response to therapy; it is mostly available for A. terreus (intrinsically resistant to this agent) and A. flavus [10•, 11•]. Alteration of the cell wall composition of A. flavus has been responsible for amphotericin B resistance (MICs > 1 μg/ml), while catalase production instead of ergosterol content has played a role in A. terreus resistance to this agent [12•].
ECVs and Breakpoints for Aspergillus spp. and Triazoles
The clinical relevance of mold testing remains uncertain, but both CLSI and EUCAST methodologies have elucidated the complexity of cross-resistance among triazoles, especially in A. fumigtus. Triazole resistance (MICs > 2 μg/ml) has been associated with single or multiple point mutations of the cyp51A gene in A. fumigtus and A. flavus, as well as the incidence of multiazole, cross-resistance and patient failure to triazole treatment [13•, 14, 15•, 16, 27•, 28•]. However, other host and drug factors cannot be ignored. Triazole molecular resistance mechanisms have not been identified for the other non-A. fumigatus spp., but the presence of the two cyp51 genes was reported in A. terreus, and azole resistance has been associated with multiplication of cyp51A in an engineered laboratory strain of A. niger [11•].
The CLSI and EUCAST have defined itraconazole and voriconazole ECVs of ≤1 μg/ml for A. fumigatus (non-WT MICs ≥ 2 μg/ml) [27•, 28•]; these values were corroborated in a recent study [31]. With the exception of ECVs for A. nidulans and itraconazole (≤2 μg/ml by the CLSI and ≤1 μg/ml by the EUCAST), ECVs and breakpoints for A. flavus and A. terreus versus itraconazole by both organizations are the same (Table 3) [26•, 28•]. More recently, two potential susceptible breakpoints for voriconazole and A. fumigatus using either CLSI (susceptible, ≤0.5 μg/ml; resistant, >1 μg/ml) or the EUCAST (susceptible, ≤1 μg/ml; resistant, >2 μg/ml) methodologies also were suggested; these breakpoints were based on the fact that as the voriconazole MIC increased, a higher area under the concentration time curve (AUCs) was needed to achieve suppression of galactomannan in an in vitro dynamic model of invasive pulmonary aspergillosis [32•]. Again, the voriconazole ECV of 1 μg/ml was corroborated, but the EUCAST ECV was one dilution higher in that recent report (WT [no mutations] range by the CLSI 0.5–1 μg/ml and by the EUCAST 0.5–2 μg/ml). The EUCAST has not yet made decisions regarding this agent and Aspergillus spp.
Posaconazole ECVs for A. fumigatus in three different studies have been either 0.12 μg/ml or 0.25 μg/ml [27•, 28•, 31]. In 2011, the EUCAST established ≤0.12 μg/ml as the susceptible breakpoint for posaconazole versus A. fumigatus and A. terreus; both values are lower than the ECVs for these two species by the CLSI (Table 3) [26•].
In a recent study, 64 % of patients infected with a resistant A. fumigatus isolate were azole naïve and the case-fatality rate of azole-resistant invasive aspergillosis was 88 %. In addition, patients suffering a hematologic or oncologic disease were more likely to harbor an azole-resistant isolate than were other patient groups (p < 0.05) [14]. Verweij et al. [53] recommended dose escalation of voriconazole and posaconazole with isolates for which MICs are above the ECV. The other consideration is bioavailability, e.g., the limited ability to increase posaconazole exposure with the oral solution and the variability of triazole serum levels. In an animal model of A. fumigatus (cyp51A mutations), the standard dosing regimen needed to be increased when the posaconazole MIC for the infecting isolate was 0.5 μg/ml to avoid treatment failure [15•]. All these results indicate that these endpoints could be useful in the monitoring and selection of antifungal therapy in aspergillosis, but more data needs to be gathered for them to be clinically relevant. This is important, since itraconazole, voriconazole and posaconazole have a role in the prevention and treatment of chronic, allergic or invasive aspergillosis.
ECVs for Aspergillus spp. and Caspofungin
Caspofungin ECVs of 0.25 and 0.5 μg/ml are also available for six Aspergillus spp. by the CLSI; these values are listed elsewhere [29•]. But, ECVs have not been defined for any other echinocandins or by the EUCAST for any species and echinocandin. Scarce information is available regarding high caspofungin MECs and clinical failure and the presence of FKS1 resistant mutations [18•]. Yet, caspofungin MECs ≥ 1 μg/ml for three of four isolates of A. fumigatus, and breakthrough infections were observed in patients receiving either empirical or prophylactic caspofungin therapy [54], but genetic studies were not performed. The latter results are in agreement with those reported for a laboratory mutant of A. fumigatus (caspofungin MEC ≥ 16 μg/ml with a S678P amino acid change) [17].
Conclusions
Standardized broth microdilution (CLSI and EUCAST) and disk diffusion (CLSI) methods are available to test licensed antifungal agents against both Candida spp. and Aspergillus spp. Standardized broth microdilution methodologies have allowed the establishment of species-specific breakpoints for most of the common Candida spp. versus fluconazole and voriconazole (CLSI and EUCAST), posaconazole and anidulafungin (EUCAST) and the three echinocandins (CLSI). In the absence of breakpoints, species-specific ECVs have been defined for amphotericin B, itraconazole and flucytosine versus most common Candida spp.; for amphotericin B, triazoles and caspofungin versus six Aspergillus spp.; and for amphotericin B, triazoles and flucytosine versus the Cryptococcus neoformans-Cryptococcus gattii species complex (CLSI). On the other hand, the EUCAST has recently established breakpoints for some Aspergillus spp. versus amphotericin B, posaconazole (two species), and itraconazole (four species). It is expected that ECVs may serve as sensitive markers for the emergence of isolates with decreased susceptibility to the agent being evaluated, or to separate WT from non-WT isolates. The association of non-WT with mechanisms of resistance has been elucidated for some of these species/agent combinations, but more related information is needed.
The question is, how harmonized are CLSI and EUCAST standards? It is clear that there are basic differences in some of the testing conditions (e.g., inoculum size), but the shortening of the CLSI incubation time to 24 h for testing Candida spp. and the adjustment to species-specific and more sensitive CBPs indicates that fluconazole, and to some extent voriconazole, CBPs are similar, and that both methods are useful to identify and monitor in vitro resistance to these agents. The same applies to the comparison of available ECVs and breakpoints by both organizations. However, further efforts are needed, since there are several gaps in the development of susceptibility endpoints, as well as the relevance of the available ones beyond in vitro assays.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Garcia-Vidal C, Upton A, Kirby KA, et al. Epidemiology of invasive mold infections in allogeneic stem cell transplant recipients: biological risk factors for infection according to time after transplantation. Clin Infect Dis. 2008;47:1041–50.
Neofytos D, Horn D, Anaissie E, et al. Epidemiology and outcome of invasive fungal infections in adult hematopoietic stem cell transplant recipients: analysis of multicenter PATH Alliance Registry. Clin Infect Dis. 2009;48:265–73.
Meis JF, Chakrabarti A. Changing epidemiology of an emerging infection: zygomycosis. Clin Microbiol Infect. 2009;15 Suppl 5:10–4.
• Skiada S, Pagano L, Zimmerli S, et al. Zygomycosis in Europe: analysis of 230 cases accrued by the registry of the European Confederation of Medical Mycology (ECMM) Working Group on zygomycosis between 2005 and 2007. Clin Microbiol Infect. 2011;17:1859–67. A recent report of the epidemiology of mucoral infections in Europe.
Clinical and Laboratory Standards Institute (CLSI). Reference method for broth dilution antifungal susceptibility testing of yeasts. Approved standard, 3rd ed. CLSI document M27-A3. 2008; Clinical and Laboratory Standards Institute. 940 West Valley Rd, Wayne, PA.
Clinical and Laboratory Standards Institute (CLSI). Reference method for broth dilution antifungal susceptibility testing of yeasts; Informational Supplement, 3rd ed. CLSI document M27-S3. 2008; Clinical and Laboratory Standards Institute. 940 West Valley Rd, Wayne, PA.
Clinical and Laboratory Standards Institute: Reference method for broth dilution antifungal susceptibility testing of filamentous fungi. Approved standard, 2nd ed. Document M38-A2. Clinical and Laboratory Standards Institute 2008. 771 E. Lancaster Avenue, Wayne, Pennsylvania 19085.
Arendrup MC, Cuenca-Estrella M, Lass-Flörl C, Hope W, EUCAST-AFST. EUCAST definitive document EDef 7.2: method for the determination of broth dilution minimum inhibitory concentrations of antifungal agents for yeasts. Clin Microbiol Infect. 2012;18(7):E246–7. doi:10.1111/j.1469-0691.2012.03880.x. Epub 2012 May 8. PubMed PMID: 22563750
Subcommittee on Antifungal Susceptibility Testing of the ESCMID European Committee for Antimicrobial Susceptibility Testing. EUCAST technical note on the method for the determination of broth dilution minimum inhibitory concentrations of antifungal agents for conidia-forming moulds. Clin Microbiol Infect. 2008;14:982–84.
• Espinel-Ingroff A. Mold in vitro susceptibility testing: is it ready for clinical practice? Int J Clin Rev. 2012;07:o6d0i: 5275/IJCR. This recent review describes in detail reference approaches for susceptibility testing of moulds; the clinical relevance of recently defined ECVs for Aspergillus spp. is provided.
• Espinel-Ingroff A, Cantón E, Pemán J. Antifungal susceptibility testing of filamentous fungi. 2012. Curr Fungal Infect Rep. 2012;6:41–50. This article describes standard and alternative methods for the susceptibility testing of filamentous fungi as well as available susceptibility cutoff values.
• Blum G, Perkhofer S, Haas H, et al. Potential basis for amphotericin B resistance in Aspergillus terreus. Antimicrob Agents Chemother. 2008;52:1553–55. The basis for the intrinsic resistance of A. terreus to amphotericin B was investigated and it was concluded that catalase high levels may be the cause of resistance.
• Howard SJ, Cerar D, Anderson MJ, et al. Frequency and evolution of azole resistance in Aspergillus fumigatus associated with treatment failure. Emerg Infect Dis. 2009;15:1068–76. The higher incidence of azole resistance in Europe was reported.
van der Linden JW, Snelders E, Kampinga GA. Clinical implications of azole resistance in Aspergillus fumigatus, the Netherlands, 2007–2009. Emerg Infec Dis. 2011;17:1846–54.
• Mavridou E, Bruggemann RJM, Melchers WJG, et al. Efficacy of posaconazole against three clinical Aspergillus fumigatus isolates with mutations in the cyp51A gene. Antimicrob Agents Chemother. 2010;54:860–65. Higher posaconazole doses could be required for patients infected with posaconazole MICs of > 0.5 μg/ml; gene mutations were present.
Camps SMT, van der Linden JWM, Li Y, et al. Rapid Induction of multiple resistance mechanisms in Aspergillus fumigatus during azole therapy: a case study and review of the literature. Antimicrob Agents Chemother. 2012;56:1–16.
Rocha EM, Garcia-Effron G, Park S, Perlin DS. A ser67Pro substitution in Fk51p confers resistance to echinocandin drugs in Aspergillus fumigatus. Antimicrob Agents Chemother. 2007;51:4174–76.
• Walker LA, Gow NA, Munro CA. Fungal echinocandin resistance. Fungal Genet Biol. 2010;47:117–26. A summary of resistance mechanisms of echinocandins in Candida spp., and Aspergillus fumigatus is provided.
Espinel-Ingroff A. Mechanisms of resistance to antifungal agents: yeasts and filamentous fungi. Rev Iberoam Micol. 2008;25:99–104.
• Pfaller MA, Andes D, Diekema DJ, et al. Wild-type MIC distributions, epidemiological cutoff values and species-specific clinical breakpoints for fluconazole and Candida: time for harmonization of CLSI and EUCAST broth microdilution methods. Drug Resistance Updates. 2010;13:180–95. Adjusted fluconazole species-specific CBPs for Candida spp. are provided.
• Pfaller MA, Andes D, Arendrup MC, et al. Clinical breakpoints for voriconazole and Candida spp. revisited: review of microbiologic, molecular, pharmacodynamic, and clinical data as they pertain to the development of species-specific interpretive criteria. Diag Microbiol Infect Dis. 2011;70:330–43. Adjusted voriconazole species-specific CBPs for Candida spp. are provided.
• Pfaller, MA, Diekema DJ, Andes D, et al. Clinical breakpoints for the echinocandins and Candida revisited: integration of molecular, clinical, and microbiological data to arrive at species-specific interpretive criteria. Drug Resistance Updates. 2011;14:164–76. Adjusted echinocandin species-specific CBPs for Candida spp. are provided.
• Arendrup MC, Cuenca-Estrella M. Donnelly JP, and the European committee on antimicrobial susceptibility testing–subcommittee on antifungal susceptibility testing. EUCAST technical note on posaconazole. Clin Microbiol Infect. 2011;17:E16–7. doi:10.1111/j.1469-0691.2011.03646.x. Epub 2011 Sep 16. PubMed PMID: 21923779. EUCAST posaconazoleBPs for C. albicans and C. parapilosis are provided, which were not included in Table 2 of our paper.
• Arendrup MC, Rodriguez-Tudela J-L, Lass-Florl C, and the European committee on antimicrobial susceptibility testing-Subcommittee on antifungal susceptibility testing. EUCAST technical note on anidulafungin. Clin Microbiol Infect. 2011;17:E18–20. doi:10.1111/j.1469-0691.2011.03647.x. Epub 2011 Sep 16. PubMed PMID: 21923778. EUCAST anidulafungin BPs for some common Candida spp. are provided.
• Lass-Florl C, Arendrup MC, Rodriguez-Tudela J-L, and the European committee 14. on antimicrobial susceptibility testing–Subcommittee on antifungal susceptibility testing (EUCAST–AFST). EUCAST technical note on amphotericin B. Clin Microbiol Infect. 2011;17:E27–9. doi:10.1111/j.1469-0691.2011.03644.x. Epub 2011 Oct 19. PubMed PMID: 22011310. EUCAST BPs of amphotericin B for common Candida spp. are provided.
• Arendrup MC, Cuenca-Estrella M, Lass-Flörl C, Hope WW. European Committee on Antimicrobial Susceptibility Testing Subcommittee on Antifungal Susceptibility Testing (EUCAST–AFST). EUCAST technical note on Aspergillus and amphotericin B, itraconazole, and posaconazole. Clin Microbiol Infect. 2012;18(7):E248–50. doi:10.1111/j.1469-0691.2012.03890.x. Epub 2012 Apr 30. PubMed PMID: 22540149. EUCAST Breakpoints of amphotericin B, itraconazole and posaconazole for some Aspergillus spp. are provided.
•Rodriguez-Tudela JL, Alcazar-Fuoli L, Mellado E, et al. Epidemiological cutoffs and cross-resistance to azole drugs in Aspergillus fumigatus. Antimicrob Agents Chemother. 2008;52:2468–72. EUCAST ECVs for A. fumigatus and the triazoles were provided in this article for the first time. Triazole cross-resistance was associated with specific cyp51A mutations.
• Espinel-Ingroff A, Diekema DJ, Fothergill A, et al. Wild-type MIC distributions and epidemiological cutoff values for the triazoles and six Aspergillus spp. for the CLSI broth microdilution method (M38-A2). J Clin Microbiol. 2010;48:3251–57. CLSI ECVs for six Aspergillus spp. and the triazoles were provided in this article.
• Espinel-Ingroff A, Fothergill A, Fuller J, et al. Wild-Type MIC distributions and epidemiological cutoff values for caspofungin and Aspergillus spp. for the CLSI broth microdilution method (M38-A2 document). Antimicrob Agents Chemother. 2011;55:2855–59. CLSI ECVs for six Aspergillus spp. and caspofungin, which are not listed in Table 3 of our article, were provided in this article.
• Espinel-Ingroff A, Cuenca-Estrella M, Fothergill A, et al. Wild-Type MIC distributions and epidemiological cutoff values for amphotericin B and Aspergillus spp. for the CLSI broth microdilution method (M38-A2 document). Antimicrob Agents Chemother. 2011;55:5150–54. CLSI ECVs for six Aspergillus spp. and amphotericin B were provided in this article.
Meletiadis J, Mavridou E, Melchers WJG, et al. Epidemiological cutoff values for azoles and Aspergillus fumigatus based on a novel mathematical approach incorporating cyp51A sequence analysis. Antimicrob Agents Chemother. 2012;56:2224–29.
• Jeans AR, Howard SJ, Al-Nakeeb Z, et al. Pharmacodynamics of voriconazole in a dynamic in vitro model of invasive pulmonary aspergillosis: Implications for in vitro susceptibility breakpoints. J Infect Dis Advance. 2012;206(3):442–52. BPs are suggested to test voriconazole and A. fumigatus using both CLSI and EUCAST methodologies.
• Espinel-Ingroff A, Chowdhary A, Cuenca-Estrella M, et al. Cryptococcus neoformans- Cryptococcus gattii species complex: An international study of wild-type susceptibility endpoint distributions and epidemiological cutoff values for amphotericin B and flucytosine. Antimicrob Agents Chemother. 2012;56:3107–13. CLSI ECVs of amphotericin B and flucytosine were provided for this fungal group.
• Espinel-Ingroff A, Aller I, Canton E, et al. Cryptococcus neoformans-Cryptococcus gattii species complex: An international study of Wild-Type susceptibility endpoint distributions and epidemiological cutoff values for fluconazole, itraconazole, posaconazole and voriconazole. Antimicrob Agents Chemother. 2012;56:5898–906. CLSI ECVs of four triazoles were provided for this fungal group.
• Pfaller MA, Espinel-Ingroff A, Canton E, et al. Wild type MIC distributions and epidemiological cutoff values for amphotericin B, flucytosine, and itraconazole and Candida spp. as determined by CLSI broth microdilution. J Clin Microbiol. 2012;50:2040–46. CLSI ECVs of amphotericin B, flucytosine and itraconazole for Candida spp. were provided.
Pappas PG, Kauffman CA, Andes D, et al. Clinical practice guidelines for the management of candidiasis: 2009 update by the Infectious Diseases Society of America. Clin Infect Dis. 2009;48:503–35.
Perfect JR, Dismukes WE, Francoise Dromer F, et al. Clinical practice guidelines for the management of cryptococcal disease: 2010 update by the Infectious Diseases Society of America. Clin Infect Dis. 2010;50:291–22.
Walsh TJ, Anaissie EJ, Denning DW, et al. Treatment of aspergillosis: clinical practice guidelines of the Infectious Diseases Society of America. Clin Infect Dis. 2008;46:327–60.
Alastruey-Izquierdo A, Cuenca-Estrella M. EUCAST and CLSI: how to assess in vitro susceptibility and clinical resistance. Curr Fungal Infect Rep. 2012;6:229–34.
Pfaller MA, Castanheira M, Jones RN. Advances in antifungal susceptibility testing of Candida, 2010–2012. Curr Fungal Infect Rep. 2012;6:141–53.
Pfaller MA, Boyken LB, Hollis RJ, et al. Validation of 24-hour posaconazole and voriconazole MIC readings versus the CLSI 48-hour broth microdilution reference method: Application of epidemiological cutoff values to results from a global Candida Antifungal Surveillance Program. J Clin Microbiol. 2011;49:1274–79.
Espinel-Ingroff A, Barchiesi F, Cuenca-Estrella M, et al. International and multicenter comparison of EUCAST and CLSI M27-A2 broth microdilution methods for testing susceptibilities of Candida spp. to fluconazole, itraconazole, posaconazole, and voriconazole. J Clin Microbiol. 2005;43:3884–9.
Rodriguez-Tudela JL, Donnelly JP, Pfaller MA, et al. Statistical analyses of correlation between fluconazole MICs for Candida spp. assessed by standard methods set forth by the European Committee on Antimicrobial Susceptibility Testing (EDef. 7.1) and CLSI (M27-A2). J Clin Microbiol. 2007;45:109–11.
Pfaller MA, Espinel-Ingroff A, Boyken LB, et al. Comparison of the broth microdilution (BMD) method of the European committee on antimicrobial susceptibility testing with the 24-hour CLSI BMD method for testing susceptibility of Candida species to fluconazole, posaconazole, and voriconazole by use of epidemiological cutoff values. J Clin Microbiol. 2011;49:845–50.
Cuenca-Estrella M, Lee-Yang W, Ciblak MA, et al. Comparative evaluation of NCCLS M27-A and EUCAST broth microdilution procedures for antifungal susceptibility testing of Candida species. Antimicrob Agents Chemother. 2002;46:3644–7.
• Zaragoza O, Mesa-Arango AC, Gomez-Lopez A, et al. Process analysis of variables for standardization of antifungal susceptibility testing of nonfermentative yeasts. Antimicrob Agents Chemother. 2011;55:1563–70. EUCAST standard testing parameters for Cryptococcus spp. and other nonfermentative yeasts are proposed in this article.
Gomez-Lopez A, Aberkane A, Petrikkou E, et al. Analysis of the influence of tween concentration, inoculum size, assay medium, and reading time on susceptibility testing of Aspergillus spp. Antimicrob Agents Chemother. 2005;43:1251–5.
• Dalhoff A, Ambrose PG, Mouton JW. A long journey from minimum inhibitory concentration testing to clinically predictive breakpoints: deterministic and probabilistic approaches in deriving breakpoints. Infection. 2009;37:296–305. Definitions/differences between CBPs and ECVs are provided.
Garcia-Effron G, Park S, Perlin DS. Correlating echinocandin MIC and kinetic inhibition of fks1 mutant glucan synthases for Candida albicans: implications for interpretive breakpoints. Antimicrob Agents Chemother. 2009;53:112–22.
Garcia-Effron G, Lee S, Park S, et al. Effect of Candida glabrata FKS1 and FKS2 mutations on echinocandin sensitivity and kinetics of 1,3-ß-D-glucan synthase: implication for the existing susceptibility breakpoint. Antimicrob Agents Chemother. 2009;53:3690–9.
Turnidge J, Kahmeter G, Kronvall G. Statistical characterization of bacterial wild-type MIC value distributions and the determination of epidemiological cut-off values. Clin Microbiol Infect. 2006;12:418–25.
Park BJ, Arthington-Skaggs BA, Hajjeh RA, et al. Evaluation of amphotericin B interpretive breakpoints for Candida bloodstream isolates by correlation with therapeutic outcome. Antimicrob Agents Chemother. 2006;50:1287–92.
Verweij PE, Howard SJ, Melchers WJG, et al. Azole resistance in Aspergillus: proposed nomenclature and breakpoints. Drug Resist Updat. 2009;12:141–47.
Madureira A, Bergeron B, Claire Lacroixet C, et al. Breakthrough invasive aspergillosis in allogeneic hematopoietic stem cell transplant recipients treated with caspofungin. Int J Antimicrob Agents. 2007;30:551–4.
Disclosure
A. Espinel-Ingroff: grants from Astellas and MICOMOLSL, received payment for contribution to the Journal of Invasive Fungal Infections; M. Cuenca-Estrella: has received grants and payment for consultancy, expert testimony, and lectures from Astellas, Pfizer, Gilead, and MSD; E. Cantón: none
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Espinel-Ingroff, A., Cuenca-Estrella, M. & Cantón, E. EUCAST and CLSI: Working Together Towards a Harmonized Method for Antifungal Susceptibility Testing. Curr Fungal Infect Rep 7, 59–67 (2013). https://doi.org/10.1007/s12281-012-0125-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12281-012-0125-7