Abstract
The receptor for advanced glycation end products (RAGE) plays a key role in the development of vascular inflammation and acceleration of atherosclerosis in type 2 diabetes. We investigated the effect of candesartan cilexetil (CDRT) and amlodipine orotate (AMDP) on the expression of RAGE in the aortic walls of Otsuka Long-Evans Tokushima Fatty (OLETF) rats and AGE-treated endothelial cells. Twenty five-week-old OLETF rats were randomized to 8 week treatments consisting of CDRT (n = 8), AMDP (n = 8) or saline (control, n = 8). Immunohistochemical and dihydroethidine staining revealed reduced RAGE and reactive oxygen species (ROS) signals in rats treated with CDRT or AMDP compared with control rats. Both CDRT and AMDP suppressed the expression of p22phox and p47phox NADPH oxidase subunits. However, only CDRT significantly reduced expression of phosphorylated extracellular signal regulated kinase (pERK)1/2 in the aortic wall of OLETF rats. In addition, both drugs reduced RAGE expression and total and mitochondrial ROS production in the AGE-treated endothelial cells. Both ARBs and CCBs reduced RAGE expression in the aortic walls of OLETF rats, which was attributed to decreased ROS production through inhibition of NADPH oxidase. In addition, only CDRT reduced aortic expression of RAGE via suppression of the ERK1/2 pathway unlike AMDP.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diabetes is a chronic metabolic disorder characterized by chronic hyperglycemia and the development of vascular complications (Bierhaus et al. 2001; Fan et al. 2004; Farmer and Kennedy 2009; Ihm et al. 2009). Among various mechanisms explaining diabetic complications, increased formation of advanced glycation end products (AGEs) have been known to play a central role of in the pathogenesis of vascular disease (Yamagishi et al. 2008b). AGEs are reactive derivatives of nonenzymatic glucose-protein reactions, which have been associated with increased oxidative stress in vitro and in vivo studies (Miyata et al. 2002; Fan et al. 2004). The best-characterized receptor for AGE, designated as RAGE (receptor for AGE), is a polypeptide of the immunoglobulin superfamily that has recently been widely implicated as a mediator of both acute and chronic vascular inflammation in conditions such as atherosclerosis and in particular as a complication of diabetes (Fan et al. 2004; Yamagishi et al. 2008a; Farmer and Kennedy 2009; Matsui et al. 2010). Accordingly, the development of pharmacological strategies that specifically target AGE-RAGE axis, appear promising for the treatment of vascular complications in diabetes (Fan et al. 2004; Yamagishi et al. 2008b). Furthermore, oxidative stress including excessive production of reactive oxygen species (ROS) plays a key role in the pathogenesis of atherosclerosis, vascular inflammation and endothelial dysfunction related to AGE-RAGE axis (Schramm et al. 2012).
Activation of RAGEs by AGEs makes nuclear transcription factor produce proinflammatory cytokines, growth factors and RAGE via multiple signals, such as NADPH oxidase, the mitogen-activated protein kinases (MAPKs), extracellular signal–regulated kinase (ERK)1/2 and p38 (Goldin et al. 2006). And some studies demonstrated that especially RAGE-ERK1/2 pathway had an important role of diabetic complications (Li et al. 2004, 2012).
Angiotensin-II-receptor blockers (ARB) have been reported to reduce the formation of AGEs in vitro (Miyata et al. 2002) Some studies demonstrated that ARBs inhibited AGEs by suppressing RAGE expression in renal tubular cells, cultured microvascular endothelial cells in vitro (Yamagishi et al. 2008a; Matsui et al. 2010). In another study, candesartan, an ARB, reduced AGE accumulation by attenuating RAGE expression and decreasing the nicotinamide adenine dinucleotide phosphate (NADPH) oxidase in diabetic mouse kidneys (Fan et al. 2004). Several studies have shown that calcium channel blockers (CCBs) may have anti-atherogenic and antioxidant properties, independent of their effects on vasodilation (Mason 2002). Interestingly, nifedipine, a long acting dihydropyridine CCB, also inhibited RAGE expression in AGE exposed endothelial cells, mesangial cells in vitro (Matsui et al. 2009). Therefore, these observations suggest that ARBs and CCBs could play a protective role against AGE-RAGE pathway in diabetic patients.
However, most of studies related to drug effects on AGE-RAGE pathway were in vitro studies and focused on kidney in case of in vivo studies. Little is known about the effects of candesartan cilexetil (CDRT, AstraZeneca, UK; ARB) and amlodipine orotate (AMDP, Dong-A Pharmacy, Korea: CCB) on AGE-RAGE axis especially in the aortic wall of type 2 diabetic (T2D) rat model (in vivo). The purpose of this study was to investigate the effect of CDRT and AMDP on RAGE expression using Otsuka Long-Evans Tokushima Fatty (OLETF) rats as a T2D model (in vivo) and human coronary artery endothelial cells (HCAECs; in vitro), focusing on production of ROS and NADPH oxidase expression.
Materials and methods
This study was in accordance with the Guide for the Care and Use of Laboratory Animals published by the US National Institutes of Health (NIH Publication No. 85-23, revised 1996) and was approved by the Institutional Animal Care and Utilization Committee of the Department of Internal Medicine (CUMC-2009-0089-01), Catholic University of Korea, Seoul, Republic of Korea.
In vivo studies of OLETF rats
Twenty-four male OLETF rats were used as models for type 2 diabetes. The Tokushima Research Institute, of Otsuka Pharmaceuticals (Otsuka Pharmaceutical, Tokushima, Japan), kindly provided all of the OLETF rats. The starting age of OLETF rats was 6 weeks of age. All rats were caged individually and received normal rat chow and tap water in a temperature-controlled environment under a 12-h artificial light and dark cycle. A total 24 OLETF rats at 25 weeks of age were randomized into three equal groups consisting of daily treatment by gastric gavage orally with CDRT (3 mg/kg, n = 8), AMDP (3 mg/kg, n = 8) or saline (n = 8) for 8 weeks.
Measurement of body weight, blood pressure, plasma glucose
In all 25-week-old rats, body weight, blood pressure, and heart rate were determined by tail-cuff plethysmography (BP-2000, Visitech system, Apex, NC, USA) after a 12-h fasting period at rest immediately prior to drug administration. Body weight, blood pressure, and heart rate were measured again every 4 weeks thereafter for 8 weeks. At 33 weeks, intraperitoneal glucose tolerance test (IP-GTT) was performed at approximately 8 a.m. after a 12-h fasting period. Briefly, an intraperitoneal injection of a 25 % glucose solution at a dose of 2 g/kg was administered. During fasting states, serum glucose levels were measured using a Beckman Glucose Analyzer (Beckman Instrument Co., Palo Alto, CA, USA).
Reverse transcription-polymerase chain reaction (RT-PCR) for RAGE
Total RNA was extracted from each aortic wall using TRIZOL reagent (Invitrogen Crop., Carlsbad, CA, USA) according to the manufacturer’s instructions. Total RNA was subjected to reverse transcription using the one step RT kit (Invitrogen Crop., Carlsbad, CA, USA). Expression of RAGE and glyceraldehyde 3-phosphate dehydrogenase (GAPDH) was evaluated by real-time PCR using SYBR Green dye. The primers used in this study were as follows: rat RAGE (sense, 50-GAATCCTCCCCAATGGT TCA-30 and antisense 50-CCCGACACCGGAAAGT-30) and rat GAPDH (sense, 50-GTATGACTCTACCCACGGC AAGT and antisense, 50-TTCCCGTTGATGACCAGCTT-30). Results were expressed as relative messenger RNA (mRNA) content, which was normalized for GAPDH expression as determined by real-time PCR.
Immunohistochemical analysis for NADPH oxidases and RAGE
Sections (5 μm) of thoracic aortas were cut from 4 % paraformaldehyde-fixed, paraffin embedded tissue blocks and mounted on poly-lysine coated slides. Antigens were retrieved by heating the sections in a 10 mM citrate buffer (60 °C oven overnight). The cooled sections were then incubated with 3 % H2O2 for 10 min to block endogenous peroxidases. For p22phox immunostaining, the primary antibody consisted of the anti-p22phox rabbit polyclonal antibody (Santa Cruz Biotechnology, Dallas, TX, USA) used at a 1:50 dilution. The secondary antibody was coupled to alexafluor 488 (Invitrogen Crop., Carlsbad, CA, USA) and was used at a 1:2000 dilution. For p47phox immunostaining, sections were incubated at 4 °C overnight with a rabbit polyclonal anti-p47phox antibody (Santa Cruz Biotechnology, Dallas, TX, USA) at a 1:50 dilution in 0.5 M TBST. The secondary antibody was coupled to alexafluor 555 (Invitrogen Crop., Carlsbad, CA, USA) used at a 1:2000 dilution. For RAGE immunostaining, the primary antibody consisted of the anti-RAGE rabbit polyclonal antibody (Santa Cruz Biotechnology, Dallas, TX, USA), used at a 1:50 dilution. The secondary antibody in this case was coupled to alexafluor 594 (Invitrogen Crop., Carlsbad, CA, USA) used at a 1:2000 dilution. Nuclear counterstaining was performed with DAPI at a 1:10,000 dilution. Sections were kept in the dark until fluorescence was analyzed by inverted fluorescence microscope (Zeiss, Jena, Germany).
Determination of vascular ROS formation in the aortic walls
The oxidative fluorescent dye dihydroethidine (DHE, Sigma-Aldrich, Milwaukee, WI, USA) was used to evaluate the in situ formation of ROS as previously detailed (Miller et al. 1998; Ihm et al. 2009). Thoracic aortas from OLETF were embedded in OCT compound (Tissue-Tek, Sakura Finetek, Torrance, CA, USA) and frozen in a liquid nitrogen bath prior to development of cryostat sections. Unfixed frozen aortic rings were cut into Sects. 5 μm thin and dihydroethidine (2.5 μM) was applied to all tissue sections, which were then incubated in a light-protected humidified chamber for 30 min at 37 °C. The sections were next examined using a confocal microscope (LSM 510 META Carl Zeiss Inc., Overkochen, Germany) with a 20 × epifluorescence objective. After excitation at 543 nm, the emission signal was recorded with a Zeiss 560–615 nm filter. Mean intensities were expressed as arbitrary densitometry units.
Western blotting
Frozen aortic tissue of rats were lysed in radioimmunoprecipitation assay (RIPA) buffer [0.1 % SDS, 1 % deoxycholate, 1 % Triton X-100, 150 mM NaCl, 5 mM EDTA, 10 mM Tris pH 7.4, and 10 % protease inhibitor cocktail (Sigma–Aldrich, Milwaukee, WI, USA)] for 30 min at 4 °C followed by centrifugation at 13,000 rpm at 4 °C for 30 min. The resulting supernatant fluid was collected and the protein content was quantified using Bio-Rad Protein assay reagent (Bio-Rad, Regents Park, NSW, Australia). Aortic tissue lysates were resolved on SDS–polyacrylamide gel electrophoresis according to standard protocols. After being transferred to membranes, the samples were immunoblotted with primary antibodies, followed by secondary antibodies conjugated with horseradish peroxidase. Bands were revealed by the use of an enzyme-linked chemiluminescence detection kit (Amersham Biosciences, Piscataway, NJ, USA). Western blotting was performed on aortic tissues to identify phosphorylated ERK1/2 and ERK1/2. Western blotting was also performed on cultured HCAECs to identify RAGE, p-ERK1/2 and ERK1/2.
In vitro studies
Advanced glycation end product-modified bovine serum albumin (AGE-BSA) was purchased from BioVision (Milpitas, CA, USA). HCAECs were purchased from Cambrex Bioscience (Walkersville, MD, USA). Cells were used between passages 4 to 5 for experiments to avoid the effects of in vitro cell aging. Cells were grown in endothelial growth media-2 (EGM-2; Cambrex Bioscience, Walkersville, MD, USA) supplemented with growth factors and 5 % (v/v) fetal bovine serum (FBS) to 70–80 % confluency. Cells were cultured in a humidified incubator at 37 °C in a 5 % CO2 atmosphere, and the culture medium was changed every other day. Before the experiments, HCAECs were cultured in low serum medium (0.1 % FBS) for 24 h and incubated with 100 µg/ml AGE-BSA or non-glycated BSA in the presence or absence of CDRT or AMDP at 100 nM, 1 µM, and 10 µM for 24 h, followed by determination of expression of RAGE, relative total ROS, mitochondrial ROS and phosphorylated & total ERK 1/2.
Mitochondrial ROS
Production of ROS was measured using the oxidation-sensitive fluorescence probe 2′,7′-dichlorodihydrofluorescin diacetate (H2DFF-DA, Molecular probes). HCAECs were seeded into 96-well plates and incubated for 24 h at 37 °C. Cell cultures were preincubated with 10 μl DFFH-DA for 30 min at 37 °C. The fluorescence of DCFs was measured using a microplate reader at an excitation wavelength of 485 nm and emission wavelength of 530 nm.
The production of Mitochondrial ROS was measured using MitoSOX (Molecular probes). Briefly, HCAECs were seeded into each well of a 6-well plate and incubated for 24 h at 37 °C. After treatment, cells were preincubated with 5 μl MitoSOX for 10 min at 37 °C. After removal of excess stains, cells were imaged by fluorescence microscopy (Zeiss, Jena, Germany).
Statistical analysis
Statistical analysis was performed using the Statistical Package for the Social Sciences (SPSS) software version 15.0 (SPSS Inc., Chicago, IL, USA). All values were reported as the mean ± SEM. Differences in measured values among multiple groups were analyzed by ANOVA with Bonferroni correction for multiple comparisons. For all statistical analyses, p values less than 0.05 were considered statistically significant.
Results
Both CDRT and AMDP lower blood pressure in the OLETF rats
There was no difference in body weight between 25 and 33 weeks of age in control and treatment groups. However, while systolic BP was similar in both groups at 25 weeks of age, which represented the beginning of treatment, systolic BP was significantly lower at 33 weeks of age in the treatment group, whereas no such decrease was observed in the control group. Likewise, plasma fasting glucose levels were similar among the three groups at 33 weeks of age. CDRT-treated group exhibited lower plasma fasting glucose and postprandial 30-min and 1 h glucose levels compared with the control group. AMDP-treated group showed lower only 30-min glucose levels compared with the control group. However, there was no significant difference in any glucose levels between CDRT and AMDP groups (Table 1).
Both CDRT and AMDP decrease RAGE expression in the HCAECs and aortic walls of the OLETF rats
In HCAECs, AGE stimulated endothelial RAGE protein expression. The endothelial expression of RAGE decreased as the dose of study drugs was titrated from 100 nM to 10 μM in the AGE-stimulated HCAECs with AMDP and CDRT compared with the AGE-stimulated HCAECs without drug (Fig. 1a). To compare RAGE expression in the aortic wall of OLETF rats, expression at both the protein levels and mRNA was examined. Suppression of RAGE expression in the media was observed in CDRT & AMDP groups compared with the control group as determined by immunohistochemical staining (Fig. 1b). Thus, compared with the control group, mRNA levels of RAGE were significantly lower in the CDRT and AMDP groups, while the AMDP group exhibited a significant decrease of RAGE mRNA compared with the CDRT group (Fig. 1c).
The levels of RAGE expression in the HCAECs and aortic walls of OLETF rats. a RAGE expression decreased as the dose was escalated in CDRT or AMDP treated group in HCAECs. Upper panel showed the RAGE expression according to AGE and CDRT or AMDP, lower panel showed relative RAGE expression ratio. Results are shown as mean ± SD. (n = 5) *p < 0.05 versus AGE (+) & CDRT (−) or AMDP (−). b The aortic RAGE expression decreased significantly in the CDRT or AMDP treated group compared to the control group. Upper panel showed Immunohistochemical stain for RAGE protein expression, lower panel showed analysis of relative intensity in IHC stain of OLETF rats. (n = 8 different rats) *p < 0.05 versus control. c RT PCR for RAGE m-RNA expression in the aortic wall of OLETF rats. (n = 8 different rats) *p < 0.05 versus control
Both CDRT and AMDP decrease total and mitochondrial ROSs in HCAECs and prevent excessive vascular formation of ROS by inhibiting NADPH oxidase activity in the OLETF rats
In HCAECs, AGE increased ROS production. However, in vitro analysis of HCAECs treated CDRT & AMDP groups revealed a reduced abundance of ROS production compared with the AGE_BSA group (Fig. 2a). Specifically, immunofluorescence staining of mitochondrial ROS production revealed reduced fluorescence in the CDRT & AMDP groups (Fig. 2b). Furthermore, we performed in vivo studies to evaluate whether the effect of CDRT and AMDP in OLETF rats is associated with a reduced vascular pro-oxidant response as assessed using the redox-sensitive fluorescent probe dihydroethidine (DHE). In the control group, a marked fluorescence signal throughout the entire aortic wall was observed, whereas intake of CDRT and AMDP significantly reduced the fluorescent signal in OLETF groups (Fig. 3). In addition, low fluorescent signals for p22phox and p47phox (green fluorescence) were detected throughout the aortic wall in the CDRT & AMDP group compared with the control group (Fig. 4a, b).
Total and mitochondrial ROS expressions in the HCAECs. a Total ROS in HCAECs. HCAECs were incubated with 100 μg/ml non-glycated BSA (control), H2O2 or 100 μg/ml AGE-BSA. And HCAECs were incubated with 100 μg/ml AGE-BSA in the presence or absence of CDRT or AMDP at 100 nM (+), 1 μM (++), and 10 μM (+++). All doses of CDRT and AMDP treated group showed significantly reduced total ROS compared to AGE-BSA group. (n = 5). *p < 0.05 versus AGE-BSA group. b Mitochondrial ROS in HCAECs, upper panel showed control group (incubated with 100 μg/ml AGE-BSA), middle panel showed CRDT treated group (100 nM, coincubated with 100 μg/ml AGE-BSA), lower panel AMDP group (100 nM, coincubated with 100 μg/ml AGE-BSA). Immunofluorescence stain of mitochondrial ROS production showed reduced fluorescence signal in CDRT or AMDP treated group compared to control group
The vascular formation of reactive oxygen species in the aorta of OLEFT rats. Upper panel showed the oxidative fluorescent dye dihydroethidine (DHE) staining, lower panel showed analysis of relative intensity in DHE stain in the OLETF rats. A marked fluorescence signal throughout the entire aortic wall was observed, whereas only a slight signal was observed in CDRT or AMDP treated groups. DHE intensity graph showed that both drugs significantly reduced the DHE intensity. (n = 8 different rats) *p < 0.05 versus control
NADPH oxidase expression in the aorta of OLEFT rats. Expression of NADPH oxidase subunit (p22phox or p47phox) using a purified polyclonal antibody and a fluorescence-tagged secondary antibody by confocal microscopy in the aortic wall of OLETF rats. Left, middle and right figures represent p22phox or p47phox immunoreactivity (red), cell nuclei (blue) and merged images, respectively. Upper panels show Immunofluorescence labeling of p22phox or p47phox in control group, middle panels in CDRT-treated group, lower panels in AMDP-treated group, middle and lower panels show decreased immunofluorescence labeling of p22phox or p47phox rather than control group. a p22phox, b p47phox
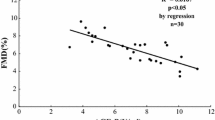
Only CDRT significantly reduce expression of pERK1/2 in the HCAECs and aortic walls of OLETF rats
To determine whether ERK1/2 signaling pathway was activated or suppressed by CDRT or AMDP, the extent of ERK1/2 phosphorylation was measured by Western blot. In HCAEC, AGE stimulated endothelial pERK1/2 protein expression. The endothelial expression of pERK 1/2 significantly decreased as the dose of CDRT was titrated 100 nM in the AGE-stimulated HCAECs compared with the AGE-stimulated HCAECs without drug. However, the endothelial expression of pERK 1/2 did not significantly decrease as the dose of AMDP was titrated 100 nM in the AGE-stimulated HCAECs compared with the AGE-stimulated HCAECs without drug (Fig. 5a). Treatment with CDRT suppressed enhancement of ERK 1/2 phosphorylation while pERK 1/2 expression was not significantly decreased in the AMDP group compared with the control group in the aortic walls of the OLETF rats (Fig. 5b). Both CDRT and AMDP decrease RAGE expression in the aortic walls of the OLETF rats.
Phosphorylated ERK 1/2 (pERK 1/2) expression in the AGE stimulated HCAECs and aortic walls of diabetic rats. The pERK 1/2 expression measured by Western blotting was significantly lower in the CDRT group compared with the control group in vitro, whereas there was no significant change between the control and AMDP group (a). Activation of ERK 1/2 in isolated aortic ring from control, CDRT- and AMDP treated OLETF rats. Upper panel showed representative immunoblots of pERK 1/2 and total ERK 1/2 proteins. Lower panel showed densinometric analysis of ERK 1/2 phosphorylation. Data are expressed the phosphorylated: total ERK 1/2 protein ratios. Results are shown as mean ± SD of 8 different rats. *p < 0.05 versus control group (b)
Discussion
In the present study, we demonstrated for the first time the ability of CDRT and AMDP to inhibit the expression of RAGE in the aortic walls of OLETF rats in vivo and AGE-stimulated HCAECs in vitro simultaneously. We assessed the effects of CDRT and AMDP on markers for RAGE in OLETF rats (a model for T2D) and AGE treated HCAECs (endothelial cell). We showed that both CDRT and AMDP significantly downregulate the markers for RAGE (total and mitochondrial ROS and NADPH oxidase subunits (p22phox & p47phox)) in the aortic wall of the OLETF rats as well as in AGE-treated endothelial cells. Moreover we demonstrated that the downregulation was associated with a decrease in phospho-ERK1/2. However only CDRT was found to significantly suppress phosphorylation of ERK1/2 in contrast to AMDP.
The OLETF rat is a distinct model of T2D and has several unique characteristics such as late onset of hyperglycemia, hyperinsulinemia, and obesity (Ihm et al. 2009, 2010). Considering the fact that diabetes is a major public health issue due to its increasing prevalence and the severity of its secondary vascular complications, OLETF rats are regarded as an important animal model in the understanding of human T2D (Ihm et al. 2009, 2010). Especially we chose 25 week old OLEFT rats, because that age of OLETF rats have overt diabetes with obesity and hypertension. We recently showed that RAGE proteins are expressed at significantly higher levels in endothelial cells of OLETF rats compared with a nondiabetic control animal model (Ihm et al. 2010). Likewise, in the present study, we demonstrated increased RAGE expression in the aortic wall of untreated OLETF rats, and decreased expression of RAGE at both the mRNA and protein level in CDRT and AMDP treated OLETF rats.
HCAECs are the preferred model for studies related to coronary atherosclerotic disease in humans because of differences in production of angiotensin-converting enzymes and response to cytokine stimulation compared to veins (Miller et al. 2001; Goldin et al. 2006; Morita et al. 2013). Indeed, previous studies have demonstrated that AGEs stimulate ROS production in human aortic wall endothelial cells (HAoEC) (Morita et al. 2013). Similarly, Yamagishi and Takeuchi (2004) reported that nifedipine downregulates RAGE mRNA expression in AGE-induced human umbilical vein endothelial cells (HUVECs) in vitro. However, it is not yet to be demonstrated the AGE-RAGE interactions and subsequent responses to therapeutic intervention in the human coronary artery endothelial cells. In the present study, treatment of HCAECs with AGE increased RAGE expression which was decreased after treatment with either CDRT or AMDP.
AGEs contribute to the progression of a variety of vascular diabetic complications via increased ROS production (Goldin et al. 2006; Barlovic et al. 2011; Yamagishi et al. 2012; Morita et al. 2013). Specifically, AGEs are capable of activating multiple signal transduction pathways through AGE-RAGE axis, including NADPH oxidase and mitogenic pathways involving protein kinase ERK1/2 (Li et al. 2004; Coughlan et al. 2009; Li et al. 2012; Morita et al. 2013). AGE-RAGE interaction can increase the activity of NADPH oxidase and evoke the generation of oxidative stress in numerous cell types (Yamagishi et al. 2008b; Barlovic et al. 2011; Yamagishi et al. 2012). In addition, the AGE-RAGE interaction paradigm in endothelial cells has been reported to stimulate the mitochondrial electron transport system (Bierhaus et al. 2001; Coughlan et al. 2009; Barlovic et al. 2011; Morita et al. 2013). Thus, overproduction of ROS by NADPH oxidases induces mitochondrial oxidative damage and disturbs the electron transport chain, resulting in enhanced ROS production (Nakamura et al. 2005; Ray and Shah 2005; Yamagishi et al. 2008a; Matsui et al. 2009, 2010; Schramm et al. 2012). Binding of AGEs to RAGE can also trigger activation of NF-κB through stimulation of NADPH oxidase and ERK1/2 MAP kinase pathways in various type of cells (Li et al. 2004; Yamagishi et al. 2008b; Barlovic et al. 2011). Interestingly, AGE-RAGE interactions have been reported to cause a positive feed-forward loop, in which inflammatory stimuli activates NF-κB, which in turn induces RAGE expression and reinforces NF-κB activation (Bierhaus et al. 2001; Li et al. 2004; Barlovic et al. 2011). In present study, we showed that CDRT and AMDP decrease ROS and NADPH oxidase expression in aortic walls of OLETF rats. In addition, both drugs reduce both total and mitochondrial ROS production in AGE treated HCAECs simultaneously. These findings have been reported in previous studies indicating that RAGE expression and ROS generation can be suppressed by treatment with ARBs in human renal tubular epithelial cells, human adult skin microvascular endothelial cells, and human mesangial cells in vitro (Miyata et al. 2002; Nakamura et al. 2005; Yamagishi et al. 2008a; Matsui et al. 2010). Likewise, AMDP has been demonstrated to decrease NADPH oxidase expression in intramyocardial arteries by restoring copper/zinc containing superoxide dismutase (Cu/Zn SOD) expression in stroke-prone spontaneously hypertensive rats (SPSHR) model in vivo (Umemoto et al. 2004).
AGE-RAGE interactions are capable of activating the ERK1/2 MAP kinase pathway (Li et al. 2004). As such, it is important to note that ERK1/2 activation induces altered vascular function, which in turn accelerates the progression of atherosclerosis in diabetic human patients as well as animal models (Brownlee 2001; Ihm et al. 2009; Li et al. 2012). Similarly, AGEs can upregulate key components of the renin-angiotensin system (RAS) in the vasculature, which can be inhibited by specific inhibitors (Yamagishi et al. 2008b; Barlovic et al. 2011). Likewise, recent studies have shown that ARB suppresses ERK-1 protein expression in a spontaneously hypertensive rat (SHR) model (Wang et al. 2004). The results of the present study revealed that pERK1/2 expression can be altered by the presence of AGEs in the HCAECs, and that CDRTs, unlike AMDPs, can significantly reduce the function of pERK1/2 in the aortic wall of OLETF rats. Therefore, while AGE-RAGE interactions may induce up-regulation of the ERK1/2 pathway, this effect can be significantly blocked only by CDRTs, but not AMDPs.
Both drugs lowered post-prandial 30 min blood glucose levels and CDRT lowered fasting and postprandial 1 h blood glucose levels. There are reciprocal relationships between endothelial dysfunction and insulin resistance (Kim et al. 2006). Therefore the improvements in endothelial dysfunction would be accompanied by simultaneous improvement in metabolic parameters. In general, ACE inhibitors, ARBs and CCBs improve endothelial dysfunction (Koh et al. 2010). Furthermore CDRT have direct effects to augment insulin-stimulated glucose uptake and induce peroxisome proliferator-activated receptor (PPAR)-γ activity (Sharma et al. 2002; Schupp et al. 2004). Therefore we suggested that CDRT may affect glucose metabolism by improving insulin resistance and PPAR-r activity. On the other hand, AMDP does not improve insulin sensitivity in some studies, but AMDP improves insulin resistance and adiponectin levels in other studies (Koh et al. 2010). So we concluded here that AMDP may have a minor effect on glucose metabolism by those mechanisms.
The strength of our study was the parallel experimental approach to address our goal using a rat model of type 2 diabetes (in vivo) and human coronary endothelial cells (in vitro). However there are some limitations to the present study. First, although CDRT reduced RAGE expression through its known anti-atherogenic properties, the relationship among NADPH oxidase, ERK1/2 pathway-related proteins, and NF-κB remains unclear. For this reason, we did not provide an exact mechanism of how CDRT exerts its anti-atherogenic properties in either HCAECs or in aortic walls of OLETF rats. We suggest that CDRT may suppress NF-κB by down-regulating expression of ERK1/2 pathway, NADPH oxidase and subsequently modulating oxidative stress to attenuate the expression of RAGE. Therefore further studies including in vitro will be needed for evaluation of exact mechanism. Second, we did not measure plasma insulin and other lipid levels, because we focused on the effects of antihypertensive drugs on RAGE and oxidative stress. In general, ACE inhibitors, ARBs and CCBs improve endothelial dysfunction and insulin resistance. Therefor we inferred that CDRT and AMDP could affect insulin and lipid metabolism.
In conclusion, CDRT may reduce aortic expression of RAGE via suppression of aortic wall oxidative stress and the ERK1/2 signaling pathway. Likewise, AMDP may reduce aortic RAGE via suppression of aortic wall oxidative stress, but not the ERK1/2 pathway. Together, these results suggest that both CDRT and AMDP may have anti-atherosclerotic effects relevant to diabetes through different pathways.
References
Barlovic DP, Soro-Paavonen A, Jandeleit-Dahm KA (2011) RAGE biology, atherosclerosis and diabetes. Clin Sci (Lond) 121:43–55
Bierhaus A, Schiekofer S, Schwaninger M, Andrassy M, Humpert PM, Chen J, Hong M, Luther T, Henle T, Kloting I, Morcos M, Hofmann M, Tritschler H, Weigle B, Kasper M, Smith M, Perry G, Schmidt AM, Stern DM, Haring HU, Schleicher E, Nawroth PP (2001) Diabetes-associated sustained activation of the transcription factor nuclear factor-kappaB. Diabetes 50:2792–2808
Brownlee M (2001) Biochemistry and molecular cell biology of diabetic complications. Nature 414:813–820
Coughlan MT, Thorburn DR, Penfold SA, Laskowski A, Harcourt BE, Sourris KC, Tan AL, Fukami K, Thallas-Bonke V, Nawroth PP, Brownlee M, Bierhaus A, Cooper ME, Forbes JM (2009) RAGE-induced cytosolic ROS promote mitochondrial superoxide generation in diabetes. J Am Soc Nephrol 20:742–752
Fan Q, Liao J, Kobayashi M, Yamashita M, Gu L, Gohda T, Suzuki Y, Wang LN, Horikoshi S, Tomino Y (2004) Candesartan reduced advanced glycation end-products accumulation and diminished nitro-oxidative stress in type 2 diabetic KK/Ta mice. Nephrol Dial Transplant 19:3012–3020
Farmer DG, Kennedy S (2009) RAGE, vascular tone and vascular disease. Pharmacol Ther 124:185–194
Goldin A, Beckman JA, Schmidt AM, Creager MA (2006) Advanced glycation end products: sparking the development of diabetic vascular injury. Circulation 114:597–605
Ihm SH, Lee JO, Kim SJ, Seung KB, Schini-Kerth VB, Chang K, Oak MH (2009) Catechin prevents endothelial dysfunction in the prediabetic stage of OLETF rats by reducing vascular NADPH oxidase activity and expression. Atherosclerosis 206:47–53
Ihm SH, Chang K, Kim HY, Baek SH, Youn HJ, Seung KB, Kim JH (2010) Peroxisome proliferator-activated receptor-gamma activation attenuates cardiac fibrosis in type 2 diabetic rats: the effect of rosiglitazone on myocardial expression of receptor for advanced glycation end products and of connective tissue growth factor. Basic Res Cardiol 105:399–407
Kim J-A, Montagnani M, Koh K, Quon M (2006) Reciprocal relationships between insulin resistance and endothelial dysfunction: molecular and pathophysiological mechanisms. Circulation 113:1888–1904
Koh K, Quon M, Han S, Lee Y, Kim S, Koh Y, Shin E (2010) Distinct vascular and metabolic effects of different classes of anti-hypertensive drugs. Int J Cardiol 140:73–81
Li JH, Wang W, Huang XR, Oldfield M, Schmidt AM, Cooper ME, Lan HY (2004) Advanced glycation end products induce tubular epithelial-myofibroblast transition through the RAGE-ERK1/2 MAP kinase signaling pathway. Am J Pathol 164:1389–1397
Li Y, Liu S, Zhang Z, Xu Q, Xie F, Wang J, Ping S, Li C, Wang Z, Zhang M, Huang J, Chen D, Hu L, Li C (2012) RAGE mediates accelerated diabetic vein graft atherosclerosis induced by combined mechanical stress and AGEs via synergistic ERK activation. PLoS ONE 7:e35016
Mason RP (2002) Mechanisms of plaque stabilization for the dihydropyridine calcium channel blocker amlodipine: review of the evidence. Atherosclerosis 165:191–199
Matsui T, Yamagishi S, Takeuchi M, Ueda S, Fukami K, Okuda S (2009) Nifedipine, a calcium channel blocker, inhibits advanced glycation end product (AGE)-elicited mesangial cell damage by suppressing AGE receptor (RAGE) expression via peroxisome proliferator-activated receptor-gamma activation. Biochem Biophys Res Commun 385:269–272
Matsui T, Yamagishi S, Takeuchi M, Ueda S, Fukami K, Okuda S (2010) Irbesartan inhibits advanced glycation end product (AGE)-induced proximal tubular cell injury in vitro by suppressing receptor for AGEs (RAGE) expression. Pharmacol Res 61:34–39
Miller FJ Jr, Gutterman DD, Rios CD, Heistad DD, Davidson BL (1998) Superoxide production in vascular smooth muscle contributes to oxidative stress and impaired relaxation in atherosclerosis. Circ Res 82:1298–1305
Miller S, Walker SW, Arthur JR, Nicol F, Pickard K, Lewin MH, Howie AF, Beckett GJ (2001) Selenite protects human endothelial cells from oxidative damage and induces thioredoxin reductase. Clin Sci (Lond) 100:543–550
Miyata T, De Strihou CVY, Ueda Y, Ichimori K, Inagi R, Onogi H, Ishikawa N, Nangaku M, Kurokawa K (2002) Angiotensin II receptor antagonists and angiotensin-converting enzyme inhibitors lower in vitro the formation of advanced glycation end products: biochemical mechanisms. J Am Soc Nephrol 13:2478–2487
Morita M, Yano S, Yamaguchi T, Sugimoto T (2013) Advanced glycation end products-induced reactive oxygen species generation is partly through NF-kappa B activation in human aortic endothelial cells. J Diabetes Complications 27:11–15
Nakamura K, Yamagishi S, Nakamura Y, Takenaka K, Matsui T, Jinnouchi Y, Imaizumi T (2005) Telmisartan inhibits expression of a receptor for advanced glycation end products (RAGE) in angiotensin-II-exposed endothelial cells and decreases serum levels of soluble RAGE in patients with essential hypertension. Microvasc Res 70:137–141
Ray R, Shah AM (2005) NADPH oxidase and endothelial cell function. Clin Sci (Lond) 109:217–226
Schramm A, Matusik P, Osmenda G, Guzik TJ (2012) Targeting NADPH oxidases in vascular pharmacology. Vascul Pharmacol 56:216–231
Schupp M, Janke J, Clasen R, Unger T, Kintscher U (2004) Angiotensin type 1 receptor blockers induce peroxisome proliferator-activated receptor-gamma activity. Circulation 109:2054–2057
Sharma A, Janke J, Gorzelniak K, Engeli S, Luft F (2002) Angiotensin blockade prevents type 2 diabetes by formation of fat cells. Hypertension 40:609–611
Umemoto S, Tanaka M, Kawahara S, Kubo M, Umeji K, Hashimoto R, Matsuzaki M (2004) Calcium antagonist reduces oxidative stress by upregulating Cu/Zn superoxide dismutase in stroke-prone spontaneously hypertensive rats. Hypertens Res 27:877–885
Wang JM, Wang Y, Zhu ZS, Zhang MC, Zou Y, Li JJ, Li MJ, Jiang XJ, Li XY (2004) Diverse effects of long-term treatment with imidapril and irbesartan on cell growth signal, apoptosis and collagen type I expression in the left ventricle of spontaneously hypertensive rats. Life Sci 75:407–420
Yamagishi S, Takeuchi M (2004) Nifedipine inhibits gene expression of receptor for advanced glycation end products (RAGE) in endothelial cells by suppressing reactive oxygen species generation. Drugs Exp Clin Res 30:169–175
Yamagishi S, Matsui T, Nakamura K, Inoue H, Takeuchi M, Ueda S, Fukami K, Okuda S, Imaizumi T (2008a) Olmesartan blocks advanced glycation end products (AGEs)-induced angiogenesis in vitro by suppressing receptor for AGEs (RAGE) expression. Microvasc Res 75:130–134
Yamagishi S, Nakamura K, Matsui T, Ueda S, Fukami K, Okuda S (2008b) Agents that block advanced glycation end product (AGE)-RAGE (receptor for AGEs)-oxidative stress system: a novel therapeutic strategy for diabetic vascular complications. Expert Opin Investig Drugs 17:983–996
Yamagishi S, Maeda S, Matsui T, Ueda S, Fukami K, Okuda S (2012) Role of advanced glycation end products (AGEs) and oxidative stress in vascular complications in diabetes. Biochim Biophys Acta 1820:663–671
Acknowledgments
This work supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Science, ICT & Future Planning (No. NRF-2014R1A1A2058230).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors have no conflicts of interest to disclose.
Rights and permissions
About this article
Cite this article
Kang, MK., Chung, WB., Hong, SK. et al. Effects of candesartan cilexetil and amlodipine orotate on receptor for advanced glycation end products expression in the aortic wall of Otsuka Long-Evans Tokushima Fatty (OETFF) type 2 diabetic rats. Arch. Pharm. Res. 39, 565–576 (2016). https://doi.org/10.1007/s12272-016-0728-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12272-016-0728-6