Abstract
The natural course of early breast cancer has changed as a result of the introduction of mammographic screening. The present aim was a prospective analysis of screen-detected and symptomatic operable breast cancers in the era of mammographic service screening. The mode of detection (screen-detected, symptomatic or interval cancer), the type of mammographic image and other characteristics (the invasive tumor size, histological tumor type, grade, nodal, hormone receptor and HER2 status and the presence of lymphovascular invasion) of 569 invasive breast cancers were studied. Screen-detected cancers were significantly more frequently of grade I, <10 mm of size and node-negative (p < 0.001, respectively). Symptomatic/interval cancers were significantly more frequently of grade 3, >20 mm of size (p < 0.001), and exhibited lymphovascular invasion (p = 0.001). Screening-detection of the tumor favored breast-conserving surgery, sentinel lymph node biopsy and the avoidance of chemotherapy (p < 0.001). Cancers associated with casting-type calcifications on the mammogram were typically of ductal type (p = 0.043), of grade 2–3, estrogen receptor and progesterone receptor-negative and HER2-positive (p < 0.001). Interval cancers occurred significantly more often at a younger age and remained mammographically occult as compared with other cancers. Mammographic screen-detected cancers demonstrate more favorable prognostic features, and need less extensive treatment than symptomatic or interval cancers. The mammographic appearance of the tumor reflects its biological behavior, and this should be considered in the management optimization.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The role of mammographic service screening in the reduction of breast cancer mortality has been consistently revealed in numerous randomized controlled clinical studies and meta-analyses. [1–5] Thus, breast cancer-related mortality is significantly reduced in women invited to mammographic service screening as compared with those not invited to participate. [1–5] A recent analysis by the Swedish Organised Service Screening Evaluation Group demonstrated that, provided the screening program shows good quality indicators and participation is high enough, a reduction in breast cancer mortality of between 40% and 45% may be achieved. [3] In fact, the constantly developing adjuvant therapies are also contributing to the decline in breast cancer mortality. The aim of the Cancer Intervention and Surveillance Modeling Network breast cancer program was to model the impact of various cancer interventions on the trends of breast cancer incidence and mortality. An 8–23% reduction in mortality has been attributed to the mammographic screening itself. [6]
This is explained primarily by fact that the breast cancers detected by such screening are in an early stage. An appreciable number of studies have clearly indicated that the introduction of mammographic screening has been followed by a shift to tumors with better prognostic factors. [7–14] Thus, screen-detected breast cancers are smaller, more frequently lymph node-negative, [7–14] of lower grade, [9, 11, 13] and consequently need less oncological treatment than their symptomatic counterparts. [11, 13] In addition to this stage shift stemming from the earlier detection, the better outcome is explained by the different biological behavior of these early cancers, since the detection by mammographic screening has been shown to be an independent favorable prognostic factor as regards distant metastasis-free survival and overall survival relative to that in symptomatic tumors. [11–13]
The type of mammographic image has recently been suggested as an independent prognostic factor. The presence of casting-type calcifications has been demonstrated to be a prognostic factor which carries a significantly higher risk of death as compared with cancers not associated with this mammographic abnormality. [15–20] In contrast, stellate lesions on the mammogram reflect a more favorable prognosis than any other mammographic appearances. [16–18]
In the present prospective study, we set out to investigate the patient- and tumor-related features in early breast cancer shortly after the introduction of mammographic service-screening in Hungary. Conventional prognostic factors, the need for oncological treatment and the mammographic appearance were analyzed in tumors that were detected by screening or were symptomatic. The clinicopathological features of interval cancers were also addressed.
Patients and Methods
The patient- and tumor-related data on women with breast cancer attending the Breast Unit of the University of Szeged, Hungary between May 1, 2004 and January 1, 2007 were prospectively collected. The following data were registered: the age of the patient at the time of breast surgery, the type of breast surgery (breast-conserving surgery vs mastectomy), the type of lymph node surgery (sentinel lymph node biopsy vs axillary lymph node dissection), the pathological size, the histological type, the histological grade, the hormone receptor (estrogen receptor (ER) and progesterone receptor (PR)) and HER2 status of the tumor and the presence of lymphovascular invasion (LVI). The pathological nodal status was recorded when possible, but in five screen-detected and ten symptomatic, clinically N0 cases this information was missing since axillary surgery was not performed because of the advanced age of the patient. The mode of detection of the breast cancer was registered in the following categories: screen-detected (detected by breast imaging within the national mammography screening program or by opportunistic screening), symptomatic (detected via any symptom related to the tumor in a patient who did not attend any screening program) or interval cancer (the tumor was diagnosed during the interval between two successive screening rounds and within 2 years after a negative screening finding). Population-based mammographic service screening started in Hungary in 2001. Within the program, women aged 45–65 years are invited biennially by letter to screening. Double-view mammography is performed and the mammograms are read by two radiologists with skills in interpreting mammography images. Other details of the program are in accordance with the European Society of Mastology guidelines [21].
The mammographic appearance of the tumor, based on the mammography report, was registered. In the event of any ambiguity or doubt, the original mammogram was collected and evaluated. Mammographic images were classified according to Tabár et al. [15] as follows. (1) a stellate lesion, (2) a circular or oval mass, (3) a parenchymal distortion/nonspecific asymmetric density, or (4) no mammographic abnormality. Possibly associated malignant calcifications were categorized into two groups: casting-type calcifications and non casting-type calcifications (a common group of powdery, crushed stone-like, pleiomorphic, etc. calcifications). For the analysis of the association between the mammographic image and other characteristics of the tumor, the previous categories were grouped in the following way: (1) stellate lesions without calcifications, (2) casting-type calcifications with or without an associated tumor mass, and (3) others. Ten-year risks of relapse and mortality were computed on the basis of the conventional prognostic factors (ER and HER2 status, grade, invasive tumor size and nodal status) using the software Adjuvant! [22]. This system provides predicted outcomes based on the patient and tumor characteristics. The adjuvant hormonal therapy and/or chemotherapy chosen according to the local protocol, though obviously influenced by the preferences and the comorbidities of the patient, were recorded.
For the categorical parameters, chi-square or Fisher tests were applied; for the analysis of continuous data, variance analysis was used.
Results
The data on 565 patients with 569 invasive breast cancers were collected. (Four patients had synchronous bilateral invasive breast cancer.) The patient- and tumor-related characteristics were first analyzed according to the mode of detection. Overall, 258 tumors (46%) were screen-detected, while 263 (46%) were symptomatic and 48 (8%) were interval cancers. The mean ( ± SD) age of the overall patient population at the time of breast surgery was 58.1 ± 10.9 years (range 27.8–85.1), while that of the cases with screen-detected or symptomatic tumors was 58.4 ± 7.6 and 58.5 ± 13.9 years, respectively, and that of the patients with interval cancers was 54.3 ± 5.4 years (p = 0.04). While 35.4% of the patients with interval cancer, and 31% of the patients with symptomatic cancer were premenopausal, only 20.2% of the patients with screen-detected cancer were premenopausal (p = 0.007). The pathological tumor characteristics and computed 10-year risks of relapse and mortality are presented in Table 1. No data were available on the grade in 4, on the ER/PR status in 2 and on the HER2 status in four cases. No difference was found in the histological type, the ER/PR status or the HER2 status according to the mode of detection. Significantly more of the screen-detected cancers were of grade I, <10 mm and node-negative (p < 0.001), while significantly more cancers in the groups of symptomatic and interval cancers were of grade 3, >20 mm of size (p < 0.001), and exhibited LVI (p = 0.001). The predicted average 10-year risks of relapse and death were significantly (p < 0.001) superior in the screen-detected cases compared to that in the symptomatic or the interval cancer cases, respectively (Table 1).
Next, we studied the use of surgical and medical treatment options, according to the mode of detection (Table 2). The rate of breast-conserving surgery among the patients with screen-detected cancers was significantly (p < 0.001) higher than that in symptomatic or interval cancer cases. Similarly, the rate of sentinel lymph node biopsy was the highest in the group with screen-detected tumors (p < 0.001). In 15, clinically node-negative cases, no axillary surgery was performed because of the advanced age of the patient. Adjuvant chemotherapy was significantly less frequently applied in the patients with screen-detected cancers (36.8%) than in the symptomatic (53.6%) or interval cancer (66.7%) cases (p < 0.001). The frequency of use of hormone therapy was similar in the three groups (Table 2).
The patient- and tumor-related characteristics were also analyzed according to the mammographic image (Table 3). In two cases, no mammography had been performed prior to surgery, and in another three cases, the result of the mammography was not available. The cancers associated with casting-type calcifications on the mammogram were significantly more often of ductal type (p = 0.043, Fisher’s exact test), of grade 3 (p < 0.001), ER and PR-negative (p < 0.001) and HER2–2+/3+ (p < 0.001) than the cancers without casting calcifications. The mammographic images revealed no differences in tumor size, lymph node status or LVI. When the predicted outcome based on the conventional prognostic factors was compared with the mammographic image, the 10-year risks of relapse and death were significantly lower in tumors displaying a stellate lesion without calcifications, compared to tumors associated with casting calcifications or if any other mammographic image was present (p < 0.001; Table 3). Similar significant differences were found when the 10-year risks of relapse or mortality were analyzed separately in the screen-detected and non-screen-detected cancers on the basis of the mammographic appearance (data not shown).
Finally, we analyzed whether interval cancers have special mammographic features. The associations between the mammographic findings and the mode of detection are indicated in Table 4. For this analysis, a special group with “absence of any abnormality on the mammogram” was distinguished. The distribution of the mammographic abnormalities was significantly heterogeneous as regards the mode of detection (Table 4). In contrast with 8 of the 48 (16.7%) interval cancers, only 1.6% and 5.7% of the screen-detected and symptomatic cancers, respectively, were mammographically occult.
Discussion
We performed an early analysis of a prospectively collected breast cancer data base. The screen-detected breast tumors were smaller, more frequently lymph node-negative and well differentiated, LVI-negative, and needed less radical surgical and systemic treatments than the symptomatic or interval cancers. The histologic features of the cancers associated with casting calcifications on the mammogram reflected their aggressive nature. The interval cancers occurred at a younger age and were more often mammographically occult than the screen-detected tumors and the cancers diagnosed outside the screening program.
Our findings are in accordance with those studies which demonstrated that the prognostic factors are more favorable in screen-detected than in interval or symptomatic cancers. In numerous studies tumors were obviously smaller, more probably lymph node-negative, [7–11, 13, 14] and better differentiated [9, 11, 13] if screen-detected. Some groups have reported that cancers of a special histological type, such as lobular or tubular cancers, are relatively more prevalent among screen-detected tumors. [9, 11] In contrast, consistent with our data, no difference in histological type was observed among the different groups in the study by Gill et al. [13] LVI was less frequently present in screen-detected than in symptomatic cancers in that study. [13] We also found that LVI was more prevalent in interval or symptomatic cancers than in screen-detected cancers. It has been suggested previously that one indicator of the less aggressive biological behavior of screen-detected cancers is their higher hormone receptor content and the less frequent expression of HER2. Whereas Gill et al. [13] and Klemi et al. [8] reported that more screen-detected than symptomatic cancers were ER-positive, Joensuu et al. [11] did not discern any difference in the expression of ER or HER2 between screen-detected and symptomatic cancers. Similarly, we did not observe any difference in the ER, PR or HER2 status of the tumors as a function of the mode of detection.
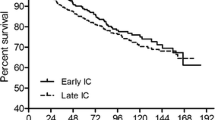
On the basis of the conventional prognostic factors, a striking difference in the predicted 10-year risks of relapse and mortality, was revealed between the screen-detected vs the symptomatic or interval tumors. The predicted outcome was computed by using the software Adjuvant! [22]. Adjuvant! version 6.0 was earlier validated in a large cohort of patients with breast cancer in British Columbia, and excellent matches were found between the predicted and experienced overall survival, breast cancer-specific survival and event-free survival [23]. The cohort in that validation study included a mixed patient population comprising both screen-detected and symptomatic cancer cases. Although our early analysis does not provide patient follow-up data, the computed 10-year risks of relapse and death probably afford a realistic insight concerning the outcome depending on the mode of detection in our patients. These data accord well with the important findings of a good number of studies [7–14], and notably the superior outcome of screen-detected breast cancers as compared with their symptomatic counterparts. Moreover, the analyses by Joensuu et al. [11] and Gill et al. [13] suggest that screening-detection itself is an independent favorable prognostic factor that should be taken into consideration when the adjuvant therapy is to be specified.
Among screen-detected cancers less radical surgical interventions were needed, and less frequent chemotherapy was utilized, as a consequence of the earlier stage of these cancers. However, the hormone therapy requirements did not differ between the groups as concerns the mode of detection. This is a consequence of the similar distributions of the hormone receptor-positive tumors in the different groups, and the frequent use of endocrine therapy even in the early tumors, with the aim of the prevention of distant metastases, local relapses or metachronous second breast cancers.
Interval cancers are detected from the symptoms in the interval between scheduled screening episodes. A failure to detect breast cancer during screening depends on the testing procedure, the interpretation by the radiologist, and the patient and tumor characteristics. A biennial screening interval, a younger age [24-26] and increased breast density [27] favor detection failure. More importantly, the nature of interval cancers may influence their detection. Interval cancers have been demonstrated to occur more often in younger women, and to exhibit a higher proliferation rate, a lower ER expression and higher HER2 expression [24–26]. In our series, the interval cancers were significantly different from the screen-detected cancers, and similar to the symptomatic cancers, as regards the tumor size, the lymph node status, the presence of LVI and the grade, but the differences in histological type, and ER/PR or HER2 status did not reach the level of statistical significance. This latter inconsistency with the literature data may be explained by the relatively low number of cases in our study. We found that a significant proportion of the interval cancers were mammographically occult even at the time of diagnosis. These tumors belong among a special subtype of interval cancers known as occult cancers [28].
In Hungary, the national mammographic breast-screening program was introduced in 2001. Women are invited biennially into one or other of the 43 screening centers for double-view bilateral mammography. The quality indicators of the screening closely match the European guidelines, with the exception of the participation rate, which is around 40%. However, the proportion of women regularly screened for breast cancer is more than 60% as a result of the contribution of opportunistic screening. The mixed population in our study, the close to equal number of screened and non-screened patients is a good indication of the low participation rate.
For elaboration of the appropriate adjuvant therapy, it is mandatory to use the maximum extent of information available on the disease. The prognostic indicators reflect the stage of the cancer and the degree of its aggressiveness. Besides the classical prognostic factors (tumor size, lymph node status, grade, the presence or absence of LVI, and the expressions of the hormone receptors and HER2), however, other specific indicators for a better identification of the high-risk cases are needed. The mammographic appearance of the cancer has recently been suggested as a prognostic factor [15–20, 29]. Among cancers measuring <15 mm and detected by mammographic screening, the presence of casting-type calcifications has been demonstrated to involve a significantly (nine-fold) higher risk of death as compared with cancers not associated with this mammographic abnormality. [16] The risk of relapse or mortality in high-risk breast cancer patients was earlier found to be about threefold if the tumor was associated with casting calcifications on the mammogram. [20] In contrast, a highly favorable prognosis was experienced in small breast cancers appearing as stellate lesions on the mammogram. [16, 18] Although our analysis—due to the lack of patient follow-up data—did not comprise the study of mammographic appearance as a new prognostic factor, we analyzed whether the conventional prognostic factors differed between tumors with different mammographic features. While the tumor size, the nodal status and the presence of LVI did not differ significantly in the groups with different mammographic appearances, the grade 3 phenotype, the ER/PR negativity and the HER2 positivity were typical for the tumors associated with casting-type calcifications. This finding is in accordance with the data of other authors [29] and our own previous results. [20] With the aim of analyzing whether the risks of relapse and mortality as predicted with the software Adjuvant! indicated a significant difference between the prognosis of tumors with or without casting-type calcifications, we compared these via the mammographic images of the tumors. Despite the fact that the tumor size and the lymph node status did not differ significantly in the groups with different mammographic appearances, a significantly poorer outcome was computed for the cancers associated with the casting calcifications. Thus, this mammographic feature is indicative of aggressive tumor behavior and should serve as a warning sign. In contrast, the outcome seems to be the most favorable for tumors which give the image of a spiculated tumor mass on the mammogram.
In conclusion, our findings reveal that screen-detected cancers have a more favorable prognosis and need less oncological treatment than do tumors detected outside mammographic service screening. The mammographic appearance of a tumor reflects its biological behavior, and should be considered when the management is to be optimized.
References
Tabar L, Fagerberg G, Duffy SW et al. (1989) The Swedish two-county trial of mammographic screening for breast cancer: recent results and calculation of benefit. J Epidemiol Community Health 43:107–114
Tabar L, Yeng M-F, Vitak B et al. (2003) Mammography service screening and mortality in breast cancer patients: 20-year follow-up before and after introduction of screening. Lancet 361:1405–1410
The Swedish Organised Service Screening Evaluation Group (2006) Reduction of breast cancer mortality from organised service screening with mammography: 1. Further confirmation with extended data. Cancer Epidemiol Biomarkers Prev 15:45–51
Miller AB, Baines C, To T et al. (1992) Canadian national breast screening study. 1. Breast cancer detection and death rates among women aged 40 to 49 years. CMAJ 147:1459–1476
Kerlikowske K, Grady D, Rubin SM et al. (1995) Efficacy of screening mammography. A meta-analysis. JAMA 273:149–154
Cronin KA, Feuer EJ, Clarke LD, et al. (2006) Impact of adjuvant therapy and mammography on U.S. mortality from 1975 to 2000. Comparison of mortality results from the CISNET breast cancer base case analysis. J Natl Cancer Inst 36:112–121
Moody-Ayers SY, Wells CK, Feinstein AR (2000) ”Benign” tumors and ”early detection” in mammography-screened patients of a natural cohort with breast cancer. Arch Intern Med 160:1109–1115
Klemi PJ, Joensuu H, Tikkanen S et al. (1992) Aggressiveness of breast cancers found with and without screening. Br Med J 304:467–469
Klemi PJ, Parvinen I, Pylkkanen L et al. (2003) Significant improvement in breast cancer survival through population-based mammography screening. Breast 12:308–313
Anttinen J, Kautiainen H, Kuopo T (2006) Role of mammography screening as a predictor of survival in postmenopausal breast cancer patients. Br J Cancer 94:147–151
Joensuu H, Lehtimäki T, Holli K et al. (2004) Risk for distant recurrence of breast cancer detected by mammography screening or other methods. JAMA 292:1064–1073
Shen Y, Yang Y, Inoues LYT et al. (2005) Role of detection method in predicting breast cancer survival: Analysis of randomized screening trials. J Natl Cancer Inst 97:1195–1203
Gill PG, Farshid G, Luke CG et al. (2005) Detection by screening mammography is a powerful independent predictor of survival in women diagnosed with breast cancer. Breast 13:15–22
Ernst MF, Voogd AC, Goebergh JWW et al. (2004) Breast carcinoma diagnosis, treatment, and prognosis before and after the introduction of mass mammographic screening. Cancer 100:1337–1344
Tabar L, Dean PB, Kaufman CS et al. (2000) A new era in the diagnosis of breast cancer. Surg Oncol Clinics NA 9:233–277
Tabar L, Chen TH, Yen AM, et al. (2004) Mammographic tumor features can predict long-term outcomes reliably in women with 1–14-mm invasive breast carcinoma. Cancer 101:1745–1759
Thurfjell E, Thurfjell MG, Lindgren A (2001) Mammographic finding as predictor of survival in 1–9 mm invasive breast cancers. Worse prognosis for cases presenting as calcifications alone. Breast Cancer Res Treat 67:177–180
Alexander MC, Yankaskas BC, Biesemier KW (2006) Association of stellate mammographic pattern with survival in small invasive breast tumors. Am J Roentgenol 187:29–73
Peacock C, Given-Wilson RM, Duffy SW (2004) Mammographic casting-type calcification associated with small screen-detected invasive breast cancers: is this a reliable prognostic indicator? Clin Radiol 59:165–170
Pálka I, Ormándi K, Gaál S et al. (in press) Casting-type calcifications on the mammogram indicate a higher probability of early relapse and death among operable high-risk breast cancer patients. Acta Oncol
Perry NM (2001) Quality assurance in the diagnosis of breast disease. EUSOMA Working Party. Eur J Cancer 37:159–172
Ravdin PM, Siminoff LA, Davis GJ et al. (2001) Computer program to assist in making decisions about adjuvant therapy for women with early breast cancer. J Clin Oncol 19:980–991
Olivotto IA, Bajdik CD, Ravdin PM, et al. (2005) Population-based validation of the prognostic model ADJUVANT! for early breast cancer. J Clin Oncol 23:2716–2725
Porter PJ, El-Bastawissi AZ, Mandelson MT et al. (1999) Breast tumor characteristics as predictors of mammographic detection: Comparison of interval- and screen-detected cancers. J Natl Cancer Inst 91:2020–2028
Gilliland FD, Joste N, Stauber PM et al. (2000) Biologic characteristics of interval and screen-detected breast cancers. J Natl Cancer Inst 92:743–749
Crosier M, Scott D, Wilson RG et al. (1999) Differences in Ki67 and c-erbB2 expression between screen-detected and true interval breast cancers. Clin Cancer Res 5:2682–2688
Porter GJ, Evans AJ, Cornford EJ et al. (2007) Influence of mammographic parenchymal pattern in screen-detected and interval invasive breast cancers on pathologic features, mammographic features, and patient survival. Am J Roentgenol 188:676–683
Porter GJ, Evans AJ, Burrell HC et al. (2007) NHSBSP type 1 interval cancers: a scientifically valid grouping? Clin Radiol 62:262–267
Zunzunegui RG, Chung MA, Oruwari J et al. (2003) Casting-type calcifications with invasion and high-grade ductal carcinoma in situ. Arch Surg 138:537–540
Acknowledgements
The excellent technical assistance of Ms. Julianna Harkai and Ms. Zsuzsanna Hegedűs is gratefully acknowledged.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pálka, I., Kelemen, G., Ormándi, K. et al. Tumor Characteristics in Screen-Detected and Symptomatic Breast Cancers. Pathol. Oncol. Res. 14, 161–167 (2008). https://doi.org/10.1007/s12253-008-9010-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12253-008-9010-7