Abstract
Background
Sleep disturbance is associated with poorer outcomes in cardiac patients, but little is known about the independent role of sleep quality in coronary artery bypass graft (CABG) patients.
Purpose
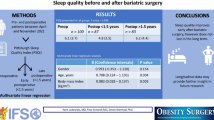
This study aims to examine the relationship between preoperative sleep complaints and post-operative emotional and physical recovery in CABG surgery patients, independently of demographic, clinical and mood factors.
Methods
Two hundred thirty CABG patients (aged 67.81 ± 9.07 years) completed measures of self-reported sleep complaints before surgery and health-related quality of life (HRQoL), physical symptoms and pain 2 months after surgery.
Results
Greater sleep complaints prior to surgery were associated with greater physical symptoms, poorer physical HRQoL and greater sensory pain after surgery (p < 0.05), but not with affective pain or mental HRQoL. Preoperative mood was not able to explain these associations.
Conclusions
Sleep complaints may be implicated in physical recovery from CABG surgery but further work is needed to understand the role of causal pathways.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Despite high survival rates and cardiac symptom relief, many patients fail to show improvements in their quality of life following coronary artery bypass graft (CABG) surgery. The reason for this is not clear and has yet to be fully accounted for in the literature. For example, Hawkes and Mortensen [1] reported cross-cultural data showing that 27 % of cardiac surgery patients have a clinically significant decline in quality of life at 6-month follow-up compared to pre-surgery levels, and this has been supported by others [2]. In addition, many patients continue to experience physical symptoms related to the surgical procedure, such as pain, fatigue and swelling, in the months following CABG [3–5].
Sleep disturbance may contribute to poorer adaptation following CABG surgery. Sleep duration and quality are thought to be particularly relevant to cardiac populations, being associated with both cardiovascular disease development and incident events [6–8]. A recent meta-analysis of prospective studies found that both short and long sleep duration were associated with increased risk of developing or dying from coronary heart disease and stroke [9]. Specific characteristics of poor sleep have also been investigated in relation to cardiac outcomes, with evidence for the cardiotoxic effects of difficulty falling asleep [10–12] and restless and disturbed sleep [13]. Although sleep is recognised to be an important issue in post-CABG recovery [14, 15], very few studies have investigated the impact of sleep disturbance on physical and emotional adaptation and recovery following cardiac surgery. Hunt and colleagues [16] studied 123 patients finding that those who reported poor sleep quality on a single-item measure were 4.8 times more likely to report poor health-related quality of life (HRQoL) 12 months following CABG. Redeker and colleagues [17] studied 72 cardiac surgery patients with both self-report and objective measures of sleep, and reported cross-sectional associations between poor sleep quality and worsened physical and emotional HRQoL at 4 and 8 weeks after surgery. Lastly, an investigation of 38 males prior to CABG surgery used prospective analyses to show that the pre-surgery sleep symptom of feeling unrefreshed on awakening explained 44.5 % of variance in HRQoL 6 months after surgery [18]. The work in this area highlights sleep as an important factor in the prediction of mental and physical adaptation following CABG; however, it is not clear to what extent sleep acts independently of depressed mood in CABG patients; this is an important area for further work given that sleep disturbance is in itself a symptom of depression, and depression is a key prognostic factor in CABG patients [19]. Moreover, it is not clear whether poor sleep quality has an impact on other aspects of surgical recovery following CABG, such as physical symptom reporting and pain.
In the current study, we aimed to examine the relationship between preoperative sleep complaints and post-operative physical and emotional recovery, in the months following CABG surgery, using a prospective design. Specifically, we hypothesised that patients who reported greater sleep complaints before surgery would be more likely to have worse physical adaptation and recovery in the months after surgery, including impaired HRQoL, greater self-reported physical symptoms and greater pain, and that the associations would be independent of baseline depression and anxiety symptoms, demographic, disease severity and clinical factors.
Method
Participants
We used data collected from the pilot and main phases of the Adjustment and Recovery after Cardiac Surgery (ARCS) Study. Participants were recruited from a pre-surgery assessment clinic at St. George's Hospital, London. Inclusion criteria permitted only patients who were undergoing elective CABG surgery or CABG plus valve replacement to participate. CABG surgery was defined to include both on-pump (i.e. cardiopulmonary bypass) and off-pump surgical procedures. In addition, participants had to be able to complete the questionnaires in English and be 18 years or older. The recruitment and retention of participants into the ARCS Study is displayed in Fig. 1. Briefly, out of the 347 participants who completed valid baseline questionnaires, those participants included in these analyses were the 230 CABG surgery patients (mean age, 67.81 ± 9.07 years; 12.2 % females) with complete data for all variables at baseline and follow-up, including covariates. Multiple imputation was not used in these analyses. Compared to the participants who were included in these analyses, the excluded participants were more likely to be female (x 2 = 8.97, p = 0.003) and have a higher European System for Cardiac Operative Risk Evaluation (EuroSCORE) (t = 2.33, p = 0.020). All procedures were carried out with the written consent of the participants. We obtained ethical approval from the South West London research ethics committee.
Study Design
The ARCS study was designed to investigate the causes and consequences of poor emotional adjustment following cardiac surgery and was powered to assess the importance of a broad range of psychological, behavioural and social factors. The ARCS study uses a prospective longitudinal design to track patients during the months after CABG surgery. The baseline assessment took place on average 27 days before patients' surgery (mean = 27.14, standard deviation = 26.66) when participants came to the hospital for their pre-assessment clinic appointment; all participants completed the baseline assessment prior to surgery. The researcher conducted a semi-structured interview with the patient to collect demographic information and the participant was given a postal questionnaire to self-complete at home. The follow-up assessment occurred on average 60 days after surgery (mean = 59.62, standard deviation = 25.47) and was carried out using a postal questionnaire.
Measures
Clinical and Socio-demographic Measures
Cardiovascular history, clinical factors during admission and management were obtained from clinical notes. Clinical risk was assessed using the EuroSCORE [20]. EuroSCORE is a composite measure of procedural mortality risk based on 17 factors comprising patient-related factors (e.g. age, sex), cardiac-related factors (e.g. unstable angina, recent myocardial infarction) and surgery-related factors (e.g. surgery on thoracic aorta). Items were scored in accordance with the “logisitic EuroSCORE” method to generate a percentage mortality risk estimate; further details of the scoring method can be found on the EuroSCORE website (www.euroscore.org/logisticEuroSCORE.htm) [21]. In addition, the number of grafts a participant received and whether they underwent cardiopulmonary bypass (yes/no) were also recorded. Participants detailed their medications prior to surgery and any longstanding illnesses. Patients who reported a sleep disorder (e.g. apnoea) or who were taking any sleep medication were used to create a binary clinical sleep disorder variable. Socio-economic status was assessed using yearly household income on a five-point scale ranging from <£10,000 per year to >£40,000 per year (coded 0–4). Smoking was measured as a binary variable (current smoker/non-smoker). Body mass index (BMI) was assessed at the preoperative clinic appointment and calculated using the standard formula (kilogram per square metre).
Sleep and Mood Factors
Subjective sleep disturbance was assessed at baseline and post-operative follow-up using an adapted version of the Jenkins Sleep Problems Scale [22], a widely used brief self-report instrument, which assesses sleep complaints. This scale has previously been used in sleep studies [23–27] and has been administered in CABG samples [28]. In line with previous work by our colleagues, in addition to the original four-item scale, a fifth item was included: “how often in the past month did you have disturbed or restless sleep?” [24] since this item has been found to be important for cardiac health [13]. Participants respond by estimating the number of days each sleep complaint was experienced during the previous month. Individual item scores range from 0 (not at all) to 5 (22 to 31 days a month) with total scores ranging from 0 to 25, with higher scores indicating greater sleep complaints (baseline Cronbach's α = 0.85; follow-up Cronbach's α = 0.88).
The Beck Depression Inventory (BDI) [29] was used to measure depression symptoms at baseline. We removed items 16 (sleep disturbance) and 17 (fatigue) from the total score throughout these analyses. The remaining 19 items were scored by summing responses (on a scale of 0 to 3), with higher scores indicating greater emotional disturbance (Cronbach's α = 0.83).
The Hospital Anxiety and Depression Scale (HADS) was designed as a self-report, 14-item measure of anxiety and depression for use in outpatient settings [30]. Only the seven-item anxiety scale was utilised in the ARCS study, with questions being answered on a Likert scale ranging from 0 to 3, to indicate the extent to which the symptom had been experienced over the past 2 weeks. Items were summed to generate an overall score, with reverse coding on item 4 and item 5; higher scores indicate greater anxiety (Cronbach's α = 0.84).
Recovery Outcome Measures
The Short Form health survey–12-item (SF-12) [31] was used in this study at baseline and follow-up as a brief measure of mental and physical HRQoL. The SF-12 is comparable to the SF-36 in detecting change across time in longitudinal studies, for both the mental and physical component scores [32]. Responses to the questions were calibrated to give mental and physical HRQoL scores with normative values of 50; scores below 50 are suggestive of poor quality of life.
The Coronary Revascularisation Outcomes Questionnaire (CROQ) [33] was designed to assess quality of life and health outcomes following cardiac surgery. This study used the adverse effects subscale from the version adapted for CABG surgery. Patients were asked to rate the extent to which they had experienced a series of physical symptoms related to their surgery such as bruising, numbness and tingling and swelling, using a five-point Likert scale ranging from 0 (not at all) to 4 (a lot); higher scores indicate greater negative symptoms (Cronbach's α = 0.79).
The McGill Pain Questionnaire–Short Form (MPQ-SF) [34] was developed as a brief version of the standard MPQ and is suitable for use in post-surgical patients. Two scores were calculated: the affective pain score is the sum of the intensity values for the affective descriptor words and the sensory pain score is the sum of the intensity values for the sensory descriptor words. Higher scores indicate greater pain (sensory pain Cronbach's α = 0.90; affective pain Cronbach's α = 0.77).
Statistical Analysis
Paired sample t tests were used to assess changes in measures over time. Hierarchical multiple regression was used to examine the relationship between preoperative sleep complaints and post-operative recovery. The independent variable in analyses was baseline sleep complaints and the dependent variables were physical and mental HRQoL, physical symptom reporting and sensory and affective pain. We included covariates in each model that might potentially relate to the outcomes. Covariates were entered in steps; first we entered age and sex into the models, followed by marital status, BMI, smoking status and household income. Next, we entered clinical sleep disorder, cardiopulmonary bypass, number of grafts and EuroSCORE. Finally, we entered baseline scores on the BDI (items 16 and 17 removed) and the anxiety subscale of the HADS. Baseline SF-12 scores were also entered into the final step of the models predicting follow-up scores on this measure. Preoperative measures of physical symptoms and pain were not collected and so were not included as covariates in models predicting follow-up scores on the CROQ or MPQ-SF. Since removing the participants who reported a sleep disorder from the analyses did not affect the results, these participants were retained in the analyses we report here. Variance inflation factor values were generated for all regression models to assess the assumption of multicollinearity; all were within the acceptable range. All analyses were conducted using SPSS version 21.
Results
Characteristics of the sample at the pre-surgical baseline are summarised in Table 1. The sample had an age range between 22 to 90 years, was predominantly male (87.80 %) and overweight (BMI >25 = 81.70 %). The majority of participants were hypertensive, and approximately one in five patients suffered from diabetes. The majority of participants had on-pump cardiopulmonary bypass surgery in isolation. Participants reported significantly greater sleep complaints after surgery (mean = 10.47, standard deviation = 7.11) than before surgery (mean = 9.52, standard deviation = 7.02; t = −2.15 p = 0.033). The only significant association between baseline sleep complaints and the demographic and clinical variables was with marital status (t = 2.61, p = 0.010), with unmarried participants (mean = 11.70, standard deviation = 7.24) having higher Jenkins total scores at baseline compared to married participants (mean = 8.87, standard deviation = 6.84). Scores on the Jenkins questionnaire were not correlated with the presence of a clinical sleep disorder (r = 0.12, p = 0.078). Baseline sleep complaints were positively associated with both baseline anxiety (r = 0.33, p <0.001) and baseline depression symptoms (r = 0.42, p < 0.001). Interestingly, post-operative physical HRQoL was lower in the patients who had received cardiopulmonary bypass (mean = 34.51, standard deviation = 8.35) compared to those who had not (mean = 38.39, standard deviation = 8.14; t = 2.95, p = 0.004). Similarly, the patients who had received cardiopulmonary bypass (mean = 14.91, standard deviation = 7.57) reported greater physical symptoms following surgery on the CROQ, compared to those who had off-pump surgery (mean = 12.39, standard deviation = 6.91; t = −2.14, p = 0.033).
Mean scores of the dependent variables are displayed in Table 2. Participants reported significantly poorer physical HRQoL on the SF-12 after surgery (mean = 35.37, standard deviation = 8.44) than before surgery (mean = 39.02, standard deviation = 10.83; t = 4.36, p < 0.001). This is consistent with results from cross-sectional correlations between the dependent variables, which revealed that lower physical HRQoL scores at follow-up were correlated with greater sensory pain (r = −0.29, p < 0.001), greater affective pain (r = −0.21, p = 0.001) and greater CROQ physical symptom scores (r = −0.34, p < 0.001). Regression analyses were carried out to assess whether baseline sleep complaints predicted physical HRQoL at follow-up. The results displayed in Table 3 show that baseline total sleep complaints were a significant predictor in the model (t = −2.83, p = 0.005) after controlling for covariates. This is a negative association such that higher preoperative sleep complaint scores were associated with lower physical HRQoL. The only other significant predictors of lower physical HRQoL in the final model were use of cardiopulmonary bypass (t = −3.25, p = 0.001) during surgery and, contrary to our hypothesis, lower EuroSCORE values (t = 2.21, p = 0.028). The complete model accounted for 14.6 % of the variance in post-CABG physical SF-12 scores. Participants reported significantly better mental HRQoL on the SF-12 after surgery (mean = 57.67, standard deviation = 6.87) than before surgery (mean = 56.03, standard deviation = 6.78; t = −3.30, p = 0.001). However, baseline total sleep complaints were not a significant predictor of lower post-operative mental HRQoL (t = −0.57, p = 0.571), with the only significant predictors in this model being greater baseline anxiety (t = −2.18, p = 0.031) and lower mental HRQoL scores (t = 3.40, p = 0.001).
Table 4 displays the regression coefficients for the models predicting post-operative CROQ physical symptoms scores. Baseline total sleep complaints were a significant predictor of greater physical symptoms (t = 2.90, p = 0.004) independent of covariates. The other significant predictors in the final model were female sex (t = 2.23, p = 0.027), lower household income (t = −2.35, p = 0.020), greater number of grafts (t = 3.25, p = 0.001) and use of cardiopulmonary bypass (t = 2.96, p = 0.003). The complete model accounted for 21.2 % of the variance.
Table 5 shows the regression analyses using baseline sleep complaint scores to predict sensory pain at follow-up. The results show that greater total preoperative sleep complaints (t = 2.28, p = 0.024) were a significant predictor of high sensory pain scores after surgery, independent of covariates. Lower income (t = −2.27, p = 0.024), higher BMI (t = 2.17, p = 0.031) and higher anxiety (t = 2.26, p = 0.025) at baseline were all also significant predictors in the final model. The final model accounted for 15.4 % of the variance. Baseline sleep complaints were not a significant predictor of post-operative affective pain (t = 1.36, p = 0.176), with the only significant predictor in this model being baseline anxiety (t = 3.87, p < 0.001).
Discussion
In the present study, we examined the associations between self-rated sleep complaints in the month prior to CABG surgery with physical and emotional recovery in the 2 months following surgery. The main findings of this study were that greater sleep complaints before surgery were associated with poorer physical HRQoL, greater physical symptoms and greater sensory pain after CABG surgery independently of baseline mood, disease severity and demographic factors. Baseline sleep was not associated with emotional HRQoL or affective pain following surgery, after controlling for covariates. Baseline depression symptoms were not a significant predictor of recovery in any of the models. However, greater preoperative anxiety was a significant predictor of greater post-operative mental HRQoL and sensory and affective pain.
A number of studies have shown improvements to HRQoL following CABG surgery [35–38]. However, in our study, we reported an overall decrease in physical HRQoL from preoperative to 2-month post-operative values. The reason for the discrepancy between our data and previous studies is not entirely clear, though is potentially due to differences concerning the study method. For example, differences in participant demographic and disease severity and the timing of quality of life assessments are all likely to be contributing factors. The fact that our participants reported an overall decline in physical HRQoL at follow-up was consistent with the pain and physical symptom data, suggesting that participants were still in an active stage of physical recovery 2 months following surgery. While we report a decline in mean physical HRQoL over time (39.02 pre-CABG to 35.37 post-CABG), the scores are not dissimilar to scores reported by other authors investigating HRQoL in CABG patients. Thomson and colleagues [39] reported a mean pre-CABG physical SF-12 score of 30.45 and a 4-month post-CABG score of 41.47, and Lie and colleagues [40] reported a mean physical SF-36 score of 38.6 before surgery and 40.9 six weeks after surgery. These figures can be seen to reflect reduced physical HRQoL in this patient group when viewed in light of UK population norms on the physical component of the SF-12 of between 36.48 and 48.80 for >45 year olds [41].
Our findings are in line with the results from Hunt and colleagues [16] and Redeker and colleagues [17] who reported cross-sectional associations between poor sleep quality and worsened quality of life after CABG. The results from our study were prospective in that greater sleep complaints prior to surgery were associated with poorer physical recovery following surgery. Poor sleep is also thought to be closely linked to emotional well-being. For example, Edéll-Gustafsson and Hetta [18] found that those CABG patients reporting greater anxiety were more prone to sleep disturbance. We found that baseline sleep complaints and anxiety were associated at baseline, but that in regression models Jenkins total scores were a significant independent predictor of physical HRQoL and physical symptom reporting even after controlling for anxiety. Anxiety and sleep complaints were both significant predictors of sensory pain following surgery. In addition, research has shown an association between poor sleep quality and depression [42, 43]. Depressive symptoms after CABG have been shown to be associated with a host of poorer outcomes including increased risk of graft disease progression [44], greater hospital readmissions [45], poorer functional recovery such as shorter walking distances [46] and poorer physical recovery including more infections, impaired wound healing [46, 47] and greater pain [48]. However, we found no evidence for preoperative depression being associated with short-term post-operative recovery, suggesting sleep quality exerted independent effects on CABG outcomes. Additionally, we controlled for the possible influence of sleep medication and history of sleep disorders in our analyses, with the effect of sleep complaints on physical recovery remaining.
Possible alternative pathways linking sleep complaints with CABG recovery include the role the neuroendocrine system and, in particular, cortisol [49]. Changes to the neuroendocrine system have been observed after sleep loss, although the findings are inconsistent, with some studies reporting a slight elevation in cortisol in response to sleep deprivation [50, 51], while others have reported no changes or even small decrements in cortisol levels [52, 53]. Modulation of cortisol responses may have particular importance as greater cortisol output has been associated with slower wound healing [54, 55]. In addition, sleep deprivation or disruption may act as a stressor, leading to increased sympathetic nervous system activation. If sleep recovery is insufficient, these effects have been shown to continue, with studies showing persistent elevated heart rate and blood pressure [56, 57]. Other mechanisms are also likely to be involved, such as dysregulation of inflammatory responses [58, 59]; this is likely to be particularly salient in CABG patients since the surgical procedure itself is known to be associated with an acute inflammatory response [60]. Impaired behavioural adaptation may also be at play, with the link between poor sleep and poor quality of life potentially attributable to a host of health behaviours. We were able to adjust for smoking and BMI in our analyses, still demonstrating an independent effect of sleep complaints on poor recovery; however, other health behaviours such as physical inactivity and alcohol consumption may also be important. These biological and behavioural pathways warrant future investigation in sleep studies in cardiac patients. Other, non-causal, pathways should also be borne in mind. For example, since sleep disorders were self-reported, it cannot be entirely ruled out that undiagnosed sleep apnoea was not responsible for the reported association between sleep complaints and recovery.
The timing of the follow-up assessment is likely to affect how well the results can predict long-term prognosis. For example, Hedner and colleagues [61] assessed sleep in over 1,200 individuals prior to CABG surgery and 1 year following surgery, and reported that baseline sleep disturbance was not generally associated with survival at 5-year follow-up. This study has shown baseline sleep complaints to be associated with short-term differences in recovery; however, we do not know to what extent these effects would be maintained in the longer term or the impact of sleep complaints on mortality risk. Future work is needed to address these issues.
Sleep measurement is also likely to be important in studies of this type. Marked discrepancies have been observed between subjective and objective measures of sleep [62–65], with self-rated sleep being modulated by psychosocial characteristics and affect [26]. As with other self-report measures, questionnaire measures of sleep disturbance are likely to be subject to recall bias. However, since the baseline assessment occurred on average a month prior to participants' surgery, it is unlikely that acute sleep disturbance in anticipation of the operation affected participants' responses on this measure. In addition, it should be noted that the Jenkins Sleep Problems Scale that we utilised here has not previously been validated against objective measures of sleep disturbance such as polysomnography, and thus our observations are restricted to the subjective experience of sleep.
Our study had a number of strengths. We used a longitudinal design so were able to demonstrate a prospective relationship from pre- to post-operative periods. In addition, we included a large number of demographic and clinical covariates in our analyses and a wide range of recovery outcome measures, showing sleep complaints to have independent effects on several different markers of physical recovery. However, our sample was restricted to elective surgery participants and therefore does not capture the full range of disease severity and co-morbidities that may be apparent in patients undergoing cardiac surgery. Attrition is another limitation of our study, since female participants and those with higher EuroSCOREs were more likely to be excluded from our analyses; we endeavoured to address this issue by controlling for these variables in all analyses, but care must be taken when generalising our results to the wider CABG population. Reverse causality should also be borne in mind given that we did not measure pain and physical symptoms on the CROQ preoperatively, since these measures were focused on experiences following surgery. It is conceivable that preoperative physical symptoms contributed to the preoperative poor sleep of some patients. In addition, we used self-report measures of sleep and this may be influenced by negative affectivity [26]. We tried to overcome this by controlling for anxiety and depressive symptoms in our regression models and indeed the associations between poor sleep and recovery remained significant even after these adjustments. While we identified preoperative sleep complaints as a significant predictor of poorer recovery, other factors that were not taken into consideration in these analyses are also likely to be at play given the total variance explained across our models varied from between 14.6 and 21.2 %. Our findings have important clinical implications, suggesting that interventions to target sleep quality prior to surgery could have beneficial effects on several aspects of physical recovery following surgery.
In conclusion, our findings suggest greater sleep complaints before surgery may partly explain why some patients fail to show improvements in physical adjustment after CABG surgery. Future work would benefit from both objective and subjective measures of sleep and larger sample sizes for the exploration of biological pathways to delineate the causal mechanisms by which sleep can affect recovery in cardiac surgery patients.
References
Hawkes AL, Mortensen OS. Up to one third of individual cardiac patients have a decline in quality of life post-intervention. Scand Cardiovasc J. 2006; 40(4): 214-218.
Covinsky KE, Lin F, Bittner V, Hlatky MA, Knight SJ, Vittinghoff E. Health-related quality of life following coronary artery bypass graft surgery in post-menopausal women. J Gen Intern Med. 2008; 23(9): 1429-1434.
Moore SM. A comparison of women's and men's symptoms during home recovery after coronary artery bypass surgery. Heart Lung. 1995; 24(6): 495-501.
Parry M, Watt-Watson J, Hodnett E, Tranmer J, Dennis C-L, Brooks D. Pain experiences of men and women after coronary artery bypass graft surgery. J Cardiovasc Nurs. 2010; 25(3): E9-E15.
Zimmerman L, Barnason S, Young L, Tu C, Schulz P, Abbott AA. Symptom profiles of coronary artery bypass surgery patients at risk for poor functioning outcomes. J Cardiovasc Nurs. 2010; 25(4): 292-300.
Leineweber C, Kecklund G, Janszky I, Akerstedt T, Orth-Gomér K. Poor sleep increases the prospective risk for recurrent events in middle-aged women with coronary disease. The Stockholm Female Coronary Risk Study. J Psychosom Res. 2003; 54(2): 121-127.
Sabanayagam C, Shankar A. Sleep duration and cardiovascular disease: Results from the National Health Interview Survey. Sleep. 2010; 33(8): 1037-1042.
Schwartz SW, Cornoni-Huntley J, Cole SR, Hays JC, Blazer DG, Schocken DD. Are sleep complaints an independent risk factor for myocardial infarction? Ann Epidemiol. 1998; 8(6): 384-392.
Cappuccio FP, Cooper D, D'Elia L, Strazzullo P, Miller MA. Sleep duration predicts cardiovascular outcomes: A systematic review and meta-analysis of prospective studies. Eur Heart J. 2011; 32(12): 1484-1492.
Eaker ED, Pinsky J, Castelli WP. Myocardial infarction and coronary death among women: Psychosocial predictors from a 20-year follow-up of women in the Framingham Study. Am J Epidemiol. 1992; 135(8): 854-864.
Mallon L, Broman JE, Hetta J. Sleep complaints predict coronary artery disease mortality in males: A 12-year follow-up study of a middle-aged Swedish population. J Intern Med. 2002; 251(3): 207-216.
Nilsson PM, Nilsson JA, Hedblad B, Berglund G. Sleep disturbance in association with elevated pulse rate for prediction of mortality—consequences of mental strain? J Intern Med. 2001; 250(6): 521-529.
Chandola T, Ferrie JE, Perski A, Akbaraly T, Marmot MG. The effect of short sleep duration on coronary heart disease risk is greatest among those with sleep disturbance: A prospective study from the Whitehall II cohort. Sleep. 2010; 33(6): 739-744.
Jenkins CD, Jono RT, Stanton BA. Predicting completeness of symptom relief after major heart surgery. Behav Med. 1996; 22(2): 45-57.
Redeker NS, Hedges C. Sleep during hospitalization and recovery after cardiac surgery. J Cardiovasc Nurs. 2002; 17(1): 56-68. quiz 82–83.
Hunt JO, Hendrata MV, Myles PS. Quality of life 12 months after coronary artery bypass graft surgery. Heart Lung. 2000; 29(6): 401-411.
Redeker NS, Ruggiero JS, Hedges C. Sleep is related to physical function and emotional well-being after cardiac surgery. Nurs Res. 2004; 53(3): 154-162.
Edéll-Gustafsson UM, Hetta JE. Anxiety, depression and sleep in male patients undergoing coronary artery bypass surgery. Scand J Caring Sci. 1999; 13(2): 137-143.
Blumenthal JA, Lett HS, Babyak MA, et al. Depression as a risk factor for mortality after coronary artery bypass surgery. Lancet. 2003; 362(9384): 604-609.
Roques F, Michel P, Goldstone AR, Nashef SAM. The logistic EuroSCORE. Eur Heart J. 2003; 24(9): 881-882.
Goldstone T. How to calculate the logistic EuroSCORE [Internet]. euroSCORE.org. [cited 2013 Apr 19]. Available from: http://www.euroscore.org/logisticEuroSCORE.htm
Jenkins CD, Stanton BA, Niemcryk SJ, Rose RM. A scale for the estimation of sleep problems in clinical research. J Clin Epidemiol. 1988; 41(4): 313-321.
Steptoe A, O'Donnell K, Marmot M, Wardle J. Positive affect, psychological well-being, and good sleep. J Psychosom Res. 2008; 64(4): 409-415.
Kumari M, Badrick E, Ferrie J, Perski A, Marmot M, Chandola T. Self-reported sleep duration and sleep disturbance are independently associated with cortisol secretion in the Whitehall II study. J Clin Endocrinol Metab. 2009; 94(12): 4801-4809.
Kudielka BM, Von Känel R, Gander M-L, Fischer JE. Effort–reward imbalance, overcommitment and sleep in a working population. Work & Stress. 2004; 18(2): 167-178.
Jackowska M, Dockray S, Hendrickx H, Steptoe A. Psychosocial factors and sleep efficiency: Discrepancies between subjective and objective evaluations of sleep. Psychosom Med. 2011; 73(9): 810-816.
Lyytikäinen P, Lallukka T, Lahelma E, Rahkonen O. Sleep problems and major weight gain: A follow-up study. Int J Obes (Lond). 2011; 35(1): 109-114.
Jenkins CD, Stanton BA, Jono RT. Quantifying and predicting recovery after heart surgery. Psychosom Med. 1994; 56(3): 203-212.
Beck AT, Steer RA, Carbin MG. Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clin Psychol Rev. 1988; 8(1): 77-100.
Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983; 67(6): 361-370.
Ware J, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: Construction of scales and preliminary tests of reliability and validity. Med Care. 1996; 34(3): 220-233.
Jenkinson C, Layte R, Jenkinson D, et al. A shorter form health survey: Can the SF-12 replicate results from the SF-36 in longitudinal studies? Journal of Public Health. 1997; 19(2): 179-186.
Schroter S, Lamping DL. Coronary Revascularisation oOutcome Questionnaire (CROQ): Development and validation of a new, patient based measure of outcome in coronary bypass surgery and angioplasty. Br Med J. 2004; 90(12): 1460.
Melzack R. The short-form McGill pain questionnaire. Pain. 1987; 30(2): 191-197.
Hokkanen M, Järvinen O, Huhtala H, Tarkka MR. A 12-year follow-up on the changes in health-related quality of life after coronary artery bypass graft surgery. Eur J Cardiothorac Surg. 2013. doi:10.1093/ejcts/ezt358
Peric V, Borzanovic M, Stolic R, et al. Predictors of worsening of patients' quality of life six months after coronary artery bypass surgery. J Card Surg. 2008; 23(6): 648-654.
Cheng DC, Bainbridge D, Martin JE, Novick RJ. Evidence-Based Perioperative Clinical Outcomes Research Group. Does off-pump coronary artery bypass reduce mortality, morbidity, and resource utilization when compared with conventional coronary artery bypass? A meta-analysis of randomized trials. Anesthesiology. 2005; 102(1): 188-203.
Jokinen JJ, Hippeläinen MJ, Turpeinen AK, Pitkänen O, Hartikainen JEK. Health-related quality of life after coronary artery bypass grafting: A review of randomized controlled trials. J Card Surg. 2010; 25(3): 309-317.
Thomson P, Niven CA, Peck DF, Eaves J. Patients' and partners' health-related quality of life before and 4 months after coronary artery bypass grafting surgery. BMC Nurs. 2013; 12(1): 16.
Lie I, Arnesen H, Sandvik L, Hamilton G, Bunch EH. Health-related quality of life after coronary artery bypass grafting. The impact of a randomised controlled home-based intervention program. Qual Life Res. 2009; 18(2): 201-207.
Jenkinson C, Chandola T, Coulter A, Bruster S. An assessment of the construct validity of the SF–12 summary scores across ethnic groups. J Public Health. 2001; 23(3): 187-194.
Almeida OP, Alfonso H, Yeap BB, Hankey G, Flicker L. Complaints of difficulty to fall asleep increase the risk of depression in later life: The health in men study. J Affect Disord [Internet]. 2011 [cited 2011 Jun 27]; Available from: http://www.ncbi.nlm.nih.gov/pubmed/21680026
Benca RM, Obermeyer WH, Thisted RA, Gillin JC. Sleep and psychiatric disorders. A meta-analysis. Arch Gen Psychiatry. 1992; 49(8): 651-668. discussion 669–670.
Wellenius GA, Mukamal KJ, Kulshreshtha A, Asonganyi S, Mittleman MA. Depressive symptoms and the risk of atherosclerotic progression among patients with coronary artery bypass grafts. Circulation. 2008; 117(18): 2313-2319.
Tully PJ, Baker RA, Turnbull D, Winefield H. The role of depression and anxiety symptoms in hospital readmissions after cardiac surgery. J Behav Med. 2008; 31(4): 281-290.
Doering LV, Moser DK, Lemankiewicz W, Luper C, Khan S. Depression, healing, and recovery from coronary artery bypass surgery. Am J Crit Care. 2005; 14(4): 316-324.
Doering LV, Martínez-Maza O, Vredevoe DL, Cowan MJ. Relation of depression, natural killer cell function, and infections after coronary artery bypass in women. Eur J Cardiovasc Nurs. 2008; 7(1): 52-58.
Morone NE, Weiner DK, Belnap BH, et al. The impact of pain and depression on recovery after coronary artery bypass grafting. Psychosom Med. 2010; 72(7): 620-625.
Meerlo P, Sgoifo A, Suchecki D. Restricted and disrupted sleep: Effects on autonomic function, neuroendocrine stress systems and stress responsivity. Sleep Med Rev. 2008; 12(3): 197-210.
Chapotot F, Buguet A, Gronfier C, Brandenberger G. Hypothalamo-pituitary-adrenal axis activity is related to the level of central arousal: Effect of sleep deprivation on the association of high-frequency waking electroencephalogram with cortisol release. Neuroendocrinology. 2001; 73(5): 312-321.
Spiegel K, Leproult R, Van Cauter E. Impact of sleep debt on metabolic and endocrine function. Lancet. 1999; 354(9188): 1435-1439.
Akerstedt T, Palmblad J, de la Torre B, Marana R, Gillberg M. Adrenocortical and gonadal steroids during sleep deprivation. Sleep. 1980; 3(1): 23-30.
Follenius M, Brandenberger G, Bandesapt JJ, Libert JP, Ehrhart J. Nocturnal cortisol release in relation to sleep structure. Sleep. 1992; 15(1): 21-27.
Ebrecht M, Hextall J, Kirtley L-G, Taylor A, Dyson M, Weinman J. Perceived stress and cortisol levels predict speed of wound healing in healthy male adults. Psychoneuroendocrinology. 2004; 29(6): 798-809.
Vedhara K, Miles JNV, Wetherell MA, et al. Coping style and depression influence the healing of diabetic foot ulcers: Observational and mechanistic evidence. Diabetologia. 2010; 53(8): 1590-1598.
Lusardi P, Mugellini A, Preti P, Zoppi A, Derosa G, Fogari R. Effects of a restricted sleep regimen on ambulatory blood pressure monitoring in normotensive subjects. Am J Hypertens. 1996; 9(5): 503-505.
Tochikubo O, Ikeda A, Miyajima E, Ishii M. Effects of insufficient sleep on blood pressure monitored by a new multibiomedical recorder. Hypertension. 1996; 27(6): 1318-1324.
Ferrie JE, Kivimäki M, Akbaraly TN, Singh-Manoux A, Miller MA, Gimeno D, et al. Associations between change in sleep duration and inflammation: Findings on C-reactive protein and interleukin 6 in the Whitehall II Study. Am J Epidemiol. 2013; 178(6):956-961
Prather AA, Epel ES, Cohen BE, Neylan TC, Whooley MA. Gender differences in the prospective associations of self-reported sleep quality with biomarkers of systemic inflammation and coagulation: Findings from the Heart and Soul Study. J Psychiatr Res. 2013; 47(9): 1228-1235.
Ascione R, Lloyd CT, Underwood MJ, Lotto AA, Pitsis AA, Angelini GD. Inflammatory response after coronary revascularization with or without cardiopulmonary bypass. Ann Thorac Surg. 2000; 69(4): 1198-1204.
Hedner J, Caidahl K, Sjöland H, Karlsson T, Herlitz J. Sleep habits and their association with mortality during 5-year follow-up after coronary artery bypass surgery. Acta Cardiol. 2002; 57(5): 341-348.
Fernandez-Mendoza J, Calhoun SL, Bixler EO, et al. Sleep misperception and chronic insomnia in the general population: Role of objective sleep duration and psychological profiles. Psychosom Med. 2011; 73(1): 88-97.
Lauderdale DS, Knutson KL, Yan LL, Liu K, Rathouz PJ. Self-reported and measured sleep duration: How similar are they? Epidemiology. 2008; 19(6): 838-845.
Silva GE, Goodwin JL, Sherrill DL, et al. Relationship between reported and measured sleep times: The Sleep Heart Health Study (SHHS). J Clin Sleep Med. 2007; 3(6): 622-630.
Van Den Berg JF, Van Rooij FJA, Vos H, et al. Disagreement between subjective and actigraphic measures of sleep duration in a population-based study of elderly persons. J Sleep Res. 2008; 17(3): 295-302.
Acknowledgments
This research was funded by the British Heart Foundation.
Conflict of Interest
The authors have no conflict of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Poole, L., Kidd, T., Leigh, E. et al. Preoperative Sleep Complaints Are Associated with Poor Physical Recovery in the Months Following Cardiac Surgery. ann. behav. med. 47, 347–357 (2014). https://doi.org/10.1007/s12160-013-9557-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12160-013-9557-8