Abstract
Tumor lysis syndrome (TLS), including hyperuricemia, is a frequent serious complication in patients with hematologic malignancies. This study in Japanese patients evaluated the efficacy, safety, and pharmacokinetic profile of rasburicase in pediatric patients with hematologic malignancies. Patients aged <18 years at high risk for TLS, with newly diagnosed hematologic malignancies, were randomized to intravenous rasburicase 0.15 mg/kg/day (n = 15) or 0.20 mg/kg/day (n = 15) for 5 days. Chemotherapy was started 4–24 h after the first rasburicase dose. Response was defined as a reduction in plasma uric acid to ≤6.5 mg/dL (patients <13 years) or ≤7.5 mg/dL (patients ≥13 years) by 48 h after the first administration, lasting until 24 h after the final administration. Response rates were 93.3 and 100% with rasburicase 0.15 and 0.20 mg/kg/day, respectively. Uric acid levels declined rapidly within 4 h of starting rasburicase administration in both groups. Most adverse events were related to the underlying chemotherapy regimens. Two hypersensitivity reactions, including grade 1/2 pruritus, were considered to be related to rasburicase. Rasburicase is effective and well tolerated for the management of hyperuricemia in Japanese pediatric patients at high risk of developing TLS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Patients with hematologic malignancies are usually treated with aggressive chemotherapy regimens that result in the rapid destruction of tumor cells and the release of purine metabolites into the circulation [1]. This may lead to the development of tumor lysis syndrome (TLS), which is characterized by severe hyperuricemia, hyperphosphatemia, hyperkalemia, and hypocalcemia [2, 3]. Moreover, as a consequence of hyperuricemia, crystals of uric acid may form in the renal tubules and distal collecting system, leading to renal insufficiency and acute renal failure [4]. Patients with malignancies that have a high proliferation rate or a large tumor burden, such as acute lymphoblastic leukemia or Burkitt’s lymphoma, have a particularly high risk of developing TLS. The metabolic disturbances resulting from TLS may lead to acute renal failure and rapidly become life threatening in pediatric patients. Appropriate management for metabolic abnormalities in these patients is therefore essential in order to reduce the risk of developing acute renal failure [5–7].
The current treatment of hyperuricemia in Japan includes urinary alkalinization, hydration, and allopurinol. Allopurinol inhibits xanthine oxidase and thus prevents the formation of uric acid and controls plasma uric acid levels during purine catabolism [4]. Allopurinol, however, cannot reduce the level of pre-existing uric acid and causes increases in serum levels of xanthine and hypoxanthine, which may lead to xanthine nephropathy [8, 9]. In addition, urinary alkalinization can cause renal precipitation of calcium phosphate [4].
Rasburicase is a recombinant form of the endogenous enzyme urate oxidase. It is produced following the proteolytic hydrolysis of Aspergillus flavus urate oxidase, which permits the formation of oligodeoxynucleotide probes that are used to obtain DNA fragments from Aspergillus flavus cDNA and genomic libraries [10]. Rasburicase is approved for the prevention and treatment of hyperuricemia in children with leukemia or lymphoma in the USA and the EU. This agent oxidizes uric acid, converting it to allantoin, a substance that is approximately 5–10 times more soluble than uric acid and is easily excreted in the urine [8]. Rasburicase is administered intravenously, making it more convenient to administer to patients with chemotherapy-associated gastrointestinal toxicities than the oral drug allopurinol. Moreover, rasburicase can reduce pre-existing uric acid levels [11].
In a US open-label, randomized study in 52 children with leukemia or lymphoma at high risk for TLS, administration of rasburicase (0.20 mg/kg/day) for 5–7 days during induction chemotherapy achieved significantly more rapid control of uric acid and lower levels of plasma uric acid than allopurinol (300 mg/m2/day) for 5–7 days [12]. This led the investigators to conclude that rasburicase is a safe and an effective alternative to allopurinol during initial chemotherapy in pediatric patients.
The aim of this study was to investigate the efficacy, safety, and pharmacokinetic profile of rasburicase as a single agent in Japanese pediatric patients with hematologic malignancies at high risk for TLS. In particular, the safety of rasburicase administered before chemotherapy was evaluated in this patient population.
2 Materials and methods
2.1 Study design and patients
This was a multicenter, open-label, randomized, parallel-group study of repeated doses of rasburicase in Japanese pediatric patients with newly diagnosed hematologic malignancies at high risk of developing TLS.
The study protocol was approved by the institutional review boards of all participating centers. Written informed consent was obtained from the legally authorized representative of each patient before randomization to one of two doses of rasburicase (0.15 or 0.20 mg/kg).
Japanese pediatric patients (aged <18 years) were eligible for study entry if they had newly diagnosed hematologic malignancies with hyperuricemia (uric acid >7.5 mg/dL for patients aged ≥13 years; uric acid >6.5 mg/dL for patients aged <13 years) or newly diagnosed hematologic malignancies presenting with a high tumor burden, regardless of uric acid level [defined as non-Hodgkin’s lymphoma (NHL) stage IV; NHL stage III with at least one lymph node or mass >5 cm in diameter or lactate dehydrogenase (LDH) three or more times the upper limit of normal (ULN)]; or acute leukemia with a white blood cell (WBC) count ≥50,000/mm3 and LDH three or more times ULN. Patients were required to have a performance status of 3 or less on the Eastern Cooperative Oncology Group (ECOG) scale (or 30 or more on the Lansky score) and a minimum life expectancy of 45 days. Patients received induction chemotherapy between 4 and 24 h after the first administration of rasburicase.
Exclusion criteria included the administration of allopurinol within 72 h before the start of rasburicase administration; known history of severe allergy and/or severe asthma; low birth weight (<2,500 g) or gestational age (<37 weeks); previous therapy with urate oxidase; known positive tests for hepatitis B surface antigen, hepatitis C virus antibodies, or HIV-1 or HIV-2 antibodies; severe disorders of the liver or kidney [alanine aminotransferase (ALT) levels more than five times ULN, total bilirubin more than three times ULN, creatinine more than three times ULN]; or uncontrollable infection (including viral infection). The enzymatic conversion of uric acid to allantoin by rasburicase produces hydrogen peroxide [13]. This can lead to methemoglobinemia and hemolysis in certain “at-risk” populations such as those with glucose-6-phosphate dehydrogenase (G6PD) deficiency, and hence G6PD deficiency contraindicates the use of rasburicase. Therefore, patients with a known family history of G6PD deficiency, and known history of methemoglobinemia and hemolysis, were also excluded.
Randomization was performed centrally, and patients were stratified by baseline weight (<10 or ≥10 kg) until 15 patients had been enrolled in each dose group. To ensure the exact evaluation of pharmacokinetics, at least 10 patients weighing ≥10 kg were included in each dose group. The protocol did not require that a minimum number of patients weighing <10 kg should be enrolled.
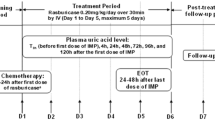
2.2 Treatment
Rasburicase (SR29142) was supplied by sanofi-aventis (Tokyo, Japan). Patients were randomized to one of two dose groups of rasburicase (0.15 or 0.20 mg/kg). Rasburicase 0.20 mg/kg has been approved in 50 countries worldwide, but in the USA, the doses of rasburicase 0.15 and 0.20 mg/kg have been approved. Given that the efficacy of rasburicase 0.15 and 0.20 mg/kg was recently demonstrated in a previous study in adult Japanese patients [14], both these doses were selected for use in this pediatric trial. Rasburicase was administered intravenously for 30 min once daily for 5 consecutive days.
Chemotherapy, including cytoreductive corticosteroids, was started 4–24 h after the first dose of rasburicase. Separate lines were used for administration of chemotherapy and infusion of rasburicase to prevent drug–drug interactions. When this was not possible, the line was flushed with isotonic saline (≥15 mL) before and after infusion of rasburicase. Other anti-hyperuricemic agents (e.g. allopurinol) or treatment with sodium bicarbonate for urine alkalization were not permitted until the final blood sampling for plasma uric acid was completed on day 6.
2.3 Efficacy assessments
The primary efficacy endpoint was response rate (RR), as determined by assays of plasma uric acid concentration. Treatment was considered to be successful and the patient considered to be a responder if the plasma uric acid level decreased to ≤7.5 mg/dL in patients aged ≥13 years or ≤6.5 mg/dL in patients aged <13 years by 48 h after the start of the first rasburicase administration, and lasting until 24 h after the start of the final rasburicase administration (day 5).
Secondary endpoints included plasma uric acid concentration and change in concentration from baseline. The rate of plasma uric acid inhibition over time versus baseline was also evaluated at 4 and 48 h after the first rasburicase administration and at 24 h after the last rasburicase administration. The rate of uric acid inhibition (%) was calculated as the concentration of plasma uric acid at baseline minus the concentration of plasma uric acid at each timepoint divided by the concentration at baseline multiplied by 100. Blood samples were collected for the plasma uric acid levels ≤10 min before and 4 h (±10 min) after the first rasburicase administration on day 1; samples were also collected before rasburicase administration (±10 min) on days 2–5, and 24 h (±10 min) after the last rasburicase administration on day 6.
2.4 Safety assessments
Safety was assessed by clinical observations (including vital signs), standard laboratory tests, and the occurrence of adverse events (AEs). AEs were summarized by type of event and toxicity grade according to the National Cancer Institute Common Terminology Criteria for Adverse Events version 3.0 (translated into Japanese by the Japan Clinical Oncology Group/Japan Society of Clinical Oncology). These events were classified by each investigator as either rasburicase-related or other (related to underlying hematologic malignancies or chemotherapy). Rasburicase-related AEs were defined as all events excluding events due to the underlying disease or chemotherapy. Renal function (creatinine, potassium, phosphorus, and calcium levels) was also assessed at baseline (7 days before starting the first administration of rasburicase), and on day 3, 5, 8, 15, 22, 29, and 36.
2.5 Evaluation of anti-rasburicase antibodies
To evaluate the relationship between hypersensitivity reactions and the appearance of anti-rasburicase antibodies, the antibodies were assessed by qualitative enzyme-linked immunosorbent assay (ELISA) at baseline and on day 29. The results were expressed qualitatively due to the lack of immunopurified reference human antibody directed against rasburicase, with the conventional properties of antibodies utilized to detect antibodies directed against rasuburicase. The range of anti-human immunoglobulin calibration was between 0 and 1,000 ng/mL and plasma samples from healthy volunteers were used as reference controls. Plasma collected from healthy volunteers was assayed by ELISA to determine background interference in the detection of anti-rasburicase immunoglobulin. If the samples were positive for anti-rasburicase antibodies on day 29, then further blood samples were collected from the patient at 6 months (±2 weeks) and every 6 months (±2 weeks) thereafter until the sample was negative. Samples that were antibody positive were analyzed for inhibition of rasburicase uricolytic activity. Anti-S. cerevisiae protein (SCP) antibodies were also assessed by ELISA at baseline.
2.6 Pharmacokinetics
The pharmacokinetic assay was performed in 10 patients (weight ≥10 kg) in each dose group at the following 10 timepoints: Day 1, before rasburicase administration (within 10 min of the start of administration), at the end of the first administration (within 10 min following completion of administration), 4 and 8 h (±10 min) after the start of administration; day 2, before rasburicase administration (within 10 min of the start of administration); and day 5, before rasburicase administration (within 10 min of the start of administration), at the end of administration, 4, 8, and 24 h (±10 min) after the last administration. A total sample of 10 mL from each patient was immediately centrifuged at <4°C and then frozen until assay. Frozen samples were sent to the laboratories (SBI-BIO, Paris, France), where they were assayed concomitantly.
The following pharmacokinetic parameters were determined: area under the rasburicase plasma concentration–time curve from 0 to 24 h (AUC0–24) on days 1 and 5; minimum rasburicase plasma concentration observed before treatment administration during repeated dosing (C min) on days 1 and 5; plasma concentration of rasburicase at the end of infusion (C eoi) on days 1 and 5; terminal half-life (t 1/2z) on day 5; and accumulation ratio for AUC0–24 and C eoi (defined as the ratio of day 5 to day 1 for AUC0–24 and C eoi). Rasburicase plasma concentrations were determined by ELISA.
2.7 Statistical analysis
All patients who received at least one dose of rasburicase were evaluated for efficacy and safety. The RR, with 95% exact binomial confidence intervals (CIs), was calculated as the number of responding patients divided by the number of evaluable patients multiplied by 100. Patients who failed to complete days 1–5 of treatment, for reasons other than hyperuricemia, were considered as nonevaluable for RR. Descriptive statistics were used to summarize uric acid concentrations, and change from baseline and the rate of plasma uric acid concentration decline over time.
For the purposes of the statistical analysis, the study had a planned sample size of 30 patients, i.e. 15 in each dose group (0.15 and 0.20 mg/kg). Assuming that the true RR would be 95% in each dose group, the probability of at least one failure among 15 patients treated with each dose of rasburicase would be 79%, with an expected lower 95% CI of 71%. Based on a sample size of 15 patients per dose group, it could therefore be concluded with 95% confidence that the true RR would be at least 71%.
Pharmacokinetic parameters for rasburicase were determined using WinNonlin Professional Edition software (version 3.3 Pharsight Corp, Mountain View, CA, USA) using a noncompartmental method. To assess drug accumulation from day 1 to day 5, the parameters AUC0–24 and C eoi were analyzed using the linear mixed-effects model:
Fixed-effect terms included dose (0.15 and 0.20 mg/kg), day (1 and 5), and the interaction term dose by day. The random-effect term was patient within dose. The model was estimated using generalized least squares (GLS) with restricted maximum likelihood (REML) estimates of random effects, using SAS® PROC MIXED.
The 95% CIs for the variance estimates were computed using the simple chi-squared method for within-patient variance, the Modified Large Sample procedure for between-patient variance, and the Graybill–Wang procedure for the total-patient variance [15].
3 Results
3.1 Patients
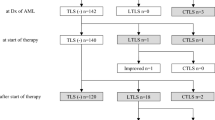
Between June 2005 and April 2006, 31 patients were enrolled and 30 patients were subsequently randomized and treated (rasburicase 0.15 mg/kg, n = 15; rasburicase 0.20 mg/kg, n = 15). One enrolled patient was not randomized to treatment because of an ineligible ALT level. This patient was excluded from the efficacy and safety analyses.
Patient baseline characteristics were similar between the rasburicase dose groups (Table 1). The median age was 8.8 years, and over half of the patients (53.3%) were aged between 6 and 12 years. Overall median weight was 30.8 kg, and one patient weighed <10 kg. Most patients had an ECOG performance status of 0 (40%) or 1 (40%). A total of 43.3% of patients were hyperuricemic, and 73.3% of patients had acute leukemia. All patients were classified as high risk for TLS in accordance with the inclusion criteria (i.e. had a newly diagnosed hematologic malignancy with hyperuricemia or a high tumor burden).
3.2 Administration of rasburicase
Twenty-nine of 30 patients completed days 1–5 of treatment; one patient in the rasburicase 0.20 mg/kg group withdrew from the study on day 1 after the first administration of rasburicase due to the lack of WBC count at baseline. Another patient (0.15 mg/kg group) completed 5 days of treatment but withdrew from the study on day 8 to avoid life-threatening complications due to three concomitant grade 4 AEs (cerebral hemorrhage, brain edema, and brain herniation). Fifteen patients in the 0.15 mg/kg group and 14 patients in the 0.20 mg/kg group were therefore evaluable for response.
3.3 Efficacy
The overall RR for all patients was 96.6% (95% CI 82.2–99.9%) (Table 2). The RR was slightly higher in the rasburicase 0.20 mg/kg group than in the 0.15 mg/kg group (100% [95% CI 76.8–100.0%] vs. 93.3% [95% CI 68.1–99.8%]).
RRs for patients with hyperuricemia at baseline were 87.5 and 100.0% in the rasburicase 0.15 and 0.20 mg/kg groups, respectively (Table 2).
Mean plasma uric acid concentrations by dose of rasburicase over time are presented in Fig. 1. Rasburicase produced a rapid decrease in plasma uric acid concentrations in both dose groups. Uric acid levels remained low throughout treatment in all patients except one non-responder in the 0.15 mg/kg group. Uric acid levels declined rapidly within 4 h of the first rasburicase dose in both dose groups and remained low up to 120 h after the first administration of rasburicase (Fig. 1). Mean plasma uric acid concentrations were reduced by 84.8% (95% CI 76.7–92.9%) and 92.9% (95% CI 88.7–97.0%) compared with baseline at 4 h after the first rasburicase administration for the 0.15 and 0.20 mg/kg groups, respectively. Reductions in the level of plasma uric acid were similar between the two groups at 24 h after the last administration of rasburicase on day 6 (approximately 88%).
Mean plasma uric acid concentration by dose over time. Patients aged <18 years with newly diagnosed hematologic malignancies with hyperuricemia, or newly diagnosed hematologic malignancies presenting with a high tumor burden regardless of uric acid level, were randomly allocated (based on stratification by weight [<10 or ≥10 kg]) to receive rasburicase (SR29142) administered at either 0.15 or 0.20 mg/kg/day for 5 days, followed by chemotherapy starting from 4 to 24 h after the first infusion of rasburicase
3.4 Safety
Owing to the severity of the underlying disease, all patients experienced at least one grade 3/4 AE, regardless of rasburicase treatment. The most common grade 3/4 AEs were leukopenia (86.7% of patients), neutropenia (83.3%), lymphocytopenia (80.0%), and increased ALT levels (70.0%). All of these AEs occurred with a similar frequency in both dose groups, with the exception of neutropenia (rasburicase 0.15 mg/kg, 93.3%; rasburicase 0.20 mg/kg, 73.3%). The majority of AEs reported during the study period were judged by the investigators to be related to the underlying malignancies and/or chemotherapy. There was no difference in the safety profiles of rasburicase 0.15 mg/kg/day for 5 days and rasburicase 0.20 mg/kg/day for 5 days.
The three grade 4 AEs (cerebral hemorrhage, brain edema, and brain herniation) experienced by one patient in the rasburicase 0.15 mg/kg group who withdrew from the study on day 8, were judged by the investigators to be unrelated to rasburicase treatment. The patient died after withdrawal from the study. No other deaths were reported during the study.
Drug-related AEs occurred in six patients (n = 4 in the rasburicase 0.15 mg/kg group; n = 2 in the 0.20 mg/kg group). One patient in the rasburicase 0.20 mg/kg group experienced grade 3/4 hemolysis; the patient did not have G6PD deficiency. The risk of rasburicase-induced hemolysis, possibly leading to hemolytic anemia and methemoglobinemia, is greater in patients with G6PD deficiency because of the accumulation of hydrogen peroxide [13]. However, rare cases of rasburicase-induced methemoglobinemia have been reported in patients without G6PD deficiency [12, 16]. Two rasburicase-related AEs occurred after the administration of rasburicase but before the start of chemotherapy (grade 1/2 hypersensitivity in the rasburicase 0.15 mg/kg group and grade 3/4 anemia in the rasburicase 0.15 mg/kg group).
Hypersensitivity reactions (all grades) were reported in 8 patients (53.3%) in the 0.15 mg/kg group and 12 patients (80.0%) in the 0.20 mg/kg group. Grade 3/4 events were only reported in two patients in the 0.15 mg/kg group: one patient completely recovered from the hypersensitivity reaction by day 6, although the other patient experienced persistent drug hypersensitivity until day 32. However, these grade 3/4 hypersensitivity reactions were judged to be unrelated to rasburicase. Only two AEs (hypersensitivity [grade 1/2] and hemoglobin decreased [grade 1/2]), observed before chemotherapy, were considered to be related to rasburicase. Anti-rasburicase antibodies or anti-SCP antibodies were not observed in any patients with hypersensitivity reactions.
A slight decrease in serum creatinine levels from baseline was observed. The mean values (±standard deviation) of serum creatinine were 52.3 μmol (±22.6) at baseline, 43.6 μmol (±16.3) on day 3, and 33.5 μmol (±11.5) on day 36 for the 0.15 mg/kg rasburicase group; and 44.4 μmol (±19.1) at baseline, 36.7 μmol (±11.8) on day 3, and 27.1 μmol (±7.1) on day 36 for the 0.20 mg/kg group. No clinically significant changes were observed for the other renal function parameters (potassium, phosphorous, and calcium) during the study period.
3.5 Antibodies
Anti-SCP antibodies were detected in one patient before administration of rasburicase 0.20 mg/kg. Anti-rasburicase antibodies were detected in another patient in this group on day 29 and the patient tested negative for antibodies 6 months after the first administration. Neither patient experienced a hypersensitivity reaction during the study.
3.6 Pharmacokinetics
Blood samples to determine plasma concentrations of rasburicase were collected from 20 patients, 10 in each dose group. One patient in the 0.20 mg/kg dose group was excluded due to only two samples having been collected on day 1 of the study. Therefore, 19 patients were evaluable for AUC0–24 on day 1 and C min, C eoi, AUC0–24, and t 1/2z on day 5.
The pharmacokinetic profile of rasburicase is summarized in Table 3. Increase in exposure to rasburicase over days 1–5, as measured by AUC0–24 and C eoi, was dose proportional. For the 1.33-fold increase in dose from 0.15 to 0.20 mg/kg, AUC0–24 increased 1.13-fold and 1.30-fold on days 1 and 5, respectively, while C eoi increased 1.21-fold and 1.23-fold on days 1 and 5, respectively.
Rasburicase accumulated slightly on day 5, as assessed by AUC0–24 and C eoi. The accumulation ratios of AUC0–24 and C eoi (defined as the ratio of day 5 to day 1 for AUC0–24 and C eoi) were 1.13 (95% CI 1.02–1.25) and 1.17 (95% CI 1.09–1.27), respectively, indicating slight accumulation. Mean t 1/2z was comparable for both dose groups.
4 Discussion
The data from this study show that administration of rasburicase 0.15 or 0.20 mg/kg before the start of chemotherapy is well tolerated in Japanese pediatric patients with acute leukemia or non-Hodgkin’s lymphoma. A rapid reduction in plasma uric acid levels to ≤7.5 mg/dL in patients ≥13 years or ≤6.5 mg/dL in patients <13 years within 48 h after the start of the first rasburicase administration occurred and lasted until 24 h after the last rasburicase administration on day 5 in 28 of 29 patients (96.6%). Moreover, 12 of 13 patients with hyperuricemia at baseline responded to treatment. A high overall RR of 96.6% was observed, indicating the efficacy of rasburicase for both the prophylaxis and treatment of hyperuricemia in pediatric patients receiving chemotherapy.
Notably, all evaluable patients in the rasburicase 0.20 mg/kg group achieved a response and only one evaluable patient in the 0.15 mg/kg group did not respond. In addition, there was a greater reduction in plasma uric acid concentrations from baseline at 4 h with the higher dose of rasburicase (92.9 vs. 84.8%), further demonstrating the greater efficacy of the rasburicase 0.20 mg/kg dose.
These findings add further credence to the results of the randomized US study conducted by Goldman et al. [12], which demonstrated more rapid control of uric acid and a lower plasma uric acid concentration during the first 96 h of therapy with rasburicase 0.20 mg/kg/day compared with 5–7 days of treatment with allopurinol in pediatric patients with high risk for TLS. In addition, several single-arm studies conducted in Europe, North America, Australia, and Asia have evaluated the 0.20 mg/kg dose of rasburicase for up to 7 days in pediatric and adult patients with high risk for TLS [17–21]. In line with our findings and those of Goldman et al. [12], these studies also reported numerically greater response rates (based on normalization of uric acid concentration) of 97–100% with rasburicase 0.20 mg/kg.
This is the first report to comprehensively assess rasburicase-related AEs occurring before the start of chemotherapy in pediatric patients. The majority of AEs reported during the treatment period were judged to be related to the underlying malignancies or chemotherapy by the investigators, with a low incidence of rasburicase-related AEs. Only two rasburicase-related AEs, including one hypersensitivity reaction, were observed before the start of chemotherapy in the rasburicase 0.15 mg/kg group. Most rasburicase-related AEs observed after the start of chemotherapy had a similar profile to those related to the underlying malignancies or chemotherapy. Patients who receive chemotherapy for hematologic malignancies are often exposed to risk of renal dysfunction. In the present study, renal parameters such as serum creatinine were not aggravated until completion of chemotherapy, suggesting that rasburicase might preserve renal function during induction chemotherapy.
Interestingly, new guidelines regarding the management of patients at risk of developing TLS and its prevention have recently been published [22]. Prevention strategies, including hydration and prophylactic rasburicase in high-risk patients, hydration plus allopurinol or rasburicase for intermediate-risk patients, and close monitoring for low-risk patients, are advised [22]. In addition, the guidelines advise aggressive hydration and diuresis plus allopurinol or rasburicase for hyperuricemia as primary management of established TLS.
An observational study has shown that treatment with rasburicase according to this new guideline is effective in preventing and controlling hyperuricemia and TLS in children with hematologic malignancies [23]. The study reported that the duration of rasburicase treatment should be tailored to the duration and intensity of tumor cell lysis in the patient by closely monitoring clinical chemistry. The superiority of rasburicase in comparison with allopurinol for the prophylaxis and treatment of hyperuricemia in children with leukemia and lymphoma has been demonstrated [24]. Rasburicase, administered at a dose of 0.20 mg/kg for 5 consecutive days, resulted in a rapid and significant decrease in uric acid levels after 4 h [24], in line with the findings reported in the current study. Rasburicase was also a more potent and more rapid uricolytic agent than allopurinol.
As rasburicase is a recombinant protein, antibodies can be produced against this agent. However, the clinical implication of such anti-rasburicase antibodies is unknown. In this trial, anti-rasburicase antibody production was reported in one patient on day 29, however, this patient did not experience a hypersensitivity reaction during the study. None of the patients had any anti-rasburicase antibodies on day 8. In previous studies in which rasburicase was administered to patients with cancer, although a small number of patients were shown to have anti-rasburicase antibodies, production of the antibody was not associated with the clinical status of the patients or the occurrence of AEs, including hypersensitivity reactions [25]. Goldman et al. [12] reported no cases of rasburicase antibody production in the US pediatric study using rasburicase 0.20 mg/kg, whereas Pui et al. [26] reported antibody production in 17 of 121 children and young adults treated with rasburicase 0.15 or 0.20 mg/kg. Other studies evaluating rasburicase did not assess rasburicase antibody production [18–21]. The production of anti-SCP antibody was also reported in one patient before the first administration of rasburicase. In this patient, a hypersensitivity reaction was not experienced during this study. This suggests that there was no correlation between the presence of anti-rasburicase or anti-SCP antibodies and the occurrence of hypersensitivity reactions in this study. However, because of the limited number of patients with antibody production in the current study, further studies are required in order to confirm this finding.
The pharmacokinetic data obtained in this study support the premise of dose proportionality of rasburicase, with only slight drug accumulation during 5 days of treatment. These data are consistent with the known pharmacokinetic profile of rasburicase in Western populations [26], suggesting that there is no ethnic variation in terms of the pharmacokinetic profile of rasburicase. Based on the results presented here, a daily rasburicase dose of 0.20 mg/kg might be recommended, particularly for patients who are more seriously ill and at high risk of developing TLS. However, as only a small sample size was studied in the present study and no comparator or placebo arm was included for comparison, further studies are needed to confirm the optimal dose of rasburicase for patients in different risk categories.
In conclusion, this study provides further evidence that rasburicase is highly effective in the control of hyperuricemia, a component of TLS, in pediatric patients undergoing chemotherapy for non-Hodgkin’s lymphoma or acute leukemia. The study also demonstrates that rasburicase is safe and well tolerated when administered before the start of chemotherapy in this group of patients.
References
Ronco C, Inguaggiato P, Bordonia V, De Cal M, Bonello M, Andrikos E, et al. Rasburicase therapy in acute hyperuricemia and renal dysfunction. Contrib Nephrol. 2005;147:115–23.
Jones DP, Stapleton FB, Kalwinsky D, McKay CP, Kellie SJ, Pui CH. Renal dysfunction and hyperuricemia at presentation and relapse of acute lymphoblastic leukemia. Med Pediatr Oncol. 1990;18:283–6.
Arrambide K, Toto RD. Tumor lysis syndrome. Semin Nephrol. 1993;13:273–80.
Davidson MB, Thakkar S, Hix JK, Bhandarkar ND, Wong A, Schreiber MJ. Pathophysiology, clinical consequences, and treatment of tumor lysis syndrome. Am J Med. 2004;116:546–54.
Cohen LF, Balow JE, Magrath IT, Poplack DG, Ziegler JL. Acute tumor lysis syndrome. A review of 37 patients with Burkitt’s lymphoma. Am J Med. 1980;68:486–91.
Stapleton FB, Strother DR, Roy S, Wyatt RJ, McKay CP, Murphy SB. Acute renal failure at onset of therapy for advanced stage Burkitt lymphoma and B cell acute lymphoblastic lymphoma. Pediatrics. 1988;82:863–9.
Bowman WP, Shuster JJ, Cook B, Griffin T, Behm F, Pullen J, et al. Improved survival for children with B-cell acute lymphoblastic leukemia and stage IV small noncleaved-cell lymphoma: a pediatric oncology group study. J Clin Oncol. 1996;14:1252–61.
Cheson BD, Dutcher BS. Managing malignancy-associated hyperuricemia with rasburicase. J Support Oncol. 2005;3:117–24.
Sood AR, Burry LD, Cheng DK. Clarifying the role of rasburicase in tumor lysis syndrome. Pharmacotherapy. 2007;27:111–21.
Legoux R, Delpech B, Dumont X, Guillemot J-C, Ramond P, Shire D, et al. Cloning and expression in Escherichia coli of the gene encoding Aspergillus flavus urate oxidase. J Biol Chem. 1992;267:8565–70.
Oldfield V, Perry CM. Spotlight on rasburicase in anticancer therapy-induced hyperuricemia. BioDrugs. 2006;20:197–9.
Goldman SC, Holcenberg JS, Finklestein JZ, Hutchinson R, Kreissman S, Johnson FL, et al. A randomized comparison between rasburicase and allopurinol in children with lymphoma or leukemia at high risk for tumor lysis. Blood. 2001;97:2998–3003.
Bessmertny O, Robitaille LM, Cairo MS. Rasburicase: a new approach for preventing and/or treating tumor lysis syndrome. Curr Pharm Des. 2005;11:4177–85.
Ishizawa K, Ogura M, Hamaguchi M, Hotta T, Ohnishi K, Sasaki T, et al. Safety and efficacy of rasburicase (SR29142) in a Japanese phase II study. Cancer Sci. 2008 Dec 14. [Epub ahead of print].
Graybill FA, Wang C. Confidence intervals on nonnegative linear combinations of variances. J Am Stat Assoc. 1980;75:869–73.
Kizer N, Martinez E, Powell M. Report of two cases of rasburicase-induced methemoglobinemia. Leuk Lymphoma. 2006;47:2648–50.
Pui CH, Jeha S, Irwin D, Camitta B. Recombinant urate oxidase (rasburicase) in the prevention and treatment of malignancy-associated hyperuricemia in pediatric and adult patients: results of a compassionate-use trial. Leukemia. 2001;15:1505–9.
Bosly A, Sonet A, Pinkerton CR, McCowage G, Bron D, Sanz MA, et al. Rasburicase (recombinant urate oxidase) for the management of hyperuricemia in patients with cancer: report of an international compassionate use study. Cancer. 2003;98:1048–54.
Jeha S, Kantarjian H, Irwin D, Shen V, Shenoy S, Blaney S, et al. Efficacy and safety of rasburicase, a recombinant urate oxidase (Elitek™), in the management of malignancy-associated hyperuricemia in pediatric and adult patients: final results of a multicenter compassionate use trial. Leukemia. 2005;19:34–8.
Shin HY, Kang HJ, Park ES, Choi HS, Ahn HS, Kim SY, et al. Recombinant urate oxidase (rasburicase) for the treatment of hyperuricemia in pediatric patients with hematologic malignancies: results of a compassionate prospective multicenter study in Korea. Pediatr Blood Cancer. 2006;46:439–45.
Wang L-Y, Shih LY, Chang H, Jou ST, Lin KH, Yeh TC, et al. Recombinant urate oxidase (rasburicase) for the prevention and treatment of tumor lysis syndrome in patients with hematologic malignancies. Acta Haematol. 2006;115:35–8.
Coiffier B, Altman A, Pui CH, Younes A, Cairo MS. Guidelines for the management of pediatric and adult tumor lysis syndrome: an evidence-based review. J Clin Oncol. 2008;26:2767–78.
Bertrand Y, Mechinaud F, Brethon B, Mialou V, Auvrignon A, Nelken B, et al. for SFCE (Société Française de Lutte contre les Cancers et Leucémies de l’Enfant et de l’Adolescent) recommendations for the management of tumor lysis syndrome (TLS) with rasburicase: an observational survey. J Pediatr Hematol Oncol. 2008;30:267–71.
Rényi I, Bárdi E, Udvardi E, Kovács G, Bartyik K, Kajtár P, et al. Prevention and treatment of hyperuricemia with rasburicase in children with leukemia and non-Hodgkin’s lymphoma. Pathol Oncol Res. 2007;13:57–62.
Pui CH. Rasburicase: a potent uricolytic agent. Expert Opin Pharmacother. 2002;3:433–42.
Pui CH, Mahmoud HH, Wiley JM, Woods GM, Leverger G, Camitta B, et al. Recombinant urate oxidase for the prophylaxis or treatment of hyperuricemia in patients with leukemia or lymphoma. J Clin Oncol. 2001;19:697–704.
Acknowledgments
We thank the following additional investigators: Shoichi Koizumi, M.D., Ph.D. (Department of Pediatrics, Kanazawa University Hospital); Akira Ohara, M.D. (Department of Blood Transfusion, Toho University Omori Medical Center); Yoshihiro Komada, M.D., Ph.D. (Institute of Molecular and Experimental Medicine, Mie University Hospital); Takashi Kaneko, M.D. (Department of Hematology/Oncology, Tokyo Metropolitan Kiyose Children’s Hospital). Members of the Efficacy and Safety Evaluation Committee: Fumio Bessho, M.D. (Kyorin University Hospital); Shuki Mizutani, M.D. (Tokyo Medical and Dental University Hospital); Hideo Mugishima, M.D. (Nihon University Itabashi Hospital). Other participating institutions: Nippon Medical School Hospital; National Center for Child Health and Development; Tohoku University Hospital, Saga Medical School Hospital; Shizuoka Children’s Hospital; National Hospital Organization Hokkaido Cancer Center; Hiroshima University Hospital. Editorial support provided by sanofi-aventis.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Kikuchi, A., Kigasawa, H., Tsurusawa, M. et al. A study of rasburicase for the management of hyperuricemia in pediatric patients with newly diagnosed hematologic malignancies at high risk for tumor lysis syndrome. Int J Hematol 90, 492–500 (2009). https://doi.org/10.1007/s12185-009-0402-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12185-009-0402-6