Abstract
This study evaluated the effect of low-molecular weight chitosan on Staphylococcus epidermidis, a common colonizer of joint implants and other prosthetic devices. We have also attempted to elucidate its mechanism of action. Chitosan was found to be effective against both the planktonic and biofilm cells (MIC80 35–40 mg/L; MBIC80 40–150 mg/L), in contrast to the antibiotics erythromycin and tetracycline with no antibiofilm activity (MBIC80 not found). In combination, chitosan had an additive effect with antibiotics on suspension growth of S. epidermidis (FICi 0.7–1.0), and the combinatory action caused a complete inhibition of biofilm metabolic activity in some cases. In addition, chitosan caused rapid cellular damage and enhanced antihaemolytic activity of tetracycline in combination towards S. epidermidis biofilm cells. Chitosan efficiently inhibited S. epidermidis growth acting via cell membrane damage, yet the extent of antimicrobial and antibiofilm activities was quite strain-specific. It was proved to be a very efficient antimicrobial agent worth further examination as a potent candidate in pharmaceutical research. Apart from antimicrobial activity, it also acted as antivirulence enhancing agent which is a very promising strategy for alternative infectious diseases treatment.
Graphical abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Staphylococcus epidermidis nowadays represents one of the most clinically relevant opportunistic pathogens (Singh et al. 2010). It is also responsible for a wide spectrum of symptoms and diseases mostly related to biofilm formation (Amorena et al. 1999; Jarraud et al. 2002; Males et al. 1975). Staphylococcus epidermidis belongs to the most commonly isolated microorganisms from colonized medical devices which are often infected when in contact with human skin, where this species naturally occurs as part of human skin microbiome (Montanaro et al. 2011). However, the ability of this species to form biofilm on such devices poses a significant problem in medicine of prosthetic devices, especially in orthopaedics (artificial joint implants and prosthetics), urology (urinary catheters) and cardiology (venous catheters, prosthetic heart valves) (Cobrado et al. 2013). Biofilm formation is responsible for more than 70% of overall microbial infections in humans, and there are a comprehensive number of studies concerned with its medical impact (Costerton et al. 1999; Davey and O'Toole 2000; Ehrlich et al. 2010; Fux et al. 2005; Hall-Stoodley and Stoodley 2009; Mah and O'Toole 2001). Biofilm consists of microbial cells firmly attached to each other and to the colonized surface. The cells within it are enveloped in a self-produced extracellular matrix, which enables them to efficiently evade host immune system and to withstand high concentrations of possible antibiotic treatment (Branda et al. 2005). Since the antibiotics often fail to cure biofilm-related infections due to increased endurance of these cells and the inability to penetrate the complex structure of biofilm, the acquired microbial resistance towards these antimicrobial agents is even more likely to be developed in such environment than in planktonic cells (Livermore 2000; Mah and O'Toole 2001). The resistance of microbes towards various groups of antibiotics complicates the treatment of infectious diseases and puts a great pressure on the development of novel drugs. Beside conventional antibiotics used for the treatment of such infections, there are several novel approaches to regulate these pathogens. Such approach might include the targeting of specific components of biofilm to promote the penetration of other drugs (Anderl et al. 2000; Singh et al. 2010). Another possible option is to specifically target the microbial virulence and inhibit it, therefore diminishing the ability of the pathogen to infect the host in the first place and to further promote the host resistance in the case of already developed illness (Barczak and Hung 2009; Baron 2010; Barretti et al. 2009; Haynes 2001; Johnson and Abramovitch 2017; Males et al. 1975). Another way to regulate biofilm-related infections might be the use of naturally occurring substances with a strikingly different mode of action than those of the currently used antibiotics and other drugs, which would be less liable to lead to the development of microbial resistance (Adrian et al. 2000; Bandeira et al. 2018; Cerovsky 2014; Cobrado et al. 2013; Kolouchová et al. 2018; Mikstacka et al. 2010). Such compounds are often capable of acting in synergy with the antibiotics, thus overcoming the microbial resistance and decreasing the effective concentration of antibiotics to be used (Anderl et al. 2000; Ishak et al. 2016; Maťátková et al. 2017; Monzon et al. 2001). The importance of such dose decrement would benefit the patient, since there would not be the need to, for example, take multiple doses or to withstand unpleasant negative effects due to high doses of many antibiotics (nephrotoxicity, gastrointestinal problems, etc.).
Here, we focused on the effect of low-molecular weight chitosan (LMWCH) compared to two commercial antibiotics erythromycin (ERM) and tetracycline (TET) used for the treatment of staphylococcal infections. Chitosans are polysaccharides consisting of semi-acylated glucosamine monomers (Devlieghere et al. 2004). They are produced by partial deacetylation of chitin, which is obtained from crustaceans. They are relatively cheap to obtain, which makes them promising compounds for the research. Chitosan can be produced also biotechnologically, since it is a component of the cell wall of some fungi and the production by Aspergillus niger might be possible (Muslim et al. 2018). Chitosans are known to be effective against both gram-positive and gram-negative bacteria, yeast and even fungi as mentioned in a comprehensive reviews by Kumar (2000) and Goy et al. (2009), but the extent of their antimicrobial activity is dependent on their chemical and physical properties, mainly their molecular weight and deacetylation degree. They are also applicable in a plastic industry as a degradable plastic and as a possible carrier for other compounds used for various purposes (both industrial and medical) (Kumirska et al. 2011; Pillai et al. 2009; Wang et al. 2005). Generally, there are three proposed mechanisms of antimicrobial effect of chitosan (Goy et al. 2009; Raafat et al. 2008). It might act via electrostatic interaction of amino groups with a negatively charged cellular surface, which can eventually lead to cell surface damage or alteration in its function. Another possible mechanism of chitosan action lies in its ability to chelate ions (Pillai et al. 2009; Rinaudo 2006). Cytoplasmic membrane of microorganisms is often stabilized by Ca2+ and Mg2+ ions, which can be chelated by chitosan, thus weakening the cytoplasmic membrane rigidity. The last proposed mode of action is said to involve its ability to penetrate to cell nucleus, bind to negatively charged nucleic acids and inhibit DNA replication and transcription (Rabea et al. 2003). The last-mentioned mechanism is very controversial since chitosan is usually a very large molecule which would hardly penetrate the cell core entirely (Dmitriev et al. 2004). We have focused on its effect specifically on the growth of S. epidermidis and have evaluated whether it can act synergistically in combination with antibiotics, which would be otherwise ineffective against this pathogen. In connection to the above mechanisms of action, we have also attempted to evaluate LMWCH mechanism of action against studied microorganism and how it could possibly affect its combinatory effect with antibiotics and whether it would, alone or combined with antibiotics, somehow affect the haemolytic activity of this species.
Materials and methods
Antimicrobial agents
Commercially available low-molecular weight (50–75 kDa) partially deacylated (96%) chitosan (LMWCH) was provided by Sigma-Aldrich (Czech Republic). The stock solution was prepared by sonication (15 min) of LMWCH in 99% (v/v) acetic acid, which was then diluted in a growth medium to a final concentration of 1% acetic acid. The prepared solution was sonicated again until LMWCH was fully dissolved (30–45 min). Erythromycin (ERM) and tetracycline (TET) were acquired from Sigma-Aldrich (Czech Republic). The stock solutions of the antibiotics were prepared by dissolving the substance in the growth medium. All agents were studied in a final concentration range of 0.5–400 mg/L.
Microorganisms
Three collection strains and one clinical isolate of Staphylococcus epidermidis were studied. Staphylococcus epidermidis DBM 3179 was kindly provided by Department of Biochemistry and Microbiology, UCT Prague, Czech Republic. A type strain S. epidermidis ATCC 14990 was acquired from Czech National Collection of Type Cultures (Prague, Czech Republic). An elastase-positive strain S. epidermidis CCM 2343 was obtained from Czech Collection of Microorganisms (Brno, Czech Republic). Lastly, the clinical isolate of S. epidermidis, named M-1, was isolated from artificial knee implant infection from a patient in Motol University Hospital in Prague, Czech Republic. All microorganisms were stored in 50% (v/v) glycerol at − 70 °C. The microorganisms were precultured in TSB medium (Tryptone Soya Broth, Oxoid, UK) for 24 h at 37 °C and 150 rpm.
Cultivation of planktonic cells
The precultured inoculum optical density was adjusted to OD600nm = (0.100 ± 0.010) (approximately 1 × 107 CFU mL−1) and added into polystyrene microtitre plate wells (Honeycomb 2, Growth Curves, USA) in a volume of 30 µL. The rest of well volume was completed with either stock solution of antimicrobial agents or/and growth medium to a final volume of 320 µL. The cultivation took place in the automatic microcultivation device Bioscreen C (Labsystems, Finland) for 24 h at 37 °C. The minimum inhibitory concentration (MIC80) was determined as the lowest concentration of the antimicrobial agent which has already caused 80% decrease of suspension growth of the microorganism after 24 h of cultivation in comparison to the growth of cells without the antimicrobial agent (Vaňková et al. 2020a, b). The experiments were carried out in triplicates in three independent repetitions.
The antimicrobial effect of the antibiotics in combination with LMWCH was also studied. For the purpose, fractional inhibitory concentration index (FICi) was used according to Maťátková et al. (2017). This index determines whether the effect of a combination on suspension growth of microorganism is synergistic (FICi = 0.1–0.5), additive (FICi = 0.5–1.0), indifferent (FICi = 1.0–3.0) or antagonistic (FICi < 4.0). The value of FICi can be calculated from the following equation: FICi = FICA + FICB = cA (comb.)/MIC80,A + cB (comb.)/MIC80,B. According to this formula, FICi is a summation of FICA and FICB, which are fractional inhibitory concentrations for substance A or substance B in the combination. FIC is a ratio of the lowest effective concentration of the substance A or B in combination cA(comb.) and cB(comb.), and a minimum inhibitory concentration of these substances when acting alone against this microorganism (MIC80,A and MIC80,B). In this study, cA(comb.) and cB(comb) are the concentrations of each substance in the combination which has caused at least 80% decrease in suspension growth.
Cultivation of biofilm cells
The optical density of precultured inoculum was adjusted to OD600nm = (0.800 ± 0.020) (approximately 1 × 108 CFU/mL) and added into a 96-well polystyrene microtitre plate (TPP, Switzerland) in a volume of 210 µL. The rest of the well volume was completed with antimicrobial agent and growth medium to a final volume of 280 µL. The substances were added alone or in their combination.
The experiments evaluating the antibiofilm effect of antibiotics in combination with LMWCH were carried out according to Mishra and Wang (2017). The additions of LMWCH were derived from approximate average MIC80 of LMWCH for all S. epidermidis strains, which were added in combination with antibiotics. The LMWCH concentrations used were 33 mg/L, 50 mg/L and 66 mg/L. The antibiotics were studied in a range of concentrations from 5 to 100 mg/L. The cells were cultured for 24 h at 37 °C and 150 rpm. The experiments were executed in quadruplicates in three independent repetitions.
For the purpose of enzymatic activity determination, the biofilm was cultured in 24-well microtitre plates (TPP, Switzerland). The adjusted inoculum (OD600nm = 0.800) was added into each well in a volume of 1 mL. The well was filled to a final volume of 1100 µL with stock solution of the antimicrobial agent and medium. The cultivation took place under the same conditions as mentioned above. The experiments were executed in quadruplicates in three independent repetitions.
Determination of antibiofilm effect of antimicrobial agents
Metabolic activity of cells in biofilm
The formed biofilm was rinsed with sterile phosphate buffer saline (PBS, pH 7.4). The metabolic activity of cells in the biofilm was evaluated using MTT viability assay modified according to Riss et al. (2013). In short, 50 µL of MTT (3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide; Across Organics Belgium) at a concentration of 1 g/L (dissolved in PBS and filtered across 0.22-µm filter (EDM Millipore, USA)) and 60 µL of d-glucose at a concentration of 57.4 g/L (dissolved in PBS) was added into each well containing biofilm. The biofilm was then incubated for 1–3 h (depending on the colour change of the samples) at 37 °C and 150 rpm. The formed crystals of formazan were dissolved by adding 100 μL of formazan dissolving solution into each well. The solution comprised of 40% (v/v) dimethylformamide (Carl Roth, Germany) dissolved in 2% acetic acid (Penta, Czech Republic) (diluted in PBS) and 16% (w/v) sodium dodecylsulphate (Carl Roth, Germany). The biofilm was incubated for another 30 min at 230 rpm. An absorbance of 100 µL aliquot from each well was measured at 570 nm.
Minimum biofilm inhibitory concentration (MBIC80) was determined as the lowest concentration of each antimicrobial substance, which has lowered the metabolic activity of cells in biofilm by 80% in comparison to control (cells without any antimicrobial agent) after 24 h of cultivation. A similar approach was used also in the case of a combination study, where the main aim was to determine any combination, which would result in at least 80% inhibition of metabolic activity of biofilm cells in comparison to control (rel. 100%) after 24 h of cultivation. All experiments were carried out in quadruplicates in three independent repetitions.
Crystal violet staining
The biofilm biomass content was evaluated by crystal violet staining according to Kvasničková et al. (2016). Briefly, the rinsed biofilm grown in wells of 96-well plate was stained with 200 µL of filtered 0.1% aqueous solution of crystal violet (Carl Roth, Germany) for 20 min at room temperature. After staining, the liquid content of the wells was poured away, and the excess dye was removed by rinsing the biofilm with sterile saline. For the extraction of dye bound in the biofilm, 200 µL of 96% ethanol was poured into each well, and the extraction lasted 10 min at room temperature. An absorbance of 100 µL aliquot from each well was measured at 580 nm. The results are depicted in relative percentage (control samples represent 100%). All experiments were carried out in quadruplicates in three independent repetitions.
Alcian blue staining
The content of mucous exopolysaccharides in biofilm was evaluated by alcian blue staining modified according to several studies (Jordan et al. 1998; Knudsen et al. 1999; Semedo et al. 2015; Thornton et al. 2007) and described in Vaňková et al. (2020a, b). Briefly, the rinsed biofilm grown in wells of 96-well plate was stained with 200 µL of filtered 1% solution of alcian blue 8GX (Sigma-Aldrich, Czech Republic) in 1% acetic acid for 20 min at room temperature. After staining, the liquid content of the wells was poured away, and the excess dye was removed by rinsing the biofilm with sterile saline. For the extraction of dye bound in the biofilm, 200 µL of 50% ethanol was poured into each well, and the extraction lasted 10 min at room temperature. An absorbance of 100 µL aliquot from each well was measured at 620 nm. The results are depicted in relative percentage (control samples represent 100%). All experiments were carried out in quadruplicates in three independent repetitions.
Propidium iodide uptake
The membrane permeabilization activity was evaluated using propidium iodide (PI) uptake according to Nešuta et al. (2016) with a slight modification as mentioned in our previous work Kašparová et al. (2021). The biofilm of S. epidermidis DBM 3179 was cultured as described above but in black microtitre plates (black 96-well Microplate, F-BOTTOM (chimney well), Greiner Bio-One International GmbH, Austria) in the presence of LMWCH in a concentration range of 1–200 mg/L for 1, 2, 4, 8 and 24 h. The biofilm was rinsed twice with PBS. For the evaluation of permeabilization activity, 200 µL of 5 mg/L PI was added to the wells containing biofilm. After 5 min of incubation at room temperature in the dark, the fluorescence intensity of PI was measured by Infinite M200 Pro Reader (Tecan, Austria) at excitation/emission wavelength of 544/620 nm. The experiment contained also blank wells containing only PBS and PI, which later served for the measurement of background intensity signal, which was subtracted from fluorescence intensity values of the samples. All experiments were performed in quadruplicates in three independent repetitions.
Scanning electron microscopy
The biofilm formation of S. epidermidis DBM 3179 was visualized on medical grade silicone urinary catheters (All Silicone Foley Catheter, Well Lead Medical, China) by NanoSEM 450 (Fei, USA) microscope according to the procedure described in Vaňková et al. (2020a, b). For the purpose of cultivation and visualization, the catheters were aseptically cut into 1-cm long pieces and put into microtubes containing 1 mL of adjusted inoculum (OD600nm = 0.8) and 100 µL of growth media with or without antimicrobial agent. The cultivation of catheters was carried out for 24 h at 37 °C and 150 rpm. The colonized catheters were gently rinsed with distilled water and dried out completely by laminar flow and put into desiccator for 1 week before visualization. The dried colonized catheters were examined by SEM working at 10 kV at low vacuum by LVD detector at a magnification of 2500 × , spot size 5.0 and dwell time of 20 µs.
Haemolysis assay
The haemolytic activity of biofilm cells was evaluated according to Bandeira et al. (2018). The suspension above biofilm cultured in a 24-well microtitre plate was harvested by centrifugation (10,000 × g, 10 min, RT). The supernatant in a volume of 1 mL was incubated with 100 µL of 5% (v/v) defibrinated sheep blood (LabMediaServis, Czech Republic) diluted in TSB medium for 90 min at 37 °C. The positive control (100% haemolysis) comprised 1 mL of 2% (v/v) solution of SDS dissolved in TSB medium with 100 µL of diluted blood. The negative control (0% haemolysis) was 1 mL of TSB medium with 100 µL of diluted blood. The absorbance of the 100 µL aliquot of supernatant was measured at 540 nm, and the haemolytic activity was calculated from linear regression. The experiments were carried out in 4 parallels.
Statistical analysis
The distant results were identified and omitted according to Dixon’s Q Test. The arithmetic mean and standard deviation were calculated from colorimetric data. The significance of results was evaluated by one-way analysis of variance (ANOVA) with a significance level p < 0.05.
Results
Effect of LMWCH and antibiotics on suspension growth of S. epidermidis
The antimicrobial susceptibility of S. epidermidis was evaluated by determining minimum inhibitory concentrations (MIC80) for each substance tested. ERM was the most efficient against planktonic cells of all studied strains with MIC80 ranging from 0.25 to 0.75 mg/L (Table 1). In contrast, TET had various effects on planktonic cells of S. epidermidis. It was quite effective against the strain S. epidermidis CCM 2343 (MIC80 = 20 mg/L) (Table 2). The clinical isolate M-1 was the least susceptible, with MIC80 of TET 100 mg/L. The MIC80 values of LMWCH for S. epidermidis were between those for the two studied antibiotics, ranging from 35 to 40 mg/L (Tables 1 and 2). The influence of LMWCH in combination with ERM on suspension growth of S. epidermidis was rather ineffective (Table 1). Additive effects of the combinations were found only in case of the strains S. epidermidis ATCC 14990 and the clinical isolate M-1. The other two strains were not effectively inhibited by any combination. In the case of S. epidermidis ATCC 14990, the combination of 3.5 mg/L (10% MIC80) of LMWCH with 0.45 mg/L (60% MIC80) of ERM resulted in 0.7 value of FICi indicating an additive action of such combination. Similarly, an additive action was also found for LMWCH combined with ERM against the clinical isolate M-1. In this case, 16 mg/L (40% MIC80) of LMWCH was combined with 0.025 mg/L (10% of MIC80) of ERM resulting also in 0.7 of FICi.
In the case of TET in combination with LMWCH, additive effects were found for all studied strains (Table 2). The most effective combination was found against S. epidermidis DBM 3179 resulting in the lowest FICi value of 0.7 indicating an additive action of such combination. The LMWCH (3.5 mg/L, 10% MIC80) was in this case combined with 39 mg/L of TET (60% MIC80). In the case of S. epidermidis ATCC 14,990 and the clinical isolate M-1, the most effective combinations resulted in FICi with value of 0.8, i.e. acting also additively.
Effect of LMWCH and antibiotics on biofilm metabolic activity of S. epidermidis
Although ERM was very effective against planktonic cells of S. epidermidis, it was found to be completely ineffective against the biofilm cells. The minimum biofilm inhibitory concentrations (MBIC80) for observed strains were not determined in a studied range of concentrations (1–400 mg/L of ERM) (Table 3). A similar trend was observed also for TET. Only in the case of S. epidermidis CCM 2343, the MBIC80 was determined for 350 mg/L TET. In contrast to both antibiotics, LMWCH maintained its activity even against metabolic activity of biofilm cells with MBIC80 ranging between 40 and 200 mg/L.
Effect of LMWCH on metabolic activity, total biofilm biomass and mucous exopolysaccharide content in S. epidermidis biofilm
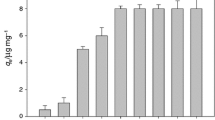
To elucidate the antibiofilm action of LMWCH, we studied its effect on various aspects of biofilm formation of S. epidermidis DBM 3179 (Fig. 1). Metabolic activity of biofilm cells decreased significantly in a dose-dependent manner. LMWCH at a concentration of 40 mg/L caused more than 80% inhibition and this concentration was determined as MBIC80 for this strain as mentioned above (p = 0.021; Table 3). Although metabolic activity of biofilm cells decreased rapidly with low LMWCH concentrations, the biofilm biomass increased its content up to 242% in the case of treatment with 40 mg/L LMWCH. The content of mucous polysaccharides, one of the components of S. epidermidis biofilm, was not significantly altered by the treatment with 1–80 mg/L of LMWCH (p < 0.05). Higher concentrations of LMWCH (150–200 mg/L) resulted in a decrement of both total biofilm biomass and the content of mucous exopolysaccharides (p < 0.05). LMWCH at a concentration of 200 mg/L caused a complete inhibition of metabolic activity of biofilm cells and decreased total biofilm biomass and content of mucous polysaccharides by 50% and 40%, respectively.
Effect of chitosan (LMWCH) on metabolic activity of biofilm cells, content of mucous polysaccharides and total biofilm biomass of S. epidermidis DBM 3179 (24 h, 37 °C, 150 rpm). Black bars—metabolic activity of biofilm cells, grey bars—content of mucous polysaccharides, white bars—total biofilm biomass; y-axis depicts results of all assays in relative percentage (control represents 100%), error bars represent standard deviation
Membrane damage and disruption S. epidermidis biofilm cells by LMWCH
To further examine the effect of LMWCH on biofilm cells of S. epidermidis, the membrane damage of biofilm cells due to treatment with it was evaluated using propidium iodide (PI) uptake assay, as depicted in Fig. 2. The treatment of biofilm cells with even very low concentrations of LMWCH (1–20 mg/L) led to slight membrane damage in whole course of cultivation (Fig. 2A). As the concentration tested increased (40–100 mg/L) so did fluorescence intensity indicating a higher extent of cellular damage in the biofilm treated for 24 h (Fig. 2B). As described previously, there was a significant increment of total biofilm biomass of biofilm cells of S. epidermidis DBM 3179 as opposed to its metabolic activity when treated with 40 mg/L. Such concentration also caused a further increase in fluorescence intensity of PI indicating a great cellular damage leading probably to cell lysis and rapid viability decrease in biofilm cells. The less notable increment in total biofilm biomass might indicate that the cell damage caused by 80 mg/L LMWCH was less tolerated, yet the cells still attempted to “hide themselves” inside the biofilm (Fig. 2B). LMWCH at a concentration of 100 mg/L caused the PI signal to reach its maximum reflecting a great damage caused by such concentration. As mentioned above, such concentration completely inhibited the metabolic activity of biofilm cells. The increased concentration of LMWCH (200 mg/L) resulted in a decreased PI fluorescence signal in comparison to 100 mg/L probably due to a smaller portion of cells still able to attach to surface and form biofilm (Fig. 2B).
Disruption of Staphylococcus epidermidis DBM 3179 biofilm cells by chitosan (LMWCH) cultured for 1–24 h measured as fluorescence intensity of uptaken propidium iodide (PI) (TSB, 37 °C, 150 rpm). A Kinetics of biofilm cells disruption measured for 24 h; white □—untreated biofilm cells, biofilm cells cultured in presence of 1 mg/L LMWCH (black
 ), 2 mg/L LMWCH (dark grey
), 2 mg/L LMWCH (dark grey
 ), 4 mg/L LMWCH (light grey
), 4 mg/L LMWCH (light grey
 ), biofilm cells cultured in presence of 8 mg/L LMWCH (black
), biofilm cells cultured in presence of 8 mg/L LMWCH (black
 ), 20 mg/L LMWCH (dark grey
), 20 mg/L LMWCH (dark grey
 ), 40 mg/L LMWCH (light grey
), 40 mg/L LMWCH (light grey
 ), biofilm cells cultured in presence of 80 mg/L LMWCH (black
), biofilm cells cultured in presence of 80 mg/L LMWCH (black
 ), 100 mg/L LMWCH (dark grey
), 100 mg/L LMWCH (dark grey
 ), 200 mg/L LMWCH (light grey
), 200 mg/L LMWCH (light grey
 ). B Effects of LMWCH concentration on biofilm cells disruption after 24 h treatment with LMWCH, error bars represent standard deviations
). B Effects of LMWCH concentration on biofilm cells disruption after 24 h treatment with LMWCH, error bars represent standard deviations
Effect of LMWCH in combination with antibiotics on biofilm metabolic activity of S. epidermidis
The effect of LMWCH in combination with ERM on studied strains of S. epidermidis was largely strain-dependent, as can be seen in Fig. 3. Staphylococcus epidermidis DBM 3179 was not particularly inhibited by the ERM alone, but in the presence of 5 mg/L of this antibiotic combined with 33 mg/L of LMWCH, the metabolic activity of biofilm cells was inhibited by 18% in comparison with control (p < 0.05; Fig. 3A). Additionally, ERM at a concentration of 10 mg/L combined with 50 mg/L LMWCH and at 5 mg/L combined with 66 mg/L LMWCH caused an almost complete (˃ 95%) reduction in metabolic activity of biofilm cells (p = 0.0001). The higher concentrations of LMWCH caused complete reduction of metabolic activity of this strain biofilm cells. In the case of S. epidermidis ATCC 14990 (Fig. 3B), there was a significant decrease in metabolic activity when ERM was combined with 50 and 66 mg/L of LMWCH (p < 0.05). There was no promising activity of ERM combinations with LMWCH in case of S. epidermidis CCM 2343 (Fig. 3C) and clinical isolate M-1 (Fig. 3D).
Combined effect of erythromycin (ERM) with chitosan (LMWCH) on metabolic activity of S. epidermidis biofilm cells (24 h, 37 °C, 150 rpm). A DBM 3179, B ATCC 14990, C CCM 2343, D clinical isolate M-1. X-axis and Z-axis depict concentrations of ERM and LMWCH, respectively. Y-axis depicts metabolic activity of cells in biofilm in relative percentage (control is always 100%)
LMWCH in combination with TET was shown to be more promising than with ERM, as can be seen in Fig. 4. Similarly, S. epidermidis DBM 3179 was susceptible towards the combinations of TET with LMWCH (Fig. 4A). An effective combination resulting in 90% inhibition of metabolic activity was observed when 10 mg/L of TET was combined with 50 mg/L of LMWCH. The addition of 66 mg/L of LMWCH to every concentration of TET also resulted in a significant decrease of metabolic activity (more than 90% inhibition; p = 0.003). In the case of this particular strain, the experiments with combinations of TET with 50 and 66 mg/L LMWCH were carried out to confirm the lack of any antagonistic effect of such combinations and to further promote complete inhibition of metabolic activity of biofilm cells, since the MBIC80 of LMWCH alone was 40 mg/L. TET combined with LMWCH was very effective on biofilm cells of S. epidermidis CCM 2343 (Fig. 4C). The greatest decrease of metabolic activity (90%) was observed when biofilm cells were grown in the presence of 100 mg/L TET with 50 mg/L LMWCH (p = 0.003). In the case of S. epidermidis ATCC 14990 (Fig. 4B) and the clinical isolate M-1 (Fig. 4D), however, no promising combinatory action was determined.
Combined effect of tetracycline (TET) with chitosan (LMWCH) on metabolic activity of S. epidermidis biofilm cells (24 h, 37 °C, 150 rpm). A DBM 3179, B ATCC 14990, C CCM 2343, D clinical isolate M-1. X-axis and Z axis depict concentrations of TET and LMWCH, respectively. Y-axis depicts metabolic activity of cells in biofilm in relative percentage (control is always 100%)
Visualization of S. epidermidis biofilm formed on silicone catheters by SEM
The biofilm of S. epidermidis DBM 3179 formed on medical grade silicone catheters in the presence of studied antimicrobial agents was visualized by SEM (Fig. 5). When this strain was cultivated without the antimicrobial agents, it formed a slightly less compact biofilm in comparison with other strains (visualizations performed in previous study (Kašparová et al. 2021) with apparent clusters of cells enveloped in extracellular matrix (Fig. 5A). The treatment with 33 mg/L of LMWCH resulted in weakened adhesion of cells and formation of isolated microcolonies, as is apparent in Fig. 5B. ERM (5 mg/L) inhibited biofilm formation of S. epidermidis cells, which attached in smaller colonies (Fig. 5C). A combination of 5 mg/L ERM with 33 mg/L LMWCH however suppressed the biofilm formation completely, with only a small ratio of solitary adhered cells apparent (Fig. 5D). In the case of 5 mg/L TET, the biofilm formation was mostly unaffected, as can be seen in Fig. 5E. In the case of its combination with 33 mg/L LMWCH, the treatment resulted in a complete suppression of biofilm formation, with only a few individual cells still attached to the silicone catheter surface (Fig. 5F). When combined with LMWCH, both antibiotics completely prevented the colonization of catheters.
SEM micrographs depicting the biofilm of S. epidermidis DBM 3179 formed on silicone catheters when cultured alone and in presence of erythromycin (ERM), tetracycline (TET), chitosan (LMWCH) or their combinations in growth medium (24 h, 37 °C, 150 rpm). A Cells grown without any antimicrobial agent, B cells grown in presence of 33 mg/L LMWCH, C cells grown in presence of 5 mg/L ERM, D cells grown in presence of 5 mg/L ERM and 33 mg/L LMWCH, E cells grown in presence of 5 mg/L TET, F cells grown in presence of 5 mg/L TET and 33 mg/L LMWCH. Parameters of image taking: low vacuum, LVD detector, 10 kV, magnification 2500 × , spot size 5, dwell time 20 µs, scale bar = 30 µm
Effect of LMWCH alone and in combination with antibiotics on the haemolytic activity of S. epidermidis biofilm cells
The effect of LMWCH alone and in combination with antibiotics on the haemolytic activity of S. epidermidis biofilm cells was observed (Table 4). The untreated biofilm cells of three S. epidermidis strains (DBM 3179, CCM 2343 and clinical isolate M-1) displayed approximately 50% haemolytic activity in comparison with positive control (2% SDS; 100%). The type strain of S. epidermidis (ATCC 14990) interestingly possessed particularly lower haemolytic activity (25%). The treatment with 33 mg/L of LMWCH did not result in a significant change of haemolysis by S. epidermidis biofilm cells in case of all strains. ERM and TET on the other hand mostly decreased it with an exception of the effect of ERM (5 mg/L) in the case of S. epidermidis ATCC 14990 and S. epidermidis CCM 2343. In the case of S. epidermidis DBM 3179, the combination of ERM or TET with LMWCH resulted in an even greater inhibition of haemolytic activity of biofilm cells of this strain. On the contrary, ERM in combination with LMWCH manifested a rather antagonistic effect on haemolytic activity of biofilm cells in the case of all strains except for S. epidermidis DBM 3179. In the case of TET combined with LMWCH, the results consistently showed synergistic antihaemolytic action of such combination.
Discussion
The great spread of antimicrobial resistance among pathogens provided an impetus for the search for novel antimicrobial compounds or alternative antimicrobial approaches for treatment of infectious diseases. Among other strategies, science turns to naturally occurring compounds as a possible source of new substances for antimicrobial drug development. One such compound is chitosan, which, due to its antimicrobial potential, origin and cheap manufacturing cost seems very promising. It had already been a subject of a large number of studies dealing with its use as a potent antimicrobial agent (Asli et al. 2017; Begin and Van Calsteren 1999; Carlson et al. 2008; Cobrado et al. 2012; Costa et al. 2017; Goy et al. 2009). Although its activity is thus documented, the extent of antimicrobial efficacy of chitosan is variable.
Chitosans generally are substances with various physical and chemical properties, with variable molecular weight, viscosity or percentage of deacetylation (Kong et al. 2010). Chitosans might also be derivatized with ammonium to a quaternized form or to chitosans containing carboxymethyl functions (Kong et al. 2010; Rabea et al. 2003; Shagdarova et al. 2016; Tam et al. 2015; Tan et al. 2013). All these parameters can affect the antimicrobial activity of all chitosan derivatives, and each studied type of chitosan has to be properly described in every study for better comparison and inclusion of all the important aspects. Apart from its potency as antimicrobial agent, chitosan is frequently studied as a carrier for other antimicrobial substances either in the form of nanoparticles or as a coating of materials binding in its structure other antimicrobial agents (Goy et al. 2009). Such protective films propose an elegant way to prevent any pathogen from colonizing medical devices like catheters or joint implants (Begin and Van Calsteren 1999; Carlson et al. 2008; Costa et al. 2017; Dutta et al. 2009; Hayder et al. 2018; Lin et al. 2016; Mantripragada and Jayasuriya 2016; Peng et al. 2015; Piras et al. 2015; Shi et al. 2006; Tan et al. 2014). In each type of such formulations, the antimicrobial efficacy of chitosan alone differs from its use in solution, which was the main topic of our work.
Here, we have dealt with low-molecular weight (50–75 kDa) 92% deacetylated LMWCH which was effective against planktonic growth and biofilm formation of S. epidermidis including its potential antivirulence effect on haemolytic activity of the cells. LMWCH maintained its antimicrobial activity in relatively low concentrations even against biofilm metabolic activity of S. epidermidis in contrast to the antibiotics ERM and TET, which affected the metabolic activity of biofilm cells only partially (MBIC80 of LMWCH ranged from 40 to 200 mg/L whereas antibiotics failed to cause any inhibition of biofilm metabolic activity even in 400 mg/L). Although the efficacy of LMWCH was proven, the strains varied in their susceptibility greatly, which was given by their origin as mentioned in materials and methods section. The work included distinct strains with variable ability to form biofilm to cover all aspects of the studied species for better generalization of the overall LMWCH effect. Even though there were some differences in each strain response, interestingly, chitosan concentrations routinely used in the literature are in g/l, which is in a strict contrast with our study that proved LMWCH effective in much lower concentrations.
LMWCH was very effective since it caused significant inhibition of planktonic growth in distinctively lower concentrations than those used in the literature (Asli et al. 2017; Raafat et al. 2008; Rubini et al. 2018). Tavaria et al. (2013) determined MIC100 of LMWCH at 1250 mg/L for S. epidermidis, which is many times more than in our study (MIC80 ranged between 35 and 40 mg/L for all studied strains). Asli et al. (2017) and Rubini et al. (2018) evaluated the effect of LMWCH on Staphylococcus aureus, a species related to S. epidermidis, and determined MIC100 at 1000 mg/L, and between 200 and 600 mg/L, respectively. Raafat et al. (2008) however determined MIC80 for the same species at 23 mg/L, and two other studies also reported MIC80 for S. aureus at identical 20 mg/L (Liu et al. 2001; Raafat et al. 2008; Rabea et al. 2003). Cobrado et al. (2012) studied LMWCH and used it against S. epidermidis. They determined its MIC100 at 160 mg/L. It might have been due to different strains studied, but still, the determined MIC100 was considerably higher than in our study. The authors however observed great activity of chitosan against biofilm formation of S. epidermidis, with 78 mg/L of chitosan decreasing metabolic activity of biofilm cells by 80% (Cobrado et al. 2012). Correspondingly, in our study, we have achieved 80% inhibition at a concentration range of 40–200 mg/L of LMWCH. In their following study (Cobrado et al. 2013), 80 mg/L of low-molecular weight chitosan caused 58% decrease in metabolic activity of biofilm cells of S. epidermidis and also a 40% decrease in total biofilm biomass. In our study, LMWCH at the same concentration caused an almost total reduction of metabolic activity of biofilm cells. The total biofilm biomass on the other hand was not inhibited by the LMWCH and even, in some cases, the presence of LMWCH caused a slight increase, which contradicts the results by Cobrado et al. (2013). Interestingly, we have also evaluated the content of mucous polysaccharides, which represent a major component of extracellular biofilm matrix, and we found that it was unchanged in almost the whole studied range of concentrations (1–150 mg/L of LMWCH). Only the highest studied concentration of 200 mg/L of LMWCH caused an approximately 50% decrease in both total biofilm biomass and the content of mucous polysaccharides (Thomas et al. 1997). To evaluate further why the total biofilm biomass increased its volume as indicated by crystal violet staining, we studied the extent of cytoplasmic membrane damage in biofilm cells formed in the presence of LMWCH (range 1–200 mg/L). Interestingly, 100 and 150 mg/L caused the greatest disruption of cytoplasmic membranes, which indicated that most of the biofilm cells were lysed, releasing its intracellular content to its surrounding. The leakage of cell content might have increased the crystal violet staining results, as was also proved by the inverse microscopy of biofilm cells treated with chitosan and stained by crystal violet, since there was a decreasing trend in stained biofilm coverage of microtitre plate well bottom.
Furthermore, the ability of LMWCH to inhibit cell adhesion was proved also by scanning electron microscopy, which proved LMWCH at a concentration of 33 mg/L lowered the biofilm formation of visualized strain of S. epidermidis DBM 3179 (in contrast to total biofilm biomass determination). The proposed cytoplasmic membrane damage and subsequent lysis of S. epidermidis cells treated with LMWCH were also proved by other studies (Kong et al. 2010; Liu et al. 2004; Raafat et al. 2008). LMWCH might facilitate the uptake of otherwise inefficient antibiotics. Thus, the disrupted cell membrane after treatment with LMWCH would lead to a rapid uptake of antibiotics to cell interior and the promotion of their antimicrobial effect. In our study, such cooperation was observed in some cases of combinations of ERM and TET with LMWCH acting on both planktonic cells and biofilm formation. ERM activity was not greatly enhanced by the addition of LMWCH, and both substances acted independently of each other against both planktonic growth (additive or indifferent action according to FICi) and biofilm metabolic activity (no significant decrease due to combining both agents with the exception of S. epidermidis DBM 3179). On the other hand, TET combined with LMWCH indeed achieved a significant decrease in both planktonic growth and to some extent also metabolic activity of biofilm cells. Such efficient combinatory action might be for example due to LMWCH ability to chelate metals. The efflux of ions from cells is a powerful tool for inactivation of TET and other antibiotics from the same group (Agwuh and MacGowan 2006). With LMWCH chelating such ions, TET might have been able to interact with cells and possibly penetrate inside. Once TET started affecting the cell, the life cycle was retarded, and LMWCH had possibly a greater chance to disrupt the cells and eventually cause their lysis and death. This is, however, only our hypothesis and such presumptions must be further verified.
Lastly, in all cases, the addition of LMWCH to TET further decreased the production of haemolysins in S. epidermidis; this points to the possible antivirulence action of such combinations. Khan et al. (2019) also investigated the antivirulence effect of chitooligosaccharides (substances derived from chitosan) on S. aureus and found that they indeed suppress the haemolytic activity of studied strains (Khan et al. 2019). To our best knowledge, there are no other studies dealing with antihaemolytic activity of LMWCH on staphylococci. In a similar study, Khan et al. (2019) evaluated its antivirulence effect on Pseudomonas aeruginosa (a gram-negative pathogenic bacterium) and indeed found that LMWCH might possess an antivirulence activity apart from its great antimicrobial properties. The potential antivirulence activity of LMWCH has not been thoroughly examined yet, and to our best knowledge, there is only one other study focusing on antivirulence action of non-derivatized LMWCH on a representative of genus Staphyloccocus. Rubini et al. (2018) observed that LMWCH decreased the production of staphyloxanthin, a pigment of S. aureus, as well as the production of the slime in its biofilm, thus proving the antivirulence action of this substance.
In conclusion, we have evaluated the effect of LMWCH on S. epidermidis planktonic growth and biofilm formation. All studied strains were tolerant to TET and susceptible to ERM in planktonic form, but their biofilm metabolic activity was not greatly affected by the antibiotics. In contrast, LMWCH effectively inhibited biofilm formation probably via severe cytoplasmic membrane damage as was shown by PI-uptake assay. LMWCH also promoted TET antihaemolytic action thus increasing the antivirulence activity of such combinations. An antimicrobial action of ERM was not significantly enhanced by LMWCH in combination and additive action of such combination was observed only for two strains. The combination of TET with LMWCH however acted additively on planktonic growth of all studied S. epidermidis strains, but it was inefficient in inhibition of its biofilm formation. The convenient combinatory action of TET with LMWCH on planktonic growth might be given due to its complex mechanism of action (e.g. chelation of metals, interaction and possible disruption of cytoplasmic membrane). Such combinations of drugs might find application in medicine, specifically in orthopaedics for the treatment of intricate biofilm-related infections.
References
Adrian M, Jeandet P, Douillet-Breuil AC, Tesson L, Bessis R (2000) Stilbene content of mature Vitis vinifera berries in response to UV-C elicitation. J Agric Food Chem 48:6103–6105. https://doi.org/10.1021/jf0009910
Agwuh KN, MacGowan A (2006) Pharmacokinetics and pharmacodynamics of the tetracyclines including glycylcyclines. J Antimicrob Chemother 58:256–265. https://doi.org/10.1093/jac/dkl224
Amorena B, Gracia E, Monzon M, Leiva J, Oteiza C, Perez M, Alabart JL, Hernandez-Yago J (1999) Antibiotic susceptibility assay for Staphylococcus aureus in biofilms developed in vitro. J Antimicrob Chemother 44:43–55. https://doi.org/10.1093/jac/44.1.43
Anderl JN, Franklin MJ, Stewart PS (2000) Role of antibiotic penetration limitation in Klebsiella pneumoniae biofilm resistance to ampicillin and ciprofloxacin. Antimicrob Agents Chemother 44:1818–1824
Asli A, Brouillette E, Ster C, Ghinet MG, Brzezinski R, Lacasse P, Jacques M, Malouin F (2017) Antibiofilm and antibacterial effects of specific chitosan molecules on Staphylococcus aureus isolates associated with bovine mastitis. Plos One 12:1–23. https://doi.org/10.1371/journal.pone.0176988
Bandeira G, Sutili FJ, Gressler LT, Ely VL, Silveira BP, Tasca C, Reghelin M, Matter LB, Vargas APC, Baldisserotto B (2018) Antibacterial potential of phytochemicals alone or in combination with antimicrobials against fish pathogenic bacteria. J Appl Microbiol 125:655–665. https://doi.org/10.1111/jam.13906
Barczak AK, Hung DT (2009) Productive steps toward an antimicrobial targeting virulence. Curr Op Microbiol 12:490–496. https://doi.org/10.1016/j.mib.2009.06.012
Baron C (2010) Antivirulence drugs to target bacterial secretion systems. Curr Op Microbiol 13:100–105. https://doi.org/10.1016/j.mib.2009.12.003
Barretti P, Montelli AC, Batalha JEN, Caramori JCT, Cunha M (2009) The role of virulence factors in the outcome of staphylococcal peritonitis in CAPD patients. Bmc Infect Dis 9:1–8. https://doi.org/10.1186/1471-2334-9-212
Begin A, Van Calsteren MR (1999) Antimicrobial films produced from chitosan. Int J Biol Macromol 26:63–67. https://doi.org/10.1016/s0141-8130(99)00064-1
Branda SS, Vik A, Friedman L, Kolter R (2005) Biofilms: the matrix revisited. Trends Microbiol 13:20–26. https://doi.org/10.1016/j.tim.2004.11.006
Carlson RP, Taffs R, Davison WM, Stewart PS (2008) Anti-biofilm properties of chitosan-coated surfaces. J Biomat Sci-Polym E 19:1035–1046. https://doi.org/10.1163/156856208784909372
Cerovsky V (2014) Antimicrobial peptides isolated from Insects. Chem Listy 108:344–353
Cobrado L, Azevedo MM, Silva-Dias A, Ramos JP, Pina-Vaz C, Rodrigues AG (2012) Cerium, chitosan and hamamelitannin as novel biofilm inhibitors? J Antimicrob Chemother 67:1159–1162. https://doi.org/10.1093/jac/dks007
Cobrado L, Silva-Dias A, Azevedo MM, Pina-Vaz C, Rodrigues AG (2013) in vivo antibiofilm effect of cerium, chitosan and hamamelitannin against usual agents of catheter-related bloodstream infections. J Antimicrob Chemother 68:126–130. https://doi.org/10.1093/jac/dks376
Costa EM, Silva S, Vicente S, Neto C, Castro PM, Veiga M, Madureira R, Tavaria F, Pintado MM (2017) Chitosan nanoparticles as alternative anti-staphylococci agents: bactericidal, antibiofilm and antiadhesive effects. Mat Sci Eng C-Mater 79:221–226. https://doi.org/10.1016/j.msec.2017.05.047
Costerton JW, Stewart PS, Greenberg EP (1999) Bacterial biofilms: a common cause of persistent infections. Science 284:1318–1322. https://doi.org/10.1126/science.284.5418.1318
Davey ME, O’Toole GA (2000) Microbial biofilms: from ecology to molecular genetics. Microbiol Mol Biol Rev 64:847–852. https://doi.org/10.1128/mmbr.64.4.847-867.2000
Devlieghere F, Vermeulen A, Debevere J (2004) Chitosan: antimicrobial activity, interactions with food components and applicability as a coating on fruit and vegetables. Food Microbiol 21:703–714. https://doi.org/10.1016/j.fm.2004.02.008
Dmitriev BA, Holst O, Rietschel ET, Ehlers S (2004) Tertiary structure of Staphylococcus aureus cell wall murein. J Bacteriol 186:7141–7148. https://doi.org/10.1128/jb.186.21.7141-7148.2004
Dutta PK, Tripathi S, Mehrotra GK, Dutta J (2009) Perspectives for chitosan based antimicrobial films in food applications. Food Chem 114:1173–1182. https://doi.org/10.1016/j.foodchem.2008.11.047
Ehrlich GD, Ahmed A, Earl J, Hiller NL, Costerton JW, Stoodley P, Post JC, Demeo P, Hu FZ (2010) The distributed genome hypothesis as a rubric for understanding evolution in situ during chronic bacterial biofilm infectious processes. Fems Immunol Med Mic 59:269–279. https://doi.org/10.1111/j.1574-695X.2010.00704.x
Fux CA, Costerton JW, Stewart PS, Stoodley P (2005) Survival strategies of infectious biofilms. Trends Microbiol 13:34–40. https://doi.org/10.1016/j.tim.2004.11.010
Goy RC, de Britto D, Assis OBG (2009) A review of the antimicrobial activity of chitosan. Polimeros 19:241–247
Hall-Stoodley L, Stoodley P (2009) Evolving concepts in biofilm infections. Cell Microbiol 11:1034–1043. https://doi.org/10.1111/j.1462-5822.2009.01323.x
Hayder J, Chaouch MA, Amira N, Ben Mansour M, Majdoub H, Chaubet F, Maaroufi RM (2018) Co-immobilization of chitosan and dermatan sulfate from Raja montagui skin on polyethylene terephthalate surfaces: characterization and antibiofilm activity. Int J Polym Mater Po 67:277–287. https://doi.org/10.1080/00914037.2017.1320664
Haynes K (2001) Virulence in Candida species. Trends Microbiol 9:591–596. https://doi.org/10.1016/s0966-842x(01)02237-5
Ishak SF, Ghazali AR, Zin NM, Basri DF (2016) Pterostilbene enhanced anti-methicillin resistant Staphylococcus aureus (MRSA) Activity of Oxacillin. Am J Infec Dis 12:1–10. https://doi.org/10.3844/ajidsp.2016.1.10
Jarraud S, Mougel C, Thioulouse J, Lina G, Meugnier H, Forey F, Nesme X, Etienne J, Vandenesch F (2002) Relationships between Staphylococcus aureus genetic background, virulence factors, agr groups (Alleles), and human disease. Infect Immun 70:631–641. https://doi.org/10.1128/iai.70.2.631-641.2002
Johnson BK, Abramovitch RB (2017) Small molecules that sabotage bacterial virulence. Trends Pharmacol Sci 38:339–362. https://doi.org/10.1016/j.tips.2017.01.004
Jordan N, Newton J, Pearson J, Allen A (1998) A novel method for the visualization of the in situ mucus layer in rat and man. Clin Sci 95:97–106. https://doi.org/10.1042/cs19980081
Kašparová P, Vaňková E, Brázdová L, Lokočová K, Maťátková O, Masák J (2021) Antibiofilm agent pterostilbene is able to enhance antibiotics action against Staphylococcus epidermidis. Microb Pathogen 152. https://doi.org/10.1016/j.micpath.2020.104632
Khan F, Manivasagan P, Pham DTN, Oh J, Kim SK, Kim YM (2019) Antibiofilm and antivirulence properties of chitosan-polypyrrole nanocomposites to Pseudomonas aeruginosa. Microb Pathogen 128:363–373. https://doi.org/10.1016/j.micpath.2019.01.033
Knudsen G, Sorum H, Press CM, Olafsen JA (1999) in situ adherence of Vibrio spp. to cryosections of Atlantic salmon, Salmo salar L., tissue. J Fish Dis 22:409–418. https://doi.org/10.1046/j.1365-2761.1999.00183.x
Kolouchová I, Maťátková O, Paldrychová M, Kodeš Z, Kvasničková E, Sigler K, Čejková A, Šmidrkal J, Demnerová K, Masák J (2018) Resveratrol, pterostilbene, and baicalein: plant-derived anti-biofilm agents. Folia Microbiol 63:261–272. https://doi.org/10.1007/s12223-017-0549-0
Kong M, Chen XG, Xing K, Park HJ (2010) Antimicrobial properties of chitosan and mode of action: a state of the art review. Int J Food Microbiol 144:51–63. https://doi.org/10.1016/j.ijfoodmicro.2010.09.012
Kumar M (2000) A review of chitin and chitosan applications. React Funct Polym 46:1–27. https://doi.org/10.1016/S1381-5148(00)00038-9
Kumirska J, Weinhold MX, Thoming J, Stepnowski P (2011) Biomedical activity of chitin/chitosan based materials-influence of physicochemical properties apart from molecular weight and degree of N-acetylation. Polymers 3:1875–1901. https://doi.org/10.3390/polym3041875
Kvasničková E, Paulicek V, Paldrychova M, Jezdik R, Mat’atkova O, Masak J (2016) Aspergillus fumigatus DBM 4057 biofilm formation is inhibited by chitosan, in contrast to baicalein and rhamnolipid. World J Microb Biot 32:187–197. https://doi.org/10.1007/s11274-016-2146-9
Lin WT, Zhang YY, Tan HL, Ao HY, Duan ZL, He G, Tang TT (2016) Inhibited bacterial adhesion and biofilm formation on quaternized chitosan-loaded titania nanotubes with various diameters. Materials 9:155–167. https://doi.org/10.3390/ma9030155
Liu H, Du YM, Wang XH, Sun LP (2004) Chitosan kills bacteria through cell membrane damage. Int J Food Microbiol 95:147–155. https://doi.org/10.1016/j.ijfoodmicro.2004.01.022
Liu XF, Guan YL, Yang DZ, Li Z, De Yao K (2001) Antibacterial action of chitosan and carboxymethylated chitosan. J App Polym Sci 79:1324–1335. https://doi.org/10.1002/1097-4628(20010214)79:7%3c1324::AID-APP210%3e3.0.CO;2-L
Livermore DM (2000) Antibiotic resistance in staphylococci. Int J Antimicrob Agents 16:S3–S10
Mah TFC, O’Toole GA (2001) Mechanisms of biofilm resistance to antimicrobial agents. Trends Microbiol 9:34–39. https://doi.org/10.1016/s0966-842x(00)01913-2
Males BM, Rogers WA, Parisi JT (1975) Virulence factors of biotypes of Staphylocccus epidermidis from clinical sources. J Clin Microbiol 1:256–261
Mantripragada VP, Jayasuriya AC (2016) Effect of dual delivery of antibiotics (vancomycin and cefazolin) and BMP-7 from chitosan microparticles on Staphylococcus epidermidis and pre-osteoblasts in vitro. Mat Sci Eng C-Mater 67:409–417. https://doi.org/10.1016/j.msec.2016.05.033
Maťátková O, Kolouchová I, Kvasničková E, Ježdík R, Masák J, Čejková A (2017) Synergistic action of amphotericin B and rhamnolipid in combination on Candida parapsilosis and Trichosporon cutaneum. Chem Pap 71:1471–1480. https://doi.org/10.1007/s11696-017-0141-8
Mikstacka R, Rimando AM, Ignatowicz E (2010) Antioxidant effect of trans-resveratrol, pterostilbene, quercetin and their combinations in human erythrocytes in vitro. Plant Food Hum Nutr 65:57–63. https://doi.org/10.1007/s11130-010-0154-8
Mishra B, Wang GS (2017) Individual and combined effects of engineered peptides and antibiotics on Pseudomonas aeruginosa biofilms. Pharmaceuticals 10:1–15. https://doi.org/10.3390/ph10030058
Montanaro L, Speziale P, Campoccia D, Ravaioli S, Cangini I, Pietrocola G, Giannini S, Arciola CR (2011) Scenery of Staphylococcus implant infections in orthopedics. Future Microbiol 6:1329–1349. https://doi.org/10.2217/fmb.11.117
Monzon M, Oteiza C, Leiva J, Amorena B (2001) Synergy of different antibiotic combinations in biofilms of Staphylococcus epidermidis. J Antimicrob Chemother 48:793–801. https://doi.org/10.1093/jac/48.6.793
Muslim SN, Al Kadmy IMS, Ali ANM, Salman BK, Ahmad M, Khazaal SS, Hussein NH, Muslim SN (2018) Chitosan extracted from Aspergillus flavus shows synergistic effect, eases quorum sensing mediated virulence factors and biofilm against nosocomial pathogen Pseudomonas aeruginosa. Int J Biol Macromol 107:52–58. https://doi.org/10.1016/j.ijbiomac.2017.08.146
Nesuta O, Hexnerova R, Budesinsky M, Slaninova J, Bednarova L, Hadravova R, Straka J, Veverka V, Cerovsky V (2016) Antimicrobial peptide from the wild bee Hylaeus signatus venom and its analogues: structure-activity study and synergistic effect with antibiotics. J Nat Products 79:1073–1083. https://doi.org/10.1021/acs.jnatprod.5b01129
Peng ZX, Ao HY, Wang L, Guo SR, Tang TT (2015) Quaternised chitosan coating on titanium provides a self-protective surface that prevents bacterial colonisation and implant-associated infections. Rsc Advances 5:54304–54311. https://doi.org/10.1039/c5ra07540h
Pillai CKS, Paul W, Sharma CP (2009) Chitin and chitosan polymers: chemistry, solubility and fiber formation. Prog Polym Sci 34:641–678. https://doi.org/10.1016/j.progpolymsci.2009.04.001
Piras AM, Maisetta G, Sandreschi S, Gazzarri M, Bartoli C, Grassi L, Esin S, Chiellini F, Batoni G (2015) Chitosan nanoparticles loaded with the antimicrobial peptide temporin B exert a long-term antibacterial activity in vitro against clinical isolates of Staphylococcus epidermidis. Front Microbiol 6:372–382. https://doi.org/10.3389/fmicb.2015.00372
Raafat D, von Bargen K, Haas A, Sahl HG (2008) Insights into the mode of action of chitosan as an antibacterial compound. App Environ Microbiol 74:3764–3773. https://doi.org/10.1128/aem.00453-08
Rabea EI, Badawy MET, Stevens CV, Smagghe G, Steurbaut W (2003) Chitosan as antimicrobial agent: applications and mode of action. Biomacromolecules 4:1457–1465. https://doi.org/10.1021/bm034130m
Rinaudo M (2006) Chitin and chitosan: properties and applications. Prog Polym Sci 31:603–632. https://doi.org/10.1016/j.progpolymsci.2006.06.001
Riss TL, Moravec RA, Niles AL, Duellman S, Benink HA, Worzella TJ, Minor L (2013) Cell Viability Assays. Nati C Biotechnol Inf. Eli Lilly & Company and the National Center for Advancing Translational Sciences .
Rubini D, Banu SF, Hari BNV, Devi DR, Gowrishankar S, Pandian SK, Nithyanand P (2018) Chitosan extracted from marine biowaste mitigates staphyloxanthin production and biofilms of Methicillin-resistant Staphylococcus aureus. Food Chem Toxicol 118:733–744. https://doi.org/10.1016/j.fct.2018.06.017
Semedo MC, Karmali A, Fonseca L (2015) A novel colorimetric assay of b-D-glucans in Basidiomycete strains by alcian blue dye in a 96-Well Microtiter Plate. Biotechnol Prog 31:1526–1535. https://doi.org/10.1002/btpr.2163
Shagdarova BT, Il’ina AV, Varlamov VP (2016) Antibacterial activity of alkylated and acylated derivatives of low-molecular weight chitosan. Appl Biochem Micro 52:222–225. https://doi.org/10.1134/s0003683816020149
Shi ZL, Neoh KG, Kang ET, Wang W (2006) Antibacterial and mechanical properties of bone cement impregnated with chitosan nanoparticles. Biomaterials 27:2440–2449. https://doi.org/10.1016/j.biomaterials.2005.11.036
Singh R, Ray D, Das A, Sharma M (2010) Penetration of antibiotics through Staphylococcus aureus and Staphylococcus epidermidis biofilms. J Antimicrob Chemother 65:1955–1958. https://doi.org/10.1093/jac/dkq257
Tam JP, Wang SJ, Wong KH, Tan WL (2015) Antimicrobial Peptides from Plants Pharmaceuticals 8:711–757. https://doi.org/10.3390/ph8040711
Tan HL, Ao HY, Ma R, Lin WT, Tang TT (2014) in vivo effect of quaternized chitosan-loaded polymethylmethacrylate bone cement on methicillin-resistant Staphylococcus epidermidis infection of the tibial metaphysis in a rabbit model. Antimicrob Agents Chemother 58:6016–6023. https://doi.org/10.1128/aac.03489-14
Tan HL, Ma R, Lin CC, Liu ZW, Tang TT (2013) Quaternized chitosan as an antimicrobial agent: antimicrobial activity, mechanism of action and biomedical applications in orthopedics. Int J Mol Sci 14:1854–1869. https://doi.org/10.3390/ijms14011854
Tavaria FK, Costa EM, Gens EJ, Malcata FX, Pintado ME (2013) Influence of abiotic factors on the antimicrobial activity of chitosan. J Dermatol 40:1014–1019. https://doi.org/10.1111/1346-8138.12315
Thomas VL, Sanford BA, Moreno R, Ramsay MA (1997) Enzyme-linked lectinsorbent assay measures N-acetyl-D-glucosamine in matrix of biofilm produced by Staphylococcus epidermidis. Curr Microbiol 35:249–254. https://doi.org/10.1007/s002849900248
Thornton DCO, Fejes EM, DiMarco SF, Clancy KM (2007) Measurement of acid polysaccharides in marine and freshwater samples using alcian blue. Limnol Oceanogr-Meth 5:73–87. https://doi.org/10.4319/lom.2007.5.73
Vaňková E, Kašparová P, Dulíčková N, Čeřovský V (2020a) Combined effect of lasioglossin LL-III derivative with azoles against Candida Albicans virulence factors: biofilm formation, phospholipases, proteases and hemolytic activity. Fems Yeast Res 20:1–16. https://doi.org/10.1093/femsyr/foaa020
Vaňková E, Paldrychová M, Kašparová P, Lokočová K, Kodeš Z, Maťátková O, Kolouchová I, Masák J (2020b) Natural antioxidant pterostilbene as an effective antibiofilm agent, particularly for gram-positive cocci. World J Microbiol Biotech 30:101–114. https://doi.org/10.1007/s11274-020-02876-5
Wang XH, Du YM, Fan LH, Liu H, Hu Y (2005) Chitosan-metal complexes as antimicrobial agent: synthesis, characterization and structure-activity study. Polym Bull 55:105–113. https://doi.org/10.1007/s00289-005-0414-1
Funding
This work was supported by the “Operational Programme Prague—Competitiveness” (CZ.2.16/3.1.00/24503) and the “National Programme of Sustainability I”—NPU I LO1601.
Author information
Authors and Affiliations
Contributions
Conceptualization: Eva Vaňková, Olga Maťátková, Petra Kašparová; Methodology: Petra Kašparová, Eva Vaňková; Formal analysis and investigation: Petra Kašparová, Martin Zmuda; Writing–original draft preparation: Petra Kašparová; Writing–review and editing: Eva Vaňková, Olga Maťátková; Funding acquisition: Olga Maťátková, Jan Masák; Resources: Jan Masák; Supervision: Olga Maťátková, Jan Masák.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kašparová, P., Zmuda, M., Vaňková, E. et al. Low-molecular weight chitosan enhances antibacterial effect of antibiotics and permeabilizes cytoplasmic membrane of Staphylococcus epidermidis biofilm cells. Folia Microbiol 66, 983–996 (2021). https://doi.org/10.1007/s12223-021-00898-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12223-021-00898-6