Abstract
The translocation t(8;21), leading to a fusion between the RUNX1 gene and the RUNX1T1 locus, was the first chromosomal translocation identified in cancer. Since the first description of this balanced rearrangement in a patient with acute myeloid leukemia (AML) in 1973, RUNX1 translocations and point mutations have been found in various myeloid and lymphoid neoplasms. In this chapter, we summarize the currently available data on the clinical relevance of core binding factor gene alterations in hematological disorders. In the first section, we discuss the prognostic implications of the core binding factor translocations RUNX1-RUNX1T1 and CBFB-MYH11 in AML patients. We provide an overview of the cooperating genetic events in patients with CBF-rearranged AML and their clinical implications, and review current treatment approaches for CBF AML and the utility of minimal residual disease monitoring. In the next sections, we summarize the available data on rare RUNX1 rearrangements in various hematologic neoplasms and the role of RUNX1 translocations in therapy-related myeloid neoplasia. The final three sections of the chapter cover the spectrum and clinical significance of RUNX1 point mutations in AML and myelodysplastic syndromes, in familial platelet disorder with associated myeloid malignancy, and in acute lymphoblastic leukemia.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- RUNX1
- Acute myeloid leukemia
- Core binding factor leukemia
- Myelodysplastic syndromes
- Chromosomal translocations
- Point mutations
- Prognosis
1 Introduction
The balanced translocation t(8;21)(q22;q22), initially described by Janet D. Rowley in 1973 in a patient with acute myeloid leukemia (AML), was the first reciprocal chromosomal translocation identified in cancer cells (Rowley 1973). In 1991, Miyoshi and co-workers cloned and sequenced a novel gene, located on the breakpoint on chromosome 21, in AML patients with this translocation (Miyoshi et al. 1991). The gene was initially called AML1, and is now named Runt-related transcription factor 1 (RUNX1) due to its homology with the Drosophila gene Runt. Soon afterwards, it was established that on the molecular level, t(8;21)(q22;q22) leads to the formation of a chimeric fusion transcript that today is named RUNX1-RUNX1T1 (Erickson et al. 1992; Miyoshi et al. 1993). The RUNX1 protein is part of a heterodimeric transcription factor called the “core binding factor”, or CBF. Today, three different DNA-binding CBFα subunits (RUNX1, RUNX2 and RUNX3) and one common non-DNA-binding CBFβ subunit (encoded by the CBFB gene) have been identified in humans (Speck and Gilliland 2002). In 1993, Liu and co-workers identified CBFB and the myosin heavy chain gene MYH11 as the fusion partners in another recurrent balanced chromosomal rearrangement in AML, namely inv(16)(p13q22) and its variant, t(16;16)(p13;q22) (Liu et al. 1993). These seminal discoveries pointed towards an important role of CBF genes not only in normal hematopoiesis, but also in leukemia, and opened the road for further studies revealing that the RUNX1 gene is frequently altered in myeloid malignancies and other hematological disorders through various mechanisms including chromosomal translocations, point mutations and deletions. In this chapter, we will review the clinical and prognostic significance of RUNX1 alterations and the CBFB-MYH11 fusion in AML and other hematological disorders.
2 Balanced Translocations Involving the Core Binding Factor Subunits in AML: t(8;21)(q22;q22); RUNX1-RUNX1T1 and inv(16) (p13q22)/t(16;16)(p13;q22); CBFB-MYH11
2.1 Background
Between 1978 and 1984, the International Workshops on Chromosomes in Leukemia established that t(8;21)(q22;q22) is a recurrent event in AML, and closely linked to M2 morphology according to the French-American-British (FAB) classification (i.e., acute myelogenous leukemia with maturation) (Rowley and de la Chapelle 1978; Rowley 1980; Bloomfield et al. 1984). In subsequent studies, the incidence of the RUNX1-RUNX1T1 rearrangement in adult AML was 4–8% (Slovak et al. 2000; Byrd et al. 2002; Mrózek 2004), and it was 7% in a very large cohort of 5876 patients aged 16–59 years (Grimwade et al. 2010). RUNX1-RUNX1T1 is extremely rare in infants but occurs in 11–14% of children and adolescents, and represents the single most common balanced translocation in pediatric AML (Leverger et al. 1988; Raimondi et al. 1999; Mrózek et al. 2004; von Neuhoff et al. 2010; Harrison et al. 2010). The incidence of RUNX1-RUNX1T1 decreases with age, and the translocation is less frequent in patients aged ≥60 years (Bloomfield et al. 1984; Byrd et al. 2002; Grimwade et al. 2010).
The pericentric inversion inv(16)(p13q22) was first described as a recurrent abnormality in AML in 1983. The original publications described an association with myelomonocytic leukemia with abnormal eosinophils (FAB M4eo), and reported that affected patients had favorable response to treatment (Le Beau et al. 1983; Bloomfield et al. 1984). The incidence of CBFB-MYH11 in adults was 5% in the large British Medical Research Council (MRC) cohort, and 2–9% in other series, and it is found in 6–9% of pediatric AML (Raimondi et al. 1999; Mrózek et al. 2004; Grimwade et al. 2010; von Neuhoff et al. 2010; Harrison et al. 2010). Similar to RUNX1-RUNX1T1, the CBFB-MYH11 fusion is less frequent in older adults (i.e., ≥60 years) (Byrd et al. 2002).
2.2 Prognosis of AML Patients with t(8;21)(q22;q22); RUNX1-RUNX1T1 and inv(16)(p13q22) /t(16;16)(p13;q22); CBFB-MYH11
The reports from the International Workshops on Chromosomes in Leukemia established that karyotype is an important prognostic factor in AML, and revealed that both CBF rearrangements, t(8;21)(q22;q22) and inv(16)(p13q22), associate with relatively favorable outcomes. This finding was confirmed by long-term follow-up of the initial cohorts, although treatment was not uniform in these early series (Rowley 1980; Larson et al. 1983; Bloomfield et al. 1984; Swansbury et al. 1994). Later studies in patients who received more standardized, cytarabine-based induction and consolidation chemotherapy on cooperative group trials consistently showed that patients with CBF rearrangements had higher complete remission (CR) rates compared to patients with cytogenetically normal AML, and longer disease-free survival (DFS) and overall survival (OS) (Keating et al. 1987; Fenaux et al. 1989; Slovak et al. 2000). In a study of 1213 patients enrolled on 5 consecutive Cancer and Leukemia Group B (CALGB) treatment protocols, Byrd and colleagues demonstrated that the RUNX1-RUNX1T1 and CBFB-MYH11 fusions associated with high CR rates (91% and 85%, respectively), a low rate of primary refractory disease, and favorable DFS and OS (Byrd et al. 2002). In a more recent analysis of 5876 younger adults (<60 years) treated on trials of the MRC, RUNX1-RUNX1T1 positive patients had a CR rate of 97% and a 10-year OS of 61%, while those with CBFB-MYH11 had a CR rate of 92% and a 10-year OS of 55% (Fig. 12.1) (Grimwade et al. 2010). When patients with acute promyelocytic leukemia (APL) are excluded, t(8;21)(q22;q22) and inv(16)(p13q22) / t(16;16)(p13;q22) represent the most favorable cytogenetic subset in this very large cohort. In older adults (≥60 years) with CBF leukemias who received at least one cycle of induction chemotherapy, the CR rate was 88%, but 5-year OS was only 31% (Prébet et al. 2009). Pediatric AML patients with CBF rearrangements have excellent outcomes with reported OS rates of ~90% at 5 years and ~80% at 10 years (von Neuhoff et al. 2010; Harrison et al. 2010). Based on these data, it is generally accepted today that the CBF rearrangements, t(8;21)(q22;q22), inv(16)(p13q22) and t(16;16)(p13;q22), define a favorable cytogenetic subset of adult and pediatric AML patients, and this is reflected by current risk stratification systems and international guidelines (Grimwade et al. 2010; Döhner et al. 2010; Creutzig et al. 2012).
Prognosis of AML patients with t(8;21)(q22;q22); RUNX1-RUNX1T1 and inv(16)(p13q22)/t(16;16)(p13;q22); CBFB-MYH11. Overall survival of younger patients (age, 16–59) treated on British Medical Research Council trials, stratified according to cytogenetic findings. Survival for patients with t(8;21) is shown in red and survival for patients with inv(16) is shown in green (Figure reproduced from Grimwade et al. (2010) with permission)
2.3 Role of Cooperating Cytogenetic Changes and Gene Mutations in AML with CBF Gene Rearrangement
Additional chromosomal alterations are found in most AML patients with the translocation t(8;21). Loss of a sex chromosome was identified as the most common secondary alteration in adults and children, followed by deletions in the long arm of chromosome 9 (band 9q22) (Larson et al. 1983; Bloomfield et al. 1984; Raimondi et al. 1999; Kuchenbauer et al. 2006). In a series of 111 adult patients, additional chromosomal abnormalities were found in 70%, including loss of a sex chromosome in 47%, 9q deletion in 15% and trisomy 8 in 6% (Krauth et al. 2014). Loss of a sex chromosome associated with favorable, and trisomy 8 with unfavorable event-free survival (EFS) in this series, although treatment was heterogeneous and the number of patients with +8 was small. Other reports also suggested that specific additional cytogenetic abnormalities, including del(9q) and loss of the Y chromosome in male patients, or RUNX1-RUNX1T1 rearrangement in the context of a complex karyotype, adversely affect the outcomes of RUNX1-RUNX1T1-positive patients (Schoch et al. 1996; Schlenk et al. 2004; Appelbaum et al. 2006). In contrast, several large studies in children and adults demonstrated that the presence of secondary cytogenetic alterations including loss of a sex chromosome, del(9q), or trisomy 8 have no adverse impact on outcomes (Fenaux et al. 1989; Byrd et al. 2002; Grimwade et al. 2010; Harrison et al. 2010). Importantly, patients with RUNX1-RUNX1T1 and CBF-MYH11 have favorable outcomes even when these abnormalities occur within a complex karyotype (Byrd et al. 2002; Grimwade et al. 2010).
In AML patients with inv(16) or t(16;16), the most frequently identified additional cytogenetic alterations are trisomy 22, trisomy 11, and deletions on the short arm of chromosome 7, which are found in 14–19%, 10–16%, and 5–6% of patients, respectively (Schlenk et al. 2004; Marcucci et al. 2005; Grimwade et al. 2010; Paschka et al. 2013). At least three independent studies reported that patients with CBFB-MYH11 and an additional chromosome 22 have a particularly low risk of relapse and favorable survival (Grimwade et al. 2010; Schlenk et al. 2004; Marcucci et al. 2005).
More recent analyses also include information on molecular gene mutations. Data from the German AML Study Group (AMLSG) show that 56% of RUNX1-RUNX1T1 rearranged AML and 84% of CBF-MYH11 rearranged AML harbor mutations in KIT, FLT3, NRAS or KRAS (Paschka and Döhner 2013). The frequency of KIT and FLT3 gene mutations was similar in both subsets of CBF leukemias. KIT mutations were detected in 30% of RUNX1-RUNX1T1 positive cases and 37% CBF-MYH11 positive cases, and FLT3 mutations were present in 13% and 17%, respectively. RAS mutations, however, were more common in AML with CBF-MYH11 (53% vs. 21% in RUNX1-RUNX1T1 rearranged AML). In another analysis of 11 different genes in 139 RUNX1-RUNX1T1-positive AML patients, at least one gene mutation was found in 50%, with KIT, NRAS and ASXL1 being most commonly affected (Krauth et al. 2014).
In 2014, Micol and colleagues discovered novel mutations in the additional sex combs-like 2 (ASXL2) gene in almost a quarter of patients with RUNX1-RUNX1T1 fusion. Notably, mutations in this gene were absent in patients with CBFB-MYH11 rearrangement or mutated RUNX1 (Micol et al. 2014). More comprehensive genetic analyses have revealed that mutations affecting epigenetic modifiers, including ASXL1, ASXL2, EZH2 and KDM6A, the cohesin complex, and the zink finger transcription factor ZBTB7A are common in RUNX1-RUNX1T1 rearranged AML, but rare or absent in patients with CBFB-MYH11 (Hartmann et al. 2016; Duployez et al. 2016; Lavallée et al. 2016; Sood et al. 2016). The prognostic relevance of these mutations in CBF AML remains to be determined. SNP-array studies revealed that submicroscopic copy number alterations are rare in CBF rearranged AML (Kühn et al. 2012). Overall, these data indicate that, while activation of receptor tyrosine kinase signaling pathways is a common mechanism in CBF AML, other cooperating pathways may be specific to patients with either RUNX1-RUNX1T1 or CBFB-MYH1.
2.3.1 Clinical Relevance of KITGene Mutations in CBF AML
Mutations in the KIT receptor tyrosine kinase in AML were first identified by Beghini and colleagues (Beghini et al. 1998), and were subsequently confirmed to be recurrent events in CBF leukemias, while they are rare in other cytogenetic subsets (Gari et al. 1999; Beghini et al. 2000; Schnittger et al. 2006). In some patients, KIT mutations become undetectable in CR while the RUNX1-RUNX1T1 fusion remains detectable using similarly sensitive methods, suggesting that KIT mutations constitute a secondary hit that provides a growth and/or survival advantage to the leukemic cells (Wang et al. 2005). In several cohorts of CBF-rearranged adolescents and adults, KIT mutations were found in 20–47% of RUNX1-RUNX1T1 and 30–45% of CBFB-MYH11 positive patients and tended to associate with higher white blood counts (Care et al. 2003; Beghini et al. 2004; Wang et al. 2005; Cairoli et al. 2006; Paschka et al. 2006; Allen et al. 2013). In RUNX1-RUNX1T1 rearranged AML, most of the mutations are activating missense mutations in the tyrosine kinase domain (exon 17), while mutations in the extracellular domain (exon 8) and the transmembrane and juxtamembrane domains (exons 10 and 11) occur more rarely and have not been analyzed in all studies (Allen et al. 2013). In contrast, exon 8 mutations are more common in patients with CBFB-MYH11 (Paschka et al. 2013; Allen et al. 2013).
In several moderately-sized retrospective series of RUNX1-RUNX1T1-positive AML, KIT-mutated patients had a higher incidence of relapse (70–100%) compared to KIT wild-type patients (~35%), while the results in patients with CBFB-MYH11 were discordant (Schnittger et al. 2006; Cairoli et al. 2006; Paschka et al. 2006; Nanri et al. 2005b; Boissel et al. 2006). In the largest cohort reported so far by the MRC study group, KIT mutations were found in 23% of 199 patients with RUNX1-RUNX1T1 rearrangement. Only “high-level” KIT mutations with a mutant-to-wild type ratio of ≥25% associated with higher relapse risk (41% compared to 25% for KIT wild-type patients), while KIT mutations present at lower levels had no impact on relapse. Of note, FLT3-internal tandem duplications, but not KIT mutations, associated with shorter OS in this cohort (Allen et al. 2013). In contrast, 35% of 155 CBFB-MYH11 rearranged patients in the same study had mutated KIT, and mutation status did not affect RFS or OS. In a large series of CBFB-MYH11 patients from the German AMLSG, KIT mutations negatively affected RFS, but not OS (Paschka et al. 2013).
Collectively, these results establish KIT mutations as a predictor of higher relapse risk in adult RUNX1-RUNX1T1 rearranged AML. KIT mutations were linked to shorter OS in some studies (Schnittger et al. 2006; Cairoli et al. 2006; Boissel et al. 2006) but not in others (Paschka et al. 2006; Allen et al. 2013; Nanri et al. 2005b), suggesting that KIT-mutated patients may respond favorably to salvage therapy. The prognostic relevance of KIT mutations in AML with CBFB-MYH11 is less well established, and there are conflicting reports on the prognostic relevance of KIT mutations in pediatric CBF AML patients (Paschka and Döhner 2013; Pollard et al. 2010).
2.4 Treatment of AML with CBF Leukemias
2.4.1 Chemotherapy and the Role of High-Dose Cytarabine
As outlined above, approximately 90% of adult RUNX1-RUNX1T1-positive AML patients achieve CR with cytarabine- and anthracycline -based (‘7+3’-like) induction chemotherapy. A study from CALGB demonstrated that consolidation therapy with 4 cycles of high-dose cytarabine (HDAC, 3 g/m2 twice daily on days 1,3 and 5), compared to cytarabine doses of 100 or 400 mg/m2/day for 5 days, resulted in prolonged DFS particularly in patients with CBF leukemias (Bloomfield et al. 1998). The same group later showed that patients with RUNX1-RUNX1T1 rearrangement who received three or four cycles of HDAC had superior 5-year DFS (71%) and OS (76%) compared to patients who received only one HDAC course (5 year DFS, 37%; 5-year OS, 44%). In an extended series of 96 RUNX1-RUNX1T1-positive patients, those receiving multiple HDAC courses had a 10 year survival of 56%, compared to 43% for those receiving only a single course (Marcucci et al. 2005). In patients with CBFB-MYH11, exposure to 3–4 HDAC cycles resulted in improved 5-year DFS compared to those receiving only one cycle (57% vs. 30%), with no improvement in OS (Byrd et al. 2004). A favorable impact of 3 cycles of HDAC consolidation, compared to 4 cycles of multiagent chemotherapy with lower-dose cytarabine, on DFS in CBF leukemias was also confirmed by a Japanese trial (Miyawaki et al. 2011). Daunorubicin dose escalation from 45 to 90 mg/m2 during induction resulted in a trend towards improved EFS and OS in older patients (≥60 years) with CBF leukemia (Löwenberg et al. 2009). In a large British randomized trial of mostly younger patients and in a retrospective analysis of two French trials, daunorubicin dose escalation from 60 to 90 mg/m2 during induction was not associated with improved survival in CBF leukemias (Prébet et al. 2014; Burnett et al. 2015). Therefore, ‘7+3’-like induction chemotherapy (preferentially with a daunorubicin dose of 60 mg/m2) followed by 3–4 cycles of HDAC consolidation currently can be considered the standard treatment for adult AML patients with CBF rearrangement, although one study suggested that lower cumulative doses of cytarabine may be sufficient (Löwenberg et al. 2011).
2.4.2 Gemtuzumab Ozogamicin
Gemtuzumab ozogamicin (GO) is an anti-CD33 antibody coupled to the cytotoxic drug calicheamicin. In a subgroup analysis of the British MRC AML15 trial for patients <60 years, addition of a single dose of GO to induction chemotherapy led to significantly improved OS in patients with CBF leukemias (Burnett et al. 2011). A beneficial effect of GO in CBF leukemia patients was confirmed in a large meta-analysis of five randomized trials, which found a 5-year OS of 78% for patients receiving GO compared to 55% for those not receiving GO (Hills et al. 2014). The optimal dose and schedule of GO administration in CBF AML are unknown. GO was withdrawn from the US market due to concerns about early mortality in one trial (Petersdorf et al. 2013), and the drug is currently approved in Japan, but not in the US or Europe.
2.4.3 Allogeneic Stem Cell Transplantation for CBF AML
In a retrospective comparison of 118 AML patients with RUNX1-RUNX1T1 translocation in first CR who underwent allogeneic stem cell transplantation (alloSCT) from a HLA-identical sibling to 132 patients receiving consolidation chemotherapy on German multicenter trials, patients receiving alloSCT had a reduced relapse risk, however, this was offset by increased treatment-related mortality. In summary, relapse-free survival (RFS) tended to be better for those patients receiving chemotherapy (Schlenk et al. 2008). For patients with CBFB-MYH11 rearrangement, a German meta-analysis of 170 patients in first CR also found no RFS benefit of allogeneic SCT over consolidation chemotherapy (Schlenk et al. 2004). Results of a donor-versus-no donor analysis and a large-meta analysis of 24 trials confirmed that AML patients with CBF leukemias do not profit from alloSCT in first CR (Cornelissen et al. 2007; Koreth et al. 2009). While KIT mutations predict a higher relapse risk in RUNX1-RUNX1T1-positive AML, it is unknown whether alloSCT ameliorates this increased risk. Consequently, there is currently no consensus whether KIT-mutated patients should undergo alloSCT in first CR (Allen et al. 2013).
2.4.4 Tyrosine Kinase Inhibitors
Functional analyses of KIT mutations showed that they lead to constitutive activation of the receptor (Cammenga et al. 2005). Furthermore, KIT is overexpressed in RUNX1-RUNX1T1-rearranged AML patients irrespective of its mutation status (Bullinger et al. 2004; Valk et al. 2004). Wild-type and mutant KIT isoforms can be inhibited by various tyrosine kinase inhibitors (TKIs), providing a rationale for therapeutic use of TKIs in t(8;21) AML (Growney et al. 2005; Nanri et al. 2005a; Schittenhelm et al. 2006; Chevalier et al. 2010; Paschka and Döhner 2013). Mutated KIT isoforms exhibit variable sensitivity to different inhibitors. Clinical responses were observed in single patients or small series of patients with advanced disease receiving TKI, including imatinib and dasatinib (Nanri et al. 2005a; Chevalier et al. 2010). However, in a study of 26 high-risk patients with minimal residual disease (MRD) persistence or recurrence, 12 months of dasatinib maintenance did not avert hematological relapse in patients with molecular recurrence, or improve DFS in those with suboptimal MRD response (Boissel et al. 2015). Several prospective studies of dasatinib in CBF leukemias are ongoing.
2.4.5 Treatment of Relapsed Disease
Data from the 6th International Workshop on Chromosomes in Leukemia suggested that relapsed RUNX1-RUNX1T1-positive AML is relatively sensitive to repeated chemotherapy, and second CRs can be achieved in a considerable fraction of patients (Garson et al. 1989). In a retrospective analysis of 59 patients in first relapse, the rate of second CR after salvage chemotherapy was 88%, and 5-year survival after relapse was 51%. Addition of GO to salvage chemotherapy appeared to be beneficial, with a 5 year OS of 65% compared to 44% for those receiving chemotherapy without GO (Hospital et al. 2014). An analysis by the MRC group showed that relapsed RUNX1-RUNX1T1 or CBFB-MYH11 -positive AML patients who received salvage chemotherapy without alloSCT had a 5-year OS of 41% and 47%, respectively, compared to 29 % and 39 % for those receiving an alloSCT, yet this was not a randomized comparison and survival estimates may be biased. Nevertheless, these data indicate that CBF AML frequently remains chemoresponsive at the time of relapse, in contrast to relapsed non-CBF AML which generally is considered incurable without alloSCT (Burnett et al. 2013).
2.5 Minimal Residual Disease Monitoring in CBF AML
The RUNX1-RUNX1T1 and CBFB-MYH11 fusion transcripts can be detected with high sensitivity by RT-PCR, and this technique may be used to detect persisting leukemic cells in patients in clinical remission. However, it has been shown that some patients who have been in morphological CR for up to 8 years still have detectable RUNX1-RUNX1T1 transcripts in the bone marrow (BM) and/or blood, although some studies reported that transcript levels tended to decrease and become undetectable over time (Nucifora et al. 1993; Nucifora and Rowley 1994; Kusec et al. 1994; Satake et al. 1995). Clonogenic progenitor assays revealed that the RUNX1-RUNX1T1 fusion persisted in multipotent hematopoetic progenitor cells that were able to differentiate into mature trilineage myeloid cells and mature B cells in vitro and in vivo (Miyamoto et al. 1996, 2000). These studies indicate that RUNX1-RUNX1T1-positive pre-leukemic stem cells capable of self-renewal and differentiation can persist in the BM during CR, although their frequency gradually decreases over time. Miyamoto studied RUNX1-RUNX1T1-positive patients who had been in CR for 1–12.5 years using a nested RT-PCR assay with a sensitivity of 1:10−7. They found RUNX1-RUNX1T1 transcripts in the BM of all 18 patients treated with chemotherapy only, but in none of the 4 patients who had undergone alloSCT (Miyamoto et al. 1996). Another study, however, reported that RUNX1-RUNX1T1 transcripts were also detectable in 9 of 10 patients in CR after alloSCT (Jurlander et al. 1996). Taken together, these studies establish that RUNX1-RUNX1T1-positive cells can persist at low levels in t(8;21) AML patients who achieve long-term remissions. They also demonstrate that the RUNX1-RUNX1T1 fusion alone is not sufficient to initiate AML, and secondary genetic lesions are needed.
Low-level persistence of RUNX1-RUNX1T1 transcripts in patients who may be cured limits the utility of qualitative (end-point) RT-PCR assays for the detection of clinically meaningful residual disease. Nevertheless, a French multicenter study of 51 patients suggested that many patients in long-term remission ultimately become PCR-negative. Using a less sensitive one-step qualitative PCR technique, this study showed that patients who achieved PCR negativity during follow-up had a relapse rate of 15%, while all patients with persistently positive PCR results relapsed. This study also suggested the possibility of early MRD-based response assessment, since patients who became PCR-negative after induction and before consolidation chemotherapy had a relapse rate of 11%, compared to 72% for the remaining patients (Morschhauser et al. 2000).
The development of quantitative PCR (qPCR) techniques allowed serial monitoring of RUNX1-RUNX1T1 and CBFB-MYH11 transcript levels over time, and establishing critical threshold levels that are predictive of imminent hematological relapse (Tobal and Yin 1996; Marcucci et al. 1998; Krauter et al. 1999; Tobal et al. 2000; Krauter et al. 2003; Buonamici et al. 2002; Leroy et al. 2005). If quantitative MRD monitoring is to be used for clinical decision-making, careful standardization of methods and cut-offs is necessary to ensure comparable results from different laboratories. RNA-based assays for quantitative detection of RUNX1-RUNX1T1, CBFB-MYH11 and other fusion transcripts have been established and validated by multinational consortia including the “Europe against Cancer” (EAC) initiative (van Dongen et al. 1999; Gabert et al. 2003). Of note, since the genomic breakpoints in the RUNX1 locus are distributed over a region of ~25 kilobases, MRD monitoring on genomic DNA requires development of patient-specific assays. While this approach is feasible and offers the conceptual advantage of quantifying the proportion of leukemic cells more directly, it suffers from variable sensitivity and greatly increased complexity, and is thus not widely used (Duployez et al. 2014).
The clinical relevance of MRD measurements by qPCR was demonstrated in several large, uniformly treated patient cohorts analyzed according to the EAC recommendations. The British MRC group studied 278 CBF-AML patients aged 15–70 years, and found that a >3 log reduction of RUNX1-RUNX1T1 transcript levels in BM after the first induction cycle was associated with a cumulative incidence of relapse of only 4% at 5 years, while patients with a lesser reduction had relapse rates exceeding 30%, although this did not translate into significant survival differences. Similarly, detection of <10 CBFB-MYH11 copies per 105 copies of ABL in peripheral blood after induction 1 associated with a relatively low 5-year incidence of relapse (21%) and favorable survival after CR. After completion of therapy, BM MRD levels of over 500 RUNX1-RUNX1T1 copies per 105 ABL copies were also highly predictive of relapse (relapse rate, 100% versus 7% for those with persistently lower levels) and inferior OS (5-year survival, 57% vs. 94%). For patients with CBFB-MYH11, detection of >10 copies in the peripheral blood associated with a 97% risk of relapse and 57% 5-year-survival, compared with a 7% relapse risk and 91% survival in those with MRD levels <10 copies. The median time from qPCR positivity to hematologic relapse was about 5 months, leading the authors to recommend MRD monitoring from BM every 3 months during the first 18 months of follow-up (Yin et al. 2012).
The French AML Intergroup reported data on 198 CBF-AML patients aged 18–60 years. A ≥3 log reduction of BM fusion transcripts after the first consolidation course associated with a lower relapse risk (hazard ratio, 0.31), while the risk of death was not significantly lower (hazard ratio, 0.51). Importantly, the prognostic significance of early MRD reduction with regard to relapse outweighed the impact of KIT and FLT3 gene mutations in a multivariate analysis (Jourdan et al. 2013). Among RUNX1-RUNX1T1 rearranged patients in this cohort, persistent MRD positivity or molecular relapse in blood after the end of therapy predicted hematological relapse in 21 of 28 patients, while persistent RUNX1-RUNX1T1 MRD positivity in the BM at 2 years was found in 9% of patients who maintained long-term remissions (Willekens et al. 2016).
The German AMLSG group studied a cohort of 53 CBFB-MYH11 rearranged patients and identified criteria for risk stratification. Patients who achieved qPCR negativity in at least one BM sample during consolidation therapy had favorable DFS, while qPCR negativity in at least two BM or PB samples during consolidation therapy and early follow-up predicted for superior DFS and OS. Conversion from PCR negativity to PCR positivity after consolidation therapy occurred in 10 patients, and 6 of them relapsed (Corbacioglu et al. 2010). In summary, these studies establish that MRD measurements by qPCR, and particularly early response kinetics during therapy, are strong prognostic markers in CBF AML. However, it remains unclear whether treatment modification in response to unfavorable MRD results is beneficial.
A Chinese study addressed this question and studied the role of MRD-directed treatment in 116 RUNX1-RUNX1T1-rearranged AML patients . Patients who did not sustain a 3-log reduction of RUNX1-RUNX1T1 transcript levels after 2 cycles of intermediate-dose cytarabine-based consolidation chemotherapy were considered high risk and were recommended to undergo alloSCT, while those with better responses were scheduled for 6 cycles of consolidation chemotherapy. The trial was not randomized, and about 40 % of patients crossed over between the two arms for various reasons. In this cohort, alloSCT improved DFS and OS of high-risk, but not of low-risk patients, but this result requires confirmation from controlled trials (Zhu et al. 2013). A follow-up study from the same group investigated the prognostic relevance of MRD detection in the posttransplantation setting. Patients who achieved a >3 log reduction of BM RUNX1-RUNX1T1 transcript levels during the first 3 months after alloSCT had significantly lower relapse rates and longer DFS, compared to those with higher transcript levels. A multivariate analysis suggested that MRD levels outweigh KIT mutation status as a stronger predictor of post-transplant relapse risk, although this analysis is limited by the relatively small patient cohort (Wang et al. 2014).
3 Other Balanced Translocations Involving RUNX1 in Myeloid Malignancies
Besides the t(8;21)(q22;q22), several other recurrent chromosomal translocations involving the RUNX1 locus have been described in myeloid neoplasms and are discussed in the following sections.
3.1 AML with t(3;21)(q26;q22); RUNX1-MECOM
The balanced translocation t(3;21)(q26;q22) was initially identified in patients with chronic myeloid leukemia (CML) in blast crisis, and subsequently found in 3.6% of patients with therapy-related AML or myelodysplastic syndromes (t-AML/t-MDS ) (Rubin et al. 1987; Rubin et al. 1990). In a cohort of 6515 adult AML patients, the translocation occurred in only 0.14%. More recently, this translocation was also observed in CML evolving into myeloid blast crisis after TKI treatment (Paquette et al. 2011). According to the 2016 WHO classification of haematopoietic neoplasms, detection of t(3;21)(q26;q22) is sufficient to establish a diagnosis of “AML with myelodysplasia-related changes” in patients with ≥20% blasts.
The t(3;21)(q26;q22) was shown to lead to the formation of RUNX1-EVI1 and RUNX1-MDS1 fusion transcripts (Nucifora et al. 1994; Mitani et al. 1994). The MDS1 and EVI1 genes are located closely to each other in chromosome band 3q26, and splicing of the second exon of MDS1 to the second exon of EVI1 can lead to the formation of a chimeric MDS1/EVI1 transcript. Due to this close relation, MDS1 and EVI1 now are designated the ‘MDS1 and EVI1 complex locus’ (MECOM), and the fusion gene in t(3;21)(q26;q22) has thus been named RUNX1-MECOM. High EVI1 expression is found in most patients with t(3;21)(q26;q22). MDS1/EVI1 levels were also high in some patients with t(3;21), but absent in others, indicating that RUNX1-MDS1/EVI1 as well as RUNX1-EVI1 fusions may occur depending on the location of the breakpoint in band 3q26 relative to the MECOM locus (Lugthart et al. 2010). With regard to outcomes, t-AML with t(3;21) associated with shorter OS compared to t-AML with t(8;21) in one series (Slovak et al. 2002).
3.2 AML with t(16;21)(q24;q22); RUNX1-CBFA2T3
The t(16;21)(q24;q22) is a rare, but recurrent chromosomal alteration found in therapy-related myeloid neoplasms. Gamou and colleagues reported that in this translocation, RUNX1 is fused to CBFA2T3 (previously called MTG16), a member of the conserved ETO family of transcriptional corepressors that shares a high degree of homology with RUNX1T1, the RUNX1 translocation partner in t(8;21) (Gamou et al. 1998; Davis et al. 2003). Only 24 patients with t(16;21)(q24;q22) are currently reported in the Mitelman Database of Chromosome Aberrations and Gene Fusions in Cancer, including 12 who also had trisomy 8, suggesting a possible association between the two alterations (Mitelman et al. 2016). The clinical significance of this translocation in AML is unknown.
3.3 Rare Recurrent Translocations in AML Involving RUNX1
A number of additional, very rare but recurrent translocations involving RUNX1 have been described in AML. In t(1;21)(p36;q22), RUNX1 is fused to the PRDM16 gene, a member of the positive regulatory (PR) domain gene family with similarity to MECOM (Sakai et al. 2005). In t(1;21)(p22;q22), RUNX1 is fused to the CLCA2 calcium channel gene (Giguère and Hébert 2010). In the t(11;21)(p14;q22), the fusion partner is KIAA1549L, a poorly characterized gene with unknown function (Abe et al. 2012). Finally, the t(20;21)(q13.2;q22.12) results in a ZFP64-RUNX1 fusion involving the zinc finger protein ZFP6 (Richkind et al. 2000). The clinical significance of these alterations is unknown due to their rarity.
4 Association of RUNX1 Translocations with Therapy-Related Neoplasia
Petersen -Biergard and colleagues first reported an association between chromosomal rearrangements involving chromosome band 21q22 and t-MDS or t-AML (Pedersen-Bjergaard and Philip 1991). In 2002, an international workshop identified balanced 21q22 translocations in 15.5% of patients with t-MDS or therapy-related acute leukemias (Slovak et al. 2002). The most common primary diseases were breast cancer, Hodgkin disease and non-Hodgkin lymphoma , and most patients had received topoisomerase II inhibitors and alkylating agents with or without radiotherapy. The median latency of the secondary hematologic disorder was 39 months, significantly longer than for therapy-induced neoplasms with rearrangements involving KMT2A (chromosome band 11q23) or CBFB (16q22). A t(8;21) was present in 56% of these patients, and 22 additional translocations with documented involvement of the RUNX1 locus were found, including t(3;21) in 20% and t(16;21) in 5% of patients. In a small series of 13 patients with t-AML and t(8;21), a CR rate of >90% was observed; however 10 of the 13 patients died after a median of 19 months (Gustafson et al. 2009). Likewise, Krauth and colleagues reported that among patients with t(8;21), those with t-AML had shorter OS compared to de novo patients (Krauth et al. 2014). The limited data available from retrospective case series suggests that the prognosis of t-AML patients with RUNX1 rearrangements other than t(8;21) is relatively poor, with a median survival of less than 1 year (Slovak et al. 2002).
5 RUNX1 Point Mutations in Myeloid Malignancies
5.1 RUNX1 Mutations in AML
When the RUNX1 gene was initially identified in 1991, Miyoshi et al. described a transcript encoding a 250-amino acid (AA) protein that was later named isoform AML1a, and today is known as transcript variant 3 (Miyoshi et al. 1991). Subsequently, the same group identified two additional transcript variants encoding proteins of 453 and 480 AA, which were designated AML1b (transcript variant 2) and AML1c (transcript variant 1), respectively (Miyoshi et al. 1995). The N-terminus of AML1c differs from that of AML1a and AML1b due to the use of an alternative promoter. All 3 proteins share a highly conserved, 128-AA Runt domain, a protein motif responsible for both DNA binding and heterodimerization. AML1b and AML1c contain a large C-terminal transactivation domain. Currently, the NCBI Gene database lists 13 exons, and 10 alternatively spliced RefSeq transcript isoforms, while the Ensembl database lists 9 protein-coding isoforms.
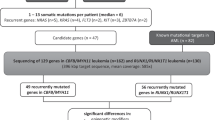
In 1999, Osato and colleagues were the first to identify somatically acquired RUNX1 point mutations in 8 of 160 patients with myeloid leukemia (7 AML and 1 CML in blast crisis) (Osato et al. 1999). These mutations, located in the Runt domain, either disturb DNA binding and/or lead to weakened nuclear expression of RUNX1. The Runt domain is located in exons 3–5 and ranges from position 50–178 in the 453 AA transcript (position 77–205 in the 480 AA transcript). Early RUNX1 mutation screening studies therefore often focused on exons 3–5, and did not include exons 1 and 2 or the C-terminal exons encoding the transactivation domain. Aggregate data from multiple cohorts available through the Catalogue of Somatic Mutations in Cancer (Forbes et al. 2015; Schnittger et al. 2011; Tang et al. 2009), and data from our own patients (Metzeler et al. 2016) indicate that RUNX1 missense mutations cluster in the Runt homology domain (spanning exons 3–5) and are predicted to interfere with DNA binding, while truncating (nonsense and frame shift) mutations are distributed along the entire coding sequence (Fig. 12.2).
Spectrum of somatic RUNX1 point mutations in AML patients. Distribution of somatic RUNX1 point mutations along the coding sequence of transcript variant 2 (NCBI accession number, NM_001001890.2). Truncating mutations (i.e., nonsense and frame shift changes) are shown in red, and missense variants are shown in green (Data are from the Catalogue of Somatic Mutations in Cancer (COSMIC) (Forbes et al. 2015) and from Metzeler et al. (2016))
The reported incidence of RUNX1 mutations in AML varies widely between studies (Tang et al. 2009), ranging from 3% in a series of pediatric AML patients (Taketani et al. 2003) to 33% in a cohort of adults with non-complex karyotypes (Schnittger et al. 2011). This large variability may be due to different baseline characteristics of the patient populations under study (e.g., age range, ethnicity, selection of cytogenetic subgroups, and de novo vs. secondary AML), and differences in the methods and target regions for mutation analyses. In recent, relatively large adult AML cohorts, the incidence of RUNX1 mutations generally was in the range of 5–15% (Osato et al. 2001; Tang et al. 2009; Gaidzik et al. 2011; Patel et al. 2012; The Cancer Genome Atlas Research Network 2013; Kihara et al. 2014). The Cancer Genome Atlas Research Network (TCGA) consortium identified RUNX1 mutations in 10% of 200 AML adult patients studied by whole-genome or whole-exome sequencing (The Cancer Genome Atlas Research Network 2013). Notably, analyses of clonal hierarchies in this cohort suggested that RUNX1 mutations always were part of the “founding clone” that initiated the disease (Miller et al. 2013).
5.2 Clinical Characteristics of AML Patients with Mutated RUNX1
Early studies indicated an association of somatic RUNX1 mutations with FAB M0 morphology, and with secondary or treatment-related myeloid neoplasia (Asou 2003; Osato 2004). For example, Preudhomme and co-workers identified RUNX1 mutations in ~10% of AML patients, and in 22% of patients with minimally differentiated (i.e., M0) AML. Twenty-one of 34 AML M0 patients in this series had biallelic RUNX1 mutations, where a point mutation on one allele was accompanied by another point mutation or deletion of the second allele, while patients with non-M0 AML had monoallelic mutations (Preudhomme et al. 2000; Roumier et al. 2003). The association of RUNX1 mutations with minimally differentiated AML was confirmed in larger series showing that 24 –65% of patients with AML M0 carry RUNX1 mutations (Dicker et al. 2007; Tang et al. 2009; Schnittger et al. 2011; Kao et al. 2014). Of note, in one large cohort that only included patients younger than 60 years, only 15% of M0 patients had mutated RUNX1, but the mutation was still enriched in this subgroup (Gaidzik et al. 2011). Tang and co-workers initially reported an association of RUNX1 mutation with older age, an association that has been confirmed by multiple subsequent studies (Tang et al. 2009; Schnittger et al. 2011; Mendler et al. 2012; Greif et al. 2012). An association with male sex was also noted in some, but not all of these studies.
5.3 Cooperating Genetic Lesions in RUNX1-Mutated AML
RUNX1 mutations are found in patients with intermediate-risk (including cytogenetically normal AML) or unfavorable karyotypes, but are absent in those with favorable karyotypes (i.e., CBF leukemias including RUNX1-RUNX1T1 rearranged AML, and APL) and in patients with balanced translocations involving 11q23 ( KMT2A; MLL ) (Tang et al. 2009; Gaidzik et al. 2011; The Cancer Genome Atlas Research Network 2013). RUNX1 mutations are particularly common in patients with isolated trisomy 13, a rare cytogenetic subgroup with a RUNX1 mutation frequency of 75–90% (Dicker et al. 2007; Schnittger et al. 2011; Herold et al. 2014). In several series, an association of RUNX1 mutations with trisomy 8 was noted (Tang et al. 2009; Gaidzik et al. 2011; Alpermann et al. 2015). Accordingly, in two studies of adult AML patients with sole trisomy 8, RUNX1 mutations were the most or second most common molecular alterations, occurring in 28% and 32% of patients, respectively (Becker et al. 2014; Alpermann et al. 2015). Finally, two studies reported an association between somatically acquired trisomy 21 and RUNX1 mutations in AML (Preudhomme et al. 2000; Taketani et al. 2003). In one of these studies, the mutated RUNX1 allele was present on two of the three copies of chromosome 21 in all 4 patients analyzed (Preudhomme et al. 2000). This indicates that trisomy 21 occurred as a secondary change after the RUNX1 mutation, possibly acting by increasing the mutant-to-wild type allelic ratio.
With regard to coexisting molecular genetic alterations, RUNX1 mutations were shown to be almost mutually exclusive with NPM1 and CEBPA mutations in multiple AML cohorts (Tang et al. 2009; Schnittger et al. 2011; Gaidzik et al. 2011; Mendler et al. 2012; Greif et al. 2012; The Cancer Genome Atlas Research Network 2013). On the other hand, a positive association was observed between mutated RUNX1 and presence of KMT2A ( MLL ) partial tandem duplications (KMT2A-PTD) (Tang et al. 2009; Schnittger et al. 2011; Gaidzik et al. 2011; Greif et al. 2012). RUNX1 has subsequently been shown to interact directly with KMT2A. This interaction mediates histone H3K4 tri-methylation in the promoter region of the SPI1 (PU.1) transcription factor that is involved in hematopoietic stem cell maintenance (Koh et al. 2013). Several groups also found a close association of mutations in ASXL1 and RUNX1, with 22–44% of RUNX1-mutated patients carrying ASXL1 mutations (Mendler et al. 2012; Schnittger et al. 2013; Paschka et al. 2015). Moreover, an association of RUNX1 mutations with mutated IDH2 was identified in two large studies (Gaidzik et al. 2011; The Cancer Genome Atlas Research Network 2013). While these associations suggest functional synergism between the RUNX1 and frequently co-mutated genes, this has not yet been proven experimentally.
5.4 RUNX1 Mutations and Prognosis in AML
Several relatively large patient cohorts provide information on the prognostic relevance of RUNX1 gene mutations. Tang and colleagues identified RUNX1 mutations in 13% of 470 patients with non-M3 AML (Tang et al. 2009). In the 330 patients who received standard induction and consolidation chemotherapy, multivariate analyses showed that RUNX1 mutations associated with lower CR rates and shorter OS, but not with differences in DFS. In another cohort of 449 patients with normal or non-complex abnormal karyotypes who received non-uniform treatment, mutated RUNX1 associated with inferior EFS and OS (Schnittger et al. 2011).
These two reports both showed an unfavorable impact of mutated RUNX1 in subgroup analyses of patients with cytogenetically normal AML (CN-AML), and several studies focused on this cytogenetic subset. Mendler and colleagues identified RUNX1 mutations in 12.5% of de novo CN-AML patients, and found an association with lower CR rates and inferior RFS, EFS and OS (Mendler et al. 2012). Similar results were obtained in multivariate analyses, and in subgroup analyses of younger (<60 years) and older (≥60 years) patients. Updated survival data are shown in Fig. 12.3. Of note, patients did not undergo alloSCT in first CR in this series. In another, smaller study focusing on CN-AML, an association between mutated RUNX1 and inferior OS was observed in the entire cohort and in the subgroups of patients aged ≥60 years, and those within the European LeukemiaNet (ELN) Intermediate-I genetic group (Greif et al. 2012).
RUNX1 mutations and prognosis of patients with de novo cytogenetically normal AML. Top: Disease-free survival of patients with de novo cytogenetically normal AML (a) aged <60 years and (b) aged ≥60 years, according to RUNX1 mutation status. Bottom: Overall survival of patients with de novo cytogenetically normal AML (c) aged <60 years and (d) aged ≥60 years, according to RUNX1 mutation status (Bloomfield et al. unpublished data)
In the largest cohort published so far, Gaidzik and colleagues studied 945 patients aged 18–60 years treated on trials of the AMLSG. Only 5.6% of the patients carried RUNX1 mutations, potentially due to the exclusion of older patients. RUNX1 mutations associated with lower CR rate, and shorter RFS and OS. In multivariate analyses, RUNX1 mutations were a significant predictor of shorter EFS and shorter RFS censored at the time of alloSCT, but not for CR rate, RFS without censoring, or OS (Gaidzik et al. 2011). In another relatively large cohort of 664 patients aged 18–86 years, RUNX1 mutations associated with unfavorable OS only in patients younger than 60 years, and particularly in those with intermediate-risk cytogenetics (Metzeler et al. 2016).
At least two groups have addressed the impact of postremission therapy on outcomes of RUNX1-mutated patients. In the study by Tang and colleagues, RUNX1 mutations were not associated with OS in the subset of patients who underwent alloSCT, suggesting that allografting might ameliorate the unfavorable prognostic impact of the mutation (Tang et al. 2009). In agreement with these results, Gaidzik et al. found that the RFS of RUNX1 mutated patients who underwent alloSCT was comparable to RUNX1-wild type patients, while all patients who did not receive a transplant uniformly relapsed, most within 1 year (Gaidzik et al. 2011).
In summary, while univariate analyses consistently showed an unfavorable prognosis of RUNX1-mutated adult AML patients, the results of multivariate analyses adjusting for potential confounders are less clear. These discrepancies may be due to different baseline characteristics, for example regarding the age range of included patients, differences in treatment regimens including the use of alloSCT, and the effects of other genetic alterations that are considered in the multivariate models. With regard to the last point, several groups have recently tried to combine the prognostic information conveyed by various genetic alterations into integrative risk stratification algorithms. In two of these models, RUNX1 mutations emerged as a factor associated with relatively unfavorable OS (Kihara et al. 2014; Grossmann et al. 2012), while in a third study, RUNX1 mutations were found in only 5% of patients and were not included in the proposed risk stratification system (Patel et al. 2012).
Besides their prognostic relevance at baseline, RUNX1 mutations could also serve as novel markers for MRD detection, yet the heterogeneity of the mutations make monitoring via conventional PCR assays difficult. This issue may be solved through the use of next-generation sequencing (NGS) techniques, as demonstrated in a cohort of 103 intensively treated, RUNX1-mutated patients with available follow-up samples (Kohlmann et al. 2014). Although the sensitivity of the NGS assay was relatively limited, residual disease was detected in 46 of the 103 patients at time points ranging from 60 to 198 days after initial diagnosis. Detectable RUNX1 mutation associated with shorter EFS and OS. Notably, RUNX1 mutations detected at the time of initial diagnosis were stable in relapsed disease in 51 of 57 evaluable patients (89%), while in 6 patients (11%), mutations were lost.
5.5 Reasons for the Different Outcomes of AML with Mutations and Balanced Translocations Involving RUNX1
Two major modes of RUNX1 gene alteration, point mutations and balanced translocations leading to chimeric fusion genes, are found in AML. As outlined above, the clinical consequences of these two types of alterations are remarkably different. RUNX1 point mutations generally associate with inferior outcomes and FAB M0 morphology, while the RUNX1-RUNX1T1 gene fusion associates with favorable outcomes and a more differentiated (FAB M2) phenotype. The causes for these discrepant effects are not well understood. Among the potential factors that have been implicated are differences in the spectrum of co-mutated partner genes, differences in the residual RUNX1 activity of the mutant allele, variable dominant-negative effects on the intact second allele, and effects of the translocation fusion partner in the case of balanced translocations (Osato et al. 2001).
5.6 RUNX1 Point Mutations in Myelodysplastic Syndromes and Other Myeloid Malignancies
RUNX1 mutations in patients with MDS were first described in 2000 (Imai et al. 2000). Harada and colleagues subsequently found RUNX1 mutations in 24% of MDS patients with elevated BM blasts (refractory anemia with excess blasts, RAEB) or post-MDS AML, while mutations were rarely observed in low-risk MDS without increased blast count (Harada et al. 2004). Of note, the frequency of RUNX1 mutations was particularly high (50%) in a cohort of patients who developed MDS or AML after chemotherapy, radiotherapy or radiation exposure due to the atomic bombs used against Japan (Harada et al. 2003; Harada et al. 2004). A link between exposure to ionizing radiation and RUNX1-mutated myelodysplasia was confirmed by a study of radiation-exposed residents near a former Soviet nuclear test site (Zharlyganova et al. 2008). In three more recently published, larger series of MDS patients, RUNX1 mutations were found in 8–11% of individuals (Bejar et al. 2011; Papaemmanuil et al. 2013; Haferlach et al. 2014). In two of these studies, analyses of recurrently mutated genes by targeted NGS revealed that mutated RUNX1 frequently co-occur with mutations in SRSF2, ASXL1, EZH2, and STAG2 (Papaemmanuil et al. 2013; Haferlach et al. 2014).
In MDS, RUNX1 mutations are relatively rare in patients with low-risk disease and are found more frequently in patients with increased BM blasts (RAEB) and those transforming to post-MDS secondary AML (s-AML) (Papaemmanuil et al. 2013; Haferlach et al. 2014). In the light of this association, it is not surprising that mutated RUNX1 associated with inferior leukemia-free survival in one cohort (Dicker et al. 2010). Moreover, RUNX1 mutations associated with shorter OS even after adjustment for the International Prognostic Scoring System (IPSS) risk group and age in another series (Bejar et al. 2011). Finally, RUNX1 mutations were included in a recently proposed 14-gene score that identifies MDS patients with shorter OS (Haferlach et al. 2014). In a study of 38 paired samples from MDS patients who later progressed to s-AML, 9 (24%) had RUNX1 mutations already at the MDS stage, and only one RUNX1-wild type patient gained a mutation at the time of progression. Although the median time between MDS diagnosis and progression to s-AML was only 9 months, these data suggest that RUNX1 mutations are a predisposing factor for s-AML transformation that is already present during the MDS phase, and not a marker that is acquired at the time of progression (Flach et al. 2011).
Mutations in RUNX1 were also detected in 9–15% of chronic myelomonocytic leukemia (CMML), but do not seem to be prognostically relevant in this entity (Itzykson et al. 2013; Kohlmann et al. 2010). Finally, in a study of 70 patients with advanced, KIT-mutated systemic mastocytosis, RUNX1 mutations were found in 23 % and associated with shorter OS (Jawhar et al. 2016).
6 Familial Platelet Disorder with Associated Myeloid Malignancy
Familial platelet disorder with associated myeloid malignancy (FPDMM; also known as familial platelet disorder with propensity to acute myelogenous leukemia, FPD/AML ; Online Mendelian Inheritance in Man [OMIM] identifier, #601399) is an extremely rare, heritable condition caused by heterozygous germline RUNX1 mutations. This syndrome was initially described in 1985 by Dowton and colleagues as an autosomal dominant disorder of platelet production and function in a large family with bleeding diathesis , and 6 members of the same family developed hematologic neoplasms (Dowton et al. 1985). Through linkage analysis, a critical region on chromosome 21 was identified in several affected families, and mutation analysis of regional candidate genes revealed mutations in RUNX1 in six of the seven families (Ho et al. 1996; Song et al. 1999).
In the meantime, at least 20 affected kindreds have been described in the literature, and 19 of them were found to carry diverse types of RUNX1 mutations including missense, frameshift and nonsense mutations as well as large deletions affecting the RUNX1 locus (Preudhomme et al. 2009). Truncating changes lead to loss of the C-terminal transactivation domain resulting in haploinsufficiency of RUNX1. Missense mutations frequently affect conserved residues in the Runt domain that are involved in DNA binding, and may exert a dominant-negative effect on the remaining, intact allele through heterodimerization (Michaud et al. 2002). Patients with FPDMM typically present with mild thrombocytopenia, an “aspirin-like” platelet aggregation defect with abnormal response to epinephrine and arachidonic acid, a dense granule storage pool deficiency, and prolonged bleeding time. The lifetime incidence of leukemia among affected individuals is reported to be 20–50% (Osato 2004). In a series of asymptomatic individuals with germline RUNX1 mutations aged <50 years, clonal hematopoiesis was detected in 67%, a proportion that is much higher than expected during normal aging (Churpek et al. 2015). Progression to AML is often accompanied by somatically acquired “second hits” (mutations or deletions) involving the second RUNX1 allele, as well as gains of additional mutations in genes recurrently mutated in sporadic AML (Antony-Debré et al. 2016). Recently, somatic mutations in the CDC25C gene, which is not known to be mutated in sporadic AML, were reported in 7 of 13 FPDMM patients from Japan, including 4 of 7 patients who had developed AML. This finding was not reproduced in a European cohort (Yoshimi et al. 2014; Antony-Debré et al. 2016).
7 RUNX1 Gene Alterations in Acute Lymphoblastic Leukemia
Although RUNX1 translocations were first detected in AML, they are also found in acute leukemias of lymphoid lineage, particularly in childhood B-cell precursor acute lymphoblastic leukemia (BCP-ALL). The t(12;21)(p13;q22), leads to rearrangement of RUNX1 with the ETV6 gene. The resulting ETV6-RUNX1 fusion transcript (previously designated TEL-AML1 ) is controlled by the ETV6 promoter and contains the N-terminal “helix-loop-helix” (HLH) domains of ETV6 fused to a large C-terminal part of the RUNX1 coding sequence, including the Runt and transactivation domains. This is in contrast to RUNX1 fusion genes found in AML, which are under the control of the RUNX1 promoter and lack the RUNX1 C-terminus including the transactivation domain (Golub et al. 1995; Romana et al. 1995a).
The t(12;21)(p13;q22) is commonly cryptic and missed by metaphase cytogenetics, and thus was initially considered to be a rare event. However, using fluorescence-in situ hybridization, the ETV6-RUNX1 rearrangement can be detected in approximately 15–35% of pediatric BCP-ALL, particularly in patients aged 1–9 years, while it is rare (<3%) in adult BCP-ALL (Romana et al. 1995b; Fears et al. 1996; Zelent et al. 2004). Thus, t(12;21)(p13;q22) is the most common structural chromosomal alteration in pediatric cancer. The translocation is accompanied by a deletion of the second ETV6 allele on the other chromosome in >50% of patients, suggesting that loss of ETV6 function plays a role in this disease (Raynaud et al. 1996; Schwab et al. 2013). Overall, ETV6-RUNX1-rearranged childhood BCP-ALL patients seem to harbor a relatively high number of copy number alterations including deletions of CDKN2A/B, PAX5 and BTG1, each occurring in 15–20% of patients (Kim et al. 1996; Mullighan et al. 2007; Schwab et al. 2013). Furthermore, mutations in the histone H3K36 methyltransferase NSD2 are found in 20% of ETV6-RUNX1 rearranged childhood ALL (Jaffe et al. 2013). Several studies conclusively demonstrated that children with the ETV6-RUNX1 rearrangement have excellent treatment outcomes (Shurtleff et al. 1995; Borkhardt et al. 1997; Moorman et al. 2010; Bhojwani et al. 2012), although in some series a high frequency of late relapses (≥5 years after diagnosis) was noted (Forestier et al. 2008). In one large study of 1725 children and adolescents with BCP-ALL, those with ETV6-RUNX1 had ~50% reduced risk of relapse or death compared to other genetic subsets, with no late relapses. These associations persisted in multivariate analyses adjusting for other known risk factors (Moorman et al. 2010).
Studies of monozygotic twins and neonatal blood spots (Guthrie cards) revealed that the RUNX1-ETV6 rearrangement is frequently acquired before birth, and BCP-ALL can develop in affected children with a reported latency of up to 14 years (Ford et al. 1998; Wiemels et al. 1999a, b). Notably, using highly sensitive assays, RUNX1-ETV6 fusion transcripts can be found in up to 1% of cord blood samples from healthy newborns (Mori et al. 2002). In these children, the rearrangement is present in 1 of 103–104 mononuclear cells, indicating that the offspring of the single cell that initially acquired the translocation gained a proliferative advantage and underwent clonal expansion. On the other hand, the proportion of newborns with detectable RUNX1-ETV6 transcripts in cord blood samples exceeds the incidence of RUNX1-ETV6-positive childhood BCP-ALL by a factor of 100, indicating that affected newborns have a low absolute risk of developing ALL, and that the acquisition of secondary genetic lesions is necessary for the development of overt leukemia. Although more rare, RUNX1-RUNX1T1 fusion transcripts have also been detected in healthy newborns (Mori et al. 2002). Quantitative PCR assays have been developed for the detection of MRD in children with t(12;21) (Pallisgaard et al. 1999; Seeger et al. 2001; Drunat et al. 2001).
Besides the t(12;21), RUNX1 point mutations have been found in sporadic childhood ALL (Song et al. 1999) and affect about 15% of children with early T-cell precursor (ETP)-ALL (Zhang et al. 2012). RUNX1 mutations also occur in T-ALL developing in patients with FPDMM (Owen et al. 2008; Preudhomme et al. 2009; Prébet et al. 2013).
References
Abe, A., Katsumi, A., Kobayashi, M., et al. (2012). A novel RUNX1-C11orf41 fusion gene in a case of acute myeloid leukemia with a t(11;21)(p14;q22). Cancer Genetics, 205(11), 608–611.
Allen, C., Hills, R. K., Lamb, K., et al. (2013). The importance of relative mutant level for evaluating impact on outcome of KIT, FLT3 and CBL mutations in core-binding factor acute myeloid leukemia. Leukemia, 27(9), 1891–1901.
Alpermann, T., Haferlach, C., Eder, C., et al. (2015). AML with gain of chromosome 8 as the sole chromosomal abnormality (+8sole) is associated with a specific molecular mutation pattern including ASXL1 mutations in 46.8 % of the patients. Leukemia Research, 39(3), 265–272.
Antony-Debré, I., Duployez, N., Bucci, M., et al. (2016). Somatic mutations associated with leukemic progression of familial platelet disorder with predisposition to acute myeloid leukemia. Leukemia, 30(4), 999–1002.
Appelbaum, F. R., Kopecky, K. J., Tallman, M. S., et al. (2006). The clinical spectrum of adult acute myeloid leukaemia associated with core binding factor translocations. British Journal of Haematology, 135(2), 165–173.
Asou, N. (2003). The role of a runt domain transcription factor AML1/RUNX1 in leukemogenesis and its clinical implications. Critical Reviews in Oncology/Hematology, 45(2), 129–150.
Becker, H., Maharry, K., Mrózek, K., et al. (2014). Prognostic gene mutations and distinct gene- and microRNA-expression signatures in acute myeloid leukemia with a sole trisomy 8. Leukemia, 28(8), 1754–1758.
Beghini, A., Larizza, L., Cairoli, R., & Morra, E. (1998). c-kit activating mutations and mast cell proliferation in human leukemia. Blood, 92(2), 701–702.
Beghini, A., Peterlongo, P., Ripamonti, C. B., et al. (2000). C-kit mutations in core binding factor leukemias. Blood, 95(2), 726–728.
Beghini, A., Ripamonti, C. B., Cairoli, R., et al. (2004). KIT activating mutations: Incidence in adult and pediatric acute myeloid leukemia, and identification of an internal tandem duplication. Haematologica, 89(8), 920–925.
Bejar, R., Stevenson, K., Abdel-Wahab, O., et al. (2011). Clinical effect of point mutations in myelodysplastic syndromes. The New England Journal of Medicine, 364(26), 2496–2506.
Bhojwani, D., Pei, D., Sandlund, J. T., et al. (2012). ETV6-RUNX1-positive childhood acute lymphoblastic leukemia: Improved outcome with contemporary therapy. Leukemia, 26(2), 265–270.
Bloomfield, C. D., Goldman, A., Hassfeld, D., & de la Chapelle, A. (1984). Fourth international workshop on chromosomes in leukemia 1982: Clinical significance of chromosomal abnormalities in acute nonlymphoblastic leukemia. Cancer Genetics and Cytogenetics, 11(3), 332–350.
Bloomfield, C. D., Lawrence, D., Byrd, J. C., et al. (1998). Frequency of prolonged remission duration after high-dose cytarabine intensification in acute myeloid leukemia varies by cytogenetic subtype. Cancer Research, 58(18), 4173–4179.
Boissel, N., Leroy, H., Brethon, B., et al. (2006). Incidence and prognostic impact of c-Kit, FLT3, and Ras gene mutations in core binding factor acute myeloid leukemia (CBF-AML). Leukemia, 20(6), 965–970.
Boissel, N., Renneville, A., Leguay, T., et al. (2015). Dasatinib in high-risk core binding factor acute myeloid leukemia in first complete remission: A French acute myeloid leukemia intergroup trial. Haematologica, 100(6), 780–785.
Borkhardt, A., Cazzaniga, G., Viehmann, S., et al. (1997). Incidence and clinical relevance of TEL/AML1 fusion genes in children with acute lymphoblastic leukemia enrolled in the German and Italian multicenter therapy trials. Associazione Italiana Ematologia Oncologia Pediatrica and the Berlin-Frankfurt-Münster Study Group. Blood, 90(2), 571–577.
Bullinger, L., Döhner, K., Bair, E., et al. (2004). Use of gene-expression profiling to identify prognostic subclasses in adult acute myeloid leukemia. The New England Journal of Medicine, 350(16), 1605–1616.
Buonamici, S., Ottaviani, E., Testoni, N., et al. (2002). Real-time quantitation of minimal residual disease in inv(16)-positive acute myeloid leukemia may indicate risk for clinical relapse and may identify patients in a curable state. Blood, 99(2), 443–449.
Burnett, A. K., Hills, R. K., Milligan, D., et al. (2011). Identification of patients with acute myeloblastic leukemia who benefit from the addition of gemtuzumab ozogamicin: Results of the MRC AML15 trial. Journal of Clinical Oncology, 29(4), 369–377.
Burnett, A. K., Goldstone, A., Hills, R. K., et al. (2013). Curability of patients with acute myeloid leukemia who did not undergo transplantation in first remission. Journal of Clinical Oncology, 31(10), 1293–1301.
Burnett, A. K., Russell, N. H., Hills, R. K., et al. (2015). A randomized comparison of daunorubicin 90 mg/m2 vs 60 mg/m2 in AML induction: Results from the UK NCRI AML17 trial in 1206 patients. Blood, 125(25), 3878–3885.
Byrd, J. C., Mrózek, K., Dodge, R. K., et al. (2002). Pretreatment cytogenetic abnormalities are predictive of induction success, cumulative incidence of relapse, and overall survival in adult patients with de novo acute myeloid leukemia: Results from Cancer and Leukemia Group B (CALGB 8461). Blood, 100(13), 4325–4336.
Byrd, J. C., Ruppert, A. S., Mrózek, K., Carroll, A. J., et al. (2004). Repetitive cycles of high-dose cytarabine benefit patients with acute myeloid leukemia and inv(16)(p13q22) or t(16;16)(p13;q22): Results from CALGB 8461. Journal of Clinical Oncology, 22(6), 1087–1094.
Cairoli, R., Beghini, A., Grillo, G., et al. (2006). Prognostic impact of c-KIT mutations in core binding factor leukemias: An Italian retrospective study. Blood, 107(9), 3463–3468.
Cammenga, J., Horn, S., Bergholz, U., et al. (2005). Extracellular KIT receptor mutants, commonly found in core binding factor AML, are constitutively active and respond to imatinib mesylate. Blood, 106(12), 3958–3961.
Cancer Genome Atlas Research Network. (2013). Genomic and epigenomic landscapes of adult de novo acute myeloid leukemia. The New England Journal of Medicine, 368(22), 2059–2074.
Care, R. S., Valk, P. J., Goodeve, A. C., et al. (2003). Incidence and prognosis of c-KIT and FLT3 mutations in core binding factor (CBF) acute myeloid leukaemias. British Journal of Haematology, 121(5), 775–777.
Chevalier, N., Solari, M. L., Becker, H., et al. (2010). Robust in vivo differentiation of t(8;21)-positive acute myeloid leukemia blasts to neutrophilic granulocytes induced by treatment with dasatinib. Leukemia, 24(10), 1779–1781.
Churpek, J. E., Pyrtel, K., Kanchi, K. L., et al. (2015). Genomic analysis of germ line and somatic variants in familial myelodysplasia/acute myeloid leukemia. Blood, 126(22), 2484–2490.
Corbacioglu, A., Scholl, C., Schlenk, R. F., et al. (2010). Prognostic impact of minimal residual disease in CBFB-MYH11-positive acute myeloid leukemia. Journal of Clinical Oncology, 28(23), 3724–3729.
Cornelissen, J. J., van Putten, W. L., Verdonck, L. F., et al. (2007). Results of a HOVON/SAKK donor versus no-donor analysis of myeloablative HLA-identical sibling stem cell transplantation in first remission acute myeloid leukemia in young and middle-aged adults: Benefits for whom? Blood, 109(9), 3658–3666.
Creutzig, U., van den Heuvel-Eibrink, M. M., Gibson, B., et al. (2012). Diagnosis and management of acute myeloid leukemia in children and adolescents: Recommendations from an international expert panel. Blood, 120(16), 3187–3205.
Davis, J. N., McGhee, L., & Meyers, S. (2003). The ETO (MTG8) gene family. Gene, 303, 1–10.
Dicker, F., Haferlach, C., Kern, W., et al. (2007). Trisomy 13 is strongly associated with AML1/RUNX1 mutations and increased FLT3 expression in acute myeloid leukemia. Blood, 110(4), 1308–1316.
Dicker, F., Haferlach, C., Sundermann, J., et al. (2010). Mutation analysis for RUNX1, MLL-PTD, FLT3-ITD, NPM1 and NRAS in 269 patients with MDS or secondary AML. Leukemia, 24(8), 1528–1532.
Döhner, H., Estey, E. H., Amadori, S., et al. (2010). Diagnosis and management of acute myeloid leukemia in adults: Recommendations from an international expert panel, on behalf of the European LeukemiaNet. Blood, 115(3), 453–474.
Dowton, S. B., Beardsley, D., Jamison, D., et al. (1985). Studies of a familial platelet disorder. Blood, 65(3), 557–563.
Drunat, S., Olivi, M., Brunie, G., et al. (2001). Quantification of TEL-AML1 transcript for minimal residual disease assessment in childhood acute lymphoblastic leukaemia. British Journal of Haematology, 114(2), 281–289.
Duployez, N., Nibourel, O., Marceau-Renaut, A., et al. (2014). Minimal residual disease monitoring in t(8;21) acute myeloid leukemia based on RUNX1-RUNX1T1 fusion quantification on genomic DNA. American Journal of Hematology, 89(6), 610–615.
Duployez, N., Marceau-Renaut, A., Boissel, N., et al. (2016). Comprehensive mutational profiling of core binding factor acute myeloid leukemia. Blood, 127(20), 2451–2459.
Erickson, P., Gao, J., Chang, K. S., et al. (1992). Identification of breakpoints in t(8;21) acute myelogenous leukemia and isolation of a fusion transcript, AML1/ETO, with similarity to Drosophila segmentation gene, runt. Blood, 80(7), 1825–1831.
Fears, S., Vignon, C., Bohlander, S. K., et al. (1996). Correlation between the ETV6/CBFA2 (TEL/AML1) fusion gene and karyotypic abnormalities in children with B-cell precursor acute lymphoblastic leukemia. Genes, Chromosomes and Cancer, 17(2), 127–135.
Fenaux, P., Preudhomme, C., Lai, J.-L., et al. (1989). Cytogenetics and their prognostic value in de novo acute myeloid leukaemia: A report on 283 cases. British Journal of Haematology, 73(1), 61–67.
Flach, J., Dicker, F., Schnittger, S., et al. (2011). An accumulation of cytogenetic and molecular genetic events characterizes the progression from MDS to secondary AML: An analysis of 38 paired samples analyzed by cytogenetics, molecular mutation analysis and SNP microarray profiling. Leukemia, 25(4), 713–718.
Forbes, S. A., Beare, D., Gunasekaran, P., et al. (2015). COSMIC: Exploring the world’s knowledge of somatic mutations in human cancer. Nucleic Acids Research, 43(Database issue), D805–D811.
Ford, A. M., Bennett, C. A., Price, C. M., et al. (1998). Fetal origins of the TEL-AML1 fusion gene in identical twins with leukemia. Proceedings of the National Academy of Sciences USA, 95(8), 4584–4588.
Forestier, E., Heyman, M., Andersen, M. K., et al. (2008). Outcome of ETV6/RUNX1-positive childhood acute lymphoblastic leukaemia in the NOPHO-ALL-1992 protocol: Frequent late relapses but good overall survival. British Journal of Haematology, 140(6), 665–672.
Gabert, J., Beillard, E., van der Velden, V. H. J., et al. (2003). Standardization and quality control studies of “real-time” quantitative reverse transcriptase polymerase chain reaction of fusion gene transcripts for residual disease detection in leukemia – A Europe Against Cancer program. Leukemia, 17(12), 2318–2357.
Gaidzik, V. I., Bullinger, L., Schlenk, R. F., et al. (2011). RUNX1 mutations in acute myeloid leukemia: Results from a comprehensive genetic and clinical analysis from the AML study group. Journal of Clinical Oncology, 29(10), 1364–1372.
Gamou, T., Kitamura, E., Hosoda, F., et al. (1998). The partner gene of AML1 in t(16;21) myeloid malignancies is a novel member of the MTG8(ETO) family. Blood, 91(11), 4028–4037.
Gari, M., Goodeve, A., Wilson, G., et al. (1999). c-kit proto-oncogene exon 8 in-frame deletion plus insertion mutations in acute myeloid leukaemia. British Journal of Haematology, 105(4), 894–900.
Garson, O. M., Hagemeijer, A., Sakurai, M., et al. (1989). Cytogenetic studies of 103 patients with acute myelogenous leukemia in relapse. Cancer Genetics and Cytogenetics, 40(2), 187–202.
Giguère, A., & Hébert, J. (2010). CLCA2, a novel RUNX1 partner gene in a therapy-related leukemia with t(1;21)(p22;q22). Cancer Genetics and Cytogenetics, 202(2), 94–100.
Golub, T. R., Barker, G. F., Bohlander, S. K., et al. (1995). Fusion of the TEL gene on 12p13 to the AML1 gene on 21q22 in acute lymphoblastic leukemia. Proceedings of the National Academy of Sciences USA, 92(11), 4917–4921.
Greif, P. A., Konstandin, N. P., Metzeler, K. H., et al. (2012). RUNX1 mutations in cytogenetically normal acute myeloid leukemia are associated with a poor prognosis and up-regulation of lymphoid genes. Haematologica, 97(12), 1909–1915.
Grimwade, D., Hills, R. K., Moorman, A. V., et al. (2010). Refinement of cytogenetic classification in acute myeloid leukemia: Determination of prognostic significance of rare recurring chromosomal abnormalities among 5876 younger adult patients treated in the United Kingdom Medical Research Council trials. Blood, 116(3), 354–365. doi:10.1182/blood-2009-11-254441.
Grossmann, V., Schnittger, S., Kohlmann, A., et al. (2012). A novel hierarchical prognostic model of AML solely based on molecular mutations. Blood, 120(15), 2963–2972.
Growney, J. D., Clark, J. J., Adelsperger, J., et al. (2005). Activation mutations of human c-KIT resistant to imatinib mesylate are sensitive to the tyrosine kinase inhibitor PKC412. Blood, 106(2), 721–724.
Gustafson, S. A., Lin, P., Chen, S. S., et al. (2009). Therapy-related acute myeloid leukemia with t(8;21) (q22;q22) shares many features with de novo acute myeloid leukemia with t(8;21)(q22;q22) but does not have a favorable outcome. American Journal of Clinical Pathology, 131(5), 647–655.
Haferlach, T., Nagata, Y., Grossmann, V., et al. (2014). Landscape of genetic lesions in 944 patients with myelodysplastic syndromes. Leukemia, 28(2), 241–247.
Harada, H., Harada, Y., Tanaka, H., et al. (2003). Implications of somatic mutations in the AML1 gene in radiation-associated and therapy-related myelodysplastic syndrome/acute myeloid leukemia. Blood, 101(2), 673–680.
Harada, H., Harada, Y., Niimi, H., et al. (2004). High incidence of somatic mutations in the AML1/RUNX1 gene in myelodysplastic syndrome and low blast percentage myeloid leukemia with myelodysplasia. Blood, 103(6), 2316–2324.
Harrison, C. J., Hills, R. K., Moorman, A. V., et al. (2010). Cytogenetics of childhood acute myeloid leukemia: United Kingdom Medical Research Council Treatment trials AML 10 and 12. Journal of Clinical Oncology, 28(16), 2673–2681.
Hartmann, L., Dutta, S., Opatz, S., et al. (2016). ZBTB7A mutations in acute myeloid leukemia with t(8;21) translocation. Nature Communications, 7, 11733.
Herold, T., Metzeler, K. H., Vosberg, S., et al. (2014). Isolated trisomy 13 defines a homogeneous AML subgroup with high frequency of mutations in spliceosome genes and poor prognosis. Blood, 124(8), 1304–1311.
Hills, R. K., Castaigne, S., Appelbaum, F. R., et al. (2014). Addition of gemtuzumab ozogamicin to induction chemotherapy in adult patients with acute myeloid leukaemia: A meta-analysis of individual patient data from randomised controlled trials. Lancet Oncology, 15(9), 986–996.
Ho, C. Y., Otterud, B., Legare, R. D., et al. (1996). Linkage of a familial platelet disorder with a propensity to develop myeloid malignancies to human chromosome 21q22.1-22.2. Blood, 87(12), 5218–5224.
Hospital, M. A., Prebet, T., Bertoli, S., et al. (2014). Core-binding factor acute myeloid leukemia in first relapse: A retrospective study from the French AML intergroup. Blood, 124(8), 1312–1319.
Imai, Y., Kurokawa, M., Izutsu, K., et al. (2000). Mutations of the AML1 gene in myelodysplastic syndrome and their functional implications in leukemogenesis. Blood, 96(9), 3154–3160.
Itzykson, R., Kosmider, O., Renneville, A., et al. (2013). Prognostic score including gene mutations in chronic myelomonocytic leukemia. Journal of Clinical Oncology, 31(19), 2428–2436.
Jaffe, J. D., Wang, Y., Chan, H. M., et al. (2013). Global chromatin profiling reveals NSD2 mutations in pediatric acute lymphoblastic leukemia. Nature Genetics, 45(11), 1386–1391.
Jawhar, M., Schwaab, J., Schnittger, S., et al. (2016). Additional mutations in SRSF2, ASXL1 and/or RUNX1 identify a high-risk group of patients with KIT D816V(+) advanced systemic mastocytosis. Leukemia, 30(1), 136–143.
Jourdan, E., Boissel, N., Chevret, S., et al. (2013). Prospective evaluation of gene mutations and minimal residual disease in patients with core binding factor acute myeloid leukemia. Blood, 121(12), 2213–2223.
Jurlander, J., Caligiuri, M. A., Ruutu, T., et al. (1996). Persistence of the AML1/ETO fusion transcript in patients treated with allogeneic bone marrow transplantation for t(8;21) leukemia. Blood, 88(6), 2183–2191.
Kao, H. W., Liang, D. C., Wu, J. H., et al. (2014). Gene mutation patterns in patients with minimally differentiated acute myeloid leukemia. Neoplasia, 16(6), 481–488.
Keating, M. J., Cork, A., Broach, Y., et al. (1987). Toward a clinically relevant cytogenetic classification of acute myelogenous leukemia. Leukemia Research, 11(2), 119–133.
Kihara, R., Nagata, Y., Kiyoi, H., et al. (2014). Comprehensive analysis of genetic alterations and their prognostic impacts in adult acute myeloid leukemia patients. Leukemia, 28(8), 1586–1595.
Kim, D. H., Moldwin, R. L., Vignon, C., et al. (1996). TEL-AML1 translocations with TEL and CDKN2 inactivation in acute lymphoblastic leukemia cell lines. Blood, 88(3), 785–794.
Koh, C. P., Wang, C. Q., Ng, C. E. L., et al. (2013). RUNX1 meets MLL: Epigenetic regulation of hematopoiesis by two leukemia genes. Leukemia, 27(9), 1793–1802.
Kohlmann, A., Grossmann, V., Klein, H. U., et al. (2010). Next-generation sequencing technology reveals a characteristic pattern of molecular mutations in 72.8 % of chronic myelomonocytic leukemia by detecting frequent alterations in TET2, CBL, RAS, and RUNX1. Journal of Clinical Oncology, 28(24), 3858–3865.
Kohlmann, A., Nadarajah, N., Alpermann, T., et al. (2014). Monitoring of residual disease by next-generation deep-sequencing of RUNX1 mutations can identify acute myeloid leukemia patients with resistant disease. Leukemia, 28(1), 129–137.
Koreth, J., Schlenk, R., Kopecky, K. J., et al. (2009). Allogeneic stem cell transplantation for acute myeloid leukemia in first complete remission: Systematic review and meta-analysis of prospective clinical trials. JAMA, 301(22), 2349–2361.
Krauter, J., Wattjes, M. P., Nagel, S., et al. (1999). Real-time RT-PCR for the detection and quantification of AML1/MTG8 fusion transcripts in t(8;21)-positive AML patients. British Journal of Haematology, 107(1), 80–85.
Krauter, J., Gorlich, K., Ottmann, O., et al. (2003). Prognostic value of minimal residual disease quantification by real-time reverse transcriptase polymerase chain reaction in patients with core binding factor leukemias. Journal of Clinical Oncology, 21(23), 4413–4422.
Krauth, M.-T., Eder, C., Alpermann, T., et al. (2014). High number of additional genetic lesions in acute myeloid leukemia with t(8;21)/RUNX1-RUNX1T1: Frequency and impact on clinical outcome. Leukemia, 28(7), 1449–1458.
Kuchenbauer, F., Schnittger, S., Look, T., et al. (2006). Identification of additional cytogenetic and molecular genetic abnormalities in acute myeloid leukaemia with t(8;21)/AML1-ETO. British Journal of Haematology, 134(6), 616–619.
Kühn, M. W., Radtke, I., Bullinger, L., et al. (2012). High-resolution genomic profiling of adult and pediatric core-binding factor acute myeloid leukemia reveals new recurrent genomic alterations. Blood, 119(10), e67–e75.
Kusec, R., Laczika, K., Knöbl, P., et al. (1994). AML1/ETO fusion mRNA can be detected in remission blood samples of all patients with t(8;21) acute myeloid leukemia after chemotherapy or autologous bone marrow transplantation. Leukemia, 8(5), 735–739.
Larson, R. A., Le Beau, M. M., Vardiman, J. W., et al. (1983). The predictive value of initial cytogenetic studies in 148 adults with acute nonlymphocytic leukemia: A 12-year study (1970–1982). Cancer Genetics and Cytogenetics, 10(3), 219–236.
Lavallée, V.-P., Lemieux, S., Boucher, G., et al. (2016). RNA-sequencing analysis of core binding factor AML identifies recurrent ZBTB7A mutations and defines RUNX1-CBFA2T3 fusion signature. Blood, 127(20), 2498–2501.
Le Beau, M. M., Larson, R. A., Bitter, M. A., et al. (1983). Association of an inversion of chromosome 16 with abnormal marrow eosinophils in acute myelomonocytic leukemia. A unique cytogenetic-clinicopathological association. The New England Journal of Medicine, 309(11), 630–636.
Leroy, H., de Botton, S., Grardel-Duflos, N., et al. (2005). Prognostic value of real-time quantitative PCR (RQ-PCR) in AML with t(8;21). Leukemia, 19(3), 367–372.
Leverger, G., Bernheim, A., Daniel, M. T., Flandrin, G., et al. (1988). Cytogenetic study of 130 childhood acute nonlymphocytic leukemias. Medical and Pediatric Oncology, 16(4), 227–232.
Liu, P., Tarlé, S. A., Hajra, A., et al. (1993). Fusion between transcription factor CBF beta/PEBP2 beta and a myosin heavy chain in acute myeloid leukemia. Science, 261(5124), 1041–1044.
Löwenberg, B., Ossenkoppele, G. J., van Putten, W., et al. (2009). High-dose daunorubicin in older patients with acute myeloid leukemia. The New England Journal of Medicine, 361(13), 1235–1248.
Löwenberg, B., Pabst, T., Vellenga, E., et al. (2011). Cytarabine dose for acute myeloid leukemia. The New England Journal of Medicine, 364(11), 1027–1036.
Lugthart, S., Gröschel, S., Beverloo, H. B., et al. (2010). Clinical, molecular, and prognostic significance of WHO type inv(3)(q21q26.2)/t(3;3)(q21;q26.2) and various other 3q abnormalities in acute myeloid leukemia. Journal of Clinical Oncology, 28(24), 3890–3898.
Marcucci, G., Livak, K. J., Bi, W., et al. (1998). Detection of minimal residual disease in patients with AML1/ETO-associated acute myeloid leukemia using a novel quantitative reverse transcription polymerase chain reaction assay. Leukemia, 12(9), 1482–1489.
Marcucci, G., Mrózek, K., Ruppert, A. S., et al. (2005). Prognostic factors and outcome of core binding factor acute myeloid leukemia patients with t(8;21) differ from those of patients with inv(16): A cancer and leukemia group B study. Journal of Clinical Oncology, 23(24), 5705–5717.
Mendler, J. H., Maharry, K., Radmacher, M. D., et al. (2012). RUNX1 mutations are associated with poor outcome in younger and older patients with cytogenetically normal acute myeloid leukemia and with distinct gene and MicroRNA expression signatures. Journal of Clinical Oncology, 30(25), 3109–3118.
Metzeler, K. H., Herold, T., Rothenberg-Thurley, M., et al. (2016). Spectrum and prognostic relevance of driver gene mutations in acute myeloid leukemia. Blood, 128(5), 686–698.
Michaud, J., Wu, F., Osato, M., et al. (2002). In vitro analyses of known and novel RUNX1/AML1 mutations in dominant familial platelet disorder with predisposition to acute myelogenous leukemia: Implications for mechanisms of pathogenesis. Blood, 99(4), 1364–1372.
Micol, J. B., Duployez, N., Boissel, N., et al. (2014). Frequent ASXL2 mutations in acute myeloid leukemia patients with t(8;21)/RUNX1-RUNX1T1 chromosomal translocations. Blood, 124(9), 1445–1449.
Miller, C. A., Wilson, R. K., & Ley, T. J. (2013). Genomic landscapes and clonality of de novo AML. The New England Journal of Medicine, 369(15), 1473.
Mitani, K., Ogawa, S., Tanaka, T., et al. (1994). Generation of the AML1-EVI-1 fusion gene in the t(3;21)(q26;q22) causes blastic crisis in chronic myelocytic leukemia. EMBO Journal, 13(3), 504–510.
Mitelman, F., Johansson, B., & Mertens, F. (Eds.). (2016). Mitelman database of chromosome aberrations and gene fusions in cancer [Online]. http://cgap.nci.nih.gov/Chromosomes/Mitelman.
Miyamoto, T., Nagafuji, K., Akashi, K., et al. (1996). Persistence of multipotent progenitors expressing AML1/ETO transcripts in long-term remission patients with t(8;21) acute myelogenous leukemia. Blood, 87(11), 4789–4796.
Miyamoto, T., Weissman, I. L., & Akashi, K. (2000). AML1/ETO-expressing nonleukemic stem cells in acute myelogenous leukemia with 8;21 chromosomal translocation. Proceedings of the National Academy of Sciences USA, 97(13), 7521–7526.
Miyawaki, S., Ohtake, S., Fujisawa, S., et al. (2011). A randomized comparison of 4 courses of standard-dose multiagent chemotherapy versus 3 courses of high-dose cytarabine alone in postremission therapy for acute myeloid leukemia in adults: The JALSG AML201 study. Blood, 117(8), 2366–2372.
Miyoshi, H., Shimizu, K., Kozu, T., et al. (1991). t(8;21) breakpoints on chromosome 21 in acute myeloid leukemia are clustered within a limited region of a single gene, AML1. Proceedings of the National Academy of Sciences USA, 88(23), 10431–10434.
Miyoshi, H., Kozu, T., Shimizu, K., et al. (1993). The t(8;21) translocation in acute myeloid leukemia results in production of an AML1-MTG8 fusion transcript. The EMBO Journal, 12(7), 2715–2721.
Miyoshi, H., Ohira, M., SHimizu, K., et al. (1995). Alternative splicing and genomic structure of the AML1 gene involved in acute myeloid leukemia. Nucleic Acids Research, 23(14), 2762–2769.
Moorman, A. V., Ensor, H. M., Richards, S. M., et al. (2010). Prognostic effect of chromosomal abnormalities in childhood B-cell precursor acute lymphoblastic leukaemia: results from the UK Medical Research Council ALL97/99 randomised trial. Lancet Oncology, 11(5), 429–438.
Mori, H., Colman, S. M., Xiao, Z., et al. (2002). Chromosome translocations and covert leukemic clones are generated during normal fetal development. Proceedings of the National Academy of Sciences USA, 99(12), 8242–8247.
Morschhauser, F., Cayuela, J. M., Martini, S., et al. (2000). Evaluation of minimal residual disease using reverse-transcription polymerase chain reaction in t(8;21) acute myeloid leukemia: A multicenter study of 51 patients. Journal of Clinical Oncology, 18(4), 788–794.
Mrózek, K., Heerema, N. A., & Bloomfield, C. D. (2004). Cytogenetics in acute leukemia. Blood Reviews, 18(2), 115–136.
Mullighan, C. G., Goorha, S., Radtke, I., et al. (2007). Genome-wide analysis of genetic alterations in acute lymphoblastic leukaemia. Nature, 446(7137), 758–764.
Nanri, T., Matsuno, N., Kawakita, T., et al. (2005a). Imatinib mesylate for refractory acute myeloblastic leukemia harboring inv(16) and a C-KIT exon 8 mutation. Leukemia, 19(9), 1673–1675.
Nanri, T., Matsuno, N., Kawakita, T., et al. (2005b). Mutations in the receptor tyrosine kinase pathway are associated with clinical outcome in patients with acute myeloblastic leukemia harboring t(8;21)(q22;q22). Leukemia, 19(8), 1361–1366.
Nucifora, G., & Rowley, J. D. (1994). The AML1 and ETO genes in acute myeloid leukemia with a t(8;21). Leukemia & Lymphoma, 14(5–6), 353–362.
Nucifora, G., Larson, R. A., & Rowley, J. D. (1993). Persistence of the 8;21 translocation in patients with acute myeloid leukemia type M2 in long-term remission. Blood, 82(3), 712–715.
Nucifora, G., Begy, C. R., Kobayashi, H., et al. (1994). Consistent intergenic splicing and production of multiple transcripts between AML1 at 21q22 and unrelated genes at 3q26 in (3;21)(q26;q22) translocations. Proceedings of the National Academy of Sciences USA, 91(9), 4004–4008.
Osato, M. (2004). Point mutations in the RUNX1/AML1 gene: Another actor in RUNX leukemia. Oncogene, 23(24), 4284–4296.
Osato, M., Asou, N., Abdalla, E., et al. (1999). Biallelic and Heterozygous Point Mutations in the runt domain of the AML1/PEBP2alphaB gene associated eith myeloblastic leukemias. Blood, 93(6), 1817–1824.
Osato, M., Yanagida, M., Shigesada, K., & Ito, Y. (2001). Point mutations of the RUNX1/AML1 gene in sporadic and familial myeloid leukemias. International Journal of Hematology, 74(3), 245–251.
Owen, C. J., Toze, C. L., Koochin, A., et al. (2008). Five new pedigrees with inherited RUNX1 mutations causing familial platelet disorder with propensity to myeloid malignancy. Blood, 112(12), 4639–4645.
Pallisgaard, N., Clausen, N., Schroder, H., & Hokland, P. (1999). Rapid and sensitive minimal residual disease detection in acute leukemia by quantitative real-time RT-PCR exemplified by t(12;21) TEL-AML1 fusion transcript. Genes, Chromosomes and Cancer, 26(4), 355–365.
Papaemmanuil, E., Gerstung, M., Malcovati, L., et al. (2013). Clinical and biological implications of driver mutations in myelodysplastic syndromes. Blood, 122(22), 3616–3627 -quiz 3699.
Paquette, R. L., Nicoll, J., Chalukya, M., et al. (2011). Frequent EVI1 translocations in myeloid blast crisis CML that evolves through tyrosine kinase inhibitors. Cancer Genetics, 204(7), 392–397.
Paschka, P., & Döhner, K. (2013). Core-binding factor acute myeloid leukemia: Can we improve on HiDAC consolidation? Hematology. American Society of Hematology. Education Program, 2013(1), 209–219.
Paschka, P., Marcucci, G., Ruppert, A. S., et al. (2006). Adverse prognostic significance of KIT mutations in adult acute myeloid leukemia with inv(16) and t(8;21): A cancer and leukemia group B study. Journal of Clinical Oncology, 24(24), 3904–3911.
Paschka, P., Du, J., Schlenk, R. F., et al. (2013). Secondary genetic lesions in acute myeloid leukemia with inv(16) or t(16;16): A study of the German-Austrian AML study group (AMLSG). Blood, 121(1), 170–177.
Paschka, P., Schlenk, R. F., Gaidzik, V. I., et al. (2015). ASXL1 mutations in younger adult patients with acute myeloid leukemia: A study by the German-Austrian acute myeloid leukemia study group. Haematologica, 100(3), 324–330.
Patel, J. P., Gönen, M., Figueroa, M. E., et al. (2012). Prognostic relevance of integrated genetic profiling in acute myeloid leukemia. The New England Journal of Medicine, 366(12), 1079–1089.
Pedersen-Bjergaard, J., & Philip, P. (1991). Balanced translocations involving chromosome bands 11q23 and 21q22 are highly characteristic of myelodysplasia and leukemia following therapy with cytostatic agents targeting at DNA-topoisomerase II. Blood, 78(4), 1147–1148.
Petersdorf, S. H., Kopecky, K. J., Slovak, M., et al. (2013). A phase 3 study of gemtuzumab ozogamicin during induction and postconsolidation therapy in younger patients with acute myeloid leukemia. Blood, 121(24), 4854–4860.
Pollard, J. A., Alonzo, T. A., Gerbing, R. B., et al. (2010). Prevalence and prognostic significance of KIT mutations in pediatric patients with core binding factor AML enrolled on serial pediatric cooperative trials for de novo AML. Blood, 115(12), 2372–2379.
Prébet, T., Boissel, N., Reutenauer, S., et al. (2009). Acute myeloid leukemia with translocation (8;21) or inversion (16) in elderly patients treated with conventional chemotherapy: A collaborative study of the French CBF-AML intergroup. Journal of Clinical Oncology, 27(28), 4747–4753.
Prébet, T., Carbuccia, N., Raslova, H., et al. (2013). Concomitant germ-line RUNX1 and acquired ASXL1 mutations in a T-cell acute lymphoblastic leukemia. European Journal of Haematology, 91(3), 277–279.
Prébet, T., Bertoli, S., Delaunay, J., et al. (2014). Anthracycline dose intensification improves molecular response and outcome of patients treated for core binding factor acute myeloid leukemia. Haematologica, 99(10), e185–e187.
Preudhomme, C., Warot-Loze, D., Roumier, C., et al. (2000). High incidence of biallelic point mutations in the Runt domain of the AML1/PEBP2 alpha B gene in Mo acute myeloid leukemia and in myeloid malignancies with acquired trisomy 21. Blood, 96(8), 2862–2869.
Preudhomme, C., Renneville, A., Bourdon, V., et al. (2009). High frequency of RUNX1 biallelic alteration in acute myeloid leukemia secondary to familial platelet disorder. Blood, 113(22), 5583–5587.
Raimondi, S. C., Chang, M. N., Ravindranath, Y., et al. (1999). Chromosomal abnormalities in 478 children with acute myeloid leukemia: Clinical characteristics and treatment outcome in a cooperative pediatric oncology group study-POG 8821. Blood, 94(11), 3707–3716.
Raynaud, S., Cave, H., Baens, M., et al. (1996). The 12;21 translocation involving TEL and deletion of the other TEL allele: Two frequently associated alterations found in childhood acute lymphoblastic leukemia. Blood, 87(7), 2891–2899.
Richkind, K., Hromas, R., Lytle, C., et al. (2000). Identification of two new translocations that disrupt the AML1 gene. Cancer Genetics, 122(2), 141–143.
Romana, S. P., Mauchauffé, M., Le Coniat, M., et al. (1995a). The t(12;21) of acute lymphoblastic leukemia results in a tel-AML1 gene fusion. Blood, 85(12), 3662–3670.
Romana, S. P., Poirel, H., Leconiat, M., et al. (1995b). High frequency of t(12;21) in childhood B-lineage acute lymphoblastic leukemia. Blood, 86(11), 4263–4269.
Roumier, C., Fenaux, P., Lafage, M., et al. (2003). New mechanisms of AML1 gene alteration in hematological malignancies. Leukemia, 17(1), 9–16.
Rowley, J. D. (1973). Identificaton of a translocation with quinacrine fluorescence in a patient with acute leukemia. Annales de Génétique, 16(2), 109–112.
Rowley, J. D. (1980). General report on the second international workshop on chromosomes in leukemia. International Journal of Cancer, 26(5), 531–533.
Rowley, J. D., & de la Chapelle, A. (1978). General report on the first international workshop on chromosomes in leukemia. International Journal of Cancer, 21(3), 307–308.
Rubin, C. M., Larson, R. A., Bitter, M. A., et al. (1987). Association of a chromosomal 3;21 translocation with the blast phase of chronic myelogenous leukemia. Blood, 70(5), 1338–1342.
Rubin, C. M., Larson, R. A., Anastasi, J., et al. (1990). t(3;21)(q26;q22): A recurring chromosomal abnormality in therapy-related myelodysplastic syndrome and acute myeloid leukemia. Blood, 76(12), 2594–2598.
Sakai, I., Tamura, T., Narumi, H., et al. (2005). Novel RUNX1-PRDM16 fusion transcripts in a patient with acute myeloid leukemia showing t(1;21)(p36;q22). Genes, Chromosomes and Cancer, 44(3), 265–270.
Satake, N., Maseki, N., Kozu, T., et al. (1995). Disappearance of AML1-MTG8(ETO) fusion transcript in acute myeloid leukaemia patients with t(8;21) in long-term remission. British Journal of Haematology, 91(4), 892–898.
Schittenhelm, M. M., Shiraga, S., Schroeder, A., et al. (2006). Dasatinib (BMS-354825), a dual SRC/ABL kinase inhibitor, inhibits the kinase activity of wild-type, juxtamembrane, and activation loop mutant KIT isoforms associated with human malignancies. Cancer Research, 66(1), 473–481.
Schlenk, R. F., Benner, A., Krauter, J., et al. (2004). Individual patient data-based meta-analysis of patients aged 16 to 60 years with core binding factor acute myeloid leukemia: A survey of the German acute myeloid leukemia intergroup. Journal of Clinical Oncology, 22(18), 3741–3750.
Schlenk, R. F., Pasquini, M. C., Pérez, W. S., et al. (2008). HLA-identical sibling allogeneic transplants versus chemotherapy in acute myelogenous leukemia with t(8;21) in first complete remission: Collaborative study between the German AML intergroup and CIBMTR. Biology of Blood and Marrow Transplantation, 14(2), 187–196.
Schnittger, S., Kohl, T. M., Haferlach, T., et al. (2006). KIT-D816 mutations in AML1-ETO-positive AML are associated with impaired event-free and overall survival. Blood, 107(5), 1791–1799.
Schnittger, S., Dicker, F., Kern, W., et al. (2011). RUNX1 mutations are frequent in de novo AML with noncomplex karyotype and confer an unfavorable prognosis. Blood, 117(8), 2348–2357.
Schnittger, S., Eder, C., Jeromin, S., et al. (2013). ASXL1 exon 12 mutations are frequent in AML with intermediate risk karyotype and are independently associated with an adverse outcome. Leukemia, 27(1), 82–91.
Schoch, C., Haase, D., Haferlach, T., et al. (1996). Fifty-one patients with acute myeloid leukemia and translocation t(8;21)(q22;q22): An additional deletion in 9q is an adverse prognostic factor. Leukemia, 10(8), 1288–1295.
Schwab, C. J., Chilton, L., Morrison, H., et al. (2013). Genes commonly deleted in childhood B-cell precursor acute lymphoblastic leukemia: Association with cytogenetics and clinical features. Haematologica, 98(7), 1081–1088.
Seeger, K., Kreuzer, K. A., Lass, U., et al. (2001). Molecular quantification of response to therapy and remission status in TEL-AML1-positive childhood ALL by real-time reverse transcription polymerase chain reaction. Cancer Research, 61(6), 2517–2522.
Shurtleff, S. A., Buijs, A., Behm, F. G., et al. (1995). TEL/AML1 fusion resulting from a cryptic t(12;21) is the most common genetic lesion in pediatric ALL and defines a subgroup of patients with an excellent prognosis. Leukemia, 9(12), 1985–1989.
Slovak, M. L., Kopecky, K. J., Cassileth, P. A., et al. (2000). Karyotypic analysis predicts outcome of preremission and postremission therapy in adult acute myeloid leukemia: A Southwest Oncology Group/Eastern Cooperative Oncology Group Study. Blood, 96(13), 4075–4083.
Slovak, M. L., Bedell, V., Popplewell, L., et al. (2002). 21q22 balanced chromosome aberrations in therapy-related hematopoietic disorders: Report from an international workshop. Genes, Chromosomes and Cancer, 33(4), 379–394.
Song, W. J., Sullivan, M. G., Legare, R. D., et al. (1999). Haploinsufficiency of CBFA2 causes familial thrombocytopenia with propensity to develop acute myelogenous leukaemia. Nature Genetics, 23(2), 166–175.
Sood, R., Hansen, N. F., Donovan, F. X., et al. (2016). Somatic mutational landscape of AML with inv(16) or t(8;21) identifies patterns of clonal evolution in relapse leukemia. Leukemia, 30(2), 501–504.
Speck, N. A., & Gilliland, D. G. (2002). Core-binding factors in haematopoiesis and leukaemia. Nature Reviews Cancer, 2(7), 502–513.
Swansbury, G. J., Lawler, S. D., Alimena, G., et al. (1994). Long-term survival in acute myelogenous leukemia: A second follow-up of the fourth international workshop on chromosomes in leukemia. Cancer Genetics and Cytogenetics, 73(1), 1–7.
Taketani, T., Taki, T., Takita, J., et al. (2003). AML1/RUNX1 mutations are infrequent, but related to AML-M0, acquired trisomy 21, and leukemic transformation in pediatric hematologic malignancies. Genes, Chromosomes and Cancer, 38(1), 1–7.
Tang, J. L., Hou, H. A., Chen, C. Y., et al. (2009). AML1/RUNX1 mutations in 470 adult patients with de novo acute myeloid leukemia: Prognostic implication and interaction with other gene alterations. Blood, 114(26), 5352–5361.
Tobal, K., & Yin, J. A. (1996). Monitoring of minimal residual disease by quantitative reverse transcriptase-polymerase chain reaction for AML1-MTG8 transcripts in AML-M2 with t(8; 21). Blood, 88(10), 3704–3709.
Tobal, K., Newton, J., Macheta, M., et al. (2000). Molecular quantitation of minimal residual disease in acute myeloid leukemia with t(8;21) can identify patients in durable remission and predict clinical relapse. Blood, 95(3), 815–819.
Valk, P. J., Verhaak, R. G., Beijen, M. A., et al. (2004). Prognostically useful gene-expression profiles in acute myeloid leukemia. The New England Journal of Medicine, 350(16), 1617–1628.
van Dongen, J. J. M., Macintyre, E. A., Gabert, J. A., et al. (1999). Standardized RT-PCR analysis of fusion gene transcripts from chromosome aberrations in acute leukemia for detection of minimal residual disease. Report of the BIOMED-1 Concerted Action: Investigation of minimal residual disease in acute leukemia. Leukemia, 13(12), 1901–1928.
von Neuhoff, C., Reinhardt, D., Sander, A., et al. (2010). Prognostic impact of specific chromosomal aberrations in a large group of pediatric patients with acute myeloid leukemia treated uniformly according to trial AML-BFM 98. Journal of Clinical Oncology, 28(16), 2682–2689.
Wang, Y. Y., Zhou, G. B., Yin, T., et al. (2005). AML1-ETO and C-KIT mutation/overexpression in t(8;21) leukemia: Implication in stepwise leukemogenesis and response to Gleeve. Proceedings of the National Academy of Sciences USA, 102(4), 1104–1109.
Wang, Y., Wu, D.-P., Liu, Q.-F., et al. (2014). In adults with t(8;21)AML, posttransplant RUNX1/RUNX1T1-based MRD monitoring, rather than c-KIT mutations, allows further risk stratification. Blood, 124(12), 1880–1886.
Wiemels, J. L., Cazzaniga, G., Daniotti, M., et al. (1999a). Prenatal origin of acute lymphoblastic leukaemia in children. Lancet, 354(9189), 1499–1503.
Wiemels, J. L., Ford, A. M., Van Wering, E. R., et al. (1999b). Protracted and variable latency of acute lymphoblastic leukemia after TEL-AML1 gene fusion in utero. Blood, 94(3), 1057–1062.
Willekens, C., Blanchet, O., Renneville, A., et al. (2016). Prospective long-term minimal residual disease monitoring using RQ-PCR in RUNX1-RUNX1T1-positive acute myeloid leukemia: Results of the French CBF-2006 trial. Haematologica, 101(3), 328–335.
Yin, J. A., O’Brien, M. A., Hills, R. K., et al. (2012). Minimal residual disease monitoring by quantitative RT-PCR in core binding factor AML allows risk stratification and predicts relapse: Results of the United Kingdom MRC AML-15 trial. Blood, 120(14), 2826–2835.
Yoshimi, A., Toya, T., Kawazu, M., et al. (2014). Recurrent CDC25C mutations drive malignant transformation in FPD/AML. Nature Communications, 5, 4770.
Zelent, A., Greaves, M., & Enver, T. (2004). Role of the TEL-AML1 fusion gene in the molecular pathogenesis of childhood acute lymphoblastic leukaemia. Oncogene, 23(24), 4275–4283.
Zhang, J., Ding, L., Holmfeldt, L., et al. (2012). The genetic basis of early T-cell precursor acute lymphoblastic leukaemia. Nature, 481(7380), 157–163.
Zharlyganova, D., Harada, H., Harada, Y., et al. (2008). High frequency of AML1/RUNX1 point mutations in radiation-associated myelodysplastic syndrome around semipalatinsk nuclear test site. Journal of Radiation Research, 49(5), 549–155.
Zhu, H. H., Zhang, X. H., Qin, Y. Z., et al. (2013). MRD-directed risk stratification treatment may improve outcomes of t(8;21) AML in the first complete remission: Results from the AML05 multicenter trial. Blood, 121(20), 4056–4062.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Metzeler, K.H., Bloomfield, C.D. (2017). Clinical Relevance of RUNX1 and CBFB Alterations in Acute Myeloid Leukemia and Other Hematological Disorders. In: Groner, Y., Ito, Y., Liu, P., Neil, J., Speck, N., van Wijnen, A. (eds) RUNX Proteins in Development and Cancer. Advances in Experimental Medicine and Biology, vol 962. Springer, Singapore. https://doi.org/10.1007/978-981-10-3233-2_12
Download citation
DOI: https://doi.org/10.1007/978-981-10-3233-2_12
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-10-3231-8
Online ISBN: 978-981-10-3233-2
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)