Abstract
Background
Prayer is often used to cope with racism-related stress. Little is known about its impact on cardiovascular function.
Purpose
This study examined how prayer coping relates to cardiovascular reactivity (CVR), post-stress recovery, and affective reactivity in response to racism-related stress.
Methods
African American women (n = 81; mean age=20 years) reported their use of prayer coping on the Perceived Racism Scale and completed anger recall and racism recall tasks while undergoing monitoring of systolic and diastolic blood pressure (DBP), heart rate, heart rate variability (HRV), and hemodynamic measures. Prayer coping was examined for associations with CVR, recovery, and affective change scores using general linear models with repeated measures.
Results
Higher prayer coping was associated with decreased state stress and DBP reactivity during racism recall (p's < 0.05) and with decreased DBP and increased HRV during racism recall recovery(p's < 0.05).
Conclusions
Coping with racism by utilizing prayer may have cardiovascular benefits for African American women.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The adverse effects of stress on the cardiovascular system are well documented [1]. Adaptive and maladaptive strategies used by individuals to cope with stressors can either attenuate or augment the negative impact of stress on cardiovascular health [1]. Research has been emerging on spirituality/religiosity as a potential buffer against the negative impact of stress on physical health [2–4]. Higher levels of spirituality/religiosity have been associated with favorable levels of cardiovascular parameters at rest and during exposure to mental stress [5–12], though not consistently [4, 13, 14]. A review of religiosity/spirituality and health suggested that more attention should be given to specific practices, such as prayer [15].
In light of its suggested association with reduced sympathetic nervous system activity [16], prayer may be particularly relevant to the sympathetically mediated increases in blood pressure that are observed in studies of cardiovascular reactivity (CVR) to mental stressors [17]. Longitudinal studies have linked CVR and prolonged elevations after stress exposure to hypertension and atherosclerosis [17]. Research on prayer and cardiovascular health has produced mixed results and has largely focused on general frequency of prayer during a specified time interval rather than stressor-specific coping behavior [16, 18–22]. Prayer has been linked to lower blood pressure [18], enhanced heart rate variability (HRV) [19], and lower cardiovascular disease (CVD) [20]. Only two studies of prayer and cardiovascular health have reported data on African Americans [18, 21], with no studies reporting such data specifically for African American women.
African American women have disproportionately high rates of premature CVD [23, 24]. One contributor to these high rates of CVD in African American women may be racism-related stress, given the links between stress and CVD [1] and the research linking racism/racial discrimination to higher blood pressure, hypertension, and subclinical coronary heart disease [25–27].
Among African Americans, particularly African American women, prayer is often used when coping with stressful situations [28–30], including experiences of perceived racism [30, 31]. Perceived racism can be a source of stress that often produces negative emotions (e.g., anxiety), particularly anger [32]. Research has emerged examining how individuals cope with racism-related stress [25, 26, 30]. However, little is known about the impact of specific coping strategies, such as prayer, on cardiovascular function during exposure to racism-related stress.
In an effort to increase understanding of context-specific strategies of coping with stressors [33] that may mitigate adverse effects on cardiovascular health, this study examined how prayer coping relates to CVR, post-stress recovery, and negative affect in response to racism-related stress. It was hypothesized that the use of prayer in coping with racism would be associated with reduced subjective stress accompanied by a less adverse cardiovascular response when exposed to a racism-related stress task. Negative state affect during experimental tasks was explored for mediating or moderating effects on associations observed between prayer coping and cardiovascular responses.
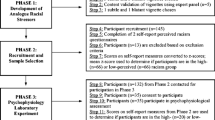
Methods
Participants
The sample included 81 non-smoking, healthy, African American (self-identified, with two parents of African descent) women, who were undergraduate and graduate students of a predominantly White mid-Atlantic state university. The majority were lifelong U.S. residents. Approximately 9 % of the sample (n = 7) had spent ≥50 % of their lives outside of the U.S. in African (n = 5), European (n = 1), or Caribbean (n = 1) countries, but all had been in the U.S. ≥2 years.
Volunteers were recruited on campus through classes, organizations, and advertisements to participate in a "Cardiovascular Study of Stress in African American Women." The target age range was between 18 and 30 years old in order to control for cohort effects and to obtain a healthier sample with a relatively homogeneous level of cardiovascular risk. Study exclusions were hypertension (i.e., blood pressure ≥140/90 mmHg) and moderate to extreme obesity [body mass index (BMI) ≥34.9 kg/m2], as well as self-reported history of CVD, diabetes, and any other major chronic medical or psychiatric illnesses; smoking, current pregnancy, usage of cardioactive medications, and consumption of >14 alcohol drinks per week. Written informed consent was obtained as directed by the university's Institutional Review Board. All participants earned 20 dollars, while eligible students also earned extra credit points.
Procedures
After affirming their adherence to the required 12-h avoidance of caffeine and alcohol, participants' were measured to confirm that they met the inclusion criteria for BMI. They then provided data on their menstrual cycle and use of oral contraceptives. In preparation for the recall tasks, participants were asked to identify two experiences from their personal lives: (1) a general anger-evoking experience that the participant deemed to be non-racial (for an anger recall task) and (2) a racially based experience that the participant perceived as racial mistreatment/disrespect (for a racism recall task). To ensure that both experiences had sufficient emotional potency for the participants, ratings of how angry/upset they were during each experience had to be ≥4 on a scale of 0 to 10 (0 = "not at all" to 10 = "extremely so") using one-item screenings created for this purpose.
Participants were then hooked up to cardiovascular monitoring equipment in a temperature-controlled, sound-attenuated experimental room, where they were left alone in the room to rest quietly for 15 min while seated with legs uncrossed in a comfortable chair. Following the rest period, an African American female experimenter re-entered the room to engage the participant in the following 3-min experimental tasks: anger recall, racism recall, and neutral speaking (all of which were counterbalanced, tape-recorded, and preceded by 1 min of preparation time). (Note: The neutral speaking task was not analyzed in the current study, because it was not intended to elicit a substantive cardiovascular or emotional response). After each stress task, the experimenter left participants alone in the room for 5 min of post-stress recovery and a 5-min rest period, before returning to administer an assessment of state affect in response to the most recently completed experimental task. Once the cardiovascular monitoring equipment was removed, participants completed a series of psychosocial questionnaires, then were debriefed and compensated.
Experimental Tasks
Anger Recall Task
Often used in laboratory studies of anger, we modified the instructions used in Waldstein et al. [34] to ask participants to give a detailed account of a non-racial personal experience in which they felt angry, irritated, annoyed, or upset. After being allowed 1 min to mentally prepare, they spoke for 3 min as they "re-lived" the details of their anger-evoking experience. Prompts selected from a designated list were provided to elicit a full 3 min of speech, if needed.
Racism Recall Task
Adapted from the anger recall task, a racism recall task was developed for this study to tap into feelings evoked by "re-living" a past personal experience of mistreatment or disrespect that participants attributed to racism. After 1 min of mental preparation, participants discussed the details of their racism experience for 3 min. Prompts selected from a designated list were given if needed to help the participant sustain three full minutes of speech.
[The protocol also included a 3-min neutral speaking task, which involved participants reading aloud from an article about the solar system in order to provide an emotionally neutral contrast to the emotionally charged anger and racism recall tasks. It was excluded from the current analyses on racism-related prayer coping.]
Measures
Predictor Variable—Prayer Coping
Perceived Racism Scale (PRS): Prayer Coping
The PRS examines multiple dimensions of perceived racism (e.g., coping, frequency) in African Americans [35]. It assesses prayer as a behavioral/coping response by asking respondents how they "generally deal" with exposure to racism across four domains: (1) racism-related statements; (2) racism experienced at work; (3) racism experienced at school; and (4) racism experienced in public. Scores for endorsements of prayer coping were summed across the four domains for a total score ranging from 0 to 4. [PRS scores for perceived racism frequency are included for descriptive purposes only and were not analyzed.) The PRS has demonstrated good validity and adequate test–retest reliability [28, 35–37]. Internal consistency of PRS-Prayer Coping in the current study was good with a Cronbach alpha coefficient of 0.86.
Dependent Variables: CVR and Post-stress Recovery
Prayer coping was examined for associations with CVR and post-stress recovery change scores of systolic and diastolic blood pressure (SBP, DBP), heart rate (HR), cardiac pre-ejection period (PEP), cardiac index (CI) (i.e., cardiac output or CO adjusted for body size), stroke index (SI) (i.e., stroke volume (SV) adjusted for body size), total peripheral resistance (TPR), and HRV.
In response to stress, SBP, DBP, and HR usually increase and HRV decreases. African Americans often exhibit a vascular (versus cardiac) reactivity pattern, with SBP, DBP, and HR stress responses showing an underlying hemodynamic pattern of greatly increased TPR and small-to-moderate declines in PEP, CO, and SV [38]. PEP varies inversely with degree of sympathetic activation (i.e., shorter PEP indicates greater sympathetic arousal) of the heart, while reduced HRV reflects reduced parasympathetic cardiac control and/or increased sympathetic activation. The volume of blood pumped from the left ventricle is a positive indicator of cardiac function, as measured by SV (i.e., blood volume pumped with each heartbeat) and CO (blood volume pumped per minute). Increased TPR (i.e., total resistance to blood flow) reflects vasoconstriction [38].
Data were collected as follows. SBP and DBP were assessed oscillometrically (cuff on non-dominant arm) with a Dinamap Vital Signs Monitor [model 8100; Critikon (Johnson & Johnson), Tampa, FL] at 60-s intervals. HR measurements were obtained from an electrocardiogram (ECG) with two electrodes attached bilaterally to the chest. Heart sounds were detected with a Hewlett-Packard Contract Transducer (Model # 21050A) positioned at the second intercostal space on the left sternal border. Grass biological amplifiers provided filtering and amplification of ECG and heart sound signals. Non-invasive estimates of PEP, CO, SV, and TPR were derived using cardiovascular signals from ECG, heart sounds, dZ/dt (first derivative of the change in thoracic impedance), and Zo (basal thoracic impedance) [IFM Minnesota Impedance Cardiograph, model 304B], with a tetrapolar band-electrode configuration [39]. Signals were acquired continuously using computerized analog-to-digital conversion at a rate of 1,000 samples per second [40].
HRV data were obtained with an Ambulatory Monitoring System (version 4.4, TD-FPP, Vrije Universiteit, Amsterdam, The Netherlands), as previously described [41]. Using a three-electrode configuration, the device records the time in milliseconds of raw R-wave inter-beat intervals from the ECG and derives root mean square of successive differences (rMSSD) of inter-beat intervals. The rMSSD is a reliable index of cardiac parasympathetic influences and is recommended as a measure of vagally mediated HRV [42].
Dependent Variables: Affective Reactivity to Recall Tasks
The association between prayer coping and affective reactivity was examined using separate reactivity change scores for state: (1) anger, (2) anxiety, and (3) stress. To assess state affect during the baseline and task periods, participants completed the state portion of the Spielberger State-Trait Personality Inventory [43]. It had been modified to ask respondents how they "felt" (rather than "feel") during the respective period and to include one additional item that assessed state stress ("I felt stressed"). Responses to the state anger and anxiety subscales (ten items each), along with the added stress item, were on a four-point scale (1: "not at all" to 4: "very much so"). Higher change scores indicated higher affective responses to tasks.
Covariate Measures
In addition to cardiovascular/affective baselines, analyses were adjusted for biomedical and psychosocial confounders, which were measured as described below.
Cardiovascular/Affective Baselines
Mean resting baseline levels of cardiovascular and affective parameters were covariates due to their influences on analyses of CVR with post-stress recovery and affective reactivity, respectively [38].
Biomedical
Self-reported data on oral contraceptive use and menstrual cycle were collected due to research linking both factors to CVR and affective responses [44, 45]. After weight was assessed on a calibrated scale, BMI was calculated as weight (kilograms) divided by height (meters squared).
Psychosocial: Chronic Stress
In light of the links between chronic stress and cardiovascular outcomes [1], perceived chronic stress was considered a potential confounder in the current analyses of responses to experimental stressors. The 14-item Perceived Stress Scale was administered to assess how frequently during the past month respondents felt that their lives were unpredictable, uncontrollable, or overloaded, using a five-point Likert scale (0: "never" to 4: "very often") [46]. This global measure of perceived stress assesses various sources of chronic stress (e.g., ongoing life circumstances, expectations about future events, reactions to specific events). Higher scores indicate higher chronic stress.
Psychosocial: Anger Coping
Individuals may cope with anger-provoking experiences (e.g., perceived racism) using approaches other than prayer. Given the literature linking anger coping style with cardiovascular outcomes [47, 48], the Anger-In, Anger-Out, and Anger-Control subscales of the widely used Speilberger Anger Expression Inventory [49] were examined as potential confounders in the current analyses. Each of the eight-item subscales assesses respondents' habitual efforts to inhibit (Anger-In), express outwardly (Anger-Out), or control anger (Anger-Control) as personality traits using a four-point scale (1: "almost never" to 4: "almost always"). Higher scores indicate higher levels of the particular anger coping style.
Exploratory Mediator or Moderator Variable: Task-Related Negative Affect
Task-Related Negative Affect
The emotional responses to the recall tasks (i.e., manipulation checks) could mediate or moderate the association [50] between prayer coping and cardiovascular responses. Using data collected from a modified Spielberger State-Trait Personality Inventory [43] (see Dependent Variables: Affective Reactivity), total negative affect was computed by summing scores for state anger, anxiety, and stress during the anger recall and racism recall. Higher scores indicated higher negative affect.
Data Analyses
Data Reduction
Averages of baseline, stress task, and post-stress recovery periods were computed for SBP, DBP, HR, PEP, CI, SI, TPR, and HRV. CVR change (or delta) scores were calculated as mean stress task scores minus mean baseline scores to represent an index of recall task-induced changes. Change scores for post-stress recovery relative to pre-stress (baseline) levels were calculated (mean recovery score minus mean baseline score) to evaluate the degree to which cardiovascular parameters return to baseline levels [51].
The calculations for CVR change scores used the average of readings from the rest period immediately preceding the task as the mean baseline. The mean baselines for SBP and DBP were computed as the average of the last four SBP and DBP readings of the respective rest period. The mean baselines for HR, PEP, CI, SI, TPR, and HRV were based on averages of continuous measures obtained during the respective rest period.
Mean task and post-stress recovery levels were calculated for SBP and DBP by averaging the four readings taken during each task and the five readings taken during each recovery, respectively. For HRV, HR, PEP, CI, SI, and TPR, mean task and recovery levels were derived from continuous measures throughout the task and recovery periods. A customized program for time domain analyses [41] produced averaged (30-s intervals) measures of rMSSD (i.e., HRV), as well as HR. Custom software for impedance data [39] was used to derive mean task and post-recovery levels of PEP, CI, SI, and TPR.
For these impedance data, software [39] was used to ensemble-average (synchronized averaging of ECG and dZ/dt signals over consecutive cardiac cycles) and score continuous ECG and impedance waveforms in 30-s intervals for the last 6 min of baseline and for the entire task and post-stress recovery periods. The systolic time intervals of PEP and left ventricular ejection time were coded in milliseconds using the intervals of the Q-wave of the digitized ECG to the B-point of the dZ/dt waveform and the B-point to X-wave of the dZ/dT waveform (i.e., coincident with the closure of the aortic valve—the second heart sound). Using a fixed value of 135 ohm*cm to estimate blood resistivity (rho), SV was calculated based on the Kubicek equation [52]: SV = [rho (L/Z0)2 × left ventricular ejection time × dZ/dt (max)]. CO and TPR were calculated as [CO = (HR × SV)/1,000] and [TPR = (mean arterial pressure/CO) × 80]. To adjust for differences in participants' body sizes, CO and SV were divided by body surface area [weight (kg).425 × height (cm).725 × 0.007184] to produce CI and SI, respectively [39].
For affective reactivity, change scores for state anger, state anxiety, and state stress were calculated as mean task affect scores minus mean baseline affect scores to represent an index of recall task-induced changes in state affect.
Data Analysis
An a priori power analysis [power=0.80; alpha=0.05] indicated that 80 participants would be sufficient to detect medium-to-large effects, like those found for blood pressure responses in conceptually similar studies [37, 53, 54], in a regression model adjusted for six covariates. While power was increased due to the use of repeated-measures analyses with a continuous predictor, 81 subjects were examined to compensate for data loss due to equipment malfunction.
The primary analyses were a series of repeated-measures general linear models (GLMs) to examine prayer coping (continuous measure) for multivariate effects (across task/recovery periods) and univariate effects (for an individual task or recovery period) on CVR and post-stress recovery, as well as affective reactivity. The dependent variables in these models were task or post-stress recovery change scores for SBP, DBP, HR, PEP, CI, SI, TPR, and HRV, along with task change scores for state anger, anxiety, and stress. Effect sizes are partial eta squared (η p 2; i.e., percentage of variance accounted for). Exploratory analyses of total task-related negative affect as a mediator or moderator of associations found between prayer coping and CVR/post-stress recovery measures were conducted with hierarchical regressions as described by Baron and Kenny [50].
Each GLM for CVR, post-stress recovery, and affective reactivity used a standard set of covariates, with exceptions as noted: baseline, BMI (only in cardiovascular GLMs), oral contraceptive use, menstrual phase, and scores from the Perceived Stress Scale, Anger-In subscale, and Anger Control–Anger Out composite. Due to significant correlation between the Spielberger Anger-Control and Anger-Out subscales (r = −0.60, p < 0.001), an Anger Control–Anger Out coping composite score was created using the approach (anger control minus anger out) reported by a comparable CVR study [48] that found similar redundancy between these two 8-item subscales. (Anger-In was not significantly correlated with Anger-Out or Anger-Control). The variables included as covariates in the respective sets of CVR/post-stress recovery and affective reactivity analyses were selected based on prior research [1, 16, 38, 44, 45, 47, 48] and their correlations (p < 0.09) with at least one outcome variable in the respective set of analyses.
Although continuous prayer coping scores were used in all GLMs and regressions in the primary and exploratory analyses, sample characteristics are provided in terms of prayer coping users versus non-users for descriptive purposes only. Due to mechanical errors, the sample size was reduced for HRV and HR (n's = 80) and for PEP, CI, SI, and TPR (n's = 77).
Results
Approximately 49 % of these young African American women reported using prayer as a coping strategy for at least one type of racism experience. Prayer coping was used most often in response to racism experienced in academic settings.
For descriptive purposes, sample characteristics (Table 1) are provided with participants categorized according to whether they reported no use of prayer coping (prayer coping non-users) or reported using prayer coping in response to at least one type of racism experience (prayer coping users). Participants who reported no use of prayer coping had higher resting (pre-experimental) levels of SBP (p < 0.01), DBP, TPR, and lower SI (p's < 0.05). Non-users of prayer coping also had lower Anger-Control and higher Anger-Out scores (p's < 0.05). Users and non-users of prayer coping did not differ significantly on any other psychosocial factor and were similar in terms of other covariates.
Negative affect scores (i.e., manipulation checks) (Table 1) suggest that participants were emotionally and cognitively engaged in the tasks and that the racism and anger recall tasks were effective in evoking stress, anger, and/or anxiety. The mean levels of state anger during the racism and anger recall tasks were similar, with slightly higher mean scores for stress (p < 0.05) and anxiety (p = 0.05) reported during the anger recall than the racism recall (p < 0.05).
Table 2 details the means of cardiovascular parameters during the experimental session. The anger recall task and the new racism recall task developed specifically for this study produced similarly potent cardiovascular responses as measured by task and recovery levels and change scores for CVR and post-stress recovery. The only significant difference was for mean DBP post-stress recovery change scores (relative to baseline), such that mean DBP remained well above baseline after racism recall but quickly returned toward baseline levels after anger recall (p < 0.001). In addition, TPR reactivity was slightly higher during the racism recall than anger recall (p = 0.08).
As shown in the table of unadjusted bivariate correlations (Table 3), prayer coping was positively related to HRV levels after the racism recall task (p < 0.01) and inversely related to DBP levels during and after that task (p’s < 0.05). Perceived stress, anger-in, and anger control-out composite scores were each related to multiple cardiovascular measures (p’s < 0.05), with the strongest correlation found between higher anger control-out scores and higher SBP levels during the anger recall recovery(p < 0.01). The follicular menstrual phase was correlated with greater SBP and TPR reactivity to the racism recall (p’s < 0.05), while oral contraceptive use was correlated with higher resting HR and greater PEP during the anger recall (p’s < 0.01).
The GLMs of prayer coping on affective reactivity to the recall tasks (Table 4) indicated that higher prayer coping was associated with lower state stress reactivity to the racism recall (p < 0.05; η p 2 = 0.05) and explained 5 % of the variance in the model. Prayer coping did not have significant univariate or multivariate effects on state anger or anxiety reactivity. Aside from the affective baselines being related to respective affective reactivity scores, the only other significant association was between higher chronic stress (i.e., the Perceived Stress Scale) and greater anxiety response to the racism recall (p < 0.05).
Table 5 shows the results of GLMs conducted for prayer coping on CVR to the recall tasks and recovery after the tasks. The results are described below.
GLMs: Prayer Coping on CVR to Stress
Multivariate analyses (Table 5) indicated that prayer coping was significantly related to DBP reactivity across the tasks [F(1, 72 = 8.25, p < 0.01; η p 2 = 0.10 ). Similar to the unadjusted bivariate correlation, higher prayer coping was associated with lower DBP during the racism recall after adjustment for covariates (p < 0.05, η p 2 = 0.07). Prayer coping accounted for 7 % of the variance in the model of DBP reactivity to the racism recall.
Regarding HR reactivity, univariate analyses indicated that higher prayer coping was marginally associated with lower HR reactivity during racism recall (p < 0.07; η p 2 = 0.05). Prayer coping was not associated with HR reactivity in multivariate analyses.
After adjustment for covariates, prayer coping was not significantly related to SBP, PEP, CI, SI, TPR, or HRV reactivity in multivariate or univariate analyses (p's > 0.05). However, higher anger-in scores were associated with lower TPR reactivity during the racism recall, while higher anger control-out scores and higher perceived stress scores were associated with lower DBP and higher PEP reactivity, respectively, during the anger recall (p’s < 0.05).
GLMs: Prayer Coping on Post-stress Cardiovascular Recovery
The GLMs for prayer coping on post-stress recovery (Table 5) showed that prayer coping had significant multivariate effects on DBP recovery [F(1,72) = 12.26, p = 0.001; η p 2 = 0.15]. Similar to the unadjusted bivariate correlation, the adjusted GLM indicated that higher prayer coping scores were associated with lower DBP during recovery from the racism recall (p < 0.01; η p 2 = 0.10) and explained 10 % of the variance in the model. However, higher prayer coping also was associated with higher DBP during recovery from the anger recall (p < 0.01; η p 2 = 0.13).
Consistent with the unadjusted bivariate correlation, higher prayer coping remained associated with higher HRV during the racism recall recovery (p < 0.01, η p 2 = 0.11) after adjustment for covariates and accounted for 11 % of the variance explained by the model. Prayer coping was not significant in multivariate analyses of HRV across recovery periods.
No significant multivariate or univariate effects were found for prayer coping on SBP, HR, PEP, CI, SI, or TPR during post-stress recovery. However, higher anger-in scores were associated with lower SBP during racism recall recovery, while higher anger control-out scores were related to higher SBP during anger recall recovery (p’s < 0.05).
Exploratory Analyses: Mediation or Moderation by Task-Related Negative Affect
Negative affect during recall tasks was not significantly correlated with prayer coping; thus, it did not meet the guideline for mediation analysis [50]. However, hierarchical regressions were conducted to examine it for moderating effects on the significant associations observed for prayer coping with DBP and HR reactivity and with post-stress recovery of DBP and HRV. Based on a significant regression coefficient for the product term of prayer coping × negative affect (entered in the regression after prayer coping and negative affect were entered in the regression separately) [50], negative affect had a significant moderator effect (β = −0.1.18, p < 0.05) on HR reactivity to the racism recall. That is, those with lower prayer coping had higher HR reactivity, if they also had higher negative affect. Negative affect did not moderate any other observed associations.
Discussion
To our knowledge, this is the first study to examine how self-reported prayer, as a coping strategy for racism-related stress, relates to multiple indicators of cardiovascular function. In response to "re-living" a personally relevant experience of racism-related stress, participants showed the hypothesized associations between higher prayer coping and favorable levels of both subjective stress and cardiovascular stress responses in terms of DBP reactivity, DBP post-stress recovery, and HRV post-stress recovery.
Greater DBP reactivity, slower DBP recovery, and reduced HRV levels have been linked to increased risk for CVD [17, 55]. These links between poorer cardiovascular function and CVD may have implications for African American women who are exposed to racism-related stress but do not use prayer or other coping strategies/processes that benefit cardiovascular health. We found that those women using less prayer coping had less favorable DBP and HRV (and marginally less favorable HR) responses during and/or after racism-related stress exposure. Importantly, those women reporting no use of prayer coping had significantly higher unadjusted resting levels of SBP, DBP, and TPR (with lower resting SI) even before they were exposed to experimental stressors.
The cardiovascular literature offers no directly comparable studies of prayer coping in the context of acute racism-related stressors. However, our finding that prayer coping was beneficially associated with lower DBP is similar to prior work showing lower DBP levels among older adults, particularly older African American adults, who more frequently engaged in private prayer or Bible study [15]. In a similar vein, a study in India found that men who prayed regularly had a lower prevalence of coronary heart disease [20].
While those studies [15, 20], like our findings, suggest prayer may be associated with better cardiovascular health, we also found that it was associated with prolonged elevation of DBP following the anger recall after adjustments for anger coping styles, chronic stress, and other covariates. It is unclear why those who reported using prayer to cope with racism-related stress had better DBP recovery after the racism recall but worse DBP recovery after the anger recall. Again, while there are no directly comparable studies available, greater frequency of prayer (not context-specific) showed no association with resting DBP in one study [22] but was linked to higher DBP in a study that averaged DBP across resting, reactivity (to computer stress tasks), and recovery periods [16]. Additional research is needed to examine whether prayer coping is associated with adverse cardiovascular functioning under certain stress-inducing situations. Future studies should assess whether those who utilize prayer to cope with perceived racism are likely to use prayer as a coping strategy broadly across different stressors or only with certain types of stressors.
Higher prayer coping was related to slightly lower HR reactivity to the racism recall and significantly higher HRV during recovery, with no significant association found between prayer coping and either PEP or CI during or after the racism recall. This suggests that prayer coping may be more strongly related to parasympathetic (vagal) cardiac control than to beta-adrenergically mediated sympathetic activation. In a similar vein, enhanced HRV was observed during recitation of the rosary prayer [19]. Further research is needed to determine if prayer is associated with a particular pattern of cardiac autonomic regulation.
The data on negative affect (i.e., stress, anger, anxiety) during the recall tasks provide an interesting supplement to the findings on prayer coping and cardiovascular function. We found support for our hypothesis that those reporting greater usage of prayer coping would have lower subjective stress in response to the racism recall. Prayer coping was not significantly associated with reactivity of state anger or anxiety, which suggests that participants reporting higher prayer coping underwent similar anger and anxiety inductions during the tasks as those who reported little or no use of prayer coping. Given that prayer coping was linked to lower DBP and HR reactivity during the racism recall, participants who reported more prayer coping might have been somewhat shielded from the potentially adverse cardiovascular consequences of experiencing anger and anxiety. Furthermore, our moderation analyses found that HR reactivity to the racism recall was lower among participants with higher prayer coping, if they also had lower negative affect during the task. It has been suggested that prayer promotes mental relaxation that alters physiological responses [3, 18], but the mechanisms underlying the associations between prayer, stress/affect, and cardiovascular health need further study.
Regarding the recall tasks as laboratory stressors, the racism recall task that was developed for this study was shown to have similar potency as the more widely used anger recall task in terms of cardiovascular and affective responses. Like the anger recall, the racism recall offers the advantage of being personally relevant to the study participants. Both recall tasks elicited substantial negative affect, suggesting that participants found the tasks to be engaging and perceived the tasks in a manner consistent with their designs.
The current study adds to the scant literature available on coping with racism-related stress and expands the limited research assessing how prayer relates to cardiovascular health. One of this study's strengths is that, to our knowledge, it is the first cardiovascular study to examine context-specific use of prayer as a strategy to cope with racism-related stress. It is strengthened by its use of personally relevant experimental stressors that were salient to participants, in contrast to experimental tasks with unknown relevance to participants' real world experiences. The findings showing that prayer coping was associated with favorable levels of cardiovascular parameters before, during, and after stress exposure are strengthened by the fact that these associations were found across measures derived from three different types of cardiovascular monitoring equipment. Furthermore, the study was strengthened by increased reliability of cardiovascular measures that had been derived from averages of multiple readings within sets of repeated measures for baseline/rest, task, and recovery periods. Another strength is the study's limiting of confounders through exclusion criteria, pre-session instructions to avoid caffeine and alcohol, and statistical adjustments.
This work should be replicated with a larger sample, given the relatively small sample size. With additional statistical power, the marginal association between higher prayer coping and lower HR reactivity to the racism recall may have reached conventional statistical significance. Although the sample was sufficient to detect unadjusted differences in resting SI and TPR between those who used prayer coping and those who did not, the lack of significant findings for PEP, CI, SI, and TPR in the adjusted CVR and post-stress recovery analyses may be due to the reduced sample size on those parameters. In addition to its utilization of self-reported measures, the study also may be limited by its inability to account for the use of other coping/stress management strategies (used individually or simultaneously) and psychosocial factors (e.g., social support, positive mood, higher socioeconomic status) that could possibly explain our observed associations. Despite the exclusion criteria, it is possible that undiagnosed illness or unreported medication use influenced our results. It also is unclear how well our results for this predominantly U.S.-born sample of young, healthy, college-educated African American women would generalize to other groups (e.g., male, older, less educated, less healthy, residents of other U.S. regions or countries). Further research is needed to assess the generalizability of our findings to immigrant populations, given that immigrants' approach to coping with racism may be influenced by culture and immigration status [27]. Although prayer coping had associations with favorable levels of cardiovascular parameters before, during, and after racism stress exposure, the clinical significance of these findings is unclear and requires further study. Finally, these cross-sectional data cannot establish prayer coping as the cause of the noted cardiovascular and affective variations.
Among young, healthy African American women, higher use of prayer to cope with racism-related stress was associated with a more favorable pattern of cardiovascular and affective functioning in response to a recalled experience of perceived racism. Our results provide an initial step in understanding the cardiovascular impact of prayer as a coping response to racism-related stress.
References
Dimsdale JE. Psychological stress and cardiovascular disease. J Am Coll Cardiol. 2008; 51(13): 1237-1246.
Townsend M, Kladder V, Ayele H, Mulligan T. Systematic review of clinical trials examining the effects of religion on health. South Med J. 2002; 95(12): 1429-1434.
Masters KS, Spielmans GI. Prayer and health: Review, meta-analysis, and research agenda. J Behav Med. 2007; 30(4): 329-338.
Labbé EE, Fobes A. Evaluating the interplay between spirituality, personality and stress. Appl Psychophysiol Biofeedback. 2010; 35(2): 141-146.
Steffen PR, Hinderliter AL, Blumenthal JA, Sherwood A. Religious coping, ethnicity, and ambulatory blood pressure. Psychosom Med. 2001; 63(4): 523-530.
Gillum RF, Ingram DD. Frequency of attendance at religious services, hypertension, and blood pressure: The Third National Health and Nutrition Examination Survey. Psychosom Med. 2006; 68(3): 382-385.
Bell CN, Bowie JV, Thorpe RJ Jr. The interrelationship between hypertension and blood pressure, attendance at religious services, and race/ethnicity. J Relig Health. 2010 Mar 31.
Sørensen T, Danbolt LJ, Lien L, Koenig HG, Holmen J. The relationship between religious attendance and blood pressure: The HUNT Study, Norway. Int J Psychiatry Med. 2011; 42: 13-28.
Berntson GG, Norman GJ, Hawkley LC, Cacioppo JT. Spirituality and autonomic cardiac control. Ann Behav Med. 2008; 35(2): 198-208.
Kurita A, Takase B, Shinagawa N, et al. Spiritual activation in very elderly individuals assessed as heart rate variability and plasma IL/10/IL-6 ratios. Int Heart J. 2011; 52: 299-303.
Masters KS, Knestel A. Religious motivation and cardiovascular reactivity among middle aged adults: Is being pro-religious really that good for you? J Behav Med. 2011; 34: 449-461.
Masters KS, Hill RD, Kircher JC, Lensegrav Benson TL, Fallon JA. Religious orientation, aging, and blood pressure reactivity to interpersonal and cognitive stressors. Ann Behav Med. 2004; 28(3): 171-178.
Fitchett G, Powell LH. Daily spiritual experiences, systolic blood pressure, and hypertension among midlife women in SWAN. Ann Behav Med. 2009; 37(3): 257-267.
Yeager DM, Glei DA, Au M, Lin HS, Sloan RP, Weinstein M. Religious involvement and health outcomes among older persons in Taiwan. Soc Sci Med. 2006; 63(8): 2228-2241.
Seeman TE, Dubin LF, Seeman M. Religiosity/spirituality and health. A critical review of the evidence for biological pathways. Am Psychol. 2003; 58(1): 53-63.
Tartaro J, Luecken LJ, Gunn HE. Exploring heart and soul: Effects of religiosity/spirituality and gender on blood pressure and cortisol stress responses. J Health Psychol. 2005; 10: 753-766.
Chida Y, Steptoe A. Greater cardiovascular responses to laboratory mental stress are associated with poor subsequent cardiovascular risk status: A meta-analysis of prospective evidence. Hypertension. 2010; 55(4): 1026-1032.
Koenig HG, George LK, Hays JC, Larson DB, Cohen HJ, Blazer DG. The relationship between religious activities and blood pressure in older adults. Int J Psychiatry Med. 1998; 28(2): 189-213.
Bernardi L, Sleight P, Bandinelli G, et al. Effect of rosary prayer and yoga mantras on autonomic cardiovascular rhythms: Comparative study. BMJ. 2001; 323(7327): 1446-1449.
Gupta R, Prakash H, Gupta VP, Gupta KD. Prevalence and determinants of coronary heart disease in a rural population of India. J Clin Epidemiol. 1997; 50(2): 203-209.
Feinstein M, Liu K, Ning H, Fitchett G, Lloyd-Jones DM. Burden of cardiovascular risk factors, subclinical atherosclerosis, and incident cardiovascular events across dimensions of religiosity: The multi-ethnic study of atherosclerosis. Circulation. 2010; 121(5): 659-666.
Buck AC, Williams DR, Musick MA, Sternthal MJ. An examination of the relationship between multiple dimensions of religiosity, blood pressure, and hypertension. Soc Sci Med. 2009; 68(2): 314-322.
Roger VL, Go AS, Lloyd-Jones DM, American Heart Association Statistics Committee and Stroke Statistics Subcommittee, et al. Heart disease and stroke statistics—2011 update: A report from the American Heart Association. Circulation. 2011; 123(4): e18-e209.
Jolly S, Vittinghoff E, Chattopadhyay A, Bibbins-Domingo K. Higher cardiovascular disease prevalence and mortality among younger blacks compared to whites. Am J Med. 2010; 123(9): 811-818.
Brondolo E, Love EE, Pencille M, Schoenthaler A, Ogedegbe G. Racism and hypertension: A review of the empirical evidence and implications for clinical practice. Am J Hypertens. 2011; 24(5): 518-529.
Cardarelli R, Cardarelli KM, Fulda KG, et al. Self-reported racial discrimination, response to unfair treatment, and coronary calcification in asymptomatic adults—The North Texas Healthy Heart study. BMC Publ Health. 2010; 10: 285.
Brondolo E, Brady Ver Halen N, Pencille M, Beatty D, Contrada RJ. Coping with racism: A selective review of the literature and a theoretical and methodological critique. J Behav Med. 2009; 32(1): 64-88.
Chatters LM, Taylor RJ, Jackson JS, Lincoln KD. Religious coping among African Americans, Caribbean Blacks and non-Hispanic Whites. J Community Psychol. 2008; 36(3): 371-386.
Majumdar B, Ladak S. Management of family and workplace stress experienced by women of colour from various cultural backgrounds. Can J Public Health. 1998; 89(1): 48-52.
Din-Dzietham R, Nembhard WN, Collins R, Davis SK. Perceived stress following race-based discrimination at work is associated with hypertension in African-Americans. The Metro Atlanta Heart Disease Study, 1999–2001. Soc Sci Med. 2004; 58(3): 449-461.
Barksdale DJ, Farrug ER, Harkness K. Racial discrimination and blood pressure: Perceptions, emotions, and behaviors of black American adults. Issues Ment Health Nurs. 2009; 30: 104-111.
Clark R, Anderson NB, Clark VR, Williams DR. Racism as a stressor for African Americans. A biopsychosocial model. Am Psychol. 1999; 54(10): 805-816.
Lazarus RS. Coping theory and research: Past, present, and future. Psychosom Med. 1993; 55(3): 234-247.
Waldstein SR, Kop WJ, Schmidt LA, Haufler AJ, Krantz DS, Fox NA. Frontal electrocortical and cardiovascular reactivity during happiness and anger. Biol Psychol. 2000; 55(1): 3-23.
McNeilly MD, Anderson NB, Armstead CA, et al. The perceived racism scale: A multidimensional assessment of the experience of white racism among African Americans. Ethn Dis. 1996; 6: 154-166.
McNeilly M, Anderson NB, Robinson E, et al. The convergent, discriminant, and concurrent criterion validity of the Perceived Racism Scale: A multidimensional assessment of White racism among African Americans. In: Jones RL, ed. Handbook of Tests and Measurements for Black Populations. Hampton, VA: Cobb and Henry Publishers; 1996: 359-374.
Clark R. Perceptions of interethnic group racism predict increased vascular reactivity to a laboratory challenge in college women. Ann Behav Med. 2000; 22(3): 214-222.
Blascovich J, Katkin ES, eds. Cardiovascular Reactivity to Psychological Stress and Disease. Washington, DC: American Psychological Association; 1993.
Sherwood A, Allen MT, Fahrenberg J, Kelsey RM, Lovallo WR, van Doornen LJP. Methodological guidelines for impedance cardiography. Psychophysiology. 1990; 27: 1-23.
Debski TT, Kamarck TW, Jennings JR, Young LW, Eddy MJ, Zhang YX. A computerized test battery for the assessment of cardiovascular reactivity. Int J Biomed Comput. 1991; 27: 277-289.
de Geus EJC, Willemsen GHM, Klaver CHAM, van Doornen LJP. Ambulatory measurement of respiratory sinus arrhythmia and respiration rate. Biol Psychol. 1995; 41: 205-227.
Task Force of the European Society of Cardiology and the North American Society of Pacing Electrophysiology. Heart rate variability: Standards of measurement, physiological interpretation, and clinical use. Circulation. 1996; 93: 1043-1065.
Spielberger CD. Preliminary Manual for the State-Trait Personality Inventory. Tampa, FL: University of South Florida; 1979.
Schallmayer S, Hughes BM. Impact of oral contraception and neuroticism on cardiovascular stress reactivity across the menstrual cycle. Psychol Health Med. 2010; 15(1): 105-115.
Van Goozen SH, Frijda NH, Wiegant VM, Endert E, Van de Poll NE. The premenstrual phase and reactions to aversive events: A study of hormonal influences on emotionality. Psychoneuroendocrinology. 1996; 21(5): 479-497.
Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983; 24(4): 385-396.
Igna CV, Julkunen J, Vanhanen H. Anger expression styles and blood pressure: Evidence for different pathways. J Hypertens. 2009; 27(10): 1972-1979.
Rabineau KM, Treiber FA, Poole J, Ludwig D. Interactive effects of anger expression and ET-1 Lys198Asn polymorphism on vasoconstriction reactivity to behavioral stress. Ann Behav Med. 2005; 30(1): 85-89.
Spielberger CD. State-Trait Anger Expression Inventory. Orlando, FL: Psychological Assessment Resources; 1988.
Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986; 51: 1173-1182.
Linden W, Earle TL, Gerin W, Christenfeld N. Physiological stress reactivity and recovery: Conceptual siblings separated at birth? J Psychosom Res. 1997; 42(2): 117-135.
Kubicek WG, Karnegis JN, Patterson RP, Witsoe DA, Mattson RH. Development and evaluation of an impedance cardiac output system. Aerosp Med. 1966; 37(12): 1208-1212.
Prkachin KM, Mills DE, Zwaal C, Husted J. Comparison of hemodynamic responses to social and nonsocial stress: Evaluation of an anger interview. Psychophysiology. 2001; 38: 879-885.
McNeilly MD, Robinson EL, Anderson NB, et al. Effects of racist provocation and social support on cardiovascular reactivity in African American women. Int J Behav Med. 1995; 2(4): 321-338.
Huikuri HV, Jokinen V, Syvänne M, et al. Heart rate variability and progression of coronary atherosclerosis. Arterioscler Thromb Vasc Biol. 1999; 19(8): 1979-1985.
Acknowledgments
The first author's graduate research was partially supported by a National Institute of General Medical Sciences Initiative for Minority Student Development Grant (R25-GM55036). A Department of Veterans Affairs (VA) Health Services Research and Development (HSR&D) post-doctoral fellowship currently supports her research.
Disclaimer
The views expressed in this article are solely those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs, the University of Washington, the University of Maryland, or Ohio State University.
Conflict of Interest Statement
The authors have no conflict of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Cooper, D.C., Thayer, J.F. & Waldstein, S.R. Coping with Racism: The Impact of Prayer on Cardiovascular Reactivity and Post-stress Recovery in African American Women. ann. behav. med. 47, 218–230 (2014). https://doi.org/10.1007/s12160-013-9540-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12160-013-9540-4