Abstract
Since its initial application in the pediatric patient population, the Berlin Heart EXCOR ventricular assist device has become a widely accepted form of mechanical circulatory support in Europe and the USA. The versatility of the device makes it ideal for pediatric patients because it can be tailored to the size and needs of the patient. In this review, we will explore the broad range of clinical applications of this device including bridge to cardiac transplantation, bridge to recovery, and bridge to bridge implantation where the need for cardiac transplantation may be unclear but long-term mechanical support may be required.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The EXCOR Ventricular Assist Device System
The Berlin Heart EXCOR (Mediport; Berlin, Germany) is an extracorporeal ventricular assist device (VAD) that was initially used to mechanically support adult heart failure patients [1]. The experience in adult heart failure patients as a bridge to cardiac transplantation or as destination therapy led to specific design modifications for pediatric application. Adult ventricular assist devices have limited application in pediatric patients due to smaller patient sizes, particularly infants and toddlers. Using an oversized device in pediatric patients can lead to stasis of blood within the pump and increase the thromboembolic risk [2]. Also, the excess stroke volume may lead to systolic hypertension. A miniaturized device with blood pumps of varying stroke volumes is ideal for pediatric patients. This allows the device to be tailored to the size of individual patient. The EXCOR system has three primary components, and it can be implanted in a left ventricular, right ventricular, or biventricular configuration. The components are a blood pump, cannulae for connection of the device to the great vessels and cardiac chambers, and a pneumatic drive unit.
The blood pump is made of transparent polyurethane. It has two trileaflet valves, also made of polyurethane, that allow unidirectional blood flow into and from the pump. A pneumatic compressor-operated diaphragm separates the blood chamber from the air chamber. For pediatric patients, the blood chamber is designed for 10, 25, or 30 cc stroke volumes. Multiple pump sizes allow the mechanical circulatory support system to be tailored to the needs of the infant or toddler (Fig. 1). The 10-cc pump can be used to support patients with a body weight up to 9 kg or a body surface area of 0.43 cm2, and the 25-cc pump can be used to support patients with a body weight up to 30 kg or a body surface area of 0.95 cm2 [3]. A 17-cc pump is in development by Berlin Heart for patients weighing 8 to 12 kg. Titanium connectors allow the blood pump to be attached in an extracorporeal position to the cannulae. The transparency of the device allows rigorous daily evaluation of the pump for clot formation. The extracorporeal position of the pump allows straightforward pump exchange under conscious sedation should the need arise.
The cannulae are made of silicone and are designed with several internal diameters (4.8, 6.0, 9.0 mm) for the pediatric population. A layer of Dacron velour covers the mid-portion of the cannula. The velour bridges the skin exit site and allows for rapid tissue ingrowth that is believed to prevent ascending infection (Fig. 2). For a left ventricular configuration (LVAD), two cannulation strategies are possible. Most commonly, the left ventricular apex is cannulated for inflow to the pump, but the left atrium is an alternate inflow cannulation site [4]. The ascending aorta is cannulated for pump outflow (Fig. 3). For a right ventricular configuration (RVAD), the right atrium is cannulated for inflow to the device, and the main pulmonary artery is cannulated for outflow. A biventricular configuration (BiVAD) involves use of an LVAD and RVAD.
Experience at the German Heart Institute has shown that left ventricular apical cannulation results in lower left ventricular end-diastolic pressure and consequently right ventricular afterload by 15–25 mmHg [5]. Usually this allows the patient to be supported solely with an LVAD. Biventricular support (BiVAD) has generally been reserved for patients who initially present with evidence of significant right ventricular failure in addition to left ventricular dysfunction. In the series reported by Gandhi et al. from St. Louis Children’s Hospital, the mean right ventricular ejection fraction for patients supported with a BiVAD was 29% [6].
From a technical standpoint, the large footprint of the ascending aorta cannula may require an alternative arterial cannulation strategy at the time of heart transplantation. Specifically, a Gore-Tex graft can be sewn to the innominate artery and used for arterial inflow during cardiopulmonary bypass. The arterial cannula is placed inside the graft, secured, and then connected to the bypass circuit. Using this strategy, the recipient aorta can be cross-clamped and transected leaving an adequate cuff for anastomosis to the donor heart. The skin exit site for the ascending aorta cannula has to be carefully planned to avoid right ventricular dysfunction related to compression of the right coronary artery in the atrioventricular groove. The cannula should exit the mediastinum laterally overlying the right atrial appendage and the free wall of the right atrium. The lie of the cannula should be a gentle curve avoiding pulling the cannula too taut causing compression of the cardiac chambers.
In neonates undergoing implantation of this device, the ascending aorta can be quite small. The size of the ascending aorta can make insertion of the arterial cannula challenging due to the stiffness of the sewing ring. Tjan et al. have described a technique where a cuff of bovine pericardium is attached to the sewing ring of the arterial cannula. The pericardial cuff is then used to attach the arterial cannula to the ascending aorta [7].
The EXCOR ventricular assist device has an electropneumatic driving unit called IKUS (Fig. 4). Its fundamental mechanism is the use of compressed air to move the diaphragm that separates the blood chamber from the air chamber. This movement provides pulsatile blood flow. A positive driving pressure up to 350 mmHg can be used to compress the diaphragm to end-systole allowing ejection of blood from the device. A negative driving pressure up to −100 mmHg is used to expand the diaphragm to end-diastole allowing the device to fill. The high driving pressures are necessary due to the small size of the cannulae [8].
The IKUS driver has three compressors. There is one compressor for an RVAD, one for an LVAD, and a backup. The driver can function in a left ventricular mode or a biventricular mode. The system can also function in an asynchronous mode that allows separate rates for the RVAD and LVAD when biventricular support is necessary. This asynchronous mode allows the rate of the RVAD to be less than the LVAD with a smaller stroke volume (blood pump) to prevent development of pulmonary edema. Finally, all blood contacting surfaces are heparin-coated [8] (Carmeda, Inc., San Antonio, TX, USA).
Historical Perspective
Frazier reported the first successful use of a left ventricular assist device as a bridge to cardiac transplantation in a pediatric patient in 1989. That patient was supported with a centrifugal flow device for 12 h prior to transplantation [9]. This experience was soon followed by a report from the German Heart Institute in 1991 describing the use of an adult EXCOR device (50 cc blood pump) to support an 8-year-old patient as a bridge to cardiac transplantation [10]. The disadvantages of using adult devices to support pediatric patients quickly became apparent to our colleagues in Germany, and efforts were begun to design the EXCOR device specifically for the pediatric population. The modifications made included a range of blood pump sizes and cannula sizes so that the mechanical support system could be tailored to the size and needs of the patient.
Indications for Implantation
As experience with the pediatric device was gained in Germany, the indications and criteria for implantation were better defined. These criteria include progressive heart failure refractory to medical therapy as indicated by a cardiac index less than 2.0 L/min/m2, the development of metabolic acidosis, and signs of end organ dysfunction with renal insufficiency and/or an elevation of liver enzymes. Other indicators include the need for mechanical ventilation or mixed venous oxygen saturation less than 40%. The goal of implantation at this time is to give the recipient time for end organ recovery thus making the patient a better transplant candidate [11] (Table 1).
Current Uses of the EXCOR Pediatric Ventricular Assist System
Bridge to Cardiac Transplantation or Re-transplantation
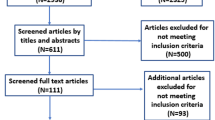
The predominant use of the Berlin Heart EXCOR ventricular assist device has been as a bridge to cardiac transplantation (Table 2). Since their initial experience implanting the adult EXCOR device in a pediatric patient, Hetzer et al. recently reported their 15-year experience implanting the pediatric EXCOR system through July 2005. This experience included 68 patients less than 18 years of age who were supported for a mean duration of 35 days. Thirty-one of the 68 patients (45%) were bridged to cardiac transplant. Eleven patients (16%) were bridged to recovery. Other indications for mechanical support in this report included end-stage congenital heart disease and postcardiotomy heart failure. Fifty-four percent of the patients were discharged home. Only four patients in this series suffered neurologic injury [12].
Perhaps the largest US experience with the EXCOR pediatric ventricular assist system has been reported by the cardiac unit at Arkansas Children’s Hospital in Little Rock, AR, USA. Rockett et al. described the initial experience of this unit with the EXCOR system in a 2008 report [13]. Seventeen patients less than 18 years of age received either an LVAD (n = 13) or BVAD (n = 4). At the time of the report, 11 patients were bridged to transplant (65%), one to recovery, one remained on support, and four children died. In 2009, Imamura et al. compared the Arkansas Children’s Hospital experience with the EXCOR system to their experience with extracorporeal membrane oxygenation (ECMO) as a bridge to cardiac transplantation. What they found was that survival to transplant and recovery was significantly higher in the EXCOR subgroup versus the ECMO group (86% versus 57%). Despite this excellent result, 40% of the patients sustained neurologic injury [14].
St. Louis Children’s Hospital reported their experience with the EXCOR ventricular assist system in 2008 [6]. Unlike the reports from Germany and Arkansas, all of the patients in this series had preoperative right ventricular dysfunction based on a preoperative echocardiogram. Consequently, all nine patients in this series were bridged to cardiac transplantation with biventricular support (BVAD). The mean duration of support was 31 days and eight of nine patients (89%) survived to transplant. None of the patients in this series had acute neurologic injury, thromboembolic events, or any evidence of hemolysis based on plasma-free hemoglobin measurement. All of the patients in this series had significantly elevated (>90%) panel reactive antibodies as determined by ELISA. Also, there were a total of 12 pump exchanges due to fibrin deposits or clot formation in the device.
Malaisrie et al. recently reported their initial experience with the EXCOR system at Stanford University Hospital and Lucile Packard Children’s Hospital [15]. Eight patients had either LVAD support (n = 5) or BVAD support (n = 3) for a mean duration of 57 days. Sixty-three percent of the patients were successfully bridged to transplant. However, five of eight patients (63%) developed neurologic injury, and four of the eight patients (50%) required device exchange.
There has been one recent report in the literature describing the use of the EXCOR system as a bridge to cardiac re-transplantation. Krokstrom et al. from the pediatric cardiac unit at the University of Lund in Sweden reported use of the EXCOR system as a BVAD in a 10-month-old infant with primary graft dysfunction after cardiac transplantation. This patient was bridged for 165 days before re-transplantation [16].
Bridge to Recovery
In 1999, Stiller et al. reported one of the largest series describing use of the EXCOR system as a bridge to recovery in pediatric patients [17]. Four patients less than 10 years of age presented with fulminant myocarditis. The youngest patient was 1 year old, and all four patients had severe cardiogenic shock with multi-organ dysfunction. This required preoperative mechanical ventilation and renal replacement therapy. Two of the four patients were supported with ECMO prior to VAD implantation. The mean time of ECMO support was 5.5 days. All four patients received biventricular support (BVAD). The mean duration of VAD support was 16 days. Three patients were successfully weaned from the device, and one patient was bridged to cardiac transplantation after 20 days of mechanical support.
Because it may take months for myocardial recovery in patients with fulminant myocarditis, the EXCOR system provides an excellent means for long-term mechanical support until recovery occurs. Among its many advantages is the ability to extubate the patient and to give the patient aggressive physical therapy which includes ambulation. Also, once extubated, the patient is able to take food by mouth which enhances the integrity of the gastrointestinal tract mucosa preventing bacterial translocation and decreasing the risk for infection (Table 3). Jones et al. reported use of an EXCOR BiVAD in an 8-month-old boy with acute myocarditis. This patient was supported for a total of 120 days until myocardial recovery occurred and the device could be explanted [18].
Another interesting case utilizing the EXCOR system as a bridge to recovery was recently reported by Tschirkov et al. from the cardiac surgery unit at University Hospital in Sofia, Bulgaria [19]. An 11-year-old boy with a partial atrioventricular canal defect sustained a myocardial infarction 2 days after repair of his congenital cardiac anomaly. After intraoperative exploration on cardiopulmonary bypass, the patient was unable to be weaned and had an EXCOR LVAD placed with cannulation of the left atrium for inflow to the device. After 29 days of support, the patient was successfully explanted with complete myocardial recovery. This case highlights the versatility of the EXCOR system with multiple cannula sizes, pump sizes, and alternate cannulation sites that allow the system to be tailored to the needs of the patient.
Bridge to Bridge
Maat et al. from The Netherlands have described a unique configuration of the Berlin Heart EXCOR system that involves connection of the EXCOR cannulae to a Centrimag (Levitronix LLC, Waltham, MA, USA) centrifugal flow pump [20]. In their series, three patients presented with a diagnosis of dilated cardiomyopathy. All three patients were initially supported with ECMO due to an acute deterioration of their clinical status. While on ECMO, each patient developed significant pulmonary venous congestion. Once this occurred, the authors chose to cannulate the patients for ventricular assist device support using EXCOR cannulae. One patient had an LVAD and two patients had a BVAD. To allow a period of stabilization and resolution of the pulmonary congestion, the EXCOR cannulae were connected to a Levitronix centrifugal flow pump. Two of the three patients were bridged to an EXCOR blood pump, and one of those patients was bridged to cardiac transplantation. The other patients died. The largest series of patients to date utilizing the Berlin Heart EXCOR ventricular assist device as bridge to bridge mechanical circulatory support was reported by Loforte et al. from the German Heart Institute in 2009 [21]. They described 55 adult patients supported with the Centrimag (Levitronix LLC, Waltham, MA, USA) centrifugal flow pump for a mean of 8.1 days before EXCOR exchange. The primary indication for bridge to bridge support in these patients was postcardiotomy cardiogenic shock. These two series again highlight the versatility of this device and its ability to be applied in a broad range of clinical situations.
Single Ventricle Physiology
The first successful case utilizing the EXCOR ventricular assist device as a bridge to cardiac transplantation after a bidirectional cavopulmonary shunt (BDG) for single ventricle physiology was recently reported by Irving et al. from the UK [22]. In that report, a 2-year-old patient with hypoplastic left heart syndrome developed severe right ventricular dysfunction and tricuspid insufficiency after a neonatal Norwood procedure and BDG performed at 4 months of age. The apex of the systemic ventricle was cannulated for inflow to the device, and the neoaorta was cannulated for outflow. The patient was bridged for 7 days prior to orthotopic heart transplantation and had an uncomplicated postoperative course. Other centers have also reported use of the EXCOR system for patients with hypoplastic left heart syndrome after a BDG [23] and Fontan [24] with mixed results.
Discussion
Since its initial application in the pediatric patient population, the Berlin Heart EXCOR ventricular assist device has become a widely accepted form of mechanical circulatory support in Europe and the USA. The versatility of the device makes it ideal for pediatric patients because it can be tailored to the size and needs of the patient. As described in this review, it has a broad range of clinical applications including bridge to cardiac transplantation, bridge to recovery, and bridge to bridge implantation where the need for cardiac transplantation may be unclear but long-term mechanical support may be required.
Prior to the introduction of this device by the German Heart Institute, adult circulatory support devices were used for pediatric patients with mixed results. One particular drawback of using adult circulatory support systems in children is the increased risk for thromboembolic events [2, 25]. But perhaps the most important disadvantage is that one-size device does not fit all pediatric patients. The need for mechanical circulatory support systems specifically designed for the vast range of pediatric patient sizes is clear. Emphasis on this need could not have been made clearer than when the National Institutes of Health funded five pediatric centers to develop novel ventricular assist systems [26].
It should be emphasized that the Berlin Heart EXCOR is an investigational device in the USA. An investigational device exemption (IDE) trial of the EXCOR device in the USA is ongoing. One question that remains unanswered about this device is the ideal anticoagulation strategy. Perhaps related to this, the rate of neurologic injury in the bridge to transplant subgroup has varied from 0% to 63% in the numerous small series that have been reported thus far [6, 12–16].
While the anticoagulation strategy is protocol based within the IDE trial, there is still institutional variability outside the IDE trial. Most often anticoagulation is initiated with unfractionated heparin after implantation of the device. After extubation, patients can be transitioned to a low molecular weight heparin, usually enoxaparin. The adequacy of heparin therapy is monitored with anti-Xa levels and can be correlated with the partial thromboplastin time. Antiplatelet agents such as aspirin and persantine are added if the platelet function is preserved, and there is no evidence of thrombocytopenia. Functional assessment can be measured using thromboelastography (TEG). The TEG incorporates the contributions of antithrombin, fibrinogen, von Willebrand factor, and other clotting proteins to the strength of the platelet plug and assesses the potential impact on device thrombogenesis.
Once it is assured that the patient has reliable gastrointestinal absorption, the patient can be bridged to warfarin as the primary systemic anticoagulant. Warfarin’s anticoagulant effect is monitored by the international normalized ratio. Given the complexity of the anticoagulation strategy, our institution and others have found consultation with a hematologist on all device patients to be a useful adjunct in their management.
Conclusions
The Berlin Heart EXCOR ventricular assist device is a versatile form of mechanical circulatory for pediatric patients with end-stage heart disease. Even though it is currently an investigational device in the USA, it is clear that the EXCOR device has filled a void in our ability to care for the increasing number of pediatric patients with end-stage heart disease. Our hope is that as our experience and acceptance of this device increases that our patients will be better served.
References
Jurmann, M. J., Weng, Y., Drews, T., Pasic, M., Hennig, E., & Hetzer, R. (2004). Permanent mechanical circulatory support in patients of advanced age. European Journal of Cardiothoracic Surgery, 25(4), 610–618.
Reinhartz, O., Hill, J., Al-Khaldi, A., Pelletier, M., Robbins, R., & Farrar, D. (2005). Thoratec ventricular assist devices in pediatric patients: Update on clinical results. ASAIO Journal, 51(5), 501–503.
Hetzer, R., & Stiller, B. (2006). Technology insight: Use of ventricular assist devices in children. Nature Clin Prac, 3(7), 377–386.
Merkle, F., et al. (2003). Pulsatile mechanical cardiac assistance in pediatric patients with the Berlin heart ventricular assist device. J Extra Corpor Technol, 35, 115–120.
Stiller, B., Weng, Y., Hubler, M., et al. (2005). Pneumatic pulsatile ventricular assist devices in children under 1 year of age. European Journal of Cardiothoracic Surgery, 28, 234–239.
Gandhi, S. K., Huddleston, C. B., et al. (2008). Biventricular assist devices as a bridge to heart transplantation in small children. Circulation, 118(suppl 1), S89–S93.
Tjan, T., Hoffmeier, A., Scheld, H., & Klotz, S. (2010). Ventricular assist device implantation in neonates: Adjustment of the BerlinHeart EXCOR arterial cannula with bovine pericardium. The Journal of Thoracic and Cardiovascular Surgery, 139(3), 783–784.
Hetzer, R., Loebe, M., Potapov, E., et al. (1998). Circulatory support with pneumatic paracorporeal ventricular assist device in infants and children. The Annals of Thoracic Surgery, 66, 1498–1506.
Frazier, O. (1989). Use of left ventricular assist device as a bridge to transplantation in a pediatric patient. Texas Heart J, 16, 46–50.
Warnecke, H., Berdjis, F., Henning, E., et al. (1991). Mechanical left ventricular support as a bridge to cardiac transplantation in childhood. European Journal of Cardiothoracic Surgery, 5, 330–333.
Hetzer, R., Potapov, E. V., et al. (2006). Improvement in survival after mechanical circulatory support with pneumatic pulsatile ventricular assist devices in pediatric patients. The Annals of Thoracic Surgery, 82, 917–925.
Hetzer, R., Meskishvili, V., Wen, Y., et al. (2006). Mechanical cardiac support in the young with the Berlin Heart EXCOR pulsatile ventricular assist device: 15 years’ experience. Semin Thorac Cardiovasc Surg Pediatr Card Surg Ann, 9, 99–108.
Rockett, S. R., Bryant, J. C., et al. (2008). Preliminary single center North American experience with the Berlin Heart pediatric EXCOR device. ASAIO Journal, 54, 479–482.
Imamura, M., Dossey, A. M., et al. (2009). Bridge to cardiac transplant in children: Berlin heart versus extracorporeal membrane oxygenation. The Annals of Thoracic Surgery, 87, 1894–1901.
Malaisrie, S. C., Pelletier, M. P., Yun, J. J., Sharma, K., et al. (2008). Pneumatic ventricular assist devices in infants and children: Initial Stanford experience. The Journal of Heart and Lung Transplantation, 27, 173–177.
Krokstrom, A., Higgins, T., Johansson, S., & Jogi, P. (2009). Use of pediatric Berlin Heart EXCOR biventricular device as a bridge to retransplantation in a 10 month old infant with acute graft failure after cardiac transplantation. ASAIO Journal, 55, 525–526.
Stiller, B., Dahnert, I., Weng, Y. G., Hennin, E., Hetzer, R., & Lange, P. E. (1999). Children may survive severe myocarditis with prolonged use of biventricular assist devices. Heart, 82, 237–240.
Jones, C. B., Cassidy, J. V., et al. (2009). Successful bridge to recovery with 120 days of mechanical support in an infant with myocarditis. The Journal of Heart and Lung Transplantation, 28, 202–205.
Tschirkov, A., Nikolov, D., & Papantchev, V. (2007). The Berlin Heart EXCOR in an 11 year old boy. A bridge to recovery after myocardial infarction. Texas Heart Institute Journal, 34(4), 445–448.
Maat, A., van Thiel, R., Dalinghaus, M., & Bogers, J. (2008). Connecting the Centrimag Levitronix pump to Berlin heart EXCOR cannulae: A new approach to bridge to bridge. The Journal of Heart and Lung Transplantation, 27, 112–115.
Loforte, A., Potapov, E., et al. (2009). Levitronix Centrimag to Berlin Heart EXCOR: A “bridge to bridge” solution in refractory cardiogenic shock. ASAIO Journal, 55, 465–468.
Irving, C. A., Cassidy, J., et al. (2009). Successful bridge to transplant with the Berlin Heart after cavopulmonary shunt. The Journal of Heart and Lung Transplantation, 28, 399–401.
Chu, M., Sharma, K., et al. (2007). Berlin Heart ventricular assist device in a child with hypoplastic left heart syndrome. The Annals of Thoracic Surgery, 83, 1179–1181.
Nathan, M., Baird, C., Fynn-Thompson, F., et al. (2006). Successful implantation of a Berlin Heart biventricular assist device in a failing single ventricle. The Journal of Thoracic and Cardiovascular Surgery, 131, 1407–1408.
Arabia, F. A., Tsau, P. H., Smith, R. G., et al. (2006). Pediatric bridge to heart transplantation: Application of the Berlin heart, Medos, and Thoratec ventricular assist devices. The Journal of Heart and Lung Transplantation, 25, 16–21.
Baldwin, J. T., Borovetz, H. S., et al. (2006). The national heart, lung, and blood institute pediatric circulatory support program. Circulation, 113, 147–155.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bryant, R., Steiner, M. & St. Louis, J.D. Current Use of the EXCOR Pediatric Ventricular Assist Device. J. of Cardiovasc. Trans. Res. 3, 612–617 (2010). https://doi.org/10.1007/s12265-010-9218-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12265-010-9218-2