Abstract
Worldwide, thalassemia is the most commonly inherited hemolytic anemia, and it is most prevalent in Asia and the Middle East. Iron overload represents a significant problem in patients with transfusion-dependent β-thalassemia. Chelation therapy with deferoxamine has traditionally been the standard therapeutic option but its usage is tempered by suboptimal patient compliance due to the discomfort and demands associated with the administration regimen. Therefore, a great deal of attention has been focused on the development of oral chelating agents. Deferiprone, even though available for nearly two decades in Asia with recent encouraging data on cardiac iron removal and long-term efficacy, has serious adverse effects including agranulocytosis and neutropenia which has impeded it from routine clinical practice. A novel oral chelator; deferasirox is effective throughout a 24 h dosing period and both preclinical and clinical data indicate that it successfully removes both hepatic and cardiac iron. In Asia, optimal management of severe thalassemia patients and the availability and access to oral iron chelators still presents a major challenge in many countries. In this regard, the development and implementation of consensus guidelines for management of Asian patients with transfusion-dependent thalassemia will be a major step towards improving and maintaining the continuity of patient care.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Thalassemia is a heterogeneous group of inherited disorders characterized by the complete or partial suppression of production of normal hemoglobin due to defective synthesis of one or more globin chains [1, 2]. Thalassemia is classified according to the particular globin chain that is affected (e.g., α-, β-thalassemia). Over 250 different mutations, primarily affecting the coding sequences of either α or β globin genes, have been described [3, 4]. These mutations mainly include deletion and non-deletion mutations with few exceptions of mutations involved in the up-stream regulatory elements [3, 5].
α-thalassemia largely results from the deletion of one to four α-globin genes, and the clinical severity is dependent on the number of remaining α-globin genes. In general, individuals lacking one α gene (αα/-α) have no clinical and hematological phenotype, while the severity increases with the number of α globin genes missing. They may be present as mild hypochromic microcytosis when there is a deletion of two α genes; (--/αα or -α/-α), moderate anemia with possible hemolytic crisis when deletion of three α genes; (--/-α) and hydrops fetalis or intrauterine death caused by the deletion of all four α-globin genes; (--/--) [6].
Inheritance of one β-thalassemia gene results in the thalassemia trait (thalassemia minor), inheritance of two defective β-globin genes, can result in a wide ranged spectrum of clinical conditions depending on the type of β-thalassemia mutation (either β0 or β+ thalassemia) and several other known and uncertain genetic factors [2]. Therefore, the clinical phenotype in β-thalassemia can range from mild-to-moderate anemia (thalassemia intermedia) or may result in transfusion dependence (thalassemia major). Without proper management, including adequate transfusion therapy, severe anemia can result in increased erythropoietin production, expansion of ineffective bone marrow, bone deformities, splenomegaly and growth retardation [2].
In Asian populations where both α- and β-thalassemia are highly prevalent, structural hemoglobin variants known as hemoglobinopathy are also common; these involve hemoglobins S, C and E. Individuals may inherit the gene for thalassemia from one parent and the gene for a hemoglobin variant from the other parent. The most clinically important type is hemoglobin E/β thalassemia syndrome that has a wide clinical severity ranging from mild thalassemia intermedia to transfusion dependence mimicking that of thalassemia major [2, 7–10].
Thalassemia is the most commonly inherited hemolytic anemia worldwide and due to the large population and high prevalence of thalassemia carriers, Asia and the Middle East account for 95% of overall thalassemia births [7]. Globally, it has been estimated that there are 300 million carriers of hemoglobin disorders, with the majority living in South East Asia. In Thailand alone, the frequency of α-thalassemia is 25%, and the World Health Organisation estimates that, without effective prevention and control programs, over 250,000 symptomatic patients will be diagnosed in this country over the next few decades [8]. A similar scenario is predicted to occur in India, Sri Lanka, Indonesia, the Philippines and Malaysia [1]. With a population of approximately 25 million, Malaysia has a β-thalassemia carrier rate of 4–5%. In a census done in 1998, transfusion-dependent β-thalassemia patients numbered 2,248, with a large proportion located in the state of Sabah [11]. The prevalence of various types of thalassemia in Asia is summarized in Table 1.
With limited resources in most of Asian countries, it is important that a prevention and control program for severe thalassemia syndromes be implemented. A National Thalassemia Screening Program, launched in 1993, with targeted screening done in early pregnancy had resulted in a decrease in the number of β-thalassemia major births in Taiwan. Approximately only 100 new cases were detected over the 10-year period from 1994 to 2003, usually due to a failure to detect parental risks [12]. In Singapore, the National Thalassemia Registry was established in 1992 with the aim of registering all individuals with thalassemia genes and offering counselling and subsidized screening for spouses and first degree relatives. As a result, there was a significant increase in the number of thalassemia carriers diagnosed and the number of thalassemia major births is now close to zero [13]. Similarly, in Hong Kong, a prenatal diagnostic screening program using DNA techniques had been established since 1982 for the diagnosis of thalassemia and other genetic disorders with significant success [14, 15].
In patients with severe β-thalassemia, although stem cell transplantation might be the treatment of choice in patients who have HLA-matched donors, such treatment has several drawbacks including limited availability of matched donors, cost of treatment, treatment related mortalities and morbidity and long-term consequences due to exposure of chemotherapy for patients’ conditioning. Therefore, the mainstay of management for most patients consists of regular blood transfusions supplemented with iron chelation therapy to prevent the effects of iron accumulation [16, 17]. Over a period of time, various transfusion regimes have been put in practice. The aim has been to promote normal growth, allow normal physical activities, minimize transfusional iron accumulation, adequately suppress bone marrow activity and reduce cardiac overload due to chronic anemia [16]. Hemoglobin levels maintained at 9–10 g/dl are thought of as optimal [18]. A higher target pre-transfusion hemoglobin level of 11–12 g/dl may be appropriate for patients with heart disease or other medical conditions [16]. Regular transfusions can be given every 3–4 weeks using leukocyte filtered, packed red blood cells with a minimum hemoglobin content of 40 g. Washed red cells may be beneficial for patients with thalassemia who have repeated severe allergic transfusion reactions. Frozen (or cryopreserved) red cells are used to maintain a supply of rare donor units for certain patients who have unusual red cell antibodies or who are missing common red cell antigens; Neocyte or young red cell transfusion may modestly reduce blood requirements, however, this approach has not been widely adopted due to several limitations [16].
2 Transfusion-dependent iron overload
As mentioned above, patients with severe β-thalassemia, particularly β-thalassemia major, require regular blood transfusions supplemented with iron chelation therapy to prevent the effects of iron accumulation [2, 19]. The Thalassemia International Federation (TIF) recommends regular blood transfusions, usually administered every 2–5 weeks, to maintain the pre-transfusion hemoglobin level above 9–10.5 g/dL [20]. Despite the judicious use of blood transfusions due to resource constraints or less dependence on transfusion therapy, many children with thalassemia may become iron loaded as a result of increased iron absorption from the diet [7].
An unfortunate consequence of transfusion therapy in transfusion dependent thalassemia is the accumulation of iron and the necessity for iron chelation therapy [21]. Excess iron can potentially penetrate cells in the liver, heart, endocrine glands and other organs, and cause progressive tissue damage by generation of hydroxyl free radicals causing oxidative stress [19, 21, 22]. The human body has a limited capacity to control iron through the tight binding of plasma iron to transferrin (Tf) protein, which will become completely saturated in heavily iron loaded patients. As a consequence, non-transferrin bound iron (NTBI) including labile plasma iron (LPI) are generated and free radical formation is accelerated in several organs and tissues [23]. Mortality in patients with β-thalassemia is primarily due to heart disease followed by infection, liver disease and malignancy [24]. The mechanism(s) by which cardiac tissue is susceptible to iron overload are not well understood.
There is a clear link between the overall iron burden and global toxicity; in patients with thalassemia the liver iron concentration (LIC) correlates with the total body iron load [22]. Serum ferritin and LIC are widely used to detect iron overload, and the latter can be measured by magnetic resonance imaging (MRI), Superconducting Quantum Interference Device (SQUID) or liver biopsy. Evidence indicates that serum ferritin is not an accurate measure of iron overload and that direct measurement of LIC via liver biopsy or MRI is more precise [25, 26]. It should be noted that the correct interpretation of LIC by liver biopsy is highly dependent on biologic, technical and analytical variability, which may be explained by factors such as the size of the biopsy sample and the possible variability in iron distribution within the liver. Alternatively, MRI offers a non-invasive option for the estimation of LIC and average iron content for the whole liver can be calculated [25].
In patients with thalassemia, iron overload can be prevented or treated with the use of a chelating agent capable of forming a complex with iron and promoting its excretion. The efficacy of a chelating agent will be partly determined by its ability to bind NTBI and LPI over sustained periods of time as an effective means to reduce excess cellular iron and iron loading in organs [22, 23].
2.1 Thalassemia intermedia: need for iron chelation
Thalassemia intermedia (HbE/β-thalassemia), is a heterogeneous condition with a wide variety of clinical presentations. In these patients, anemia can range from relatively mild (hemoglobin >10 g/dL) to severe (hemoglobin <4 g/dL). If not receiving adequate treatment, patients with moderate to severe HbE/β-thalassemia are at high risk of poor growth development [27]. The problem of iron overload in patients with thalassemia intermedia is significant, and increases with advancing age [7, 10].
While in thalassemia major, a significant correlation, although not absolute, has been demonstrated between the levels of serum ferritin and LIC (as assessed by MRI), in thalassemia intermedia there is limited data correlating these two parameters. Preliminary data suggested that in patients with thalassemia intermedia, there is a weaker correlation between serum ferritin levels and LIC than that observed in patients with thalassemia major. Serum ferritin levels underestimated the severity of iron overload in patients with thalassemia intermedia and therefore have little value in monitoring iron overload and iron chelation therapy in this group of patients [28–30]. Using levels of serum ferritin to determine the degree of iron overload could lead to a delay in chelation therapy for these patients. In transfusion-naïve thalassemia intermedia patients, LIC from liver biopsy but not serum ferritin is a good predictor of the extent of iron overload and may be used to determine the need for chelation therapy. Alternatively, LIC assessments such as MRI should be used in these patients [28].
3 Iron chelation therapy
3.1 Deferoxamine
To date, the management of iron overload has largely consisted of chelation therapy with parenteral deferoxamine (Desferal™). Deferoxamine has been the standard therapeutic option for thalassemia in the past 40 years [31–33]. A recent prospective evaluation of changes in ferritin levels and LIC in 290 thalassemia major patients [20] demonstrated that a mean daily dose of deferoxamine 42 mg/kg resulted in a decrease in serum ferritin of 364 μg/L at 1 year, whereas a mean daily dose of deferoxamine 51 mg/kg resulted in an average serum ferritin decrease of approximately 1,000 μg/L over 1 year. Deferoxamine is able to effectively maintain normal/near normal iron stores, reduce organ damage and increase life expectancy in patients with thalassemia [7]. It is therefore, still the only acceptable active comparator in clinical studies with newer iron chelators. However, patient compliance is suboptimal due to the discomfort and demands associated with the administration regimen [21, 33, 34]. Within the Asian population, there are scant data regarding deferoxamine compliance. Recently an analysis of 120 Thai patients with β-thalassemia, who had been receiving subcutaneous deferoxamine for >2 years (maximum of 12 years), demonstrated that only 14% of cases could be classified as having good compliance [35]. The major obstacles for achieving optimal compliance included inconvenience, pain and the complexity and discomfort of deferoxamine administration [35]. These findings indicate that although deferoxamine has long been available in Asia, there are significant limitations with regard to its use and compliance for the long-term control of iron overload.
Deferoxamine is associated with an increased risk of infection which necessitates suspension of treatment [17]. Dose-related complications (e.g., hearing problems, growth retardation and ocular toxicity) may also occur in patients who are not heavily iron loaded and who receive a high dosage of deferoxamine. Therefore, attention has been focused on the development of iron chelating agents that can be administered orally. Currently, oral deferiprone (L1, Ferriprox® or Kelfer®) is only licensed in Europe and Asia. Oral deferasirox (Exjade®) has however, been extensively studied in adults and children and approved in over 85 countries worldwide, including the USA and Europe, for the treatment of transfusion-induced iron overload [36]. A summary of product characteristics of the available iron chelators is provided in Table 2.
3.2 Deferiprone (L1)
Deferiprone is an orally absorbed iron chelator first licensed in India, followed by the European Union and other countries outside US and Canada, inclusive of others in Asia in the late 1990s. It is indicated mainly for use in patients with thalassemia major for whom deferoxamine therapy is contra-indicated or who present serious toxicity with deferoxamine therapy [37].
3.2.1 Clinical pharmacology
Deferiprone is a bidentate ligand which binds to iron atoms in a 3:1 molar ratio. In humans, the drug is rapidly metabolized and inactivated in the liver by glucuronidation of one of its iron binding sites. The elimination half-life in most patients is 2–3 h. Therefore, it has to be given three times a day [37]. It is eliminated mainly via the kidneys in the forms of free deferiprone, the glucuronide metabolite and the iron-deferiprone complex [37].
According to the summary of product characteristics [37], deferiprone therapy should be initiated and maintained by a physician experienced in the treatment of patients with thalassemia. It is given as 25 mg/kg body weight three times a day for a total daily dose of 75 mg/kg body weight. Doses above 100 mg/kg/day are not recommended because of the potentially increased risk of adverse reactions. It is recommended that serum ferritin concentrations be monitored monthly or at least every 2 months to access the long-term effectiveness of chelation with deferiprone. There are limited data available on the use of deferiprone in children between 6 and 10 years of age, and no data on its use in children under 6 years of age. Since deferiprone has been shown to cause neutropenia, including agranulocytosis, it is recommended that a patient’s absolute neutrophil count (ANC) be monitored every week. If the patient develops an infection, the therapy should be interrupted and the neutrophil count monitored more frequently.
3.2.2 Clinical experience
Several clinical studies demonstrated that deferiprone was effective in promoting iron excretion and can prevent the progression of iron accumulation as assessed by serum ferritin, in transfusion-dependent thalassemia patients. In the recent Cochrane review of all 10 available randomized controlled trials with deferiprone, the authors however, reported that there was little consistency between outcomes of these studies and little information to fully assess the methodological quality [38]. There was also no controlled trial reporting long-term outcomes (such as mortality and end organ damage) and no consistent effect on reduction of iron overload between all treatment comparisons [38].
Recent data have shown potential benefit of deferiprone on cardiac iron removal, however most data came from uncontrolled case series and retrospective cross sectional analysis [39–41]. In an open-label, non-randomised Italian study, eighteen adult patients who received deferiprone for around 45 ± 21 months after a long period of deferoxamine treatment were matched for age and sex with another 18 adult patients who continued on deferoxamine. Overall heart T2* was measured once using a multislice multiecho T2* MRI [42]. The value was reported significantly higher in the deferiprone group versus deferoxamine group (35 ± 7 vs. 27 ± 2 ms; p = 0.02) and the number of segments with normal T2* (>20 ms) was significantly higher in the deferiprone group (11 ± 1 vs. 8 ± 5 with deferoxamine; p = 0.03). No significant differences were found in biventricular function parameters. However, there was no baseline value available for comparison between the two groups, which may lessen the strength of the study.
The adverse events that occurred in the randomised controlled trials with deferiprone included nausea, joint pain (arthralgia) to severe arthritis, stomach upsets and low white blood count [38]. The most serious complication associated with deferiprone was agranulocytosis which occurred in 1% of patients [43]. In one trial, the risk of experiencing an adverse event with deferiprone was twice that of the risk with deferoxamine (RR = 2.24) [38]. Concerns regarding the adverse events associated with deferiprone had resulted in delays in its acceptance and regulatory approval. Its use is limited to second-line therapy for the treatment of iron overload in thalassemia major [44].
In Asia, several groups reported their experiences with deferiprone in patients with thalassemia major. An Indian retrospective study on safety profile of deferiprone in 44 children aged younger than 6 years found that 4.5% of patients experienced neutropenia and none had agranulocytosis [45]. However, they, observed thrombocytopenia in 45.45% of the study population, which occurred 3 months to 1 year after deferiprone therapy. Interruption of treatment for 2–4 weeks led to reversal of symptoms in all but two patients [45]. In Taiwan, 17 patients who received deferiprone therapy continuously for a mean period of 3.3 years and underwent liver biopsy twice were studied for hepatic toxicity of deferiprone. The researchers found no progression of hepatic fibrosis or increased liver iron stores in most patients with deferiprone treatment [46]. Another Taiwanese study group conducted a prospective 3 year study comparing cardiac and hepatic efficacy and safety of chelating treatment with deferiprone and deferoxamine [47]. Among 24 patients studied, 11 were switched from deferoxamine to deferiprone due to unwillingness or intolerability while the remaining 13 patients stayed on deferoxamine. There were no differences between the two groups in efficacy of lowering serum ferritin, serum ALT and hepatic iron levels. There was a marginal benefit in reducing cardiac iron accumulation and increasing cardiac function in the deferiprone group. The study group hence recommended the use of deferiprone in patients who failed on deferoxamine treatment [47].
Combination treatment with deferoxamine and deferiprone has been studied mainly in β-thalassemia major patients with evidence of cardiac iron overload. In a randomized, placebo-controlled, double-blind study, 65 patients with cardiac T2* between 8 and 20 ms entered the study with continuation of deferoxamine and were randomized to receive additional oral placebo or deferiprone [48]. The results of the study demonstrated that in comparison to monotherapy with deferoxamine, combination treatment reduced myocardial iron and improved the ejection fraction and endothelial function in thalassemia major patients with mild-to-moderate cardiac iron loading. It was generally well-tolerated. However, gastrointestinal symptoms were more likely to be recurrent in the combination group compared with the deferoxamine group (19 vs. 3%; p = 0.05). There were 1 episode of agranulocytosis and 2 episodes of neutropenia in the combined group. All episodes resolved after interventions [48]. So far, deferiprone appears to be a practical oral chelator for Asia due to cost and acceptable efficacy. However, several adverse events associated with deferiprone including agranulocytosis (ANC < 500/mm3), neutropenia (ANC < 1,500/mm3) and arthropathy in which all of them can be severe, might have limited its use in routine clinical practice. In several Asian countries such as the Philippines, Maldives or Indonesia, the logistics of monitoring the recommended routine WBC weekly may not be feasible. In Thailand, although a locally-made deferiprone has been available since 2008, many clinicians remain reluctant to prescribe the drug due to its potential side effects and a national guideline on deferiprone therapy is underway.
3.3 Deferasirox: a new oral iron chelator
Deferasirox, a newer oral tridentate chelator, was approved by the US Food and Drug Administration in October 2005 for first-line use in adults and children (aged ≥2 years) with chronic iron overload due to blood transfusions [49, 50]. It was developed to overcome the obstacles associated with administration of intravenous deferoxamine [51]. Deferasirox has now been approved in most Asian countries such as Malaysia, Singapore, Taiwan, Thailand, etc.
3.3.1 Clinical pharmacology
Deferasirox mobilizes iron stores by selectively binding to the ferric form of iron (high affinity, 2:1 ratio), and promoting the excretion of iron, primarily in the feces (84% of the dose) [34, 52]. Preclinical data indicates that deferasirox was 4–5 fold more effective than deferoxamine in promoting the excretion of storage iron from parenchymal iron stores and 2 to 3 times more effective in promoting reticuloendothelial iron excretion [53].
Following once-daily oral dosing, maximum plasma concentration is reached within 1.5–4 h, and deferasirox has an absolute bioavailability of 70% compared with an intravenous dose [52]. In a phase II study of patients with β-thalassemia (n = 71), deferasirox accumulation occurred between single dosing and steady state but no additional accumulation occurred after repeated daily dosing [54].
Deferasirox has a long plasma half-life of 8–16 h; which means that circulating drug is continually available to scavenge non-transferrin bound LPI [33]. Deferasirox is therefore effective throughout the 24-h dosing period [55]. An evaluation of subgroup data (n = 13) from the ESCALATOR trial, conducted in Middle Eastern patients with β-thalassemia and iron overload despite previous treatment with monotherapy or combination therapy, confirmed that once-daily dosing with deferasirox ≥20 mg/kg/day provided sustained reduction in LPI levels, suggesting 24-h protection from LPI (0.98 vs. 0.12 μmol/L pre- vs. 2 h post-administration at baseline, p < 0.0006; pre-administration LPI reached the normal range at week 4 and sustained throughout the remainder of the study vs. baseline, p ≤ 0.02) [56].
Based on Summary of Product Characteristics, treatment with deferasirox should be initiated and maintained by physicians experienced in the treatment of chronic iron overload due to blood transfusions. The recommended initial dose of deferasirox is 20 mg/kg/day, and treatment should be initiated after the transfusion of approximately 20 units (about 100 ml/kg) of packed red blood cells or when serum ferritin is consistently >1,000 μg/L [57]. An initial daily dose may be modified (to either 10 mg/kg/day or 30 mg/kg/day) depending on the number of transfusions the individual patient is receiving and whether the patient’s therapeutic goal is to decrease or maintain body iron levels [36]. Serum ferritin should be monitored monthly and the deferasirox dose should be adjusted if necessary, every 3–6 months based on the trends in serum ferritin. Deferasirox dose adjustment should be made by 5–10 mg/kg/day and tailored to the individual patient’s response and needs. It is recommended that serum creatinine be assessed in duplicate before initiating therapy and monitored monthly thereafter [57]. In patients on high doses of deferasirox or those receiving low rates of transfusion, serum creatinine should be monitored closely [36]. It is also recommended that liver function tests be performed monthly, and auditory and ophthalmic tests be performed before the start of treatment and every 12 months thereafter. As a general precautionary measure in the management of pediatric patients with transfusional iron overload, body weight, height and sexual development should be monitored at regular intervals (every 12 months) [57].
3.3.2 Clinical experience
Clinical registration and development trials with deferasirox have involved the largest number of patients ever conducted for iron chelation therapy. To date more than 1,000 patients have been enrolled [36]. A phase II randomised, open-label clinical trial in adult patients (n = 71) with β-thalassemia and transfusional iron overload demonstrated that deferasirox at daily dose of 20 mg/kg showed similar efficacy to deferoxamine 40 mg/kg with regard to decreases in LIC [58]. Deferasirox was well tolerated at 10 and 20 mg/kg/day with no patient discontinuing treatment due to adverse events. In another phase II open-label, non-comparative trial in pediatric patients, deferasirox 10 mg/kg once daily also demonstrated good tolerability and efficacy in 39 patients aged 2 to <12 years, with transfusion-dependent β-thalassemia major [59]. It is important to note that in heavily transfused patients, particularly children, a higher dosage of 20–30 mg/kg/day seemed more efficient to reduce iron burden to a safe level and to maintain an acceptable iron balance.
Data from a comparative phase III registration study in regularly transfused patients with β-thalassemia aged 2 years or older (n = 586) confirmed the efficacy and safety of deferasirox (5–30 mg/kg, depending on LIC values) and its non-inferiority to deferoxamine (20 to ≥50 mg/kg, depending on LIC values) in patients with baseline liver iron concentrations (LIC) values of 7 mg Fe/g dw or higher. Both deferasirox daily doses of 20–30 mg/kg and deferoxamine doses of ≥35 mg/kg significantly and similarly reduced the LIC (Table 3) and serum ferritin levels in patients with baseline LIC of ≥7 mg Fe/g dw [60]. In the sub-analysis of the same pivotal study, the patient-reported satisfaction and convenience were significantly higher with the deferasirox therapy [61]. Among patients who had previously taken deferoxamine and were randomized to receive deferasirox during the study, 96.9% reported a preference for deferasirox over deferoxamine. The primary reasons given for preferring deferasirox were that it was more convenient to take (37.4%), did not involve the injection-site soreness associated with DFO (25.3%), was less disruptive to their day (22.8%), less disruptive to their sleep (6.2%), and less disruptive to their family (4.2%) [61].
Deferasirox has also demonstrated safety and efficacy on LIC when administered for 1 year in the ESCALATOR study in 252 patients with β-thalassemia who had high iron burden and previously unsuccessfully chelated with deferoxamine and/or deferiprone in the Middle East [62]. In the per-protocol population, deferasirox was associated with an overall success rate (defined as LIC (mg Fe/g dw) reduction ≥3 if baseline LIC ≥10 or final LIC of 1–7 if baseline LIC 2 to <10) of 57.7% (p = 0.007). Compliance with deferasirox remained high for the duration of the study (median 99.3%). The most common treatment-emergent adverse events were transient and mild/moderate vomiting (8.3%), nausea (7.1%) and skin rash (7.5%). Due to high baseline iron burden resulted from previous inadequate chelation, dose escalation to 25/30 mg/kg/day during the course of the study was required in 76.2% patients not achieving target reduction in iron burden. This highlighted the importance of timely dose adjustments to achieve therapeutic goals [62]. Among 247 patients who entered the extension phase of ESCALATOR study, 93% completed additional 1.7 years of treatment. Deferasirox dose increases were further performed in 56% of patients, with increases to >30 mg/kg/day in 112 patients. Mean reduction in LIC from baseline to the end of study (2.7 years) was 8.9 ± 11.7 and 7.9 ± 8.7 mg Fe/g dw in adult and pediatric patients (both p < 0.0001), who were heavily iron-overloaded and previously unsuccessfully chelated. More patients were able to achieve LIC <7 mg Fe/g dw with a longer course of deferasirox therapy. Despite dose increases to ≥30 mg/kg/day in many patients during the extension phase, the safety of deferasirox was maintained with a lower AE reporting rate than that in the core study phase (22 vs. 42%) [63].
Overall, the various clinical trials showed that deferasirox has a defined safety profile that is clinically manageable with regular monitoring in adult and pediatric patients. The most frequent adverse events reported over a median 3.5 years’ treatment with deferasirox include transient, mild-to-moderate gastrointestinal disturbances (5–10%) and skin rash (5.2%) [36]. An independent post-marketing analysis in Thailand revealed that a mild transient maculopapular rash, mainly occurring within 7–10 days after start of the drug, is the most common side effect observed in Asian population who received deferasirox which is with a higher incidence than Western studies (17.7%). Other safety parameters seemed to be similar to those of previous studies, however this preliminary finding needs further confirmation [64]. Mild, non-progressive increases in serum creatinine (generally within the upper limit of normal) were observed in approximately one-third of patients in the pivotal studies of deferasirox. The levels returned spontaneously to baseline in more than two-thirds of these patients. No cases of moderate-to-severe renal insufficiency or renal failure were reported, and no patients permanently discontinued therapy due to creatinine rises, based on data collected from up to 3.5 years of treatment in 1,034 patients in the pivotal trials [36]. Deferasirox treatment had also shown no negative impact on growth measured by height and sexual development in pediatric patients followed in extension studies up to 5 years [65, 66].
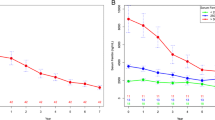
Most recently, the largest Evaluating Patients’ Iron Chelation (EPIC) multi-center, 12-months trial was initiated to evaluate whether fixed starting doses of deferasirox (based on iron intake from ongoing blood transfusions) with subsequent dose titration (up to 40 mg/kg/day) every 3 months based on serum ferritin trends and safety markers can provide clinically acceptable chelation. The results were recently presented in the 50th ASH meeting in December 2008. The study confirmed that with fixed starting dose based on transfusional iron intake and subsequent dose titration, deferasirox is effective in reducing iron burden measured by serum ferritin in iron-overloaded, regularly-transfused patients with a wide range of underlying anemias including thalassemia. In fact, among 1,744 adult and pediatric patients enrolled from 21 countries (including China, Hong Kong, Malaysia, Taiwan, South Korea and Thailand in Asia), 937 patients were with β-thalassemia major heavily transfused and pre-treated with other iron chelation therapies. In those patients, after 1 year treatment of deferasirox at an average actual dose of 24.2 ± 5.6 mg/kg/day, median serum ferritin level decreased by 129 ng/mL (P = 0.0007 vs. baseline) [52]. The safety profile and discontinuation rates were consistent with previously reported data in thalassemia patients [52]. Two sub-studies of the EPIC trial prospectively evaluated for the first time in a multicenter setting the efficacy of deferasirox in reducing cardiac iron in β-thalassemia patients with myocardial siderosis (n = 114) and in preventing cardiac iron accumulation in those with normal cardiac iron level at baseline (n = 78). After 1-year treatment of deferasirox at mean dose of 32.6 mg/kg/day, the myocardial T2* improved significantly (P < 0.0001) from baseline (geometric mean at 11.2 ms) to 12.9 ms in patients with myocardial siderosis, whose cardiac function measured by left ventricular ejection fraction (LVEF) also remained stable throughout the study [67]. In patients with normal cardiac iron level at baseline (32.0 ms), the cardiac T2* remained stable at 32.5 ms (P = ns vs. baseline) after 1-year treatment of deferasirox at mean dose of 27.6 mg/kg/day, with LVEF increased significantly from 67.7 to 69.6% (P < 0.0001) [68]. Both data showed that deferasirox at optimal doses, removed cardiac iron and potentially prevents long-term iron accumulation in the heart.
4 Current guidelines for the treatment of iron overload
The principles of treatment for thalassemia are now fairly well established. However, there are still some areas which are subject to continuing modification; these include adequate transfusion and chelation therapy, prevention and management of complications, and monitoring for new unexpected complications. Early detection of other unrelated chronic illness, especially in an ageing population of thalassemia patients, is also an important issue.
The primary goal of treatment in patients with iron overload is to achieve safe iron levels. The recent TIF guideline [20] recommends screening for iron overload at the onset of transfusions. Serum ferritin is a well established prognostic test which should be performed every 3 months, preferably in conjunction with other measures. Liver iron concentration is the reference standard for estimating iron loading and can be determined via liver biopsy or non-invasive MRI/biomagnetic susceptometry. Newer technique like T2* imaging of the cardiac tissue is increasingly being used to assess the cardiac function of patients around the world.
Treatment for iron overload should be initiated when serum ferritin levels reach approximately 1,000 μg/L or after the first 10–20 transfusions. The TIF recommends that initiation of chelation therapy should be accompanied by regular monitoring for efficacy, side effects and complications of excessive chelation, particularly with regard to auditory and ocular toxicities in cases with deferoxamine [20]. In thalassemia patients who receive deferasirox, the TIF recommends starting dose at 20 mg/kg/day (iron intake 0.3–0.5 mg/kg/day) but the dosage could be increased up to 30 mg/kg/day in patients who already have pre-existing iron overload (iron intake > 0.5 mg/kg/day). Regular monitoring of renal function is required and Deferasirox is contraindicated in patients with renal failure or significant renal dysfunction [20]. The TIF states that the majority of experience with deferiprone is with 75 mg/kg/day in 3 divided doses (up to 100 mg/kg/day with limited information), although following long-term therapy at this dose only a proportion of patients achieve the desired liver iron levels [20]. Careful monitoring of the patient’s clinical condition and laboratory testing is essential given the possibility of serious adverse effects including agranulocytosis and neutropenia. Until there are more data on the safety of deferiprone, weekly blood counts are advised, as are liver biopsies before and during therapy. At present, there is limited data on the efficacy of this agent in patients aged <10 years [20].
Within Asia, there are regional variations in thalassemia management protocols and guidelines, although most recommendations are in line with those of the TIF. In Taiwan, transfusion therapy is usually given every 2–4 weeks with the aim of maintaining pre-transfusion hemoglobin levels above 10 g/dL. Deferoxamine is administered in accordance with the TIF guidelines, and oral deferiprone three times daily and oral deferasirox once daily are also available. The treatment of thalassemia in Malaysia is largely the domain of individual clinicians although clinical practice guidelines have been available since 1998, and these were updated in 2005. In these guidelines, deferoxamine is recommended as the standard treatment and should be administered as per the TIF recommendations. Deferiprone is recommended in patients with ferritin levels >2,500 μg/L, when there is no response to deferoxamine or there are deferoxamine-related adverse effects. With the introduction of deferasirox, updated guidelines are in preparation, although the specific role of this chelator remains to be determined. In Thailand, all three chelating agents are available: deferoxamine (20–60 mg/kg/day given as subcutaneous infusion over 8–12 h, 5–6 times per week); deferiprone (50–100 mg/kg/day), and deferasirox (20–30 mg/kg/day). While in Singapore, the incidence of thalassemia intermedia is very low, the decision to transfuse is often more problematic in these patients. Iron chelation therapy is offered to all patients with β-thalassemia major and usually commence at the age of 3 years or when serum ferritin is >2,000 ng/mL. Deferoxamine, deferiprone and deferasirox are all available, although the latter has only been used recently.
5 Discussion
Despite recommendations from the TIF, adequate management of thalassemia still presents a major challenge, and difficulties arise with regards to the optimal time to commence chelation therapy, the determination of a safe ferritin level, and the accurate assessment of body iron. Furthermore, evidence from Hong Kong indicates that despite the use of iron chelation therapy with deferoxamine, severe complications still occur. In a cohort of 232 patients, the probability of survival beyond age 20 years was only 86.7%; cardiomyopathy was the leading cause of death in these patients [69].
It is anticipated that the development of new oral iron chelators, such as deferasirox, will have a major impact on the treatment of patients with thalassemia. The availability of three agents for the treatment of thalassemia will enable physicians to tailor treatment regimens to the individual patient, leading to improved life expectancy and quality of life.
In view of the increasing availability and use of deferiprone and deferasirox in the management of iron overload, there is a need for clearly defined management protocols that can be easily implemented within Asia. The development of such protocols for chelation therapy will be integral in ensuring that patients receive timely and effective treatment while minimizing adverse effects and potentially improving their compliance to treatment regimen. A clear definition of therapeutic goals and monitoring strategies will minimize the time required to find the optimal dose for each patient. Ideally, chelation therapy should be tailored to each patient, based on their baseline condition, with monitoring and dose adjustments, to achieve and maintain optimal chelation. Appropriate patient selection may further improve the effectiveness of chelation therapy.
6 Conclusion
Transfusion-dependent thalassemia represents a major healthcare burden in Asia and the development of oral iron chelators such as deferasirox represents a significant advance in iron chelation therapy. The development and implementation of consensus guidelines for management of Asian patients with transfusion-dependent thalassemia will be a major step towards improving and maintaining the continuity of patient care. However, due to a significant difference of socio-economic and medical standards among Asian countries which differ vastly from that of European or North-American standards, it is important that experts from Asian countries discuss and identify the best possible recommendations for iron chelation therapy and draw a consensus that could be used as clinical practice guidelines for optimal and appropriate management for thalassemia. There is no doubt that such a recommendation will play an important role in improving clinical management of thalassemia in Asia where many lives are affected.
References
Weatherall DJ, Clegg JB. Inherited haemoglobin disorders: an increasing global health problem. Bull World Health Organ. 2001;79:704–12.
Weatherall DJ, Clegg JB, editors. The Thalassaemia Syndromes. 4th ed. Oxford: Blackwell Science; 2001.
Higgs D. Molecular mechanisms of α thalassemia. In: Steinberg M, Forget B, Higgs D, Nagel R, editors. Disorders of hemoglobin. Cambridge: Cambridge University Press; 2001. p. 405–30.
Forget BG. Molecular mechanisms of β thalassemia. In: Steinberg MH, Forget BG, Higgs DR, Nagel RL, editors. Disorders of hemoglobin. Cambridge: Cambridge University Press; 2001. p. 252–76.
Viprakasit V, Kidd AM, Ayyub H, Horsley S, Hughes J, Higgs DR. De novo deletion within the telomeric region flanking the human alpha globin locus as a cause of alpha thalassaemia. Br J Haematol. 2003;120:867–75.
Higgs D. Clinical and laboratory features of the thalassemia syndrome. In: Bowden D, Steinberg M, Forget B, Higgs D, Nagel R, editors. Disorders of hemoglobin. Cambridge: Cambridge University Press; 2001. p. 431–69.
Cohen AR, Galanello R, Pennell DJ, Cunningham MJ, Vichinsky E. Thalassemia. Hematology Am Soc Hematol Educ Program. 2004. p. 14–34.
Tanphaichitr VS. Current situation of thalassemia in Thailand. The 7th International Conference on Thalassemia and Hemoglobinopathies. Bangkok: Ministry of Public Health, Thailand; 1999. p. 78–9.
Fucharoen S, Winichagoon P. Hemoglobinopathies in Southeast Asia: molecular biology and clinical medicine. Hemoglobin. 1997;21:299–319.
Fucharoen S, Winichagoon P. Clinical and hematologic aspects of hemoglobin E beta-thalassemia. Curr Opin Hematol. 2000;7:106–12.
George E. Beta-thalassemia major in Malaysia, an ongoing public health problem. Med J Malays. 2001;56:397–400.
Chern JP, Lin KH, Su YN, et al. Impact of a national beta-thalassemia carrier screening program on the birth rate of thalassemia major. Pediatr Blood Cancer. 2006;46:72–6.
Ng IS, Ong JB, Tan CL, Law HY. Early prenatal diagnosis of beta-thalassaemia in Singapore. Ann Acad Med Singapore. 1996;25:779–82.
Chan V, Chan TK, Tang M, Ghosh A. Prenatal diagnosis and screening of common genetic diseases in Hong Kong. Southeast Asian J Trop Med Public Health. 1995;26(Suppl 1):1–2.
Lee AC, Ha SY, Wong KW, et al. Prevention of beta-thalassemia major by antenatal screening in Hong Kong. Pediatr Hematol Oncol. 1998;15:249–54.
Cappellini MD, Cohen A, Eleftheriou A, Piga A, Porter J. Blood transfusion, chapter 3. Guidelines for the clinical management of thalassemia: Thalassemia International Federation; 2000. p. 9–10. http://www.thalassaemia.org.cy/publications.html.
Cappellini MD, Cohen A, Eleftheriou A, Piga A, Porter J. Iron overload, chapter 5. Guidelines for the clinical management of thalassemia: Thalassemia International Federation; 2000. p. 21–35. http://www.thalassaemia.org.cy/publications.html.
Marengo-Rowe AJ. The thalassemias and related disorders. Proc (Bayl Univ Med Cent). 2007;20:27–31.
Porter JB. Monitoring and treatment of iron overload: state of the art and new approaches. Semin Hematol. 2005;42:S14–8.
Cappellini MD, Cohen A, Eleftheriou A, Piga A, Porter J, Taher A. Iron overload, chapter 3. Guidelines for the clinical management of thalassemia: Thalassemia International Federation. Nicosia, Cyprus; 2007. p. 31–63. http://www.thalassaemia.org.cy/publications.html.
Morris CR, Singer ST, Walters MC. Clinical hemoglobinopathies: iron, lungs and new blood. Curr Opin Hematol. 2006;13:407–18.
Olivieri NF, Brittenham GM. Iron-chelating therapy and the treatment of thalassemia. Blood. 1997;89:739–61.
Cabantchik ZI, Breuer W, Zanninelli G, Cianciulli P. LPI-labile plasma iron in iron overload. Best Pract Res Clin Haematol. 2005;18:277–87.
Borgna-Pignatti C. Surviving with thalassemia major: the Italian experience. Pediatr Hematol Oncol. 2007;24:75–8.
Wood JC, Enriquez C, Ghugre N, et al. MRI R2 and R2* mapping accurately estimates hepatic iron concentration in transfusion-dependent thalassemia and sickle cell disease patients. Blood. 2005;106:1460–5.
Mazza P, Giua R, De Marco S, et al. Iron overload in thalassemia: comparative analysis of magnetic resonance imaging, serum ferritin and iron content of the liver. Haematologica. 1995;80:398–404.
Viprakasit V, Tanphaichitr VS, Mahasandana C, et al. Linear growth in homozygous beta-thalassemia and beta-thalassemia/hemoglobin E patients under different treatment regimens. J Med Assoc Thai. 2001;84:929–41.
Taher A, El Rassi F, Isma’eel H, Koussa S, Inati A, Cappellini MD. Correlation of liver iron concentration determined by R2 magnetic resonance imaging with serum ferritin in patients with thalassemia intermedia. Haematologica. 2008;93:1584–6.
Origa R, Galanello R, Ganz T, et al. Liver iron concentrations and urinary hepcidin in beta-thalassemia. Haematologica. 2007;92:583–8.
Pakbaz Z, Fischer R, Fung E, Nielsen P, Harmatz P, Vichinsky E. Serum ferritin underestimates liver iron concentration in transfusion independent thalassemia patients as compared to regularly transfused thalassemia and sickle cell patients. Pediatr Blood Cancer. 2007;49:329–32.
Coa A, Gabutti V, Galanello R, Masera G, Modell B, Plama A. Management protocol for the treatment of thalassemia patients (ed 1997). Nicisia: Thalassemia Internation Federation; 1997.
Cohen AR. New advances in iron chelation therapy. Hematology Am Soc Hematol Educ Program. 2006. p. 42–7.
Neufeld EJ. Oral chelators deferasirox and deferiprone for transfusional iron overload in thalassemia major: new data, new questions. Blood. 2006;107:3436–41.
Stumpf JL. Deferasirox. Am J Health Syst Pharm. 2007;64:606–16.
Kusuwan T, Pangnukroh L, Leekamnerdthai W, Sangpraypan T, Viprakasit V. Analysis of treatment complicance and related health and social determining factors in thai thalassemia patients under long-term deferrioxamine administration. Siriraj Nursing J. 2008;2(1):2–14.
Cappellini MD, Taher A. Long-term experience with deferasirox (ICL670), a once-daily oral iron chelator, in the treatment of transfusional iron overload. Expert Opin Pharmacother. 2008;9:2391–402.
Ferriprox® (deferiprone). Eurpean summary of product characteristics. Apotex Europe Ltd., UK.
Roberts DJ, Brunskill SJ, Doree C, Williams S, Howard J, Hyde CJ. Oral deferiprone for iron chelation in people with thalassaemia. Cochrane Database of Systematic Reviews 2007, Issue 3. Art. No.: CD004839. doi:10.1002/14651858.CD004839.pub2.
Taher A, Sheikh-Taha M, Koussa S, Inati A, Neeman R, Mourad F. Comparison between deferoxamine and deferiprone (L1) in iron-loaded thalassemia patients. Eur J Haematol. 2001;67(1):30–4.
Piga A, Gaglioti C, Fogliacco E, Tricta F. Comparative effects of deferiprone and deferoxamine on survival and cardiac disease in patients with thalassemia major: a retrospective analysis. Haematologica. 2003;88(5):481–2.
Borgna-Pignatti C, Cappellini MD, De Stefano P, Del Vecchio GC, Forni GL, Gamberini MR, et al. Cardiac morbidity and mortality in deferoxamine- or deferiprone-treated patients with thalassemia major. Blood. 2006;107(9):3733–7.
Pepe A, Lombardi M, Positano V, et al. Evaluation of the efficacy of oral deferiprone in β-thalassemia major by multislice multiecho T2*. Eur J Haematol. 2006;76:183–92.
Beutler E, Hoffbrand AV, Cook JD. Iron deficiency and overload. Hematology Am Soc Hematol Educ Program. 2003. p. 40–61.
Cario H, Janka-Schaub G, Janssen G, Jarisch A, Strauss G, Kohne E. Recent developments in iron chelation therapy. Klin Padiatr. 2007;219:158–65.
Naithani R, Chandra J. Sharma S Safety of oral iron chlator deferiprone in young thalassaemics. Eur J Haematol. 2005;75:217–20.
Wu SF, Peng CT, Wu KH, Tsai CH. Liver fibrosis and iron levels during long-term deferiprone treatment of thalassemia major patients. Hemoglobin. 2006;30(2):215–8.
Peng CT, Chow KC, Chen JH, Chiang YP, Lin TY. Tsai CH Safety monitoring of cardiac and hepatic systems in β-thalassemia patients with chelating treatment in Taiwan. Eur J Haematol. 2003;70:392–7.
Tanner MA, Galanello R, Dessi C, et al. A randomized, placebo-controlled, double-blind trial of the effect of combined therapy with deferoxamine and deferiprone on myocardial iron in thalassemia major using cardiovascular magnetic resonance. Circulation. 2007;115:1876–84.
Exjade® (deferasirox) Prescribing Information. Novartis Pharmaceuticals Corporation, East Hanover, New Jersey 07936, USA. December 2007.
Agarwal MB. Exjade (ICL 670): a new oral iron chelator. J Assoc Physicians India. 2006;54:214–7.
Hershko C, Konijn AM, Nick HP, Breuer W, Cabantchik ZI, Link G. ICL670A: a new synthetic oral chelator: evaluation in hypertransfused rats with selective radioiron probes of hepatocellular and reticuloendothelial iron stores and in iron-loaded rat heart cells in culture. Blood. 2001;97:1115–22.
Cappellini MD, Elalfy MS, Kattamis A, et al. Efficacy and safety of once-daily, oral iron chelator deferasirox (Exjade®) in a large group of regularly transfused patients with β-thalassemia major. Blood 2008;112(11), abstract #3878.
Hershko CM, Link GM, Konijn AM, Cabantchik ZI. Iron chelation therapy. Curr Hematol Rep. 2005;4:110–6.
Nisbet-Brown E, Olivieri NF, Giardina PJ, et al. Effectiveness and safety of ICL670 in iron-loaded patients with thalassaemia: a randomised, double-blind, placebo-controlled, dose-escalation trial. Lancet. 2003;361:1597–602.
Hershko C, Link G, Konijn AM, Cabantchik ZI. Objectives and mechanism of iron chelation therapy. Ann N Y Acad Sci. 2005;1054:124–35.
Daar S, Pathare A, Nick H, Kriemler-Krahn U, Hmissi A, Habr D, et al. Reduction in labile plasma iron during treatment with deferasirox, a once-daily oral iron chelator, in heavily iron-overloaded patients with b-thalassaemia. Eur J Haematol. 2009;82(6):454–7.
Exjade® (deferasirox). Eurpean summary of product characteristics. Novartis Europharma Ltd, UK.
Piga A, Galanello R, Forni GL, et al. Randomized phase II trial of deferasirox (Exjade, ICL670), a once-daily, orally-administered iron chelator, in comparison to deferoxamine in thalassemia patients with transfusional iron overload. Haematologica. 2006;91:873–80.
Galanello R, Piga A, Forni GL, et al. Phase II clinical evaluation of deferasirox, a once-daily oral chelating agent, in pediatric patients with beta-thalassemia major. Haematologica. 2006;91:1343–51.
Cappellini MD, Cohen A, Piga A, et al. A phase 3 study of deferasirox (ICL670), a once-daily oral iron chelator, in patients with beta-thalassemia. Blood. 2006;107:3455–62.
Cappellini MD, Bejaoui M, Agaoglu L, et al. Prospective evaluation of patient-reported outcomes during treatment with deferasirox or deferoxamine for iron overload in patients with [3-Thalassemia. Clin Therap. 2007;29:909–17.
Taher A, El-Beshlawy A, Al-Jefri A, Elalfy M, Al-Zir K, Daar S Treatment with the once daily, oral iron chelator, deferasirox (Exjade, ICL670) is effective and well tolerated in b-thalassemia patients with a high iron burden. Presented at the 12th Congress of the European Haematology Association. Vienna, Austria; 2007. Abstract 808.
Taher A, El-Beshlawy A, Elalfy MS, et al. Efficacy and safety of once-daily oral Deferasirox (Exjade®) during a median of 2.7 years of treatment in heavily iron-overloaded patients with β-Thalassemia. Blood 2008;112(11), abstract #5409.
Sripornsawan P, Tachavanich K, Viprakasit V. Clinical evaluation on adverse events due to deferasirox; a novel oral iron chelator, in 79 pediatric patients with β-thalassemia. Proceeding of the 11th International Conference on Thalassemia and the Hemoglobinopathies. Suntec International Convention, Singapore; 2008:abs-P51.
Piga A, Kebaili K, Galanello R et al. Cumulative efficacy and safety of 5-year Deferasirox (Exjade®). Treatment in pediatric patients with Thalassemia major: a phase II multicenter prospective trial. Blood 2008;112(11), abstract #5413.
Piga A, Forni GL, Kattamis A, et al. Deferasirox (Exjade®) in pediatric patients with β-Thalassemia: update of 4.7-year efficacy and safety from extension studies. Blood 2008;112(11), abstract #3883.
Pennell D, Porter JB, Cappellini MD, et al. Efficacy and safety of deferasirox (Exjade®) in reducing cardiac iron in patients with β-thalassemia major: results from the cardiac substudy of the EPIC trial. Blood 2008;112(11), abstract #3873.
Pennell D, Sutcharitchan P, El-Beshlawy A, et al. Deferasirox (Exjade®) in preventing cardiac iron overload in β-thalassemia patients with normal baseline cardiac iron: results from the cardiac substudy of the EPIC Trial. Blood 2008;112(11), abstract #3874.
Li CK, Luk CW, Ling SC, et al. Morbidity and mortality patterns of thalassaemia major patients in Hong Kong: retrospective study. Hong Kong Med J. 2002;8:255–60.
Lin KH, Lin LI, Syi S, Lin KS. The incidence of β-thalassemia trait in Taiwan. Int J of Pediatr Hematol Oncol. 1994;1:383–8.
Otto-Duessel M, Aguilar M, Nick H, Moats R, Wood JC. Comparison of twice-daily vs once-daily deferasirox dosing in a gerbil model of iron cardiomyopathy. Exp Hematol. 2007;35:1069–73.
Wood JC, Otto-Duessel M, Gonzalez I, et al. Deferasirox and deferiprone remove cardiac iron in the iron-overloaded gerbil. Transl Res. 2006;148:272–80.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Viprakasit, V., Lee-Lee, C., Chong, Q.T. et al. Iron chelation therapy in the management of thalassemia: the Asian perspectives. Int J Hematol 90, 435–445 (2009). https://doi.org/10.1007/s12185-009-0432-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12185-009-0432-0