Abstract
Purpose
Delivery of accurate doses from dry powder inhalers (DPI) involves many process variables which must be adjusted to ensure patient compliance and optimum therapy. Some of the process variables include: speed of inhalation (flow rate), assumed lung volume of patients, number and duration of inhalations.
Method
Data mining technology based on artificial neural networks and genetic algorithms were used to model the in vitro inhalation process, predict and optimize bioavailability from the inhaled doses.
Results
The delivery of terbutaline doses from Bricanyl Turbuhaler® was modeled and optimized using artificial neural network modeling and optimization software. Highly significant models (p < 0.00001) with minimum root mean squared error and high predictability: R 2 > 81 % and 91 % for the in vitro and the in vivo models were developed, respectively. The optimized models demonstrated that an optimum emitted dose (>76 %) could be obtained if the dose was withdrawn as two inhalations with inhalation volume 4 L and flow rate 60 L/min within 4 s. The same independent variables in addition to % terbutaline emitted were modeled and optimized for % drug excreted in urine. The latter model demonstrated that optimum bioavailability (79.50 %) could be obtained from Bricanyl Turbuhaler® emitting 80–87.50 % terbutaline at a flow rate of 58–60 L/min using two inhalations irrespective of subject forced expiratory volume in 1 s (FEV1) or the individual lung capacity.
Conclusion
Optimized in vitro/in vivo inhalation processes using data mining models can offer rapid solutions for dose variability problems and maximize the bioavailability of drugs from DPIs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
This study addresses the multivariable process of inhalation using dry powder inhalers. One of the dry powder inhalers, the Turbuhaler is known to have a high resistance during inhalation [1]. Dose emission from all dry powder inhaler (DPI) devices, is also dependent on the flow rate [2, 3]. The variation of the emitted dose is a direct cause of unpredicted clinical response or side effects. Patients with chronic obstructive pulmonary disease (COPD) can usually inhale a maximum of approximately 2 L as inhalation volume. Some other patients may not be able to inhale in a sufficient power or flow rate to produce the required pressure drop (4 kPa) necessary to withdraw the dose from the inhaler [4]. The Turbuhaler is a multidose reservoir DPI. It was introduced in 1988, designed to deliver 500 μg per dose of terbutaline sulfate devoid of carrier, and then it was used for other drugs.
It does not require synchronization of inhalation and actuation as in metered dose inhalers (MDIs), also, it can deliver large doses and suitable for drugs which are unstable in solution form, easy to use and safe to the environment. However, there is somewhat high variability in the delivered dose. It is the most frequently prescribed DPI that produces good deposition of drug in the lungs provided that a sufficient inspiratory flow has been achieved by the patients (i.e., 60 L min−1). Hence, the particle size generated depends on the patients’ inspiratory flow rate. It is not easy to deliver the complete dose due to its high intrinsic resistance. Therefore, patients must initially inhale in a strong way through the Turbuhaler and keep the rate during the inhalation maneuver to ensure de-agglomeration of drug particles and hence effective drug deposition [5].
Patients with severe airflow obstruction may find it difficult to use the Turbuhaler as the necessary inspiration flow may not be supported by the patient’s power of inhalation. Hence, patients utilizing the Turbuhaler must exert higher inspiratory effort for achieving the required inspiratory flow (e.g., 60 L/min) [6]. There is also a direct effect of the inspiratory flow through the Turbuhaler on the particle size distribution of drugs contained in it. This factor could deposit some of the particles in the upper respiratory regions rather than deeply in the lung. Another factor is that the internal volume of the Turbuhaler is relatively small compared to high ability to breath and it may happen that all the powder drawn from the cavity before peak inspiratory flow has been achieved [7]. There are three key elements for successful use of inhaler in lung delivery including: (1) patient compliance; (2) presence of fine particle distribution and its dependency on inspiratory flow; and (3) the clinical effect. A comparative study between terbutaline administered using a Turbuhaler and a halogenated hydrocarbon assisted inhaler in conjunction with a spacer device (Nebuhaler®) was performed in 15 COPD patients with regard to forced expiratory volume in 1 s (FEV1), forced expiratory capacity (FVC), residual volume (RV), and specific conductance (s-Gaw). The study proved that similar results were obtained from both devices [8]. This indicates the importance of turbuhalers in giving the required therapeutic goals without creating environmental hazards. Few research papers have addressed modeling and optimization of DPI inhalation process or the device-related variables, patient characteristics and formulation attributes affecting its complex domain.
The fact that increasing the number of fine particles in the carrier can help improve the aerosolization of the active pharmaceutical ingredient (API) [9] was confirmed in a study performed to evaluate the effect of various size fractions of lactose on the performance of dry powder inhaled (DPI) products using experimental design and multivariate analysis [10]. One study aimed at prediction of particles’ aerodynamic size, shape, density and their effects on sedimentation rate was used for improving pulmonary drug delivery from dry powder inhalers [11]. Other studies addressed modeling of deposition pattern of aerosolized particles into human lung using mathematical models [12] or artificial neural networks (ANNs) [13].
Most of the modeling experiments focus on the description of deposition characteristics of inhaled drugs in the respiratory system. These are employed either by the application of lung deposition models for the determination of the amount and/or the location of deposited dose or by using computational fluid dynamics techniques to describe the deposition patterns [14]. Artificial neural networks are considered a powerful tool used for modeling and optimization for multivariable and complex domain data [15]. ANNs offer numerous advantages to conventional mathematical and statistical modeling methodologies, including their ability to deal with non-linear data and no need for prior establishment of equations to describe relationship between input and output variables [16]. In addition, ANNs can be used for historical data and models generated can be updated with new experiments [17]. ANNs also enables special operations such as “what-if” predictions and optimizations [18]. This technology was also applied for building predictive models relating in vitro aerosol characteristics to pulmonary bioavailability of inhaled salbutamol sulfate [19, 20].
The design of inhalation devices must fulfill different patient needs. Patients having no airflow obstruction should get lower doses than those with obstruction, while young children need different delivery systems from adults. Therefore, the inhalation device should be evaluated based on its ability to deliver systematically uniform doses and maximize the inhaled drug bioavailability [21]. In this research, modeling of the in vitro performance of Bricanyl Turbuhaler® was addressed. Apart from the type of DPI device used or the aerodynamic parameters of the formulation, this study focused on testing other variables directly related to using the DPI device for effective inhalation including: artificial lung volume, airflow rate, inhalation maneuver (slow/fast, one/two inhalation). The modeling aimed at linking these independent variables to percentage emitted dose of terbutaline from a Turbuhaler and to pulmonary bioavailability. Data records from artificial experiments, human volunteers, and COPD patients were used for modeling using artificial neural networks and neurofuzzy logic based data mining technology.
Materials and Methods
Materials
Commercial terbutaline dry powder inhalers with capacities 500 μg (Bricanyl Turbohaler®, AstraZeneca, UK) were used in the study with DPI sampling apparatus purchased from Copley (Copley Scientific Ltd, UK). The HPLC-grade acetonitrile (Fisher Scientific, UK), bamethane hemisulfate (Sigma, UK), and orthophosphoric acid (The Egyptian Bureau of import, Cairo, Egypt) were used for the assay study.
In vitro Terbutaline Emitted Dose Studies
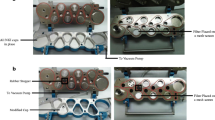
The in vitro-emitted doses of terbutaline from Bricanyl Turbuhaler® with a nominal dose of 500 μg terbutaline sulfate per puff (AstraZeneca, UK) were evaluated using a DPI sampling apparatus with a critical flow controller model TPK (Copley Scientific Ltd, UK). Total emitted dose of terbutaline [22] with volumes of 2 and 4 L with flow rates of 10, 20, 30, 40, 50, and 60 L/min were tested. The flow was measured by an electronic digital flow meter (MKS Instruments, USA). Parafilm M laboratory film (Pechiney Plastic Packaging, USA) was used to seal the apparatus. Inhalation of the dose was performed on one and two inhalation basis. The duration of the inhalation process lasted for variable times including: 24, 12, 8, 6, 4.8, and 4 s respectively for 4 L inhalation volume and 12, 6, 4, 3, 2.4, and 2 s respectively for 2 L inhalation volume (see sample data records in Table 1).
The percentage drug deposited in the plastic dose sampling apparatus and the final filter was determined using high-performance liquid chromatography (HPLC) analysis. The HPLC method used was a Water Spherisorb C18, ODS1 column through which a mobile phase of 5 mM potassium dihydrogen orthophosphate-acetonitrile (75:25), adjusted to pH 2.5 with orthophosphoric acid [2]. The mobile phase was pumped at a rate of 1 ml/min. The spectrofluorometric detector (RF-551, Shimadzu, Japan) was set at an excitation/emission of 267/313 nm. Bamethane hemisulfate (Sigma, UK) was used as the internal standard. The limit of detection was 10.9 μg/L and the lower limit of quantification was 33.1 μg/L. The total dose emitted as percentage of label claim was assigned as the output property.
In vivo Absorbed and Excreted Dose Studies
Terbutaline absorbed and excreted in urine for 24 h, was tested using 12 human COPD patients and 12 healthy volunteers following inhalation of 1,000 μg terbutaline sulfate doses (2 puffs of 500 μg terbutaline sulfate per puff). The testing process variables addressed in the in vitro study were included as input variables (n = 6) into the modeling step of the in vivo study. These included: average percentage forced expiratory volume in 1 s (% FEV1, 96 % for volunteers, and 46 % for patients), pulmonary volume (2 and 4 L), flow rates of 30 and 60 L/min, one and two inhalations, duration of inhalation (2, 4, and 8 s) and the percentage in vitro-emitted dose. The percentage Terbutaline excreted after 24 h was modeled as the output property (see sample data records in Table 2).
The study was a four-way cross-over on four different days with 7 days washout period (one inhalation fast flow, one inhalation slow flow, two inhalations fast flow, two inhalations slow flow), with a total dose of 1,000 μg of terbutaline sulfate on each occasion. An ethical approval was obtained from the University of Beni Suef for the health subjects study and all volunteers gave signed informed consent. Twelve healthy non-smoking volunteers (six males and six females), older than 18 years with a mean FEV1 > 90 % of predicted, agreed to inhale two doses through two Bricanyl Turbuhalers® (500 μg, AstraZeneca, UK), using slow and fast inhalation flows. A local hospital research ethics committee approval was obtained for the patients study. COPD patients, with FEV1 less than 50 % of predicted at screening, were asked to take part in this study. If they accepted to take part in the study, consent was obtained from each patient.
If at any time the patient requested to quit the study then they were withdrawn together with all their data and their samples were disposed. For each patient, the FEV1 was measured on the study day before taking the dose resulting in four FEV1 for each patient. The healthy subjects and the patients were trained how to inhale using a slow inhalation flow (30 L/min) and also a fast inhalation flow (60 L/min) with aid of the In-Check Dial. They also, received training on how to use the Turbuhaler. Each subject inhaled two doses from two separate Bricanyl Turbuhalers® using either a slow or a fast inhalation flow maneuvers at random order. According to the novel urinary terbutaline method [23], immediately before each study dose each subject voided their urine then provided a urine sample 30 min after the start of the first dose and cumulatively collected their urine for 24 h. The volumes of urine samples were measured and assayed for the urinary terbutaline concentration using an HPLC-fluorescence spectrophotometry. Terbutaline was extracted from the urine samples together with bamethane (Sigma, UK) as internal standard using solid phase extraction, Isolute HCX 130 mg 10 ml XL cartridge and Oasis HLB 30 mg cartridge, then injected in the HPLC system. The method used was an ODS 5 mm (4.6 × 250 mm, Zorbax, Phenomenex) C-18 HPLC column with a 4 mm × 3 mm (Phenomenex), C-18 (ODS) guard column. Both were maintained at 30 °C. The mobile phase was acetonitrile-methanol-tetrahydrofurane-ethyl acetate buffer 5:5:5:5:80 % v/v. The buffer was 40 mM phosphate buffer and 27.5 mM sodium dodecyl sulfate with pH 6.75 adjusted using 10 mM KOH. Fluorescence detection set with an excitation/emission of 267/313 nm. The limit of detection (LOD) and lower limit of quantification (LLOQ) for terbutaline was 24.2 and 73.4 μg L −1, respectively [23].
Model Training and Testing of Process Variables
The in vitro inhalation process variables (artificial lung volume, flow rate, number of inhalations and duration of inhalation) and the percentage terbutaline emitted (output) resulted in 240 data records (see Table 1) were used for model training. Modeling and optimization of the data was carried out using ANNs-Genetic algorithm package (INForm V3.6, Intelligensys Ltd., UK) [24]. The software was used as the predictive model-building and optimization tool [25, 26]. The multilayer perceptron (MLP) network embedded into the program was trained on the data to build up the cause-effect relationships as well as relative weights and importance between input variables (inhalation process variables) and output property (percentage emitted). Some data records (10 %) were selected for testing the predictability of the model and another 10 % of the records were kept for model validation (both selected using the Smart selection tool). This smart selection is similar to random selection; however, it automatically excludes records which contain values at the minimum or maximum of a range to keep them for model training.
The in vivo modeling step was applied using 80 records containing the inputs: pulmonary volume, inhalation flow rate, number of inhalations, duration of inhalation, percentage emitted from the Turbuhaler® and percentage terbutaline excreted as the output (see Table 2). Model training, testing and validation were performed in the same way as that mentioned above for the in vitro model. Predictability of trained models were evaluated by the correlation coefficient R square (R 2) values computed automatically during training, testing and validation steps [27] as shown in Tables 3 and 4 respectively. High R 2 values (>78 %) for in vitro model and >90 % for the in vivo model indicated appropriate predictability of the trained models [28]. The formula, from which R 2 values were calculated was derived from ANOVA statistics generated by the modeling software program (see Eq. 1).
Where (y i ) is the individual value of the dependent variable, (y i *) is the predicted value from the model and (y i −) is the mean of the dependent variable. In this formula the numerator represents the sum of squares for the error term (SSE) and the denominator represents the total sum of squares (SST) [29]. The values of R 2 describe how much of the variance of the dependent variable is accounted for in the model. The artificial neural network structure I(4)–H(11)–O(1) was used for in vitro model training (linking inputs and the output property). The structure demonstrated: 4 nodes representing the input layer, 11 nodes in the hidden layer, and 1 node in the output layer) was used for training. The default model training rapid back-propagation algorithm (RPROP) was used for model training [30]. The model transfer function (model activation function) was selected for inputs and outputs as asymmetric sigmoid/linear. The validation step was carried out using the consult mode of the program and during which the model predicts the output property automatically for unseen data based on previously learned cause-effect relationships. The network structure used for the in vivo model was automatically described as I(6)–H(6)–O(1) and the model transfer function was selected as sigmoid/linear. Other training and testing steps were performed in the same way as that mentioned earlier for the in vitro model (% terbutaline emitted). Good models should result in validation correlation R 2 as high as those obtained during model training and testing. The accuracy of generated models for in vitro percentage emitted dose and that generated for percentage terbutaline excreted were evaluated using model R 2 and the root mean squared error (RMSE) values calculated for both training and testing data sets (see Tables 3 and 4). Further evaluations of the models were performed by plotting the actual (experimental) values of both properties (% emitted and percentage excreted) versus their model predicted counterparts. From the plots, linear correlation R 2 values were also calculated (see Figs. 1, 2, 3, and 4).
Optimization of In Vitro-Emitted Dose and In Vivo Excretion Models
After developing of the predictive models for each of percentage terbutaline emitted and excreted, the optimization step was commenced by setting the desired constraints on some process variables and proposing an optimum range for the output property. The desirability function was selected as tent (with preset minimum and maximum for each property) in three separate optimization runs in the model optimization window. The specified minimum and maximum values for the output property (% emitted and % excreted) were assigned to three levels. In the first level, the percentage terbutaline emitted was specified to 65–75 % and the % excreted to be 75–85 %. In the second level, % emitted was specified between 70 and 80 % and the in vivo was set between 80 and 85 %. Finally, in the third level, the in vitro property was set between 75 and 85 % and % excreted to be 85–89.5 %. Three model-optimized solutions were generated (see Tables 5 and 6).
Results and Discussion
Evaluation of Model Training, Testing, and Validation
The model generated for the in vitro experiments, resulted in a good model with high predictability as evidenced by the model training and testing correlation coefficient R 2 values of 83.29 and 78.19 % respectively (see Table 3). Predictability of unseen data (validation records) also demonstrated high R 2 (81 %), indicating a validated model for predicting percentage terbutaline emitted from dry powder inhalers. The RMSE calculated for training and testing data from the in vitro model were found to be 8.01 and 5.62, respectively. The lower RMSE values of test data than those of training suggest high predictive ability and trust ability of the model. The results were also in good agreement with good predictive models mentioned in the literature with high R 2 values, which represent the ability of the model to account for variability in the data [27]. This was also clearly illustrated by high correlation coefficients between actual and predicted % emitted (see Figs. 1 and 2).
The model generated for in vivo percentage terbutaline excreted from 80 records (see Table 4) also demonstrated high predictability power as obtained from model training, testing, and validation R 2 values being 98.06, 99.10, and 91.74 %, respectively. The RMSE values for training and validation testing were found to be 5.99 and 2.94, respectively which also support model trust ability. The above findings were also found to be comparable to similar models generated for salbutamol excreted in urine in 30 min post inhalation as a measure for relative lung bioavailability [19]. In addition to model correlation, R 2, and RMSE values calculated above, the linear regression coefficients (r 2) calculated from actual experimental training and validation data versus predicted values for % terbutaline excreted also support model robustness (see Figs. 3 and 4). Moreover, the calculated p values (probability for significance) from the F-distribution statistics for both models (% terbutaline emitted and % excreted in urine) were very low (p < 0.0001), indicating the significance of the models.
Model Optimization
The developed predictive models for percentage terbutaline emitted from Turbuhaler and the percentage excreted after in vivo inhalation were then tested for optimization of both properties. The optimization stage resulted in three solutions for in vitro percentage emitted (71–76 %) with optimum values for lung volume (3–4 L), flow rate (52–59 L/min) and two inhalations lasting 3.0–4.5 s (see Table 5). Model optimization for percentage terbutaline excreted in urine within 24 h (79.50 %) resulted in optimum values for patient FEV1 (46.00–49.50 %), pulmonary volume (2.4–3.9 L), flow rate through inhaler (58–60 L/min), two number of inhalations lasting for 2.5–4.0 s and % in vitro-emitted dose between 80 and 87.50 % (see Table 6).
The relative importance of each input variable on each of the output properties (% terbutaline emitted and % terbutaline excreted in urine) was demonstrated by the response surface plots. Artificial lung volume was found to have a positive effect on the % terbutaline emitted from the inhaler whilst increasing the inhalation time (2–24 s) resulted in a decrease in % emitted (Fig. 5). The number of inhalations (one to two) was found to have a little effect on the in vitro % emitted from the Turbuhaler (Fig. 6). The inhalation flow rate of 10–30 L/min was found to have a negative effect on % emitted, while from 30 to 60 L/min increased the % emitted (Fig. 7). The improvement of percentage emitted upon increasing the inhalation flow rate was supported by studies previously reported on the use of dry powder inhalers [31]. From these results, it becomes clear that using a large lung volume and average flow rate >30 L/min with relatively fast inhalation maneuver will inevitably provide the maximum % terbutaline emitted from a dry powder inhaler (see Table 5).
The response surfaces obtained from the in vivo model demonstrated that the inhalation flow rate was found to have the largest positive effect on % excreted and the maximum influence was demonstrated at 48–54 L/min (see Fig. 8). The pulmonary volume was found to have little effect on this property which might be due to limited scatter of this independent variable in training data where the maximum and minimum values were 4 and 2 L, respectively. This finding was recently supported by other researches evaluating the flow rate and pulmonary volume [32]. The effect of FEV1 on percentage terbutaline excreted was found to have minor effect on % excreted especially in the patient range (46–66 L) and decreasing effect in the range of healthy subjects. This finding was supported by other studies found in the literature reporting that FEV1 is not a powerful differentiating variable to model pulmonary delivery [33]. The response surface obtained for the number of inhalations indicated that two inhalations are better than one (Fig. 9). The response surface for % terbutaline emitted and inhalation time indicated that above 68.5 % emitted terbutaline, the % excreted was maximized; this finding can be considered as a threshold value for effective DPIs [34]. The inhalation time had no obvious effect on the percentage terbutaline excreted (see Fig. 10).
Although major differences exist between volunteers and COPD patients regarding FEV1 (average values of 46 for patients and 96 for healthy subjects) and pulmonary volumes (2 L for patients and 4 L for healthy volunteers), yet the response surfaces concluded no strong influence of these two variables on % terbutaline excreted. The effect of FEV1 may also be offset by the two inhalation strategies (slow, fast, one and two inhalations) which helped in maximizing the bioavailable fraction regardless of the pulmonary volume or the individuals FEV1. The percentage drug emitted from the Turbuhaler, the flow rate, and the number of inhalations was found to be the prominent variables affecting the drug’s bioavailability from Bricanyl Turuhaler®. These latter variables which control the effective usage of Turbuhalers in delivering the maximum dose were found to be independent of the individual subjects used in this study. This means that the same instructions for proper use of Turbuhalers must be given to all subjects whatever the differences between the lung capacity or FEV1 between patients. The above results indicate that the in vivo model supported the use of two inhalations maneuver with optimum flow rate 50–60 L/min from a Turbuhaler delivering not less than 68.5 % of the dose to maximize the pulmonary bioavailability (79.5 %). The optimized model also suggested that individuals with lung capacity 2 or 4 L (whether healthy or with COPD) inhaling according to the above mentioned instructions will have similar pulmonary drug delivery (see Table 6).
Conclusion
The process of inhalation through dry powder inhalers depends mainly on the ability of the patient to inhale in a special manner in order to inhale a complete dose each time an administration is due. Therefore, proper training of patients on using the inhalers is essential. However, numerous process variables which are device-dependent must be adjusted for maximizing the bioavailability of inhaled dry powdered drugs. Modeling of the inhalation process which is known to be a multivariable and complex domain offers a direct tool for better control and optimization of the process. The developed linear models were found to be successful in demonstrating the importance of using two inhalation modes and flow rates >50 L/min in maximizing the in vitro % terbutaline emitted from Bricanyl Turbohaler®. These optimized variables were also found to be the key elements for improving the bioavailability of the inhaled drug if interpreted into instructions for patients and employed during inhalation.
References
Assi K, Chrystyn H. The different resistance of dry powder inhalers (DPIs). Am J Respir Crit Care Med. 2001;163:A443.
Abdelrahim M, Assi K, Chrystyn H. Dose emission and aerodynamic characterization of the terbutaline sulphate dose emitted from a Turbuhaler at low inhalation flow. Pharm Dev Technol. 2013;18:944–9.
Ross DL, Schultz RK. Effect of inhalation flow rate on the dosing characteristics of dry powder inhaler (DPI) and metered dose inhaler (MDI) products. J Aerosol Med. 1996;9:215–26.
Hawksworth G, James L, Chrystyn H. Characterization of the inspiratory manoeuvre when asthmatics inhale through a Turbohaler pre-and post-counselling in a community pharmacy. Respir Med. 2000;94:501–4.
Virchow JC, Crompton GK, Dal Negro R, Pedersen S, Magnan A, Seidenberg J, et al. Importance of inhaler devices in the management of airway disease. Respir Med. 2008;102:10–9.
Cegla UH. Pressure and inspiratory flow characteristics of dry powder inhalers. Respir Med. 2004;98(1):S22–8.
Everard ML, Devadason SG, Le Souef PN. Flow early in the inspiratory manoeuvre affects the aerosol particle size distribution from a Turbuhaler. Respir Med. 1997;91:624–8.
Formgren H, Sjokvist A, Stahl E, Wiren JE. Terbutaline in COPD comparison between turbuhaler® and chlorofluorocarbon (CFC) inhaler. Lung. 1994;172:271–80.
Richter K. Successful use of DPI systems in asthmatic patients-key parameters. Respir Med. 2004;98(2):S22–7.
Guenette E, Barrett A, Kraus D, Brody R, Harding L, Magee G. Understanding the effect of lactose particle size on the properties of DPI formulations using experimental design. Int J Pharm. 2009;380:80–8.
Crowder T, Rosati J, Schroeter J, Hickey A, Martonen T. Fundamental effects of particle morphology on lung delivery: predictions of Stokes’ law and the particular relevance to dry powder inhaler formulation and development. Pharm Res. 2002;19:239–45.
Martonen T, Katz I. Deposition patterns of polydisperse aerosols within human lungs. J Aerosol Med. 1993;6:251–74.
Nazir J, Barlow DJ, Lawrence MJ, Richardson CJ, Shrubb I. Artificial neural network prediction of aerosol deposition in human lungs. Pharm Res. 2002;19:1130–6.
Balashazy I, Alfoldy B, Molnar AJ, Hofmann W, Szoke I, Kis E. Aerosol drug delivery optimization by computational methods for the characterization of total and regional deposition of therapeutic aerosols in the respiratory system. Curr Comput Aided Drug Des. 2007;3:13–32.
Sun Y, Peng Y, Chen Y, Shukla AJ. Application of artificial neural networks in the design of controlled release drug delivery systems. Adv Drug Deliv Rev. 2003;55:1201–15.
Chen Y, Thosar SS, Forbess RA, Kemper MS, Rubinovitz RL, Shukla AJ. Prediction of drug content and hardness of intact tablets using artificial neural network and near-infrared spectroscopy. Drug Dev Ind Pharm. 2001;27:623–31.
Hussain AS, Yu X, Johnson RD. Application of neural computing in pharmaceutical product development. Pharm Res. 1991;8:1248–52.
Aksu B, Paradkar A, Matas M, Ozer O, Guneri T, York P. Quality by design approach: application of artificial intelligence techniques of tablets manufactured by direct compression. AAPS PharmSciTech. 2010;13:1138–46.
de Matas M, Shao Q, Richardson CH, Chrystyn H. Evaluation of in vitro in vivo correlations for dry powder inhaler delivery using artificial neural networks. Eur J Pharm Sci. 2008;33:80–90.
de Matas M, Shao Q, Silkstone VL, Chrystyn H. Evaluation of an in vitro in vivo correlation for nebulizer delivery using artificial neural networks. J Pharm Sci. 2007;96:3293–303.
O’Riordan TG. Optimizing delivery of inhaled corticosteroids: matching drugs with devices. J Aerosol Med. 2002;15:245–50.
Abdelrahim ME. Emitted dose and lung deposition of inhaled terbutaline from Turbuhaler at different conditions. Respir Med. 2010;104:682–9.
Abdelrahim ME, Assi KH, Chrystyn H. Relative bioavailability of terbutaline to the lung following inhalation, using urinary excretion. Br J Clin Pharmacol. 2011;71:608–10.
Ali AA, Ali AMAH. Optimization of propranolol HCl release kinetics from press coated sustained release tablets. Pharm Dev Technol. 2012; 1–9
Shao Q, Rowe RC, York P. Comparison of neurofuzzy logic and neural networks in modelling experimental data of an immediate release tablet formulation. Eur J Pharm Sci. 2006;28:394–404.
Shao Q, Rowe RC, York P. Comparison of neurofuzzy logic and decision trees in discovering knowledge from experimental data of an immediate release tablet formulation. Eur J Pharm Sci. 2007;31:129–36.
Bourquin J, Schmidli H, van Hoogevest P, Leuenberger H. Advantages of Artificial Neural Networks (ANNs) as alternative modelling technique for data sets showing non-linear relationships using data from a galenical study on a solid dosage form. Eur J Pharm Sci. 1998;7:5–16.
Rowe RC, Colbourn EA. Data mining methods in pharmaceutical formulation, in pharmaceutical data mining. Hoboken: Wiley; 2009. p. 401–21.
Plumb AP, Rowe RC, York P, Brown M. Optimisation of the predictive ability of artificial neural network (ANN) models: a comparison of three ANN programs and four classes of training algorithm. Eur J Pharm Sci. 2005;25:395–405.
Rowe RC, Roberts RJ. Intelligent software for product formulation. Bristol: Taylor & Francis; 1998.
Tarsin W, Assi K, Chrystyn H. In-vitro intra-and inter-inhaler flow rate-dependent dosage emission from a combination of budesonide and eformoterol in a dry powder inhaler. J Aerosol Med. 2004;17:25–32.
Yakubu SI, Assi KH, Chrystyn H. Aerodynamic dose emission characteristics of dry powder inhalers using an Andersen Cascade Impactor with a mixing inlet: the influence of flow and volume. Int J Pharm. 2013;455:213–8.
Niu T, Rogus JJ, Chen C, Wang B, Yang J, Fang Z, et al. Familial aggregation of bronchodilator response: a community-based study. Am J Respir Crit Care Med. 2000;162:1833–7.
Weers J, Ung K, Le J, Rao N, Ament B, Axford G, et al. Dose emission characteristics of placebo PulmoSphere® particles are unaffected by a subject’s inhalation maneuver. J Aerosol Med Pulm Drug Deliv. 2012;26:56–68.
Acknowledgments
A special acknowledgment is directed to Intelligensys Ltd., UK for the renewal of the software (INForm) license during change of computer operating system. Also, the authors acknowledge the help given by the staff of Beni Suef University during completion of the in vivo part of this study.
Ethical Standards
All experiments done in this research on human volunteers and/or patients were performed according to the laws adopted by the ethical research committee of Beni Suef University, Egypt.
Conflict of Interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ali, A.M.A., Abdelrahim, M.E.A. Modeling and Optimization of Terbutaline Emitted from a Dry Powder Inhaler and Influence on Systemic Bioavailability Using Data Mining Technology. J Pharm Innov 9, 38–47 (2014). https://doi.org/10.1007/s12247-014-9171-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12247-014-9171-8