Abstract
We developed models of pulmonary artery (PA) size in Fontan patients as a function of age and body surface area (BSA) using linear regression and breakpoint analyses based on data from 43 Fontan patients divided into two groups: the extracardiac conduit (ECC) group (n = 24) and the non-ECC group (n = 19). Model predictions were compared against those of a non-Fontan control group (n = 18) and published literature. We observed strong positive correlations of the mean PA diameter with BSA (r = 0.9, p < 0.05) and age (r = 0.88, p < 0.05) in the ECC group. The absolute percentage differences between our BSA and age model predictions against published literature were less than 16% and 20%, respectively. Predicted PA size for Fontan patients was consistently smaller than the control group. These models may serve as useful references for clinicians and be utilized to construct 3D anatomic models that correspond to patient body size or age.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Univentricular physiology represents one of the most severe forms of congenital heart disease; patients typically undergo staged surgical palliations ultimately culminating in the Fontan procedure. Exercise intolerance is one of many long-term sequelae associated with the Fontan circulation and several studies have investigated Fontan hemodynamics using patient-specific computational fluid dynamic models (CFD). These studies have indicated that the size and geometry of the Fontan surgical junction and pulmonary arteries (PA) have a significant impact on the patient’s cardiovascular performance [1,2,3,4,5,6,7,8]. 3D patient imaging data is typically used to develop patient-specific geometry for use in CFD simulations. However, the standard-of-care in most clinical centres involves angiographic imaging only immediately before and, in some centres, shortly after the Fontan procedure [9, 10]. It is difficult to construct patient-specific anatomic models for simulating Fontan hemodynamics at time points where no imaging data is available. Models that can predict PA size as a function of age and body surface area (BSA) would allow investigators to scale 3D geometries obtained from standard-of-care patient imaging data to other time points of interest. These anatomically realistic scaled up geometries could then be used to simulate Fontan hemodynamics without the need for additional imaging. Currently, no model has yet been published that describes the evolution of PA size in Fontan patients with the increases of body size and age from childhood to adulthood.
Furthermore, previous attempts to characterize PA size in Fontan patients and contrast them against healthy individuals reach no consensus, having found evidence of no growth [10], impaired growth [11], growth not in proportion to the BSA [9, 12], and normal growth [13, 14].
To help address these gaps, the objectives of our study are as follows:
-
To construct two regression models for PA size as a function of age and BSA and validate the predictions of these models against reported data of PA size in Fontan patients.
-
To compare the predictions of our regression models against the PA size of a non-Fontan control group.
Methods
Study Cohort
The Human Research Ethics Committee of the Royal Children’s Hospital Melbourne approved the retrospective use of data for this study (Ref. No: 37205A). All Fontan patients who underwent cardiac MRI scans between 2003 and 2017 at the Royal Children’s Hospital, Melbourne, Australia were considered for this study. Patients had undergone standard clinical management of univentricular circulation and hence are representative of the general population of this cohort. The surgical course would have included patients with varying sources and amounts of pulmonary blood flow prior to Fontan completion. Patients with documented PA stenosis or hypoplasia, patients manifesting symptoms of a failing Fontan physiology at the time of the MRI scan, those with significant developmental deficits/complications that could impair PA or somatic growth, and patients for whom the imaging data quality was poor were excluded. Of the 54 measurements of patients that satisfied the inclusion criteria, left PA measurements were available in 49 cases, right PA measurements in 48 cases, and measurements for both left and right PA in 43 cases. In some patients, more than one measurement had been made at different points in time. Measurements at two different time points were available for seven patients, measurements at three different time points were available in one case, and one measurement was available in all other patients. Patients were divided into two groups, one consisting of patients with the extracardiac conduit variant of the Fontan procedure (ECC group) (n = 24, age range = 5.1–28.6 years), while the other (non-ECC group) (n = 19, age range 17.7–40.2 years) comprised patients who had undergone atrio-pulmonary, atrio-pulmonary Fontan-Bjork, and lateral tunnel Fontan procedures. We divided the cohort into the two previously mentioned groups as the numbers of observations for the sub-groups of atrio-pulmonary, atrio-pulmonary Fontan-Bjork, and lateral tunnel Fontan were too small to construct models for each sub-group. In addition, as the ECC variant of the Fontan procedure is currently predominant, models developed for this group of patients will be widely applicable to future studies involving Fontan patients.
The detailed history and diagnoses of each patient are specified in the Supplementary Material (Table S1).
Data from the Fontan patients were compared with data from a control group, consisting of n = 18 images from patients with repaired aortic coarctation and apparently normal pulmonary arteries and presumed normal pulmonary pressures (age 13 ± 9 years old, range 3–33).
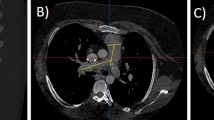
Imaging and Measurement
The MRIs included both contrast-enhanced, breath-hold (n = 49) and non-contrast, free-breathing (n = 5) angiograms without cardiac gating. Images were analysed by co-author C.G. with a standard DICOM viewer in multi-planar reconstruction view, being careful to perform measurements on slices that were perpendicular to the vessel axis. The vessel border was traced (generally with an oval-shaped segmentation tool or free draw tool) and effective diameter calculated as 2 √ (A/π), where A is the cross-sectional area. In this way, left and right PA effective diameters were measured immediately proximal to the origin of the first branches similar to the method described by Nakata et al. [15].
Statistical Methods
All data analyses were performed using R 3.5.1 [16], and all breakpoint analyses using the segmented [17, 18] packages. Our initial set of co-variates included the patient height, weight, age, and gender. Since previous studies have often indexed the PA size against BSA [14, 15, 19], this was employed as a co-variate rather than height and weight separately. In the reduced set of co-variates, gender was not found to be statistically significant, and was eliminated. Strong linear correlations were observed between BSA and age; hence, both quantities were not simultaneously employed as co-variates. A simple linear regression analysis was performed for the left PA diameter, right PA diameter, and mean (the average of the left and right) PA diameter with BSA as the explanatory variable in each case. In addition, piecewise linear regression and breakpoint analyses were performed for mean PA diameter with age as the explanatory variable. We also employed piecewise linear regression and breakpoint analyses to correlate BSA with age, with an initial guess of 15 years for the breakpoint estimation algorithm in both cases. Furthermore, we performed a simple linear regression analysis for the non-ECC group and the adults (age > 17.5) of the ECC group where the mean PA diameter was the response variable and BSA the explanatory variable. Standard F tests were used to determine the statistical significance of the estimates of slope and intercept and standard t tests to compare the slopes and intercepts between linear regression models. A significance level of 0.05 was employed for all statistical analyses.
Literature Review and Validation
We performed a broad search of English language literature in PubMed, and a detailed diagram of review process is shown in Fig. 1. All studies that reported sufficient information allowing for the calculation of mean PA size were used to validate our models; this thus excludes those studies that reported data in terms of median and range and those where the recorded age or BSA lies outside of the range of our patient cohort (and therefore outside the range of our models), as well as studies [20] which reported BSA-indexed data but without providing the BSA data. Depending on whether a study provided BSA data or age data, or both, it was used to validate the BSA model, age model, or both models, respectively. The search terms included “univentricular pulmonary arter* growth”, “Fontan pulmonary arter* growth”, “univentricular pulmonary arter* index”, “Fontan pulmonary arter* index”, “Fontan pulmonary arter* size”, and “univentricular pulmonary arter* size”. The initial search resulted in 871 possible articles, of which 765 studies were excluded based on a screening of the title and abstract. Of the remaining 106 articles, 94 were excluded based on the criteria specified above. All remaining articles that have measured the left and right PA diameters in Fontan patients are listed in Table 1. The procedure we used to extract PA measurements from published indexed data is described in the supplementary material. We used the following formula to calculate the percentage difference between our model prediction and published data:
Results
A statistically significant and strong positive linear correlation (p < 0.05, r = 0.9, n = 24) was observed between mean PA diameter and BSA in the ECC group (henceforth referred to as Model-BSA). A similar statistically significant and strong positive linear correlation was observed in the control group (henceforth referred to as the Model-BSAcontrol) between mean PA diameter and BSA (p < 0.05, r = 0.9, n = 18) (Fig. 2). Details of the point estimates and 95% confidence intervals for both models are provided in Table 2.
For the ECC group, when age was chosen to be the independent variable, a breakpoint was observed at 17.2 years (standard error = 2.5 years). In patients up to the age of 17.2, there was a statistically significant and strong positive linear correlation (p < 0.05, r = 0.88, n = 13) between the mean PA diameter and age (Fig. 3) (henceforth referred to as Model-Age). In ECC patients older than 17.2 years, the slope of the linear regression line did not achieve statistical significance (p = 0.78). Additionally, for ECC patients, we found a moderate positive linear correlation (r = 0.54, p < 0.05, n = 29) between the left PA and BSA and a strong positive linear correlation between the right PA and BSA (r = 0.82, p < 0.05, n = 27). For the non-ECC group (n = 19), the slopes of the linear regression lines were not significant for either BSA or age; therefore, no model was constructed. Comparing our model results against published data, the difference ranges between − 1.82 mm (− 15.77%) and 1.03 mm (8.24%) for Model-BSA (Table 3), and between − 2.38 mm (− 19.06%) and 2.16 mm (15.62%) for Model-Age (Table 4). In the case of the non-ECC group, the dataset included only adults (age range 17.7 to 40.2), and an analysis of the differences between the adult ECC and non-ECC groups is presented in the Supplementary Material.
Discussion
Scattered attempts have been made to study PA size in univentricular patients. The majority of the relevant literature focuses either on changes in the size of the PA between the various stages of the surgical palliation [11, 21, 22] or linking the pre-operative PA size to functional outcomes post-surgery [20, 23,24,25,26,27]. The bulk of the investigations that constitute the latter category of literature present normalized metrics of PA size such as the Pulmonary Artery Index as defined by Nakata et al. [15], and their utility in the optimal selection of patients for the Fontan procedure. The minority of the pertinent literature is composed of studies that have attempted to characterize PA growth, but reach no consensus [9,10,11,12,13,14]. These investigations of PA growth in univentricular patients have attempted to follow a cohort of univentricular patients as they grow, acquiring data regarding PA size only at a few time points. In contrast, we have modelled the statistics of PA size as a function of both age and BSA from a cohort of patients of varying ages, resulting in models applicable from post-Fontan repair to adulthood. While our models provide an estimate of the PA size using the BSA or age as the predictor, they were not constructed with the objective of making longitudinal predictions and therefore do not take current BSA or age as inputs to predict future PA size. Some of the previous studies have compared their results to normal children, and have highlighted statistically significant differences, but are again limited to one or two follow-up measurements. In contrast, the predictions of Model-BSA are consistently smaller than those of Model-BSAcontrol (Fig. 2), which is in agreement with previous reports of retarded growth [11]. The correlation between the left PA diameter and BSA is lower than that of the right PA diameter and BSA which may be due to the higher incidence of left PA stenoses, leading to higher variability and hence lower correlation.
Since our regression models were developed using data from ECC patients up to the age of 28 years, we caution against applying it on model PA size for other variations of the Fontan procedure or beyond the age of 28 years. In circumstances where height and weight are not available, Model-Age could be used to describe PA size as a function of age. Beyond the age of 17 years, the slope of the regression line in Model-Age was not statistically significant, which may indicate that PA growth halts at approximately 17 years of age.
When we compared our models against published data, the largest discrepancies for Model-BSA occur with Tatum et al., where our model underpredicts PA size by 1.8 mm (15.77%) (Table 3). The largest discrepancies for Model-Age occur with Buheitel et al., where our model underpredicts PA size by approximately 2.38 mm (~ 19%) (Table 4). A factor that may contribute to the discrepancies is that the cross section of the pulmonary arteries tends to be oval shaped rather than circular; therefore, assuming the cross section to be circular, the effective diameter calculated from cross-sectional area measurements obtained from cardiac MRI, as we have done, may be smaller than diameters measured by 2D projection methods that these studies likely have used.
Although we included a representative cohort of patients who had successfully undergone Fontan completion, the pre-Fontan course of these patients was variable. Despite the considerable heterogeneity in the native anatomy of the patients prior to the Fontan palliation and the variability in the pre-Fontan course, we observed statistically significant, strong correlations between the PA size and both BSA and age of the ECC group. In addition, both models underpredict PA size by a maximum of 2.38 mm when validated against literature data obtained from similar heterogenous Fontan samples. Given the strong correlations and the known range of validation errors, our proposed models can provide a useful estimate of PA size in ECC Fontan patients given age or BSA information.
Limitations
The lack of consistent metrics of Fontan PA size in literature limited the number of data points available for validating our proposed models. We have not examined PA growth in individuals longitudinally but have compared our results with longitudinal studies in literature. Additionally, this retrospective study divided the patients into very broad categories of ECC and non-ECC groups. Finally, the lack of data below the age of 17 years for the non-ECC group did not allow the development of models; however, ECC is the predominant surgery performed in the current era.
Clinical Relevance
At present, the immediate utility of our model is that it allows investigators conducting computational modelling studies to scale imaging data acquired as standard-of-care to any time point of interest. These anatomically realistic, scaled geometries may then be used in computational fluid dynamics simulations to study the hemodynamics of the Fontan junction and pulmonary arteries, thus aiding clinicians in surgical planning. In addition, our Model-BSA model when compared with Model-BSAcontrol model suggests that Fontan PA size is smaller than that of healthy subjects of the same body size.
Conclusion
At present, literature relating to PA size in Fontan patients is highly scattered with little consensus. Findings have been reported in a variety of metrics over varying ranges of follow-up periods, in different statistical measures and in varying measurement modalities, which hinder attempts to consolidate the reported data into a single model. Based on clinical data spanning a wide age range, we constructed mathematical models that characterize the mean PA diameter through to adulthood and have compared model results against a control cohort and published data. The results presented here could serve as a useful reference for clinicians. In addition, the models presented here can help expand the utility of geometries developed from standard-of-care imaging, by allowing them to scale to another time point of interest. These scaled geometries may then be employed in CFD simulations for investigating the hemodynamics of maturing Fontan circulations.
Abbreviations
- 3D:
-
Three-dimensional
- BSA:
-
Body surface area
- CFD:
-
Computational fluid dynamics
- ECC:
-
Extracardiac conduit
- MRI:
-
Magnetic resonance imaging
- PA:
-
Pulmonary arteries
References
de Zélicourt, D. A., & Kurtcuoglu, V. (2016). Patient-specific surgical planning, where do we stand? The example of the Fontan procedure. Annals of Biomedical Engineering, 44(1), 174–186. https://doi.org/10.1007/s10439-015-1381-9.
Bossers, S. S. M., Cibis, M., Gijsen, F. J., Schokking, M., Strengers, J. L. M., Verhaart, R. F., et al. (2014). Computational fluid dynamics in Fontan patients to evaluate power loss during simulated exercise. Heart (British Cardiac Society), 100(9), 696–701. https://doi.org/10.1136/heartjnl-2013-304969.
Tang, E., Wei, Z. (. A.)., Whitehead, K. K., Khiabani, R. H., Restrepo, M., Mirabella, L., et al. (2017). Effect of Fontan geometry on exercise haemodynamics and its potential implications. Heart, 103(22), 1806–1812. https://doi.org/10.1136/heartjnl-2016-310855.
Khiabani, R. H., Whitehead, K. K., Han, D., Restrepo, M., Tang, E., Bethel, J., et al. (2015). Exercise capacity in single-ventricle patients after Fontan correlates with haemodynamic energy loss in TCPC. Heart, 101(2), 139–143. https://doi.org/10.1136/heartjnl-2014-306337.
Kung, E., Baretta, A., Baker, C., Arbia, G., Biglino, G., Corsini, C., et al. (2013). Predictive modeling of the virtual hemi-Fontan operation for second stage single ventricle palliation: two patient-specific cases. Journal of Biomechanics, 46(2), 423–429. https://doi.org/10.1016/j.jbiomech.2012.10.023.
Baretta, A., Corsini, C., Yang, W., Vignon-Clementel, I. E., Marsden, A. L., Feinstein, J. A., et al. (2011). Virtual surgeries in patients with congenital heart disease: a multi-scale modelling test case. Philosophical transactions. Series A, Mathematical, physical, and engineering sciences, 369(1954), 4316–4330. https://doi.org/10.1098/rsta.2011.0130.
Marsden, A. L., Bernstein, A. J., Reddy, V. M., Shadden, S. C., Spilker, R. L., Chan, F. P., et al. (2009). Evaluation of a novel Y-shaped extracardiac Fontan baffle using computational fluid dynamics, Journal of Thoracic and Cardiovascular Surgery., 137(2), 394–403.e2. https://doi.org/10.1016/j.jtcvs.2008.06.043.
Dasi, L. P., KrishnankuttyRema, R., Kitajima, H. D., Pekkan, K., Sundareswaran, K. S., Fogel, M., et al. (2009). Fontan hemodynamics: importance of pulmonary artery diameter. Journal of Thoracic and Cardiovascular Surgery, 137(3), 560–564. https://doi.org/10.1016/j.jtcvs.2008.04.036.
Tatum, G. H., Sigfússon, G., Ettedgui, J. A., Myers, J. L., Cyran, S. E., Weber, H. S., & Webber, S. A. (2006). Pulmonary artery growth fails to match the increase in body surface area after the Fontan operation. Heart (British Cardiac Society), 92(4), 511–514. https://doi.org/10.1136/hrt.2005.070243.
Ovroutski, S., Ewert, P., Alexi-Meskishvili, V., Hölscher, K., Miera, O., Peters, B., et al. (2009). Absence of pulmonary artery growth after Fontan operation and its possible impact on late outcome. Annals of Thoracic Surgery, 87(3), 826–831. https://doi.org/10.1016/j.athoracsur.2008.10.075.
Buheitel, G., Hofbeck, M., Tenbrink, U., Leipold, G., von der Emde, J., & Singer, H. (1997). Changes in pulmonary artery size before and after total cavopulmonary connection. Heart (British Cardiac Society), 78(5), 488–492.
Restrepo, M., Mirabella, L., Tang, E., Haggerty, C. M., Khiabani, R. H., Fynn-Thompson, F., et al. (2014). Fontan pathway growth: a quantitative evaluation of lateral tunnel and extracardiac cavopulmonary connections using serial cardiac magnetic resonance. Annals of Thoracic Surgery, 97(3), 916–922. https://doi.org/10.1016/j.athoracsur.2013.11.015.
Robbers-Visser, D., Helderman, F., Strengers, J. L., van Osch-Gevers, L., Kapusta, L., Pattynama, P. M., et al. (2008). Pulmonary artery size and function after Fontan operation at a young age. Journal of magnetic resonance imaging : JMRI, 28(5), 1101–1107. https://doi.org/10.1002/jmri.21544.
Bossers, S. S. M., Cibis, M., Kapusta, L., Potters, W. V., Snoeren, M. M., Wentzel, J. J., et al. (2016). Long-term serial follow-up of pulmonary artery size and wall shear stress in Fontan patients. Pediatric Cardiology. https://doi.org/10.1007/s00246-015-1326-y.
Nakata, S., Imai, Y., Takanashi, Y., Kurosawa, H., Tezuka, K., Nakazawa, M., et al. (1984). A new method for the quantitative standardization of cross-sectional areas of the pulmonary arteries in congenital heart diseases with decreased pulmonary blood flow, The Journal of thoracic and cardiovascular surgery., 88(4), 610–619 Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/6482493. Accessed 10 Sept 2019.
R Core Team. (2018). R: a language and environment for statistical computing. Vienna, Austria. Retrieved from https://www.r-project.org/. Accessed 10 Sept 2019.
Muggeo, V. M. R. (2008). Segmented: an R package to fit regression models with broken-line relationships. R News, 8(1), 20–25 Retrieved from https://cran.r-project.org/doc/Rnews/. Accessed 10 Sept 2019.
Muggeo, V. M. R. (2003). Estimating regression models with unknown break-points. Statistics in Medicine, 22, 3055–3071.
Restrepo, M., Tang, E., Haggerty, C. M., Khiabani, R. H., Mirabella, L., Bethel, J., et al. (2015). Energetic implications of vessel growth and flow changes over time in Fontan patients. Annals of Thoracic Surgery, 99(1), 163–170. https://doi.org/10.1016/j.athoracsur.2014.08.046.
Kansy, A., Brzezińska-Rajszys, G., Zubrzycka, M., Mirkowicz-Małek, M., Maruszewski, P., Manowska, M., & Maruszewski, B. (2013). Pulmonary artery growth in univentricular physiology patients. Kardiologia Polska, 71(6), 581–587. https://doi.org/10.5603/KP.2013.0121.
Borowski, A., Reinhardt, H., Schickendantz, S., & Korb, H. (1998). Pulmonary artery growth after systemic-to-pulmonary shunt in children with a univentricular heart and a hypoplastic pulmonary artery bed. Implications for Fontan surgery. Japanese Heart Journal, 39(5), 671–680. https://doi.org/10.1016/j.athoracsur.2004.05.055.
Reddy, V. M., McElhinney, D. B., Moore, P., Petrossian, E., & Hanley, F. L. (1996). Pulmonary artery growth after bidirectional cavopulmonary shunt: is there a cause for concern? The Journal of Thoracic and Cardiovascular Surgery, 112(5), 1180–1190; discussion 1190-1192. https://doi.org/10.1016/S0022-5223(96)70131-9.
Knott-Craig, C. J., Julsrud, P. R., Schaff, H. V., Puga, F. J., & Danielson, G. K. (1993). Pulmonary artery size and clinical outcome after the modified Fontan operation. The Annals of Thoracic Surgery, 55(3), 646–651. https://doi.org/10.1016/0003-4975(93)90268-M.
Lehner, A., Schuh, A., Herrmann, F. E. M., Riester, M., Pallivathukal, S., Dalla-Pozza, R., et al. (2014). Influence of pulmonary artery size on early outcome after the Fontan operation. Annals of Thoracic Surgery, 97(4), 1387–1393. https://doi.org/10.1016/j.athoracsur.2013.11.068.
Adachi, I., Yagihara, T., Kagisaki, K., Hagino, I., Ishizaka, T., Kobayashi, J., et al. (2007). Preoperative small pulmonary artery did not affect the midterm results of Fontan operation. European Journal of Cardio-Thoracic Surgery, 32(1), 156–162. https://doi.org/10.1016/j.ejcts.2007.03.024.
Senzaki, H., Isoda, T., Ishizawa, A., & Hishi, T. (1994). Reconsideration of criteria for the Fontan operation. Influence of pulmonary artery size on postoperative hemodynamics of the Fontan operation. Circulation, 89(3), 1196–1202. https://doi.org/10.1161/01.CIR.89.3.1196.
Baek, J. S., Bae, E. J., Kim, G. B., Kim, W. H., Lee, J. R., Kim, Y. J., et al. (2011). Pulmonary artery size and late functional outcome after Fontan operation. Annals of Thoracic Surgery, 91(4), 1240–1246. https://doi.org/10.1016/j.athoracsur.2010.12.002.
Wagner, M., Nguyen, K.-L., Khan, S., Mirsadraee, S., Satou, G. M., Aboulhosn, J., & Finn, J. P. (2012). Contrast-enhanced MR angiography of cavopulmonary connections in adult patients with congenital heart disease. AJR. American Journal of Roentgenology, 199(5), W565–W574. https://doi.org/10.2214/AJR.11.7503.
Acknowledgements
We would like to thank the Department of Mechanical Engineering at Clemson University for their support.
Funding
This work was supported by an Award from the American Heart Association, The Children’s Heart Foundation, and the Department of Mechanical Engineering at Clemson University. J.P. Mynard is supported by a co-funded Career Development Fellowship from the National Health and Medical Research Council of Australia and a Future Leader Fellowship from the National Heart Foundation. The Heart Research group at MCRI (J.P. Mynard) is supported by the Victorian Government’s Operational Infrastructure Support Program, Big W, and RCH1000.
Author information
Authors and Affiliations
Contributions
A. Gupta contributed to the conception of this work, performed the statistical analyses and interpretation of the data, and drafted the manuscript. C. Gillett acquired data and revised the work critically for important intellectual content. P. Gerard contributed to the design of the study and performed critical revision for intellectual content. M.M.H. Cheung contributed to data acquisition and performed critical revision for intellectual content. J.P. Mynard contributed to the design of the study and performed critical revision for intellectual content. E. Kung contributed to the conception and design of the study and performed critical revision for intellectual content. All authors have approved the submitted version of the manuscript.
Corresponding author
Ethics declarations
The funding agencies/sponsors had no involvement in the study design; in the collection, analysis and interpretation of the data; in the writing of the report; and in the decision to submit the paper for publication.
Conflict of Interest
The authors declare that they have no conflict of interest.
Human Subjects/Informed Consent Statement
Informed consent was not necessary as the data did not contain any identifying information.
Institutional Review Board Approval
The Human Research Ethics Committee of the Royal Children’s Hospital Melbourne approved the retrospective use of data for this study (Ref. No: 37205A).
Animal Studies
No animal studies were carried out by the authors for this article.
Additional information
Associate Editor Ana Barac oversaw the review of this article
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic Supplementary Material
ESM 1
(DOCX 686 kb)
Rights and permissions
About this article
Cite this article
Gupta, A., Gillett, C., Gerard, P. et al. Predictive Models for Pulmonary Artery Size in Fontan Patients. J. of Cardiovasc. Trans. Res. 14, 782–789 (2021). https://doi.org/10.1007/s12265-020-09993-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12265-020-09993-4