Abstract
Core binding factor (CBF) acute myeloid leukemia (AML) is the most common cytogenetic subtype of AML, defined by the presence of t(8;21) or inv(16)/t(16;16). The chromosomal aberrations create AML1-ETO and CBFβ-MYH11 fusion genes that disrupt the functions of CBF, an essential transcription factor in hematopoiesis. Despite the relatively good outcome of patients with CBF-AML, only approximately half of the patients are cured with current therapy, indicating the need for improved therapeutic strategies. In this review, we summarize current knowledge regarding altered transcriptional regulation, aberrant signaling pathways, and cooperating genetic events in CBF leukemia, and discuss challenges ahead for translating these findings into the clinic.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
The core binding factor (CBF) is a heterodimeric transcription factor complex, which is composed of a DNA-binding CBFα protein (RUNX1, 2, or 3, also called AML1, 3,or 2, respectively) and a non-DNA-binding CBFβ protein (CBFβ). The α subunits share the RUNT homology domain at the N terminus, which is responsible for binding to both their DNA targets and CBFβ. The C terminus contains domains necessary for transcriptional activation and chromatin association. CBFβ does not bind DNA directly, but enhances the RUNX-DNA interaction. The RUNX1/CBFβ complex is essential for emergence of hematopoietic cells from an endothelial cell stage, and homozygous loss of either RUNX1 or CBFβ alleles resulted in embryonic death with lack of definitive hematopoiesis [1–4]. Deregulation of CBF leads to the development of hematological disorders, including myelodysplastic syndrome (MDS), acute lymphoblastic leukemia, and acute myeloid leukemia (AML). RUNX1 is one of the most frequent targets of chromosomal and genetic alterations in myeloid diseases. AML1-ETO, the fusion protein resulting from the chromosomal translocation t(8;21), is a common mutation associated with AML cases of the French–American–British (FAB)-M2 subtype. CBFβ is altered in AML samples with an inversion in chromosome 16 [inv(16) or t(16;16)], resulting in the fusion gene CBFβ-MYH11. The presence of CBFβ-MYH11 is associated with almost all cases of FAB subtype M4Eo. These AMLs with AML1-ETO or CBFβ-MYH11 fusion genes, so-called CBF-AML, are among the most common cytogenetic subtype of AML, being detected in 15–20% of adult de novo AML cases [5, 6]. Patients with CBF-AML have a relatively favorable prognosis compared with other types of AML patients. Complete remission rate is usually more than 90% for these patients, but approximately half of them eventually relapse [7]. Numerous laboratory and clinical discoveries have revealed the molecular basis of CBF-AML. Nevertheless, targeted therapy directed at specific molecular alterations in these leukemias has not been established. In this review, we summarize current knowledge regarding molecular pathogenesis of CBF leukemia, which provides a foundation for the development of novel therapeutic strategies.
2 Dominant inhibition of RUNX1 function: is it really a critical step for CBF leukemia?
Dominant inhibition of RUNX1 function has been considered as a common and critical pathway for CBF leukemia. In AML1-ETO, the DNA-binding RUNT domain of RUNX1 is joined to ETO, creating a fusion transcript that lacks the RUNX1 transcription activation domain. ETO is a transcriptional repressor that contains 4 Nervy Homology Regions (NHR 1-4), and interacts with several corepressors including nuclear corepressor (N-CoR), SMRT, mSin3A and the histone deacetylases (HDACs), primarily through the NHR2 and NHR4 domains [8–11]. Consequently, AML1-ETO functions as a dominant repressor for many RUNX1-responsive hematopoietic genes. The CBFβ-MYH11 fusion protein retains the RUNX-binding domain in CBFβ and contains an additional RUNX-binding domain in the MYH11, resulting in a higher binding affinity for RUNX1 than wild-type CBFβ [12]. The MYH11 region associates with transcriptional repressors, such as mSin3A and HDACs, thereby repressing RUNX1-mediated gene regulation [13, 14]. In addition, CBFβ-MYH11 plays a dominant negative role by sequestering RUNX1 from its targets in the DNA [15]. The dominant inhibitory effect of these fusion proteins on RUNX1 function was further supported by the results of gene targeted mouse models. Mice heterozygous for an AML1-ETO or a CBFβ-MYH11 allele show a nearly identical phenotype to Runx1 or Cbfβ knockout mice, namely embryonic lethality with a lack of definitive hematopoiesis [16–18]. With these observations, it has been believed that the fusion proteins (AML1-ETO and CBFβ-MYH11) block RUNX1 function, thereby interfering with normal hematopoietic differentiation and inducing a preleukemic condition. However, several recent reports challenged this concept. Knockin mice expressing a CBFβ-MYH11 fusion with a deletion of the RUNX1 high-affinity binding domain developed leukemia quickly despite its inefficient suppression of RUNX1 function [19]. The same group also showed that CBFβ-MYH11 caused Runx1 repression-independent defects in hematopoiesis [20]. These results indicate that RUNX1 inhibition may not be critical for leukemogenesis by CBFβ-MYH11. In addition, no inactivating mutations of RUNX1 have been found in CBF-AML patients, while it is frequently mutated in other types of AML patients (13–32%) [21, 22]. This clinical observation may indicate that CBF leukemia cells require some RUNX1 function for efficient proliferation and survival. Thus, whether the inhibition of RUNX1 function is absolutely required for CBF leukemogenesis remains to be elucidated.
3 Altered transcriptional regulation in CBF leukemia
In addition to their effects on RUNX1 activity, AML1-ETO and CBFβ-MYH11 modulate functions of several other transcription factors, thereby altering global patterns of gene expression. PU.1 is crucial for myeloid differentiation, and its transcriptional activity is repressed by AML1-ETO through physical interaction [23]. CEBPA is an essential gene for granulopoiesis, and AML1-ETO represses CEBPA expression and its DNA binding activity [24]. CEBPA protein expression is also blocked by CBFβ-MYH11 through upregulation of calreticulin, an inhibitor of CEBPA translation [25]. GATA1 is a major erythroid transcription factor, and AML1-ETO represses transcriptional activity of GATA1 by inhibiting its acetylation [26]. Functional suppression of these hematopoietic transcription factors represents a mechanism involved in the differentiation block in CBF-AML. A schematic representing the transcriptional changes associated with CBF fusion expression, as well as the other molecular and epigenetic changes discussed later in this section, is shown in Fig. 1.
Several tumor suppressors are also modulated in CBF leukemia. AML1-ETO transcriptionally represses p14ARF and neurofibromatosis-1 (NF1) expression through dominant inhibitory effects on RUNX1 function [27, 28]. CBFβ-MYH11 displaces RUNX1 from a CBF site in the promoter of p15INK4B and represses its expression [29]. RUNX3, a well-known tumor suppressor in solid tumors, was shown to be a common transcriptional target for repression by AML1-ETO and CBFβ-MYH11. Interestingly, CBFβ-MYH11 represses the RUNX3 promoter through cooperation with RUNX1, indicating again that normal RUNX1 function is required for inv(16) leukemogenesis [30]. In contrast to these tumor suppressors that are downregulated in CBF leukemia, p21WAF1 is upregulated by AML1-ETO at the protein, RNA, and promoter levels [31, 32]. The biological significance of p21waf1 in t(8;21) leukemogenesis is under debate; a study reported that the p21waf1 pathway is involved in blocking leukemogenesis by AML1-ETO [31], while another argued that the activated p21waf1 is critical in preventing exhaustion of leukemic stem cells in AML [33].
Among anti-apoptotic proteins, BCL2 transcription was shown to be upregulated by AML1-ETO [34]. A later study demonstrated that this effect may be dependent on the status of p53 and that t(8;21) patient samples do not uniformly show increased BCL2 expression [35]. Previous studies have also shown that genes involved in DNA repair pathways, such as OGG1 and POLE, were downregulated in AML1-ETO-expressing human hematopoietic cells [36, 37]. The downregulation of DNA repair genes led to increased DNA damage, which could facilitate accumulation of secondary genetic alterations in AML1-ETO leukemia. Interestingly, AML1-ETO-mediated DNA damage response is p53 dependent, suggesting that activation of the p53 pathway may be associated with improved prognosis of t(8;21)-AML [37]. Furthermore, AML1-ETO represses E protein transcription factors, including E2A, E2-2, and HEB, through ETO-mediated protein interaction and displacement of p300/CBP coactivators [38, 39]. Thus, the upregulation of anti-apoptotic factors, downregulation of DNA repair genes, and repression of E protein function may contribute to CBF leukemogenesis.
Accumulating evidence suggests that epigenetic regulation is involved in the deregulated gene expression in CBF leukemia. A recent large-scale study of DNA methylation profiles for 344 AML patients showed that AML1-ETO and CBFβ-MYH11 leukemia presented unique methylation signatures, with a strong shift toward genes being methylated in CBF-AML compared with normal CD34+ cells [40]. Experimentally, it has been shown that AML1-ETO recruits HDACs and DNA-methyltrasferase 1 (DNMT1) for transcriptional repression [8, 9, 41], implying that transcriptional silencing by AML1-ETO occurs through combinatorial effects of histone deacetylation and promoter DNA methylation. Interestingly, another recent study showed that normal human CD34+ cells expressing one or the other CBF fusion protein did not recapitulate the DNA methylation profile found in CBF-AML samples, indicating that additional cooperating effects may be important in addition to the leukemia fusion protein itself to effect the final transformational methylation profile found in patient samples [42]. Recently, a number of studies have implicated microRNA (miRNA) as an additional epigenetic target for CBF leukemogenesis. It was shown that miRNA-223, which is involved in myelopoiesis, is a direct transcriptional target of AML1-ETO. The repressive effect of AML1-ETO on miRNA-223 gene includes both histone deacetylation and DNA methylation, and demethylating treatment with 5-azacytidine enhanced miRNA-223 expression and also restored myeloid differentiation [43]. Furthermore, one study which assessed 260 miRNA gene expression patterns in 215 AML patients revealed that AML1-ETO and CBFβ-MYH11 leukemia showed distinctive miRNA signatures [44]. An independent study using 52 AML samples containing common recurrent translocations similarly found that the CBF-AML patient samples were associated with distinct miRNA signatures, including elevated expression of miR-126/126* [45]. The molecular and biological consequences of the altered epigenetic status and miRNA expression in CBF leukemia await further studies.
4 Aberrant signaling pathways in CBF leukemia
The deregulated signaling pathways in CBF leukemia could be good therapeutic targets. It has been shown that AML1-ETO upregulates several genes involved in specific signaling pathways. Among them, Jagged1 upregulation suggests that the Notch pathway may be affected [36], while induction of Plakoglobin (γ-Catenin) and β-Catenin indicates the activation of Wnt signaling in AML1-ETO-expressing cells [46]. In addition, tyrosine kinase receptor type 1 (TrkA), a receptor for nerve growth factor (NGF), is upregulated by AML1-ETO, allowing NGF-induced expansion of AML1-ETO-expressing human hematopoietic cells [47]. A zebrafish model combined with chemical library screening revealed cyclooxygenase (Cox)-mediated production of prostaglandin E2 (PGE2) as a critical pathway to prevent differentiation of AML1-ETO-expressing cell [48]. More recently, a study using Drosophila as a model showed that AML1-ETO-expressing precursor cells express high levels of reactive oxygen species (ROS), and that ROS plays a central role in the proliferation of these precursors [49]. As for CBFβ-MYH11 leukemia, gene expression profiling of AML-M4 subtype suggested a highly activated NF-kB pathway in inv(16) patients [50]. Given that these pathways, particularly Notch, Wnt, and Cox/PGE2 signaling, are essential for stem cell self-renewal, these pathways could contribute to a self-renewal signal of leukemia stem cells (LSCs) in CBF-AML. Indeed, it was recently shown that the Wnt pathway is required for LSC development using mouse models of AML induced either by coexpression of Hoxa9/Meis1 or by the fusion oncoprotein MLL-AF9 [51]. Identification of the crucial pathways for LSC development/maintenance in CBF leukemia will be an important future challenge.
5 Cooperating genetic events for CBF leukemia
Although AML1-ETO and CBFβ-MYH11 play an essential role in CBF leukemogenesis, it appears that they alone are not sufficient for leukemogenic transformation and require additional genetic events to develop leukemia. Transgenic or conditional expression of the fusion proteins was not able to induce AML in mice [18, 52, 53]. In line with this, retroviral expression of the fusion proteins in human CD34+ cells did not cause leukemia in immunodeficient mice, while it promoted the expansion of hematopoietic cells in vitro [54–57].
Chromosomal aberrations are frequently detected in CBF leukemia, being present in approximately 70% of t(8;21) and 40% of inv(16)/t(16;16) patients [58]. Distinctive patterns of chromosomal aberrations were found in CBF-AMLs, including −X, −Y, del(9q) exclusively in t(8;21)-AML, while +13, +21, +22 were common events in inv(16)-AML. Loss of a sex chromosome (−X or −Y) in t(8;21) occurred at diagnosis and persisted at relapse and was always present as the dominant clone, suggesting a significant role of this aberration in t(8;21)-AML. In contrast, +13 and +22 in inv(16)-AML are often subclonal at diagnosis, increase in frequency with relapse, and are sometimes lost during disease progression [59]. The molecular basis of these chromosomal aberrations is largely unknown with a few exceptions. TLE1 and TLE4 were suggested as candidate tumor suppressors residing in the genomic region lost in t(8;21) patients with del(9q) [60]. For +22 in inv(16)-AML, MN1, which is located on chromosome 22, is a good candidate for dose deregulation. MN1 is highly expressed in inv(16) with +22, and cells coexpressing CBFβ-MYH11 and MN1 quickly develop AML in mice [61].
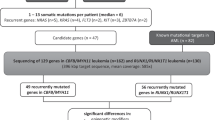
In addition to chromosome copy number changes, mutations of receptor tyrosine kinases (RTKs) and Ras genes, including KIT, FLT3, NRAS/KRAS, have been frequently detected in CBF leukemia. Activating mutations of KIT are quite prevalent in CBF leukemias (up to 40%) [62–64], suggesting a functional collaboration between KIT and the CBF fusion proteins. In fact, a recent study has confirmed that AML1-ETO and mutated KIT are able to transform murine bone marrow cells to AML [65]. Mutations in the FLT3 gene are the most frequent genetic aberration in AML. The internal tandem duplication (ITD) mutations at the juxtamembrane domain are relatively infrequent in CBF-AML, but the D835Y mutation in the kinase domain has been frequently detected in CBF-AML, particularly in inv(16) patients [2–7% in t(8;21) AML and 6–24% in inv(16) AML] [62, 66, 67]. It was also shown that cotransduction of FLT3-ITD and the CBF fusion proteins promote progression to AML using a mouse transplantation model [68, 69]. Mutations in the Ras family of proto-oncogenes (H-Ras, N-Ras and K-Ras) are very common in all human tumors. In CBF-AML, mutations of NRAS and, less often, KRAS, are common among inv(16) patients, being detected in over one-third of them. RAS mutations are also present in 10% of t(8;21) patients [62, 70]. Experimental evidence for the cooperation between RAS and AML1-ETO was recently provided with a primary human cell model system [71]. The high frequency of these mutations fits well to the classical two hit model of leukemogenesis [72], in which one class of mutations (Class I; KIT, FLT3, RAS) confers a proliferative or survival advantage to cells, and a second class of mutations (Class II; AML1-ETO, CBFβ-MYH11) interferes with hematopoietic differentiation. The specific Class I alterations and genetic aberrations that are most frequently associated with CBF-AML are illustrated in Fig. 2.
Cooperating genetic events in CBF leukemia. The CBF fusion proteins are not sufficient for leukemogenic transformation and require additional genetic events to develop AML. Loss of sex chromosome and del(9q) are frequently detected in AML1-ETO leukemia, while +13, +21, +22 are more prevalent in CBFβ-MYH11 leukemia. Mutations in KIT, FLT3, NRAS/KRAS and +8 are common genetic events in both types of leukemia
Another interesting molecular event implicated in CBF leukemogenesis is the loss of putative tumor suppressor activities present within the ETO portion of AML1-ETO. A mouse retroviral transduction-transplantation experiment showed that AML1-ETO with a C-terminal truncation mutation, deleting the NHR3 and 4 domains of ETO, gained a strong leukemogenic activity [73]. In humans, an alternatively spliced isoform of the fusion gene, AML1-ETO9a, has been identified in t(8;21) patients. AML1-ETO9a lacks NHR3 and 4 domains, and similar to the above mutant, has a strong leukemogenic potential [74]. Thus, it appears that the C-terminal portion of AML1-ETO has some tumor suppressor functions, and loss of that region transforms AML1-ETO into a potent leukemogenic protein. However, the enhanced leukemogenic activity of AML1-ETO9a has been shown only in mouse models, and its functions in primary human hematopoietic cells remain to be demonstrated.
6 Future therapeutic strategies for CBF leukemia
Because of toxicity and intrinsic disease resistance, cytotoxic chemotherapy has reached its limit in the treatment of AML patients. We therefore need new therapeutic strategies for AML. However, to begin, we should clarify the mechanisms of improved outcomes for CBF-AML patients even with conventional chemotherapy. Significant in this regard are the observations showing p53 upregulation in t(8;21) AML, which is potentially important for the favorable response to chemotherapy [37, 75]. Whether the p53 pathway is inactivated in relapsed CBF-AML patients, and whether p53 activating drugs are effective for those relapsed patients should be examined in the future. Given the high frequency of mutations in RTKs (KIT and FLT3) and RAS, blocking these signaling pathways using specific inhibitors may be a promising therapeutic strategy. To make the best use of these inhibitors, patient stratification based on gene mutation or pathway activation status will be important. In addition, the altered transcriptional regulation evident in CBF leukemia could be a good therapeutic target. Among so many deregulated genes, repression of RUNX1 function has been considered as a critical step for CBF leukemogenesis. However, as we mentioned above, the precise roles of RUNX1 in CBF leukemia remain uncertain and should be clarified. Epigenetic inhibitors of DNA methylation, histone deacetylation, and histone methylation, may have a better chance to reset the deregulated transcription in CBF leukemia rather than targeting individual molecules.
The simplest therapeutic strategy for CBF leukemia is targeting the fusion proteins themselves. RUNT domain/CBFβ interaction has been considered important for the development of CBF leukemia [76], and a small molecule that allosterically inhibits RUNT/CBFβ binding has already been developed [77]. However, a recent study reported that the transforming activity of AML1-ETO is independent of CBFβ interaction and instead requires formation of homo-oligomeric complexes through the NHR2 domain of ETO portion [78]. This controversy currently remains unresolved [79, 80]. Nevertheless, blocking the homo-oligomeric properties of AML1-ETO could be an alternative or additional strategy to suppress its leukemogenic activity. In theory, combined therapies using inhibitors targeting both RUNT/CBFβ interaction and oligomerization will provide sufficient efficacy and specificity. Furthermore, recent advances in nanoparticle delivery systems enabled RNAi-mediated gene inhibition in specific tissues and organs [81]. In the future, this technique could be applied to leukemia therapy to specifically inhibit leukemia-associated genes, including AML1-ETO and CBFβ-MYH11 (Fig. 3).
Ongoing and future therapeutic approach for CBF leukemia. Molecular pathology of CBF leukemia provides potential therapeutic targets. Those include RNAi-mediated knockdown of the fusion proteins, block of RUNT/CBFβ interaction or oligomerization, and targeting altered transcription or aberrantly activated signaling pathways by specific inhibitors. CBF core binding factor, RTKs receptor tyrosine kinases
7 Concluding remarks
With the accumulating evidence for molecular pathogenesis of CBF leukemia, it is now crucial to translate our understanding into the clinic. Several small molecules targeting a specific pathway have been under testing in clinical trials, and many more will be tested in the near future. We should examine the results carefully to determine how effective each drug is, and which patients with CBF-AML benefit from each therapy. Furthermore, we should develop better experimental models with primary human cells and patient samples to faithfully recapitulate human diseases [82, 83]. Such models will become extremely useful for preclinical evaluation of candidate drugs. Translational research, which integrates molecular pathogenesis with clinical trials, will provide new and better therapies to patients with CBF leukemia.
References
Okuda T, van Deursen J, Hiebert SW, Grosveld G, Downing JR. AML1, the target of multiple chromosomal translocations in human leukemia, is essential for normal fetal liver hematopoiesis. Cell. 1996;84:321–30.
Wang Q, Stacy T, Binder M, Marin-Padilla M, Sharpe AH, Speck NA. Disruption of the Cbfa2 gene causes necrosis and hemorrhaging in the central nervous system and blocks definitive hematopoiesis. Proc Natl Acad Sci USA. 1996;93:3444–9.
Wang Q, Stacy T, Miller JD, Lewis AF, Gu TL, Huang X, et al. The CBFbeta subunit is essential for CBFalpha2 (AML1) function in vivo. Cell. 1996;87:697–708.
Sasaki K, Yagi H, Bronson RT, Tominaga K, Matsunashi T, Deguchi K, et al. Absence of fetal liver hematopoiesis in mice deficient in transcriptional coactivator core binding factor beta. Proc Natl Acad Sci USA. 1996;93:12359–63.
Speck NA, Gilliland DG. Core-binding factors in haematopoiesis and leukaemia. Nat Rev Cancer. 2002;2:502–13.
Wakui M, Kuriyama K, Miyazaki Y, Hata T, Taniwaki M, Ohtake S, et al. Diagnosis of acute myeloid leukemia according to the WHO classification in the Japan Adult Leukemia Study Group AML-97 protocol. Int J Hematol. 2008;87:144–51.
Schlenk RF, Benner A, Krauter J, Buchner T, Sauerland C, Ehninger G, et al. Individual patient data-based meta-analysis of patients aged 16 to 60 years with core binding factor acute myeloid leukemia: a survey of the German Acute Myeloid Leukemia Intergroup. J Clin Oncol. 2004;22:3741–50.
Wang J, Hoshino T, Redner RL, Kajigaya S, Liu JM. ETO, fusion partner in t(8;21) acute myeloid leukemia, represses transcription by interaction with the human N-CoR/mSin3/HDAC1 complex. Proc Natl Acad Sci USA. 1998;95:10860–5.
Amann JM, Nip J, Strom DK, Lutterbach B, Harada H, Lenny N, et al. ETO, a target of t(8;21) in acute leukemia, makes distinct contacts with multiple histone deacetylases and binds mSin3A through its oligomerization domain. Mol Cell Biol. 2001;21:6470–83.
Lutterbach B, Westendorf JJ, Linggi B, Patten A, Moniwa M, Davie JR, et al. ETO, a target of t(8;21) in acute leukemia, interacts with the N-CoR and mSin3 corepressors. Mol Cell Biol. 1998;18:7176–84.
Gelmetti V, Zhang J, Fanelli M, Minucci S, Pelicci PG, Lazar MA. Aberrant recruitment of the nuclear receptor corepressor-histone deacetylase complex by the acute myeloid leukemia fusion partner ETO. Mol Cell Biol. 1998;18:7185–91.
Lukasik SM, Zhang L, Corpora T, Tomanicek S, Li Y, Kundu M, et al. Altered affinity of CBF beta-SMMHC for Runx1 explains its role in leukemogenesis. Nat Struct Biol. 2002;9:674–9.
Lutterbach B, Hou Y, Durst KL, Hiebert SW. The inv(16) encodes an acute myeloid leukemia 1 transcriptional corepressor. Proc Natl Acad Sci USA. 1999;96:12822–7.
Durst KL, Lutterbach B, Kummalue T, Friedman AD, Hiebert SW. The inv(16) fusion protein associates with corepressors via a smooth muscle myosin heavy-chain domain. Mol Cell Biol. 2003;23:607–19.
Shigesada K, van de Sluis B, Liu PP. Mechanism of leukemogenesis by the inv(16) chimeric gene CBFB/PEBP2B-MHY11. Oncogene. 2004;23:4297–307.
Yergeau DA, Hetherington CJ, Wang Q, Zhang P, Sharpe AH, Binder M, et al. Embryonic lethality and impairment of haematopoiesis in mice heterozygous for an AML1-ETO fusion gene. Nat Genet. 1997;15:303–6.
Okuda T, Cai Z, Yang S, Lenny N, Lyu CJ, van Deursen JM, et al. Expression of a knocked-in AML1-ETO leukemia gene inhibits the establishment of normal definitive hematopoiesis and directly generates dysplastic hematopoietic progenitors. Blood. 1998;91:3134–43.
Castilla LH, Garrett L, Adya N, Orlic D, Dutra A, Anderson S, et al. The fusion gene Cbfb-MYH11 blocks myeloid differentiation and predisposes mice to acute myelomonocytic leukaemia. Nat Genet. 1999;23:144–6.
Kamikubo Y, Zhao L, Wunderlich M, Corpora T, Hyde RK, Paul TA, et al. Accelerated leukemogenesis by truncated CBF beta-SMMHC defective in high-affinity binding with RUNX1. Cancer Cell. 2010;17:455–68.
Hyde RK, Kamikubo Y, Anderson S, Kirby M, Alemu L, Zhao L, et al. Cbfb/Runx1 repression-independent blockage of differentiation and accumulation of Csf2rb-expressing cells by Cbfb-MYH11. Blood. 2010;115:1433–43.
Tang JL, Hou HA, Chen CY, Liu CY, Chou WC, Tseng MH, et al. AML1/RUNX1 mutations in 470 adult patients with de novo acute myeloid leukemia: prognostic implication and interaction with other gene alterations. Blood. 2009;114:5352–61.
Schnittger S, Dicker F, Kern W, Wendland N, Sundermann J, Alpermann T, et al. RUNX1 mutations are frequent in de novo AML with non complex karyotype and confer an unfavourable prognosis. Blood. 2011;117:2348–57.
Vangala RK, Heiss-Neumann MS, Rangatia JS, Singh SM, Schoch C, Tenen DG, et al. The myeloid master regulator transcription factor PU.1 is inactivated by AML1-ETO in t(8;21) myeloid leukemia. Blood. 2003;101:270–7.
Pabst T, Mueller BU, Harakawa N, Schoch C, Haferlach T, Behre G, et al. AML1-ETO downregulates the granulocytic differentiation factor C/EBPalpha in t(8;21) myeloid leukemia. Nat Med. 2001;7:444–51.
Helbling D, Mueller BU, Timchenko NA, Schardt J, Eyer M, Betts DR, et al. CBFB-SMMHC is correlated with increased calreticulin expression and suppresses the granulocytic differentiation factor CEBPA in AML with inv(16). Blood. 2005;106:1369–75.
Choi Y, Elagib KE, Delehanty LL, Goldfarb AN. Erythroid inhibition by the leukemic fusion AML1-ETO is associated with impaired acetylation of the major erythroid transcription factor GATA-1. Cancer Res. 2006;66:2990–6.
Linggi B, Muller-Tidow C, van de Locht L, Hu M, Nip J, Serve H, et al. The t(8;21) fusion protein, AML1 ETO, specifically represses the transcription of the p14(ARF) tumor suppressor in acute myeloid leukemia. Nat Med. 2002;8:743–50.
Yang G, Khalaf W, van de Locht L, Jansen JH, Gao M, Thompson MA, et al. Transcriptional repression of the Neurofibromatosis-1 tumor suppressor by the t(8;21) fusion protein. Mol Cell Biol. 2005;25:5869–79.
Markus J, Garin MT, Bies J, Galili N, Raza A, Thirman MJ, et al. Methylation-independent silencing of the tumor suppressor INK4b (p15) by CBFbeta-SMMHC in acute myelogenous leukemia with inv(16). Cancer Res. 2007;67:992–1000.
Cheng CK, Li L, Cheng SH, Lau KM, Chan NP, Wong RS, et al. Transcriptional repression of the RUNX3/AML2 gene by the t(8;21) and inv(16) fusion proteins in acute myeloid leukemia. Blood. 2008;112:3391–402.
Peterson LF, Yan M, Zhang DE. The p21Waf1 pathway is involved in blocking leukemogenesis by the t(8;21) fusion protein AML1-ETO. Blood. 2007;109:4392–8.
Berg T, Fliegauf M, Burger J, Staege MS, Liu S, Martinez N, et al. Transcriptional upregulation of p21/WAF/Cip1 in myeloid leukemic blasts expressing AML1-ETO. Haematologica. 2008;93:1728–33.
Viale A, De Franco F, Orleth A, Cambiaghi V, Giuliani V, Bossi D, et al. Cell-cycle restriction limits DNA damage and maintains self-renewal of leukaemia stem cells. Nature. 2009;457:51–6.
Klampfer L, Zhang J, Zelenetz AO, Uchida H, Nimer SD. The AML1/ETO fusion protein activates transcription of BCL-2. Proc Natl Acad Sci USA. 1996;93:14059–64.
Banker DE, Radich J, Becker A, Kerkof K, Norwood T, Willman C, et al. The t(8;21) translocation is not consistently associated with high Bcl-2 expression in de novo acute myeloid leukemias of adults. Clin Cancer Res. 1998;4:3051–62.
Alcalay M, Meani N, Gelmetti V, Fantozzi A, Fagioli M, Orleth A, et al. Acute myeloid leukemia fusion proteins deregulate genes involved in stem cell maintenance and DNA repair. J Clin Invest. 2003;112:1751–61.
Krejci O, Wunderlich M, Geiger H, Chou FS, Schleimer D, Jansen M, et al. p53 signaling in response to increased DNA damage sensitizes AML1-ETO cells to stress-induced death. Blood. 2008;111:2190–9.
Zhang J, Kalkum M, Yamamura S, Chait BT, Roeder RG. E protein silencing by the leukemogenic AML1-ETO fusion protein. Science. 2004;305:1286–9.
Plevin MJ, Zhang J, Guo C, Roeder RG, Ikura M. The acute myeloid leukemia fusion protein AML1-ETO targets E proteins via a paired amphipathic helix-like TBP-associated factor homology domain. Proc Natl Acad Sci USA. 2006;103:10242–7.
Figueroa ME, Lugthart S, Li Y, Erpelinck-Verschueren C, Deng X, Christos PJ, et al. DNA methylation signatures identify biologically distinct subtypes in acute myeloid leukemia. Cancer Cell. 2010;17:13–27.
Liu S, Shen T, Huynh L, Klisovic MI, Rush LJ, Ford JL, et al. Interplay of RUNX1/MTG8 and DNA methyltransferase 1 in acute myeloid leukemia. Cancer Res. 2005;65:1277–84.
Alvarez S, Suela J, Valencia A, Fernandez A, Wunderlich M, Agirre X, et al. DNA methylation profiles and their relationship with cytogenetic status in adult acute myeloid leukemia. PLoS One. 2010;5:e12197.
Fazi F, Racanicchi S, Zardo G, Starnes LM, Mancini M, Travaglini L, et al. Epigenetic silencing of the myelopoiesis regulator microRNA-223 by the AML1/ETO oncoprotein. Cancer Cell. 2007;12:457–66.
Jongen-Lavrencic M, Sun SM, Dijkstra MK, Valk PJ, Lowenberg B. MicroRNA expression profiling in relation to the genetic heterogeneity of acute myeloid leukemia. Blood. 2008;111:5078–85.
Li Z, Lu J, Sun M, Mi S, Zhang H, Luo RT, et al. Distinct microRNA expression profiles in acute myeloid leukemia with common translocations. Proc Natl Acad Sci USA. 2008;105:15535–40.
Muller-Tidow C, Steffen B, Cauvet T, Tickenbrock L, Ji P, Diederichs S, et al. Translocation products in acute myeloid leukemia activate the Wnt signaling pathway in hematopoietic cells. Mol Cell Biol. 2004;24:2890–904.
Mulloy JC, Jankovic V, Wunderlich M, Delwel R, Cammenga J, Krejci O, et al. AML1-ETO fusion protein up-regulates TRKA mRNA expression in human CD34 + cells, allowing nerve growth factor-induced expansion. Proc Natl Acad Sci USA. 2005;102:4016–21.
Yeh JR, Munson KM, Elagib KE, Goldfarb AN, Sweetser DA, Peterson RT. Discovering chemical modifiers of oncogene-regulated hematopoietic differentiation. Nat Chem Biol. 2009;5:236–43.
Sinenko SA, Hung T, Moroz T, Tran QM, Sidhu S, Cheney MD, et al. Genetic manipulation of AML1-ETO-induced expansion of hematopoietic precursors in a Drosophila model. Blood. 2010;116:4612–20.
Sun X, Zhang W, Ramdas L, Stivers DN, Jones DM, Kantarjian HM, et al. Comparative analysis of genes regulated in acute myelomonocytic leukemia with and without inv(16)(p13q22) using microarray techniques, real-time PCR, immunohistochemistry, and flow cytometry immunophenotyping. Mod Pathol. 2007;20:811–20.
Wang Y, Krivtsov AV, Sinha AU, North TE, Goessling W, Feng Z, et al. The Wnt/beta-catenin pathway is required for the development of leukemia stem cells in AML. Science. 2010;327:1650–3.
Yuan Y, Zhou L, Miyamoto T, Iwasaki H, Harakawa N, Hetherington CJ, et al. AML1-ETO expression is directly involved in the development of acute myeloid leukemia in the presence of additional mutations. Proc Natl Acad Sci USA. 2001;98:10398–403.
Higuchi M, O’Brien D, Kumaravelu P, Lenny N, Yeoh EJ, Downing JR. Expression of a conditional AML1-ETO oncogene bypasses embryonic lethality and establishes a murine model of human t(8;21) acute myeloid leukemia. Cancer Cell. 2002;1:63–74.
Mulloy JC, Cammenga J, MacKenzie KL, Berguido FJ, Moore MA, Nimer SD. The AML1-ETO fusion protein promotes the expansion of human hematopoietic stem cells. Blood. 2002;99:15–23.
Mulloy JC, Cammenga J, Berguido FJ, Wu K, Zhou P, Comenzo RL, et al. Maintaining the self-renewal and differentiation potential of human CD34+ hematopoietic cells using a single genetic element. Blood. 2003;102:4369–76.
Wunderlich M, Krejci O, Wei J, Mulloy JC. Human CD34+ cells expressing the inv(16) fusion protein exhibit a myelomonocytic phenotype with greatly enhanced proliferative ability. Blood. 2006;108:1690–7.
Tonks A, Pearn L, Tonks AJ, Pearce L, Hoy T, Phillips S, et al. The AML1-ETO fusion gene promotes extensive self-renewal of human primary erythroid cells. Blood. 2003;101:624–32.
Mrozek K, Marcucci G, Paschka P, Bloomfield CD. Advances in molecular genetics and treatment of core-binding factor acute myeloid leukemia. Curr Opin Oncol. 2008;20:711–8.
Jones D, Yao H, Romans A, Dando C, Pierce S, Borthakur G, et al. Modeling interactions between leukemia-specific chromosomal changes. Somatic mutations, and gene expression patterns during progression of core-binding factor leukemias. Genes Chromosomes Cancer. 2010;49:182–91.
Dayyani F, Wang J, Yeh JR, Ahn EY, Tobey E, Zhang DE, et al. Loss of TLE1 and TLE4 from the del(9q) commonly deleted region in AML cooperates with AML1-ETO to affect myeloid cell proliferation and survival. Blood. 2008;111:4338–47.
Carella C, Bonten J, Sirma S, Kranenburg TA, Terranova S, Klein-Geltink R, et al. MN1 overexpression is an important step in the development of inv(16) AML. Leukemia. 2007;21:1679–90.
Boissel N, Leroy H, Brethon B, Philippe N, de Botton S, Auvrignon A, et al. Incidence and prognostic impact of c-Kit, FLT3, and Ras gene mutations in core binding factor acute myeloid leukemia (CBF-AML). Leukemia. 2006;20:965–70.
Carlsson IB, Laitinen MP, Scott JE, Louhio H, Velentzis L, Tuuri T, et al. Kit ligand and c-Kit are expressed during early human ovarian follicular development and their interaction is required for the survival of follicles in long-term culture. Reproduction. 2006;131:641–9.
Shih LY, Liang DC, Huang CF, Chang YT, Lai CL, Lin TH, et al. Cooperating mutations of receptor tyrosine kinases and Ras genes in childhood core-binding factor acute myeloid leukemia and a comparative analysis on paired diagnosis and relapse samples. Leukemia. 2008;22:303–7.
Wang YY, Zhao LJ, Wu CF, Liu P, Shi L, Liang Y, et al. C-KIT mutation cooperates with full-length AML1-ETO to induce acute myeloid leukemia in mice. Proc Natl Acad Sci USA. 2011;108:2450–5.
Schnittger S, Schoch C, Dugas M, Kern W, Staib P, Wuchter C, et al. Analysis of FLT3 length mutations in 1003 patients with acute myeloid leukemia: correlation to cytogenetics, FAB subtype, and prognosis in the AMLCG study and usefulness as a marker for the detection of minimal residual disease. Blood. 2002;100:59–66.
Thiede C, Steudel C, Mohr B, Schaich M, Schakel U, Platzbecker U, et al. Analysis of FLT3-activating mutations in 979 patients with acute myelogenous leukemia: association with FAB subtypes and identification of subgroups with poor prognosis. Blood. 2002;99:4326–35.
Kim HG, Kojima K, Swindle CS, Cotta CV, Huo Y, Reddy V, et al. FLT3-ITD cooperates with inv(16) to promote progression to acute myeloid leukemia. Blood. 2008;111:1567–74.
Schessl C, Rawat VP, Cusan M, Deshpande A, Kohl TM, Rosten PM, et al. The AML1-ETO fusion gene and the FLT3 length mutation collaborate in inducing acute leukemia in mice. J Clin Invest. 2005;115:2159–68.
Bacher U, Haferlach T, Schoch C, Kern W, Schnittger S. Implications of NRAS mutations in AML: a study of 2502 patients. Blood. 2006;107:3847–53.
Chou FS, Wunderlich M, Griesinger A, Mulloy JC. NRASG12D induces stepwise transformation in preleukemic human umbilical cord blood cultures expressing the AML1-ETO fusion gene. Blood. 2011;117:2237–40.
Gilliland DG, Jordan CT, Felix CA, The molecular basis of leukemia. Hematology Am Soc Hematol Educ Program 2004;80–97.
Yan M, Burel SA, Peterson LF, Kanbe E, Iwasaki H, Boyapati A, et al. Deletion of an AML1-ETO C-terminal NcoR/SMRT-interacting region strongly induces leukemia development. Proc Natl Acad Sci USA. 2004;101:17186–91.
Yan M, Kanbe E, Peterson LF, Boyapati A, Miao Y, Wang Y, et al. A previously unidentified alternatively spliced isoform of t(8;21) transcript promotes leukemogenesis. Nat Med. 2006;12:945–9.
Zuber J, Radtke I, Pardee TS, Zhao Z, Rappaport AR, Luo W, et al. Mouse models of human AML accurately predict chemotherapy response. Genes Dev. 2009;23:877–89.
Roudaia L, Cheney MD, Manuylova E, Chen W, Morrow M, Park S, et al. CBFbeta is critical for AML1-ETO and TEL-AML1 activity. Blood. 2009;113:3070–9.
Gorczynski MJ, Grembecka J, Zhou Y, Kong Y, Roudaia L, Douvas MG, et al. Allosteric inhibition of the protein-protein interaction between the leukemia-associated proteins Runx1 and CBFbeta. Chem Biol. 2007;14:1186–97.
Kwok C, Zeisig BB, Qiu J, Dong S, So CW. Transforming activity of AML1-ETO is independent of CBFbeta and ETO interaction but requires formation of homo-oligomeric complexes. Proc Natl Acad Sci USA. 2009;106:2853–8.
Park S, Speck NA, Bushweller JH. The role of CBFbeta in AML1-ETO’s activity. Blood. 2009;114:2849–50.
Kwok C, Zeisig BB, Dong S, So CW. The role of CBFbeta in AML1-ETO’s activity. Blood. 2010;115:3176–7.
Davis ME, Zuckerman JE, Choi CH, Seligson D, Tolcher A, Alabi CA, et al. Evidence of RNAi in humans from systemically administered siRNA via targeted nanoparticles. Nature. 2010;464:1067–70.
Mulloy JC, Wunderlich M, Zheng Y, Wei J. Transforming human blood stem and progenitor cells: a new way forward in leukemia modeling. Cell Cycle. 2008;7:3314–9.
Wunderlich M, Mulloy JC. Model systems for examining effects of leukemia-associated oncogenes in primary human CD34+ cells via retroviral transduction. Methods Mol Biol. 2009;538:263–85.
Acknowledgments
This work is supported by NIH Grant CA118319 (JCM) and by JSPS Postdoctoral Fellowship for Research Abroad (SG).
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Goyama, S., Mulloy, J.C. Molecular pathogenesis of core binding factor leukemia: current knowledge and future prospects. Int J Hematol 94, 126–133 (2011). https://doi.org/10.1007/s12185-011-0858-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12185-011-0858-z