Abstract
Background
Several studies from other countries have reported that patients with screen-detected breast cancer have better survival than those with symptomatic breast cancer. However, no such comparison has been performed in Japan. Therefore, we aimed to compare the clinicopathological characteristics and survival rates between symptomatic and screen-detected breast cancer in Japanese women.
Methods
From January 2000 to December 2004, 977 and 182 women with symptomatic or screen-detected breast cancer, respectively, underwent surgery at a single Japanese hospital. We retrospectively reviewed these patients’ clinicopathological data. Likelihood of death was estimated using the Kaplan–Meier method and the log-rank test. Multivariate analysis including mode of detection, tumor size, lymph node status, hormone receptor status, and adjuvant therapy administration was performed using the Cox proportional hazards model.
Results
Screen-detected breast cancer was associated with increased rate of breast-conserving surgery, non-invasive carcinoma, smaller tumor size, decreased lymph node involvement, increased hormone receptor positivity, and decreased adjuvant chemotherapy administration. Compared to women with symptomatic tumors, those with screen-detected tumors had improved overall and breast cancer-specific survival rates. Factors associated with survival in univariate analysis were screen detection, tumor size, lymph node status, progesterone receptor status, and adjuvant chemotherapy administration.
Conclusions
Breast cancer screening in Japanese women has led to increases in the rates of breast-conserving surgery, hormone receptor positivity, and survival rates along with reductions in axillary lymph node dissection and adjuvant chemotherapy administration.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer is one of the most common cancers in the world. In Japanese women, the age-standardized incidence of breast cancer is the highest of all cancers, and continues to increase rapidly [1]. Breast cancer screening by clinical breast examination (CBE) was introduced in 1987 for Japanese women aged >30 years in the absence of any evidence of its effectiveness [2]. Breast cancer screening combining mammography (MMG) with CBE was introduced in 2000 for Japanese women aged >50 years, and in 2004 for those aged >40 years. From 2000 to 2004, breast cancer screening involved only CBE alone or MMG with CBE. The institution of breast cancer screening using MMG was based mainly on data obtained from randomized controlled trials performed in Western countries [3].
Several studies from other countries have shown that screen-detected cancers are generally smaller in size, more frequently in situ tumors, better differentiated, less frequently associated with lymph node metastasis, and often detected at an earlier stage than symptomatic breast cancers found by patients themselves [4–8]. Therefore, patients with screen-detected breast cancer have better survival than those with symptomatic breast cancer. However, since the introduction of MMG screening in Japan, no study has compared the characteristics between symptomatic and screen-detected breast cancer. Therefore, in this study, we analyzed the clinicopathological characteristics and survival rates of symptomatic and screen-detected breast cancer in Japanese women.
Patients and methods
Patients
Women who were treated for breast cancer in the Department of Breast and Endocrine Surgery at Kanagawa Cancer Center Hospital (KCCH), Yokohama, Japan, from January 2000 through December 2004, were evaluated. Ultimately, 1159 patients with invasive carcinoma or in situ lesions were included in this study. We retrospectively reviewed these patients’ clinicopathological characteristics, including menopausal status, tumor size, lymph node status, histology, and hormone receptor status; treatment modalities, including type of operation, chemotherapy administration, and hormone therapy; breast cancer-specific survival (BCSS) status; and overall survival (OS) status. Pretreatment clinical tumor size and lymph node status were used when analyzing tumor size and lymph node status in patients who received neoadjuvant chemotherapy. Immunostaining for estrogen receptor (ER) and progesterone receptor (PgR) was performed; the cutoff used to distinguish positive from negative receptor status was ≥10 % ER- or PgR-positive tumor cells.
The Ethics Committee of KCCH approved the protocol of this study, and all study participants provided informed consent.
Methods of detection
Data regarding method of detection were identified by medical record review. Patients were classified into one of two groups: 182 were defined as having screen-detected breast cancer, and 977 were defined as having symptomatic breast cancer. Screen-detected breast cancer was defined as a tumor detected by population-based or opportunistic screening. The two screenings in this study involved only CBE alone or MMG with CBE.
Follow-up
Follow-up was performed using the KCCH Cancer Registry until March 31, 2015. Active follow-up was conducted by accessing hospital visit records, resident registration cards, and permanent domicile data. During the study period, no subject was lost to follow-up.
Endpoints
The endpoints of our analysis were all-cause and breast cancer-specific death according to the International Classification of Disease for Oncology, Tenth Edition. Survival time was calculated for each patient from the date of surgery to the date of death or the end of follow-up (March 31, 2015).
Statistical analysis
Data were analyzed using SPSS version 20 (SPSS Inc., Chicago, IL, USA). Independent t tests and Chi-square tests were used to compare clinicopathological characteristics between the two groups. The Kaplan–Meier method was used to determine OS and BCSS rates, while survival curves were compared using log-rank tests. Cox regression analysis was used to yield relative hazards of multiple variables for all-cause or breast cancer-specific death. Variables analyzed included method of tumor detection, tumor size, lymph node status, ER and PgR status, adjuvant chemotherapy administration, and hormone therapy. The 95 % confidence intervals (CIs) of these characteristics were used. All P values are two tailed, and values of <0.05 were considered statistically significant.
Results
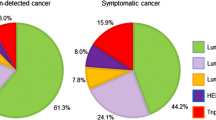
The clinical and pathologic data of 1159 patients with breast cancer were analyzed, including 977 patients (84 %) with symptomatic tumors, and 182 (26 %) with screen-detected tumors (Table 1). Compared to symptomatic breast cancer, screen-detected breast cancer was associated with higher rate of breast-conserving surgery (75 vs. 51 %), non-invasive carcinoma (20 vs. 6 %), smaller tumor size (≤20 mm, 68 vs. 40 %), decreased lymph node involvement (19 vs. 42 %), increased hormone receptor positivity (ER, 73 vs. 62 %; PgR, 60 vs. 47 %), and decreased adjuvant chemotherapy administration (30 vs. 61 %). These differences were significant.
According to the log-rank test, women with screen-detected tumors had improved OS and BCSS rates compared to those with symptomatic tumors (10-year OS, P = 0.01; 10-year BCSS, P = 0.012) (Fig. 1). Similarly, in women with invasive carcinoma, patients with screen-detected tumors had improved OS and BCSS rates compared to those with symptomatic tumors (10-year OS, P = 0.01; 10-year BCSS, P = 0.015) (Fig. 2).
Factors associated with improved survival in univariate analysis were screen detection, tumor size, lymph node status, PgR positivity, and adjuvant chemotherapy administration (Table 2). However, in multivariate analysis using the Cox proportional hazards model, the effect of screen detection on survival disappeared after adjusting for tumor size, lymph node status, PgR status, and adjuvant chemotherapy administration (OS: hazard ratio HR, 1.546; 95 % CI, 0.956–2.498; P = 0.075; BCSS: HR, 1.32; 95 % CI, 0.725–2.406; P = 0.364). Only tumor size and lymph node status remained as independent prognostic factors for OS and BCSS, while PgR status remained as an independent prognostic factor for BCSS (Table 3).
Discussion
We found that in Japanese women, screen-detected cancers were smaller in diameter, less likely to have lymph node involvement, and more likely to be ductal carcinoma in situ compared to symptomatic cancers; these findings are consistent with those of previous studies from other countries [3, 9–12]. These less aggressive pathologic characteristics of screen-detected cancer are associated with increased rate of breast-conserving surgery, avoidance of axillary lymph node dissection, and decreased adjuvant chemotherapy administration.
With these favorable clinicopathological features, women with screen-detected breast cancer benefited from improved OS and BCSS compared to women with symptomatic breast cancer. In previous studies [11–14], increments in survival could be explained by a stage shift—a reduction of patients with advanced-stage cancer in the population. However, a stage shift, which is one of the indicators determining the effect of screening, cannot sufficiently explain the improved prognosis of patients with screen-detected tumors. Wishart et al. [15] reported that although the majority of the improved survival from screen detection is due to a shift in the Nottingham Prognostic Index [16]—a prognostic tool based on tumor size, grade, and lymph node status—the residual impact on survival improvement is small but significant. This improvement can be explained by differences in tumor biology. In previous studies, screen-detected tumors have been more frequently classified as luminal A subtype compared to symptomatic cancers [7]. Breast cancer of luminal A subtype has a better prognosis than other subtypes, including luminal B, human epidermal growth factor receptor 2 (Her2), and triple-negative [17]. Screen-detected luminal A subtype breast cancer has a good prognosis compared to symptomatic cancer. On the other hand, with the other subtypes, the prognosis of screen-detected cancer is no different from that of symptomatic cancer [7, 8]. In this study, we could not evaluate the subtype of breast cancer due to the absence of immunostaining for Her2.
In recent years, we have recognized the need to evaluate the effectiveness of breast cancer screening based on both its benefits and harms [3, 18–21]. In 2009, the US Preventive Services Task Force [3, 21] reported their updated guidelines for screening MMG. They comprehensively assessed the efficacy of breast cancer screening in terms of the net benefit, which is the sum of benefits (mortality reduction) and harms (radiation exposure, pain, anxiety, overdiagnosis, and false-negative/false-positive results). In low-grade ductal carcinoma in situ, there is a possibility of overdiagnosis.
A major limitation of this study is that in most cases, Her2 and Ki-67 positivity was not evaluated and nuclear grading was not done. These tests were not routinely performed at our institution from 2000 to 2004. A second limitation of this study is that there were no data on the rate of the detection method used, i.e., the proportion of MMG with CBE versus CBE alone.
Conclusion
This study showed that early detection with breast cancer screening in Japan has led to increases in the rates of breast-conserving surgery, hormone receptor positivity, and survival rates along with reductions in axillary lymph node dissection and adjuvant chemotherapy administration.
Change history
10 January 2018
In the original publication of this article, Table 1 was published incorrectly with rows out of order under “Distant metastasis (n, %)”.
References
Matsuda T, Marugame T, Kamo K, Katanoda K, Ajiki W, Sobue T. Cancer incidence and incidence rates in Japan in 2006: based on data from 15 population-based cancer registries in the monitoring of cancer incidence in Japan (MCIJ) project. Jpn J Clin Oncol. 2012;42:139–47.
Kanemura S, Tsuji I, Ohuchi N, Takei H, Yokoe T, Koibuchi Y, et al. A case control study on the effectiveness of breast cancer screening by clinical breast examination in Japan. Jpn J Cancer Res. 1999;90:607–13.
Nelson HD, Tyne K, Naik A, Bougatsos C, Chan BK, Humphrey L. Screening for breast cancer: an update for the U.S. Preventive Services Task Force. Ann Intern Med. 2009;151:727–37, W237–42.
Joensuu H, Lehtimäaki T, Holli K, Elomaa L, Turpeenniemi-Hujanen T, Kataja V, et al. Risk for distant recurrence of breast cancer detected by mammography screening or other methods. JAMA. 2004;292:1064–73.
Shen Y, Yang Y, Inoue LY, Munsell MF, Miller AB, Berry DA. Role of detection method in predicting breast cancer survival: analysis of randomized screening trials. J Natl Cancer Inst. 2005;97:1195–203.
Kalager M, Haldorsen T, Bretthauer M, Hoff G, Thoresen SO, Adami HO. Improved breast cancer survival following introduction of an organized mammography screening program among both screened and unscreened women: a population-based cohort study. Breast Cancer Res. 2009;11:R44.
Kim J, Lee S, Bae S, Choi MY, Lee J, Jung SP, et al. Comparison between screen-detected and symptomatic breast cancers according to molecular subtypes. Breast Cancer Res Treat. 2012;131:527–40.
Crispo A, Barba M, D’Aiuto G, De Laurentiis M, Grimaldi M, Rinaldo M, et al. Molecular profiles of screen detected vs. symptomatic breast cancer and their impact on survival: results from a clinical series. BMC Cancer. 2013;13:15.
Anderson TJ, Lamb J, Donnan P, Alexander FE, Huggins A, Muir BB, et al. Comparative pathology of breast cancer in a randomised trial of screening. Br J Cancer. 1991;64:108–13.
Chu KC, Smart CR, Tarone RE. Analysis of breast cancer mortality and stage distribution by age for the Health Insurance Plan clinical trial. J Natl Cancer Inst. 1988;80:1125–32.
Cowan WK, Angus B, Henry J, Corbett IP, Reid WA, Horne CH. Immunohistochemical and other features of breast carcinomas presenting clinically compared with those detected by cancer screening. Br J Cancer. 1991;64:780–4.
Ernst MF, Roukema JA, Coebergh JW, Repelaer van Driel OJ, van Beek MW, van der Sangen MJ, et al. Breast cancers found by screening: earlier detection, lower malignant potential or both? Breast Cancer Res Treat. 2002;76:19–25.
Allgood PC, Duffy SW, Kearins O, O’Sullivan E, Tappenden N, Wallis MG, et al. Explaining the difference in prognosis between screen-detected and symptomatic breast cancers. Br J Cancer. 2011;104:1680–5.
Paci E, Ponti A, Zappa M, Patriarca S, Falini P, Delmastro G, et al. Early diagnosis, not differential treatment, explains better survival in service screening. Eur J Cancer. 2005;41:2728–34.
Wishart GC, Greenberg DC, Britton PD, Chou P, Brown CH, Purushotham AD, et al. Screen-detected vs. symptomatic breast cancer: is improved survival due to stage migration alone? Br J Cancer. 2008;98:1741–4.
Todd JH, Dowle C, Williams MR, Elston CW, Ellis IO, Hinton CP, et al. Confirmation of a prognostic index in primary breast cancer. Br J Cancer. 1987;56:489–92.
Parker JS, Mullins M, Cheang MC, Leung S, Voduc D, Vickery T, et al. Supervised risk predictor of breast cancer based on intrinsic subtypes. J Clin Oncol. 2009;27:1160–7.
Barrett B, McKenna P. Communicating benefits and risks of screening for prostate, colon, and breast cancer. Fam Med. 2011;43:248–53.
Brodersen J, Jørgensen KJ, Gøtzsche PC. The benefits and harms of screening for cancer with a focus on breast screening. Pol Arch Med Wewn. 2010;120:89–94.
U.S. Preventive Services Task Force. Screening for breast cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2009;151:716–26, W236.
Hendrick RE, Helvie MA. United States Preventive Services Task Force screening mammography recommendations: science ignored. AJR Am J Roentgenol. 2011;196:W112–6.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there are no conflicts of interest associated with this study, and that the trial was conducted independently.
Additional information
A correction to this article is available online at https://doi.org/10.1007/s12282-018-0832-1.
About this article
Cite this article
Inari, H., Shimizu, S., Suganuma, N. et al. A comparison of clinicopathological characteristics and long-term survival outcomes between symptomatic and screen-detected breast cancer in Japanese women. Breast Cancer 24, 98–103 (2017). https://doi.org/10.1007/s12282-016-0678-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12282-016-0678-3