Abstract
Objectives
To assess the efficacy and safety of dual oral iron chelation therapy (deferiprone and deferasirox) in decreasing iron overload status, using serum ferritin and liver and cardiac MRI as indicators, in transfusion dependent thalassemic children.
Methods
This was a prospective observational study conducted in a tertiary care hospital for a period of one year. Children with thalassemia between 2 and 18 y of age with serum ferritin above 1500 ng/ml were started on oral deferiprone and deferasirox. They were followed up for one year. Serum ferritin and MRI quantification of liver and cardiac iron concentration was done at enrolment and end of 12 mo. They were also monitored monthly for any adverse effects.
Results
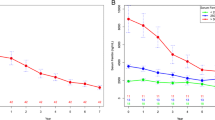
Twenty one thalassemic children with mean age of 7.8 y (range 4–12 y) and a mean ferritin value of 3129 + 1231.5 ng/ml were enrolled. Mean serum ferritin decreased by 1226.3 ng/ml (p = 0.047, 95% CI =10.2, 1504.3) with 16.8% fall from baseline. The reduction in ferritin correlated significantly with the initial ferritin level (spearman’s rho = 0.742, p = 0.001). Mean liver iron concentration and myocardial iron concentration did not change significantly. Red color urine, transient rise in creatinine and liver enzymes were noted during the study period.
Conclusions
Combined oral chelation with deferiprone and deferasirox significantly decreases the serum ferritin level in children with severe iron overload. The drugs were tolerated well without any serious adverse effects.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Adequate chelation therapy is the cornerstone of managing iron related complications and thereby improving quality of life and mortality in children with thalassemia. Deferoxamine is the first efficient iron chelator studied in thalassemia patients. But, it has to be administered parenterally. The other two main chelators are deferasirox and deferiprone; both are oral iron chelators. In patients whose iron overload is not controlled with monotherapy, combination chelation therapy with deferoxamine and deferiprone was found to be effective and safe. However, it is difficult to continue deferoxamine for long term due to prolonged parenteral infusion periods. Hence, combination chelation therapy with the two oral iron chelators- deferiprone and deferasirox is emerging as a new treatment for severe iron overload. Studies have shown that this combined oral chelation reduces serum ferritin and is also more efficacious than either of the drugs used alone [1]. Still, the data available is very limited and we need further evidence regarding efficacy and safety of this novel combination therapy. Hence, this study was planned in authors’ centre to assess the efficacy and safety of dual oral iron chelation therapy in decreasing iron overload status, using serum ferritin and liver and cardiac MRI as indicators, in transfusion dependent thalassemic children.
Material and Methods
This study was conducted in the Department of Pediatrics, JIPMER from July 2017 to July 2019 in collaboration with the Department of Radiodiagnosis. Study was approved by Institute Ethics Committee (JIP/IEC/2017/0292) and was registered in clinical trials registry of India (CTRI/2018/02/012134). Sample size was calculated using the Openepi online tool with expected change in ferritin of 36%, change in liver iron concentration of 18.7% and change in cardiac iron concentration of 19% after one year, derived from available literature [2], with power of 80% and alpha error at 5% and attrition of 20%. The expected sample size for change in ferritin, liver iron concentration (LIC) and myocardial iron concentration (MIC) were 14, 18 and 11 respectively.
Children with thalassemia of age 2–18 y and serum ferritin ≥1500 ng/ml who reported to the pediatric hematology clinic for regular follow up were enrolled consecutively. Children with serum creatinine more than two times the upper limit for age, serum aspartate amino transferase and alanine amino transferase more than five times the upper limit for age, absolute neutrophil count (ANC) less than 1500/mm3, platelets less than 1 lakh/mm3, significant proteinuria defined by protein creatinine ratio more than 0.5, cardiac failure secondary to myocardial iron toxicity and previous history of allergic reaction to deferiprone or deferasirox were excluded.
As baseline workup, anthropometry, serum ferritin, urea, creatinine, aspartate amino transferase (AST), alanine amino transferase (ALT), absolute neutrophil count, platelet count, screening for human immunodeficiency virus (HIV), hepatitis B and C viruses, echo, visual (visual acuity and fundus examination) and auditory (audiometry) evaluation was done for all children who were enrolled. All children were encouraged to maintain pre-transfusion hemoglobin of 9.0 g/dl by transfusing at regular intervals of 3–4 wk. The children under study who were on monotherapy were started on the other drug, oral deferiprone at 75 mg/kg/d in three divided doses or deferasirox at 30 mg/kg/d. Children who were already on dual therapy were advised to continue drugs. It was planned to increase deferasirox to 40 mg/kg/d if serum ferritin levels remained above 2500 ng/ml after three months of dual chelation; further to increase deferiprone to 100 mg/kg/d if serum ferritin was persistently high in next three months. If serum ferritin falls <1000 ng/ml, deferiprone was planned to be stopped. Patients were clearly counselled about the importance of taking the drugs adequately and advised to maintain drug diary. Compliance was assessed monthly by verifying the drug diary and also by counting the remaining pills. Any child defaulted for more than a week in one month was considered as poor compliance.
Every month they were reassessed clinically for gastrointestinal symptoms (nausea, vomiting, abdominal distension, hematemesis and melena), joint pain or swelling, reddish/brown colored urine and skin rash. Monthly monitoring of urea, creatinine, AST, ALT, absolute neutrophil count, platelet count and urine protein creatinine ratio were done. At the end of 12 mo all baseline workup was repeated, change in serum ferritin levels, cardiac and liver iron concentration levels were assessed and annual blood transfusion rate and iron overload rate were calculated. In case of rise in liver transaminases over five times the upper limit for age or rise in creatinine levels more than 33% from baseline, deferasirox was planned to be withheld till these parameters normalise. Deferiprone was planned to be discontinued if ANC falls less than 1500/mm3 or in case of arthropathy not responding to NSAIDS.
MRI study was done in SIEMENS AVANTO 1.5 Tesla machine. Estimation of LIC and MIC was performed using T2* multi-echo sequence. It was performed using a single thick slice T2* sequence through the centre of the liver in axial plane and a similar sequence through the mid short axis of heart, scanned at 8 different echo times. T2* image analysis was performed using T2* analysis spread sheet downloaded from ironcalculator.com. It provided calculated iron concentrations based on previous published data and their correlation in ms/Hz to direct iron measurements by biopsies [3, 4].
All data were analysed using SPSS software version 23.0. Normality of data was tested by using the Shapiro-Wilk test for normality. Categorical variables were expressed as frequencies with percentages. Continuous, normal data was expressed as mean ± SD and continuous, non-normal data as median with inter quartile range. Comparison of continuous data at the beginning and end of study was done by paired student’s t test and Wilcoxon signed rank test for normal and non-normal data respectively. Correlation of continuous non-parametric data was done by calculating spearman’s rho.
Results
Twenty three children with transfusion dependent thalassemia fulfilling the inclusion criteria were assessed for eligibility and enrolled. One child underwent bone marrow transplantation from a private centre and continued follow-up there. One child had unexplained sudden death at home. Hence, the remaining twenty one children were followed up for a period of one year.
The mean age of children enrolled was 7.8 (+ 2.5) y. There were 14 (67%) males and 7 (33%) females. Nine (43%) children were stunted and 11 (52%) were underweight. All patients tested negative for HIV, hepatitis B and C viruses. Two of the children had undergone splenectomy prior and one child underwent splenectomy during the study period. The mean pre-transfusion hemoglobin during the study period was 7.4 + 0.8 mg/dl. Mean annual blood transfusion rate was 193 + 17 ml/kg. At enrolment, there were two groups of patients. Group A had 10 (48%) children taking deferasirox alone and group B had 11 (52%) children on both deferiprone and deferasirox therapy. None of the children were on deferiprone monotherapy. The mean duration of prior chelation therapy in the children was 46 mo; Group A received for 37 mo whereas group B received for 10 mo. The mean ferritin level in group A was 2473 ng/ml which reduced to 2196 ng/ml after one year whereas in group B it was 3480 ng/ml at baseline which decreased to 2532 ng/ml. At recruitment, 10 children (5 each in group A and B) received deferasirox at 40 mg/kg, and 8 (group B) received deferiprone at 100 mg/kg. During the study period, deferasirox dose was increased in 6 children at 3 mo (2 in group A and 4 in group B) and deferiprone was increased in 5 children (3 children at 3 mo and for 2 children at 6 mo only in group A). On the other hand, deferiprone dose was decreased in only one child in group B whereas defarasirox was not reduced in anyone.
The severity and change in iron overload markers are given in Tables 1 and 2. Serum ferritin at the end was higher than baseline for six children, in which four patients had poor compliance to drugs. When there was no supply of chelation drugs from authors’ hospital, these parents could not able to procure drugs regularly due to economic constraints. They defaulted for three to four months. Other two children were taking the drugs regularly according to their mothers. One child had increase in serum ferritin of 223 ng/ml and other child had an increase of 205 ng/ml, and their annual transfusion volume was 215 ml/kg and 190 ml/kg respectively. Analysis of the 17 children who were compliant to therapy revealed a better reduction in serum ferritin.
The reduction in ferritin was found to correlate significantly with the initial ferritin level (spearman’s rho = 0.742, p = 0.001). No significant correlation was observed between total transfusion volume and pre-transfusion hemoglobin with change in serum ferritin.
Cardiac and liver iron quantification was done for nine children who were cooperative for the MRI study. Both cardiac and liver iron levels showed a falling trend, but the changes were not found to be statistically significant. No significant correlation was noted on comparing the change in ferritin with either liver or heart iron concentration.
The most common symptom noted in the study population was passing red colored urine (86%). Other side effects observed are shown in Table 3. Thrombocytosis, indicated by platelet counts above 4.5 lakhs/mm3 was seen in three children, who had undergone splenectomy.
Two children had ophthalmic abnormalities on screening. One child had superficial punctate keratitis and one child had bilateral zonular cataract. Child with zonular cataract underwent bilateral cataract surgery on follow-up. Cataracts were reported to be associated with deferiprone and deferoxamine use. However, this child was taking only deferasirox, and was never on deferiprone or deferoxamine prior to the study. It is possible that the cataract was due to free radical damage due to iron toxicity. Child with superficial punctate keratitis normalised on follow-up.
Hearing assessment and myocardial function assessed by echocardiography were normal at enrolment and at the end of study for all children. One child developed osteomyelitis of left tibia and another child had acute watery diarrhea requiring hospitalisation during the study period. All 6 (29%) patients had only mild thrombocytopenia (1–1.5 lakhs/mm3), which recovered spontaneously. None developed any serious complication requiring the stoppage of chelation drugs.
Discussion
Tissue iron overload results in significant mortality and morbidity in children with thalassemia. Dual oral iron chelation will not only reduce the iron overload but also improve compliance. Previous studies on dual chelation have been done mainly on adolescent or adult population [1, 2, 5,6,7,8] whereas the present study population is predominantly dominated by younger children with mean age of 7.8 y (range of 4–12 y).
Ferritin decreased by a mean value of 1226.3 ng/ml from the baseline ferritin of 3129 ng/ml. Previous researchers have shown the mean change in ferritin to be ranging from 1070 to 3275 ng/ml [1, 5, 6, 9]. The authors observed a strong correlation between the initial ferritin level and the change in ferritin. There was a mean percentage change in ferritin of 31.4% in patients who were compliant. Elalfy et al. and Parakh et al. have reported percentage changes of 36.59% and 34.99% respectively [2, 6].
Combination of deferiprone and deferoxamine is proven to be effective in reversing cardiac iron overload by ‘iron shuttle’ mechanism [10]. Cardiac iron loading occurs mainly from non transferrin bound iron pool and hence its control depends on duration of exposure to chelation [11]. Combination of deferiprone and deferasirox reduced the cardiac iron overload significantly higher than deferiprone and deferoxamine combination in adolescent population in Egypt [2]. MRI based cardiac iron assessment done in five children on dual iron chelation therapy in north India showed that there was no significant change at the end of one year and the change was comparable to monotherapy with deferiprone or deferasirox [1]. In the present study authors observed that mean cardiac iron concentration determined by T2* did not have any significant change after one year of chelation. But seven out of nine children in present study did not have cardiac iron overload at beginning. This relates to the fact that cardiac iron overload is usually delayed and tissue iron overload increases with age [12]. One child had severe cardiac iron overload which decreased to moderate range and another child had light iron overload that decreased to no iron overload. This observation shows that the combination may be effective in reversing myocardial iron load and studies on patients with significant cardiac iron load may reveal this effect well. However, one child with no cardiac iron overload developed light iron overload while on regular chelation. Also, the children with myocardial iron overload in present study did not have any clinical or echocardiographic features of myocardial dysfunction. This reconfirms that myocardial iron toxicity may be clinically silent and routine MRI quantification can help in identifying the children at risk earlier [13].
Hepatic iron loading occurs mainly by transferrin mediated uptake and hence its control is more dependent on dose of chelation received. The authors observed a mean fall in LIC by 23%, which was not found to be statistically significant, probably due to inadequate sample size. Serum ferritin has been found to correlate with hepatic iron concentration in an observational study done on sixty thalassemic patients, whereas cardiac iron concentration did not correlate with both ferritin and hepatic iron concentration [14]. The present study showed no correlation between serum ferritin and hepatic and cardiac iron concentration.
Arthropathy and gastrointestinal symptoms were the predominant symptoms noted in previous studies and were reported to be in the range of 12.5% to 22.2% in different studies [1, 2, 5, 6]. However, no arthropathy or significant gastrointestinal effects were observed in present patients.
Deferiprone can cause neutropenia and agranulocytosis that is usually reversible on stopping the drug [15]. Neutropenia was noted in five of the 49 patients studied by Elalfy et al. and in one patient studied by Karami et al. [2, 8], while other studies on combination chelation therapy have not reported any agranulocytosis or neutropenia [1, 5, 7]. Neutropenia was not observed in any of present subjects. Six patients (29%) had transient thrombocytopenia (1 to 1.5 lakhs/mm3) in present study, which recovered within a maximum period of three months. This may also be attributed to sequestration in spleen.
Transient hepatic enzyme elevation is a commonly noted side effect of deferasirox. Totadri et al. [5], EPIC trial on deferasirox [16] and Viprakasit et al’s. [17] observation on deferiprone showed elevation in AST or ALT above five times the upper limit for age, requiring stopping of therapy to be around 10 to 16%. But in the present study only one child had elevation in ALT just above five times the upper limit for age. Even it resolved within a month without changing the drug regimen.
Transient and permanent elevation of creatinine is an expected side effect of deferasirox [9]. But long term follow up (10 y) of patients who received prolonged duration of deferasirox has not shown any significant progressive renal dysfunction [18]. In the present study all the patients were already on deferasirox (mean duration of 45 mo). Transient elevation of creatinine above baseline was seen in ten children (48%). None of them had raise in eGFR above 33% of their baseline, requiring withholding of drugs. All of them had recovery of creatinine to baseline within three months.
Thalassemia is a hyperfiltration state and proteinuria can be seen on patients normally and it is recommended to start intervention if urine PCR is above 0.6 or 0.7 [9]. Deferasirox can cause significant renal dysfunction and proteinuria [19]. In the present study, proteinuria was seen in six children (29%). Four patients had transient proteinuria that resolved during the study period. Two children had persistent proteinuria. But none of them had urine PCR above 0.5, possibly indicating proteinuria due to the thalassemic disease state rather than due to drugs.
This study evaluated prospectively for the efficacy of combined oral chelation in decreasing iron overload in thalassemic children. The authors also studied cardiac and liver MRI at baseline and after one year in significant proportion of children apart from serum ferritin. The main limitation is that required sample size for hepatic iron concentration by MRI was not fulfilled as many children did not cooperate.
Conclusions
This study showed that combined oral chelation with deferiprone and deferasirox will help in decreasing the iron overload in thalassemia children on regular transfusions. No significant effect was noted in cardiac overload. Though there was a fall in hepatic iron status, it was not statistically significant. All the children who received the combined oral chelation tolerated the drugs well.
References
Gomber S, Jain P, Sharma S, Narang M. Comparative efficacy and safety of oral iron chelators and their novel combination in children with thalassemia. Indian Pediatr. 2016;53:207–10.
Elalfy MS, Adly AM, Wali Y, Tony S, Samir A, Elhenawy YI. Efficacy and safety of a novel combination of two oral chelators deferasirox/deferiprone over deferoxamine/deferiprone in severely iron overloaded young beta thalassemia major patients. Eur J Haematol. 2015;95:411–20.
Garbowski MW, Carpenter J-P, Smith G, et al. Biopsy-based calibration of T2* magnetic resonance for estimation of liver iron concentration and comparison with R2 Ferriscan. J Cardiovasc Magn Reson. 2014;16:40.
Carpenter J-P, He T, Kirk P, et al. On T2* magnetic resonance and cardiac iron. Circulation. 2011;123:1519–28.
Totadri S, Bansal D, Bhatia P, Attri SV, Trehan A, Marwaha RK. The deferiprone and deferasirox combination is efficacious in iron overloaded patients with β-thalassemia major: a prospective, single center, open-label study. Pediatr Blood Cancer. 2015;62:1592–6.
Parakh N, Chandra J, Sharma S, Dhingra B, Jain R, Mahto D. Efficacy and safety of combined oral chelation with deferiprone and deferasirox in children with β-thalassemia major: an experience from North India. J Pediatr Hematol Oncol. 2017;39:209–13.
Hammond J, Thompson AA, Fogel MA, Hammond K, Kokroko J, Kwiatkowski JL. Combination oral chelation in adult patients with transfusion-dependent thalassemia and high iron burden. J Pediatr Hematol Oncol. 2019;41:e47–50.
Karami H, Kosaryan M, Amree AH, Darvishi-Khezri H, Mousavi M. Combination iron chelation therapy with deferiprone and deferasirox in iron-overloaded patients with transfusion-dependent β-thalassemia major. Clin Pract. 2017;7:912.
Quinn CT, Johnson VL, Kim H-Y, et al. Renal dysfunction in patients with thalassaemia. Br J Haematol. 2011;153:111–7.
Link G, Konijn AM, Breuer W, Cabantchik ZI, Hershko C. Exploring the “iron shuttle” hypothesis in chelation therapy: effects of combined deferoxamine and deferiprone treatment in hypertransfused rats with labeled iron stores and in iron-loaded rat heart cells in culture. J Lab Clin Med. 2001;138:130–8.
Wood JC. Guidelines for quantifying iron overload. Hematology Am Soc Hematol Educ Program. 2014;2014:210–5.
Wahidiyat PA, Wijaya E, Soedjatmiko S, Timan IS, Berdoukas V, Yosia M. Urinary iron excretion for evaluating iron chelation efficacy in children with thalassemia major. Blood Cells Mol Dis. 2019;77:67–71.
Siri-Angkul N, Chattipakorn SC, Chattipakorn N. Diagnosis and treatment of cardiac iron overload in transfusion-dependent thalassemia patients. Expert Rev Hematol. 2018;11:471–9.
Eghbali A, Taherahmadi H, Shahbazi M, Bagheri B, Ebrahimi L. Association between serum ferritin level, cardiac and hepatic T2-star MRI in patients with major β-thalassemia. Iran J Pediatr Hematol Oncol. 2014;4:17–21.
Belmont A, Kwiatkowski JL. Deferiprone for the treatment of transfusional iron overload in thalassemia. Expert Rev Hematol. 2017;10:493–503.
Pennell D, Porter JB, Cappellini MD, et al. Efficacy and safety of deferasirox (Exjade®) in reducing cardiac iron in patients with β-thalassemia major: results from the cardiac substudy of the EPIC trial. Blood. 2008;112:3873.
Viprakasit V, Nuchprayoon I, Chuansumrit A, et al. Deferiprone (GPO-L-ONE(®)) monotherapy reduces iron overload in transfusion-dependent thalassemias: 1-year results from a multicenter prospective, single arm, open label, dose escalating phase III pediatric study (GPO-L-ONE; A001) from Thailand. Am J Hematol. 2013;88:251–60.
Origa R, Piga A, Tartaglione I, et al. Renal safety after more than a decade of deferasirox use in patients with transfusional hemosiderosis. Blood. 2016;128:2466.
Sarbay H, Kara MA. Proteinuria due to increased dose of deferasirox in a pediatric patient with thalassemia major: case report. Int J Contemp Pediatr. 2018;5:2338–40.
Author information
Authors and Affiliations
Contributions
CGDK and RRDJ: Conceptualized the study. RRDJ: Collected the data and drafted the initial manuscript. CGDK and GRK: Analysis of data and literature search; GRK: Intellectual input in final drafting and overall supervision. All authors contributed to the critical revision of the article. Dr. Niranjan Biswal is the Guarantor for this paper.
Corresponding author
Ethics declarations
Ethics Committee Approval
Ethics Committee approval was obtained for the study from JIPMER, Institute Ethics committee (Human studies) (JIP/IEC/2017/0292).
Conflict of Interest
None.
Informed Consent
Detailed information about the study was given to the subjects who accepted to participate in the study as well as to their parents and they were asked to sign an informed consent form.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
DivakarJose, R.R., Delhikumar, C.G. & Ram Kumar, G. Efficacy and Safety of Combined Oral Chelation with Deferiprone and Deferasirox on Iron Overload in Transfusion Dependent Children with Thalassemia – A Prospective Observational Study. Indian J Pediatr 88, 330–335 (2021). https://doi.org/10.1007/s12098-020-03442-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12098-020-03442-5