Abstract
Background
Using antiretroviral therapies for HIV prevention relies on patient adherence and avoidance of co-occurring sexually transmitted infections.
Purpose
The objective of this study is to simultaneously examine HIV treatment adherence and sexual risks for HIV transmission.
Methods
This study is a prospective cohort of 201 men and 55 women diagnosed with HIV/AIDS infection.
Results
A total of 32% men and 39% women engaged in unprotected intercourse with at least one HIV negative or unknown HIV status sex partner over 12 months. Nearly half (46%) of participants with HIV negative or unknown HIV status unprotected sex partners had detectable HIV viral load and were significantly more likely to have contracted a sexually transmitted infection since their HIV diagnosis. Individuals at higher risk for transmitting HIV were also less adherent to antiretroviral therapies.
Conclusions
Programs that aim to use antiretroviral therapies for HIV prevention require careful attention to adherence, sexually transmitted co-infections, and substance use.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Efforts to contain the spread of HIV have been frustrated by unsuccessful vaccine trials, a series of ineffective microbicides, and failure to scale up behavioral interventions [1]. Facing these challenges, public health policymakers and prevention scientists have turned to antiretroviral therapies to avert new HIV infections. The clinical success of antiretroviral therapies in slowing HIV disease progression stems from its effective suppression of HIV replication. Pre-exposure use of antiretroviral therapies as prophylaxis can impede viral replication and prevent the onset of HIV infection [2]. Antiretroviral therapies also penetrate the genital compartment with the potential to reduce HIV infectiousness [3]. For example, research with HIV serodiscordant couples in Africa has shown that initiating antiretroviral therapies reduces HIV transmission [4], and undetectable virus in blood plasma corresponds to lower rates of HIV transmission [5]. Finally, mathematical models project that under optimal conditions, specifically perfect medication adherence and no co-occurring sexually transmitted infections, new HIV infections will plummet and there is the potential to eliminate HIV epidemics [6, 7]. Enthusiasm for using antiretroviral therapies for HIV prevention led to the Swiss Federal AIDS Commission policy statement that people living with HIV/AIDS who have effectively suppressed HIV replication demonstrated by repeated undetectable viral load test results can be considered noninfectious, alleviating concern about HIV transmission [8]. Recent reports suggest that this policy shift has indeed resulted in less protected sexual behavior among men and women familiar with the Swiss Statement who have undetectable viral loads [9].
Donnell et al. [4] recently reported a study that supports the use of HIV treatment for prevention. Specifically, the prospective cohort study of Donnell et al. observed only one HIV infection among 349 HIV serodiscordant South African couples in which the infected partner had initiated antiretroviral therapies. In contrast, there were 102 HIV infections observed among the 3,032 couples with untreated HIV-positive partners. These findings provide important empirical support for mathematical modeling studies that have driven the momentum behind using antiretroviral therapies for prevention, despite their being overly optimistic [6, 10–14]. However, critical features of the study of Donnell et al. suggest that the findings illustrate another best-case scenario. First, the couples in the trial of Donnell et al. were in stable relationships; 75% were married and the median duration of their relationships was 5 years [15]. In addition, the rates of unprotected sexual behaviors were low at baseline and diminished further over time; 29% of the couples reported unprotected sex at baseline which reduced to 7% at the final follow-up. Importantly, all of the couples were routinely screened and treated for co-occurring sexually transmitted infections. Co-infection with other sexually transmitted infections is known to increase HIV viral shedding in the genital tract, resulting in infectiousness that rivals acute infection [16]. Finally, failure to adhere to antiretroviral therapies leads to incomplete viral suppression and therefore increased infectiousness. Research has shown that people who initiate antiretroviral therapies in developing countries demonstrate high levels of medication adherence [17], and adherence was certainly a factor in the findings of Donnell et al. The selection of stable couples who practice minimal risk behaviors, receive ongoing risk reduction counseling, repeated HIV testing, sexually transmitted infection diagnosis and treatment, and are likely adherent to antiretroviral therapies clearly represents an optimal situation for using antiretroviral therapies for HIV prevention.
Among the likely behavioral factors that will undermine the use of antiretroviral therapies for HIV prevention are alcohol and other drugs. Substance use is associated with both antiretroviral therapy nonadherence and HIV transmission risk behaviors in people living with HIV/AIDS [18–22]. Research shows that substance use is prevalent among people living with HIV/AIDS and poses serious challenges to HIV treatment and prevention [19, 23]. Alcohol and other drug use may interfere with the potential for antiretroviral therapies to prevent HIV transmission by impeding medication adherence and increasing risks for sexually transmitted infections. Despite research showing that alcohol use both influences sexual transmission risks and interferes with medication adherence, there are a few studies that have examined drinking as a potential barrier to using antiretroviral therapies for preventing HIV transmission.
The current study examined the sexual transmission risk behaviors and medication adherence of men and women in a prospective cohort of people living with HIV/AIDS who were receiving antiretroviral therapies. We used a longitudinal cohort design to examine the HIV transmission risk behaviors of persons who engaged in unprotected sexual intercourse with non-HIV-infected partners. Because most previous research has used cross-sectional designs, our ability to predict behavior over time is a substantial research advance. In addition, we used a community sample of people living with HIV representing a full range of relationships, rather than among stable couples participating in a prevention trial. Within this context of real world relationships, we tested two hypotheses regarding the association between HIV transmission risk and medication adherence:
-
Hypothesis 1:
Individuals who engage in HIV transmission risk behavior will demonstrate poorer HIV treatment adherence. This hypothesis is based on previous cross-sectional survey research that has found HIV risk behaviors associated with medication adherence [24–26].
-
Hypothesis 2:
The association between HIV transmission risks and medication adherence will be moderated by alcohol use, such that persons who both drink alcohol and engage in higher transmission risk behavior will demonstrate poorer HIV treatment adherence. This hypothesis is based on previous observations that alcohol use influences sexual risk behaviors [19] and that alcohol use impacts medication adherence [22]. We predict that alcohol will play a more pervasive role in the adherence of persons at higher risk for transmitting HIV.
Methods
Participants
A convenience sample of 256 men, 77 women, and 10 transgender persons were recruited from AIDS services, healthcare providers, social service agencies, and infectious disease clinics in Atlanta, GA. Recruitment relied on responses to brochures placed in waiting rooms of AIDS service providers and infectious disease clinics throughout Atlanta as well as a systematic approach to word-of-mouth chain recruitment. Specifically, participants were given study brochures and encouraged to refer their HIV positive friends to the study. The study entry criteria were age 18 years or older and having been diagnosed with HIV infection.
For the current study, we restricted the sample to 223 men, 61 women, and 10 transgender persons who were receiving antiretroviral therapies and were sexually active. Over the entire observation period, 28 men, 6 women, and 4 transgender persons were lost to follow up, resulting in 86% cohort retention. Thus, 195 men, 55 women, and 6 transgender persons completed the follow-ups. All six transgender persons were biological males and were therefore included with men in the main analyses.
Study Design
Participants were followed up in a prospective cohort with measures taken at baseline, 4-month follow-up, and 8-month follow-up. Because sexual behaviors were collected using 4-month retrospective recall periods, there were 12 continuous months of sexual behavior analyzed. The unannounced pill counts occurred monthly for 8 months. For prospective analyses, viral load was assessed by drawing blood specimens for HIV RNA testing at the final assessment.
Behavioral measures were collected using an instructor guided self-administration procedure in groups of four to eight persons. Participants were shown page by page how to complete the measures using a projected facsimile, assuring that instructions for each instrument were carefully described and that participants were given privacy when responding. We chose this method of administration to provide direct instruction and explanations for the retrospective recall portions of the assessment. Data were collected between January 2008 and June 2009. The study was approved the University of Connecticut Institutional Review Board.
Demographic and Health Characteristics
Participants were asked their age, years of education, income, ethnicity, sexual orientation, and employment status. HIV-related symptoms were assessed using a previously developed and validated measure [27]. Participants indicated whether they knew their most recent CD4 (T cell) count and HIV viral load. Participants also reported whether they understood the meaning of their viral load and whether they keep track of their viral load. Participants also indicated whether they had been diagnosed with a new sexually transmitted infections since they tested HIV positive.
Blood Specimen Collection and Laboratory Analysis
Participants provided blood specimens to test for HIV RNA within 1 week after their final unannounced pill count. We used a single blood collection for viral load at the end of the study because of the relatively brief follow-up period. Blood samples were collected at the project offices using standard phlebotomy and couriered to the lab for processing. Whole blood specimens in EDTA tube (Becton Dickinson) were centrifuged at 500 g for 10 min within 4 h of collection. The plasma HIV RNA was recovered and aliquoted into 1-ml samples and stored at −70°C. Plasma viral load was determined by the Amplicor HIV-1 Monitor test (Roche Diagnostics, Indianapolis, IN) with a sensitivity for detecting down to 50 copies per milliliter.
Alcohol and Other Drug Use
Participants completed the first three items of the Alcohol Use Disorders Test (AUDIT) to assess current alcohol use (1) frequency, (2) quantity, and (3) heavy drinking episodes. Participants also indicated whether they were currently using cannabis, cocaine/crack, and other drugs. Drugs used at the baseline assessment were summed to create a drug use index, ranging from 0 to 3.
Sexual Risk and Protective Behaviors
Participants reported their number of male and female sex partners and frequency of sexual behaviors in the previous 4 months. We assessed behaviors with regard to the HIV status of sex partners, with HIV-positive partners defining seroconcordant relationships and HIV-negative and unknown HIV status partners defining serodiscordant partnerships. Thus, we measured vaginal and anal intercourse with and without condoms separately within seroconcordant and serodiscordant partnerships. We collapsed receptive and insertive anal intercourse with vaginal intercourse because these are the highest risk sexual behaviors for HIV transmission [28]. A 4-month retrospective period was selected because previous research has shown reliable reports for numbers of partners and sexual events over this time period [29]. Participants were instructed to think back over the past 4 months and estimate the number of sex partners and number of sexual occasions in which they practiced each behavior. The instructions included cues for recollecting behavioral events over the past 4 months. The current study focused on data within HIV serodiscordant relationships.
HIV Treatment Adherence
To monitor medication adherence, we conducted telephone-based unannounced pill counts. The telephone adaptation of unannounced pill counts has been validated against home-based pill counts and patient viral load [30–32]. Participants were provided with a free cell phone that restricted service for project contacts and emergency use (e.g., 911). Participants were called at an unscheduled time by a phone assessor. Pill counts occurred over 21 to 35 day intervals. Adherence was calculated for all points at which there were two consecutive pill counts. Participants who missed a pill count were re-contacted the next month. Adherence was calculated by the difference between pills counted on two consecutive calls divided by the pills prescribed, taking into account the number of pills dispensed, pills lost, gained, and taken that day. Stopped medications were adjusted for number of days between the previous pill count and the stop date. Medication refill information, specifically the Rx numbers, filled dates, and remaining number of refills were used to verify the accuracy of medications dispensed over the course of the pill counts.
Statistical Analyses
The focus of this study was on people living with HIV/AIDS who engage in unprotected vaginal or anal intercourse with HIV-negative or unknown HIV status partners. Participants who reported having at least one occurrence of unprotected anal or vaginal intercourse with at least one HIV-negative or unknown HIV status sex partner in the previous 4 months at any of the three behavioral assessments were defined as being at higher risk for transmitting HIV. We dichotomized sexual HIV transmission risk (lower/higher transmission risk) and alcohol use (drinkers/nondrinkers) to define clinically relevant subgroups. Although dichotomizing behavioral data reduces statistical power by restricting ranges, this cost is offset by the clinical interpretation of the findings. In the current sample, 55/87 (63%) persons in the higher-risk group reported one unprotected act, 21/87 (24%) reported two acts, and 11/87 (13%) reported three unprotected anal or vaginal intercourse occasions with HIV-negative or unknown HIV status partners.
We first conducted descriptive analyses for the 12-month cumulative sexual behaviors for participants at lower and higher transmission risk. In these analyses, logistic regressions were performed between participants defined as lower and higher risk for transmitting HIV on baseline demographic, health, and substance use characteristics. We report odds ratios (OR) and 95% confidence intervals.
To test our first hypothesis that sexual transmission risk would be associated with medication adherence, we performed general estimating equations (GEE) with unstructured working correlation matrixes. Linear distribution was used for the continuous percent adherence-dependent variable. Models were tested for the main effects of transmission risk group and assessment times, and also the transmission risk group × time interaction on the dependent variable − treatment adherence. To test our second hypothesis that alcohol use would moderate the association between sexual risk and medication adherence, we repeated the GEE analysis and included dichotomized alcohol use as a blocking factor in the analysis, specifically testing the factorial model for transmission risk group × alcohol use × time on medication adherence. Planned contrasts with least significant difference adjustment were used to test for simple effects. All statistical analyses defined significance as p < 0.05.
Results
The mean sample-level viral load was 11,276.5 (SD = 24,561.9) HIV RNA copies per unit of plasma. Examining all 12 months of behavioral data showed that 32% of men and 39% of women engaged in unprotected vaginal or anal intercourse with HIV-negative or unknown HIV status partners. Over the three respective assessment points, participants reported sums of 248, 317, and 174 unprotected vaginal and anal intercourse occasions in each of the previous 4 months, respectively, for a total of 739 annual HIV exposures. As shown in Table 1, nearly half of participants who had engaged in unprotected sex with serodiscordant partners reported two or more sex partners over the course of 12 months observation. Although the transmission risk groups did not differ in disclosing their HIV status to their most recent sex partner, individuals at higher transmission risk were significantly less likely to have discussed their partner's HIV status. Table 2 shows the demographic and health characteristics of participants at lower and higher risk for HIV transmission. Results indicated few significant demographic differences between groups.
We examined participant awareness of their viral load compared to their viral load that we tested in blood plasma. Half of participants (53%) had a detectable viral load, of which 35% engaged in unprotected intercourse with HIV negative or unknown HIV status sex partners, compared to 33% participants who had an undetectable viral load, a nonsignificant difference. We found that 31% of participants did not know their viral load, of which 84% had detectable HIV RNA in their blood plasma. Among the participants who stated that their most recent viral load was undetectable, 29% were actually detectable, and among those who stated their viral load was detectable, 19% were actually undetectable. In addition, participants at higher risk for HIV transmission were significantly less likely to understand the meaning of their viral load. Results also showed that 42% of participants with recent unprotected nonconcordant sex partners had contracted a new sexually transmitted infection since the time they tested HIV positive, compared to 29% of the lower risk group, a significant difference, OR = 1.72, p < 0.05, 95% CI = 1.01–2.97 (see Table 2).
Sexual Transmission Risks and HIV Medication Adherence
One hundred participants (60%) in the lower risk group and 54 (63%) in the higher transmission risk group were currently taking antiretroviral therapies, a nonsignificant difference, OR = 1.11, p > 0.1, 95% CI = 0.65–1.90. GEE analyses tested our first hypothesis that participants at higher risk for transmitting HIV would be less adherent to their medications. Results showed that the interaction between HIV transmission risk groups and assessment time on adherence was significant, Wald X 2 = 17.52, p < 0.02. (see Table 3) Examination of the group differences across time points showed that the higher risk group had poorer medication adherence than the lower risk group for 6 out of the 8 months of adherence monitoring.
Alcohol Use as a Moderator of the Association Between Sexual Risks for HIV Transmission and Medication Adherence
Results showed that drinking and drug use were common in the sample, with more than half of participants currently using alcohol and more than one in four using some other drug in the previous 4 months. Drinking was more common in the higher risk group compared to those at lower HIV transmission risk (see Table 4). Participants who reported recent unprotected intercourse with HIV-negative or unknown HIV status partners indicated greater current frequency and quantity of alcohol use. A similar pattern of greater drug use among the higher transmission risk group was also observed, although the differences were not significant. With respect to blood plasma HIV RNA, results showed that drinkers had significantly greater HIV RNA concentrations (Mean = 14,275, SD = 28.864) compared to nondrinkers (Mean = 8,021, SD = 18,328), t(249) = 2.01, p < 0.05.
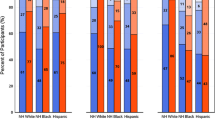
To test our second hypothesis that alcohol use moderates the association between sexual risk groups and medication adherence, we conducted a transmission risk group × alcohol use × assessment time GEE analysis on medication adherence. Results showed a significant HIV transmission risk group by alcohol use interaction, Wald X 2 = 36.76, p < 0.05, confirming our hypothesis that alcohol use would moderate the association between HIV transmission risk and adherence. Figure 1 shows that alcohol use was more strongly associated with poor adherence among those engaging in higher risk behaviors.
Discussion
One in three sexually active people living with HIV/AIDS in the current study reported engaging in unprotected vaginal or anal intercourse with an uninfected partner over the course of a year. More than half of individuals who engaged in higher transmission risk behaviors reported two or more HIV-negative or unknown HIV status sex partners. In addition, HIV status disclosure was not universal, with 56% of persons engaging in unprotected nonconcordant intercourse reporting that they had not disclosed their HIV status to their most recent sex partner and 36% had not discussed their most recent partner's HIV status. These findings illustrate the importance of considering the behavioral context in which HIV treatments will be used for prevention [33].
The current findings also demonstrate challenges of using antiretroviral therapies to prevent HIV transmission. Participants often reported that they believed they had undetectable HIV RNA in their blood plasma when in fact their viral loads were detectable. In addition, participants who engaged in higher transmission risk behaviors were significantly more likely to state that they did not understand the meaning of their viral load. Our results demonstrated that nearly half of participants who engaged in high-risk behaviors had detectable viral loads, with 32% having HIV RNA levels that indicate considerable infectiousness [34]. Our sample level viral load was similar to recent city-wide levels of community viral load in San Francisco [35], supporting the potential generalizability of our virology findings. However, 42% of participants who engaged in non-concordant unprotected sex had contracted a sexually transmitted infection since testing HIV positive, indicating highly infectious periods during sexually active times, regardless of blood plasma HIV RNA.
Treatment nonadherence undermines the potential for antiretroviral therapies to reduce HIV transmission. Overall, lower and higher transmission risk groups demonstrated average adherence below the minimal levels required for consistent suppression of HIV replication [36, 37]. Our first hypothesis was confirmed by our finding that persons who were at highest risk for HIV transmission were also less adherent to their medications. The association between sexual transmission risks and HIV treatment adherence observed in cross-sectional research is therefore supported by the current prospective analyses. Our second hypothesis was also confirmed in our finding that the association between HIV transmission risks and medication adherence was moderated by alcohol use. Suboptimal adherence was observed among more individuals who drank and engaged in nonconcordant unprotected intercourse relative to all other groups. These findings are also consistent with previous research that demonstrates a significant role of alcohol in facilitating HIV transmission risk behaviors among infected persons [19]. To our knowledge, the current findings are the first to demonstrate alcohol use as a contributing factor to poor treatment adherence among persons at high risk for HIV transmission in a prospective study design. Overall, the current findings show a clustering of behaviors that increase the risk of transmitting HIV in sexual relationships.
The findings from this study should be interpreted in light of their methodological limitations. With the exception of medication adherence and viral load, our study relied on self-reported data including sexual behavior and substance use. It is also unknown whether responding to the study measures inadvertently altered subsequent behavior. Our study relied on one assessment of blood plasma HIV RNA collected at the end of the observation period, not allowing for observations of changes in viral load over time. Another limitation to the study is the small number of women which precluded our conducting gender specific analyses. Finally, our results are based on a convenience sample that is predominantly middle-aged, African-American men living with HIV/AIDS in one southern US city. Caution is therefore warranted before generalizing these findings to other populations of people living with HIV/AIDS. With these limitations in mind, we believe that our findings have important implications for efforts to use antiretroviral therapies for HIV prevention.
HIV treatments will effectively reduce HIV transmission when HIV viral load in the genital tract is low. However, individuals must take their medications if they are to suppress viral replication. In addition, co-occurring sexually transmitted infections result in inflammatory processes that spike HIV RNA levels in the genital tract despite therapeutic responses in peripheral blood plasma [38, 39]. Programs that administer antiretroviral therapies for HIV prevention must address behaviors that will undermine their success, particularly non-adherence, substance use, and sexually transmitted co-infections. Fortunately, behavioral interventions designed to improve HIV treatment adherence [40] and interventions to reduce HIV transmission risks among people living with HIV/AIDS [41, 42] have both demonstrated meaningful positive outcomes. Studies that support using antiretroviral therapies for HIV prevention have included behavioral counseling and aggressive sexually transmitted infections diagnosis and treatment [4]. Failure to attend to the behavioral context of using antiretroviral therapies for prevention risks failure, and even worse the inadvertent spread of treatment resistant virus. Real world applications of test and treat approaches to HIV prevention will require attention to alcohol and other drug use, aggressive control of sexually transmitted co-infections, and medication adherence support.
References
Kalichman SC. Time to take stock in HIV/AIDS prevention. AIDS Behav, 2008; 12(3): p. 333–4.
Grant RM, Lama JR, Anderson PL et al., Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. New Eng J Med, 2010; epub ahead of print, November 23, 2010.
Kashuba AD, Dyer JR, Kramer L, Raasch R, Eron J, Cohen M. Antiretroviral-drug concentrations in semen: Implications for sexual transmission of human immunodeficiency virus type 1. Antimicrob Agents Chemotherther, 1999;43(8): 1817–26.
Donnell D, Baeteb JM, Kiarie J, Thomas K, Stevens W, Cohen C, MCIntyre J, Lingappa J, Celum C. Heterosexual HIV-1 transmission after initiation of antiretroviral therapy: A prospective cohort analysis. Lancet 2010;375:2092–98.
Quinn TC, Wawer M, Sewankambo MB, Serwadda D, Li C, Wabwire-Mangen F, et al. et al., Viral load and heterosexual transmission of human immunodeficiency virus type 1. New England Journal of Medicine, 2000; 342: 921–929.
Granich RM, Gilks CF, Dye C, DeCock K, Williams B. Universal voluntary HIV testing with immediate antiretroviral therapy as a strategy for elimination of HIV transmission: A mathematical model. Lancet, 2009; 373(9657):48–57.
Lima, V.D., Hogg, RS, Montaner JS. Expanding HAART treatment to all currently eligible individuals under the 2008 IAS-USA Guidelines in British Columbia, Canada. PLoS ONE, 2010; 5(6):e10991.
Vernazza P, Hirschel B, Bernasconi E, Flepp M, HIV-positive individuals without additional sexually transmitted diseases (STD) and on effective anti-retroviral therapy are sexually non-infectious. Bull des médecins suisses 2008; 89:5.
Hasse B, Ledergerber B, Hischel B, Vernazza P, Glass T, Jeannin A, et al. Frequency and Determinants of Unprotected Sex among HIV-Infected Persons: The Swiss HIV Cohort Study. Clin Inf Dis, 2010; 51(11):1314–1322.
De Cock KM, et al., Can antiretroviral therapy eliminate HIV transmission? Lancet, 2009;373(9657):7–9.
Dieffenbach CW, Fauci, A. Universal voluntary testing and treatment for prevention of HIV transmission. JAMA, 2009;301(22):2380–2.
Garnett GP, Baggaley R. Treating our way out of the HIV pandemic: Could we, would we, should we? Lancet, 2009; 373(9657):9–11.
Wagner B, Blower S. Costs of eliminating HIV in South Africa have been underestimated. Lancet, 2010;376(9745):953–4.
Wagner B, Kahn J, Blower S. Should we try to eliminate HIV epidemics by using a ‘Test and Treat’ strategy? AIDS 2010; 24(5):775–6.
Celum, C., et al., Acyclovir and transmission of HIV-1 from persons infected with HIV-1 and HSV-2. New Eng J Med 2010; 362(5):427–39.
Cohen MS, et al., Reduction of concentration of HIV-1 in semen after treatment of urethritis: Implications for prevention of sexual transmission of HIV-1. Lancet 1997;349:1868–1873.
Mills EJ, et al. Adherence to antiretroviral therapy in sub-Saharan Africa and North America: A meta-analysis. JAMA 2006; 296(6):679–90.
Kalichman SC, Eaton L, Cherry C et al. Sexually transmitted infections and infectiousness beliefs among people living with HIV/AIDS: Implications for HIV treatment as prevention. HIV Med 2010; 11:502–9.
Shuper PA, et al., Alcohol as a correlate of unprotected sexual behavior among people living with HIV/AIDS: Review and meta-analysis. AIDS Behav, 2009;13(6): 1021–36.
Theall KP, et al., Alcohol consumption, ART usage and high-risk sex among women infected with HIV. AIDS Behav, 2007;11(2):205–15.
Amico KR, et al., The Information-Motivation-Behavioral Skills Model of ART adherence in a deep south HIV+ clinic sample. AIDS Behav 2009;13(1):66–75.
Hendershot CS, et al. Alcohol use and antiretroviral adherence: Review and meta-analysis. JAIDS, 2009; 52(2):180–202.
Baliunas D, et al. Alcohol consumption and risk of incident human immunodeficiency virus infection: A meta-analysis. Internat J Public Health 2010; 55(3):159–66.
Kalichman SC, Rompa D. HIV treatment adherence and unprotected sex practices in people receiving antiretroviral therapy. Sex Transm Inf 2003;79(1) 59–61.
Diamond C, et al. Use of and adherence to antiretroviral therapy is associated with decreased sexual risk behavior in HIV clinic patients. JAIDS 2005;39: 211–218.
Kalichman SC. Co-occurrence of treatment nonadherence and continued HIV transmission risk behaviors: Implications for positive prevention interventions. Psychosom Med 2008; 70(5):593–7.
Kalichman SC, Rompa, D, Cage M. Distinguishing between overlapping somatic symptoms of depression and HIV disease in people living with HIV-AIDS. J Nervous Mental Dis 2000;188(10):662–70.
Baggaley RF, White, RG, Boily MC. HIV transmission risk through anal intercourse: Systematic review, meta-analysis and implications for HIV prevention. Internat J Epid 2010;39(4):1048–63.
Napper LE, Fisher D, Reynolds G, Johnson M. HIV Risk Behavior Self-Report Reliability at Different Recall Periods. AIDS Behav 2010;14:15–61.
Bangsberg DR, et al. Comparing objective measures of adherence to HIV antiretroviral therapy: Electronic medication monitors and unannounced pill counts. AIDS Behav 2001;5:275–281.
Kalichman SC, et al. Monitoring Antiretroviral adherence by unannounced pill counts conducted by telephone: Reliability and criterion-related validity. HIV Clinical Trials 2008;9:298–308.
Kalichman SC, et al. Adherence to antiretroviral therapy assessed by unannounced pill counts conducted by telephone. J Gen Internal Med 2007; 22: 1003–6.
Granich R, et al. Highly active antiretroviral treatment as prevention of HIV transmission: Review of scientific evidence and update. Cur Opinions HIV AIDS, 2010; 5(4):298–304.
Engsig F, et al., Risk of high-level viraemia in HIV-infected patients on successful antiretroviral treatment for more than 6 months. HIV Med 2010; 11:457–461.
Das M, et al. Decreases in community viral load are accompanied by reductions in new HIV infections in San Francisco. PLoS ONE, 2010; 5(6): e11068.
Deeks SG, et al. Trends in multidrug treatment failure and subsequent mortality among antiretroviral therapy-experienced patients with HIV infection in North America. Clin Infectious Dis 2009; 49(10):1582–90.
Parienti JJ, et al. Not all missed doses are the same: Sustained NNRTI treatment interruptions predict HIV rebound at low-to-moderate adherence levels. PLoS ONE 2008; 3(7):e2783.
Cohen MS, Gay CL. Treatment to prevent transmission of HIV-1. Clinical Infectious Diseases, 2010; 50 Suppl 3:S85-95.
Johnson LF, Lewis DA. The effect of genital tract infections on HIV-1 shedding in the genital tract: A systematic review and meta-analysis. Sex Transm Dis 2008; 35(11): 946–59.
Simoni JM, et al. Efficacy of interventions in improving highly active antiretroviral therapy adherence and HIV-1 RNA viral load. A meta-analytic review of randomized controlled trials. JAIDS 2006; 43 Suppl 1: S23-35.
Crepaz N, et al. Do prevention interventions reduce HIV risk behaviours among people living with HIV? A meta-analytic review of controlled trials. AIDS 2006; 20(2):143–57.
Johnson BT, et al. Behavioral interventions for African Americans to reduce sexual risk of HIV: A meta-analysis of randomized controlled trials. JAIDS 2009; 51(4):492–501.
Acknowledgments
This project was supported by grants from the National Institute of Mental Health (NIMH) grants R01-MH71164 (SCK) and R01-MH82633 (SCK), Emory University Center for AIDS Research NIH grant 2P30-AI-050409 (RFS & AMC), and the Department of Veterans Affairs (RFS).
Conflict of Interest Statement
The authors have no conflicts of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Kalichman, S.C., Cherry, C., White, D. et al. Sexual HIV Transmission and Antiretroviral Therapy: A Prospective Cohort Study of Behavioral Risk Factors Among Men and Women Living with HIV/AIDS. ann. behav. med. 42, 111–119 (2011). https://doi.org/10.1007/s12160-011-9271-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12160-011-9271-3