Abstract
Objective
To investigate the role of V/P SPECT/CT and HRCT quantitative parameters in evaluating COPD and asthma disease severity, airway obstructivity-grade, ventilation and perfusion distribution patterns, airway remodeling, and lung parenchymal changes.
Method
Fifty-three subjects who underwent V/P SPECT/CT, HRCT, and pulmonary function tests (PFTs) were included. Preserved lung ventilation (PLVF), perfusion function (PLPF), airway obstructivity-grade (OG), proportion of anatomical volume, ventilation and perfusion contribution of each lobe, and V/P distribution patterns were evaluated using V/P SPECT/CT. The quantitative parameters of HRCT included CT bronchial and CT pulmonary function parameters. In addition, the correlation and difference of V/P SPECT/CT-, HRCT-, and PFT-related parameters were compared.
Results
There was a statistically significant difference between severe asthma and severe-very severe COPD in CT bronchial parameters, like WA, LA and AA, in the lung segment airways (P < 0.05). CT bronchial parameters, like as WT and WA, were statistically significant (p < 0.05) among asthma patients. The EI of severe-very severe COPD was different from that of the disease severity groups in asthma patients (P < 0.05). The airway obstructivity-grade, PLVF and PLPF differed significantly among the severe-very severe COPD and mild-moderate asthma patients (P < 0.05). And the PLPF was statistically significant among the disease severity groups in asthma and COPD (P < 0.05). OG and PLVF, PLPF, and PFT parameters were significantly correlated, with the FEV1 correlation being the most significant (r = − 0.901, r = 0.915, and r = 0.836, respectively; P < 0.01). There was a strong negative correlation between OG and PLVF (r = − 0.945) and OG and PLPF (r = − 0.853) and a strong positive correlation between PLPF and PLVF (r = 0.872). In addition, OG, PLVF, and PLPF were moderately to strongly correlated with CT lung function parameters (r = − 0.673 to − 0.839; P < 0.01), while lowly to moderately correlated with most CT bronchial parameters (r = − 0.366 to − 0.663, P < 0.01). There were three different V/P distribution patterns, including matched, mismatched, and reverse mismatched patterns. Last, the CT volume overestimated the contribution in the upper lobes and underestimated the lower lobes’ contribution to overall function.
Conclusions
Quantitative assessment of ventilation and perfusion abnormalities and the degree of pulmonary functional loss by V/P SPECT/CT shows promise as an objective measure to assess the severity of disease and lung function to guide localized treatments. There are differences between HRCT parameters and SPECT/CT parameters among the disease severity groups in asthma and COPD, which may enhance, to some extent, the understanding of complex physiological mechanisms in asthma and COPD.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Chronic obstructive pulmonary disease (COPD) is a chronic airway condition characterized by progressive airflow limitation and related respiratory symptoms [1,2,3]. Its pathophysiological changes include airway disease, parenchymal lung destruction (emphysema), and vascular changes characterized by progressive vascular occlusion and loss of the vascular system due to inflammatory remodeling in areas of emphysematous destruction [4,5,6,7,8,9]. COPD will be the third leading cause of death in the next ten years [10]. The prevalence of COPD in China in people aged 20 years and older is 8.6%, and the number of deaths from COPD and related diseases is expected to exceed 5.4 million/year by 2060 [10, 11]. Asthma is a clinical syndrome characterized by reversible airway obstruction, and the primary physiological abnormality is airway hyperresponsiveness (the ability of the airway to contract excessively) [12,13,14]. Research data show that the prevalence of asthma among Asian adults ranges from 0.7 to 11.9%, and the trend has been increasing in recent years [15].
COPD and asthma are heterogeneous diseases involving complex structural and functional abnormalities, so patients have different clinical presentations, pathophysiologies, disease pattern progression, and treatment responses. Heterogeneity means that accurate and detailed information about local structural and functional abnormalities is needed to better describe the severity of the disease and improve the selection of potential treatments [16]. In clinical practice, however, the most commonly used method for diagnosing and staging COPD and asthma is the pulmonary function test (PFT), which provides an overall measure of lung function but with limited information about the regional or lobar function. The airway obstruction of COPD and asthma is currently graded by PFT indexes such as forced expiratory volume in 1 s (FEV1), forced vital capacity (FVC), and their ratio [17]. However, these indicators mainly reflect changes in the large and intermediate airways, but COPD and asthma are primarily small airway diseases. FEV1 cannot describe the complexity of chronic airway disease or the underlying pathophysiology and cannot be used alone for optimal assessment and management of the disease [18, 19]. Spirometry does not always correlate with the true degree of airway obstruction or clinical symptoms because abnormalities in clinical symptoms only occur with impairment to 30% of overall lung function. By the time symptoms of this disease appear, the FEV1 has decreased by approximately 50% in most patients [20]. Moreover, the reliability and reproducibility of spirometry are not always feasible due to patient compliance, the quality of the technician, or operating conditions. Therefore, we need better methods to adjust medication to guide individualized treatment [21].
Ventilation/perfusion single photon emission tomography/computed tomography (V/P SPECT/CT) is a nuclear medicine investigation that provides a 3-dimensional functional map of the ventilation and perfusion of the lungs at the lobe level by combining SPECT with low-dose CT. Bajc et al. [22] showed that this hybrid functional imaging technique could standardize the grading of airway obstruction and lung function in respiratory diseases. Moreover, V/P SPECT has been shown to be useful in COPD for differentiating healthy controls from COPD patients and is more sensitive than CT or FEV1 for detecting early airway changes and for semiquantitative assessment of reduced lung function [23, 24]. High-resolution computed tomography (HRCT) is a noninvasive method of measuring the anatomical structure of the bronchial system and quantifying the extent of emphysema. HRCT has been compared with PFT and pathophysiological parameters [24, 25]. Thus, this study used Q-Lung (General Electric Company, USA) to automatically and quantitatively analyze V/P SPECT images, including volume, ventilation, and perfusion in pulmonary lobes, and to determine the relative functional contribution of regional lung lobes to overall lung function. In addition, the small airway analysis software and volume quantitative analysis techniques in the Nebula 3D Imaging Data Center (Philips, Brilliance iCT) automatically analyze HRCT imaging, including structural and functional parameters of the lung lobe.
Although most studies have confirmed the use of V/P SPECT/CT in COPD, SPECT-related parameters usually include only those reflecting pulmonary ventilation and the degree of airway obstruction and are rarely compared with HRCT structural parameters. Notably, few studies have explored the value of SPECT in asthma. Therefore, our study included more SPECT and HRCT-related parameters and expanded the spectrum of SPECT in chronic airway diseases. By investigating the relationship between V/P SPECT/CT functional imaging, HRCT, and PFTs in COPD and asthma patients, this study explored the potential value of these quantitative parameters in the process of disease severity, airway obstruction degree, V/P distribution patterns, airway remodeling, and lung parenchymal changes, providing functional and anatomical information with clinical guidance value.
Materials and methods
Patient population
The ethics committee of the West China Hospital, Sichuan University approved this study and have therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and all subsequent revisions, and all patients provided written informed consent. All patients were clinically confirmed to have COPD and asthma with no history of airway infection in the last four weeks and had no changes in their medication regimen in the last three months because of condition changes. Twenty-three asthma cases were classified as mild-moderate (twelve cases) or severe (eleven cases), according to the Global Initiative for Asthma (GINA). Seventeen COPD cases were classified as mild-moderate (GOLD grade 1–2, five cases) or severe-very severe (GOLD grade 3–4, twelve cases) according to the Global Initiative for Chronic Obstructive Pulmonary Disease (GOLD) guidelines. Finally, another thirteen normal controls and healthy smoking or nonsmoking patients without lung-related diseases were included. The patient characteristics are shown in Table 1.
Pulmonary function testing
All patients underwent pulmonary function testing using a spirometer (Master Screen Spirometer, Jaeger Corp, Germany), as recommended by the American Thoracic Society (ATS)/European Respiratory Society (ERS) [26]. The measured parameters included forced vital capacity (FVC), forced expiratory volume in one second (FEV1), the ratio of the forced expiratory volume in one second to the forced vital capacity (FEV1/FVC), and maximal mid-expiratory flow (MMEF). In addition, the values were expressed as a percent of predicted.
HRCT scanning and image processing
HRCT scanning was performed with a Philips Brilliance 256-layer iCT scanner. Each subject was placed in the supine position and held their breath after full inhalation while scanning occurred from the lung apex to the bottom. The scanning parameters were as follows: tube voltage 120 kV; tube current 100 mAS, window width 1600 Hounsfield Units, window level—600 Hu; pitch 0.985, X-ray tube rotation speed 0.6 slice/rotation, matrix 512 × 512, reconstruction using a standard algorithm, slice thickness 0.625 mm, and reconstruction interval 1 mm.
Emphysema measurement (Fig. 1): The full width at half maxima correction algorithm was used to analyze the lung by density-masked CT images and automatically segment the lung into five lobes, with each lobe filled with a different color. The low-density attenuation areas at end-inspiration CT thresholds below − 950 HU were defined as emphysema and were rendered red. The emphysema index (the percent of emphysema voxels over total lung capacity, EI) was obtained automatically for both lungs, the right lung, the left lung, and each lobe.
Airway measurement (Fig. 2): The software allowed for reliable marking and segmentation of the third- and fifth-generation airways and accurate measurement perpendicular to the long axis of each airway to obtain the lumen and airway diameters. The airway analysis module automatically reconstructed the three-dimensional bronchial trees. The target bronchus was manually selected, and the bronchial parameters were defined as segments and subsegments, which were measured at the third and fifth generations of bronchial openings of the same bronchus and at half of the next generations of bronchial openings, respectively. In addition, lung segment and subsegment airway labeling and measurements were performed by an extensively trained radiologist. Two senior radiologists measured the CT-related parameters using multiple measurements to minimize error and averaged the final results. The airway structure parameters measured included wall area (WA), wall thickness (WT), lumen area (LA), airway area (AA), and the wall/lumen area ratio (WA/LA). Given the significant segmental variability in patients with chronic airway disease, measurements of a single airway might not have represented the full spectrum of airway changes. An average of 18 third- and fifth-generation airways per subject were measured (ten for the right lung and eight for the left lung).
V/P SPECT/CT protocol and image processing
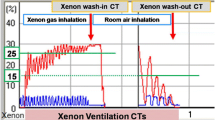
V/P SPECT/C imaging was performed according to the recommendations of the European Association of Nuclear Medicine (EANM) [27]. SPECT/CT was performed (Discovery NM/CT 670, General Electric, Connecticut, USA) using a double-headed gamma camera equipped with low-energy high-resolution collimators. Because PFTs in the respiratory laboratory and most awake activities in humans are usually performed upright, the radiotracers Technegas and 99mTc-MAA (with the deposition pattern fixed upon administration) were used to perform all the clinical imaging lung function studies in this position. Prior to inhalation of the Technegas, the subject repeatedly practiced forceful inhalation by clamping the nostrils, maintained an upright position for two minutes after inhalation of the Technegas, and collected SPECT lung ventilation in the supine position when the chest radioactivity reached 100 uSV. Subsequently, the patient was kept upright for three minutes before slowly being injected intravenously with approximately 5 mCi of 99mTc-labeled macroaggregates of human albumin (99mTc-MAA), remaining upright for two minutes after the injection. Then, a low-dose chest CT was performed in the same position without any movement prior to perfusion tomography. While using radioactive tracers, subjects were instructed to maintain normal tidal breathing. The total data acquisition time was approximately 40 min.
The SPECT/CT data were imported into the reconstruction workstation (Xeleris Functional Imaging Workstation Version 3.1, West China Hospital) to obtain 3D lung V/P SPECT/CT fusion images. In addition, image analysis was performed using in-house software (Q-Lung, General Electric Company, USA). This software allowed for semiautomatic segmentation of the pulmonary CT with automatic transfer of the resulting volume of interest (VOI) to the corresponding V/P SPECT, automatically separating pulmonary data into each lung. With reference to the coronal and transverse sections, the user was asked to define the oblique and horizontal fissures slice-by-slice using the computer mouse on sagittal CT slices, making a subdivision of each lung into the pulmonary lobes, and interpreting the relative contribution (percentage) of each lobe for both ventilation and perfusion. The sum of the lobar percentages was 100%.
V/P SPECT/CT image interpretation
V/P SPECT/CT images were reviewed by two experienced nuclear medicine physicians who did not know each patient's clinical information or CT examination results. The assessment was conducted by the EANM guidelines. The SPECT lung ventilation image quality was first assessed, including 1) uneven distribution of Technegas and 2) “Hot-Spots” distribution (i.e., deposition of inhaled radiopharmaceuticals in the conduction airways such as the primary and middle bronchi or/and peripheral airways) [28]. Then, referring to the predefined 4-point system (0–3) in COPD as described earlier, the subjects’ airway obstructivity-grade (OG) was visually graded [22]. The method was based on ventilation impairment, shown by the distribution pattern of Technegas in the airways. The scale was as follows (Fig. 3):
Normal (0): uniform distribution of Technegas, uniform distribution in the peripheral airways, and no deposition in the large or small airways.
Mild (1): slightly uneven distribution, some aerosol deposition in the small and intermediate airways, and only a small portion of peripheral airway sparse area observed.
Moderate (2): Technetium gas deposited in the intermediate and large airways and reduced distribution of peripheral airways, with more deposition in the central half of the lung.
Severe (3): deposition of Technegas in the central airway with severely impaired penetration and sparse or absent distribution of radioactivity in most of the lung fields.
According to the method proposed by Bajc et al. [29, 30] to quantify the degree of ventilation and perfusion defects, ventilation/perfusion defects were quantified by counting segments or subsegments that showed complete or reduced ventilation and/or perfusion defects and were expressed as percentages (%) of the total lung parenchyma. Segmental reduction or complete subsegmental loss of function was classified as one point, and complete segmental loss was classified as two points. Defects were expressed in points and divided by 36 to obtain the percentage of impaired lung function. Theoretically, there are 18 segments in both lungs, and 36 points were given if there was a complete loss of function. The sum of lung function defects was used to estimate the extent of total lung function reduction. Subtracting the impaired perfusion function, we obtained preserved lung function. Areas were considered to have fully preserved lung function only when both ventilation and perfusion were normal and matched. Preserved lung ventilation function (PLVF) and preserved lung perfusion function (PLPF) were obtained and are expressed as a percentage of the total lung parenchyma.
Statistical analysis
All analyses were performed using SPSS 19.0 software (SPSS Inc., Chicago, IL). The Spearman rank correlation test was used to calculate correlations between V/P SPECT, PFT and HRCT. Last, p < 0.05 indicated statistical significance. The differences were tested for significance using the One-way analysis of variance (ANOVA) or Kruskal–Wallis test.
Results
All patients successfully underwent PFTs, HRCT, and V/P SPECT/CT. The patient characteristics and spirometry values are shown in Table 1. Table 2 shows the differences of V/P SPECT/CT and HRCT quantitative parameters between asthma and COPD. In addition, Table 3 gives Spearman’s correlations between V/P SPECT/CT and CT lung function, CT bronchial parameters and PFTs.
CT bronchial parameters
There was a statistically significant difference between severe asthma and severe-very severe COPD in CT bronchial parameters, such as WA, LA and AA, in the lung segment airways (P < 0.05). Similarly, CT bronchial parameters, such as WT and WA, were statistically significant (p < 0.05) among the disease severity groups in asthma patients. CT bronchial parameters in the lung subsegment airways did not differ among the disease severity groups in asthma and COPD (p > 0.05). And the CT bronchial parameters of asthma and COPD were different from those of the control group (p < 0.05).
CT lung function parameters
The EI of severe-very severe COPD was different from that of the disease severity groups in asthma patients, and the EI of asthma and COPD was different from that of the control group (P < 0.05).
V/P SPECT/CT parameters
The airway obstructivity-grade, PLVF and PLPF differed significantly among the severe-very severe COPD and mild-moderate asthma patients (P < 0.05). And the PLPF was statistically significant among the disease severity groups in asthma and COPD (P < 0.05). The airway obstructivity-grade, PLVF and PLPF in asthma and COPD differed significantly from the control group (P < 0.05).
PFT parameters
SPECT/CT parameters (OG, PLVF and PLPF) and PFT parameters were significantly correlated, with the FEV1 correlation most significant (r = − 0.901, r = 0.915, and r = 0.836, respectively). In addition, there was a strong negative correlation between OG and PLVF (r = − 0.945) and PLPF (r = − 0.853) and a significant positive correlation between PLPF and PLVF (r = 0.872). Otherwise, there was no correlation between each lobe’s ventilation and perfusion percentage and PFTs.
CT bronchial parameters
There were low-to-moderate correlations between SPECT/CT parameters and most of the CT bronchial parameters. However, among the lung segment airways, WA correlated most significantly with OG, PLVF, and PLPF (r = 0.647, r = − 0.634, and r = − 0.663, respectively). In addition, among the lung subsegment airways, WA/LA correlated most significantly with OG, PLVF, and PLPF (r = 0.544, r = − 0.488, and r = − 0.606, respectively).
CT lung function parameters
The OG, PLVF, and PLPF were moderate to significantly correlated with all parameters of CT lung function, with both lung EI having the strongest correlation (r = 0.810, r = − 0.839, and r = − 0.754, respectively).
Furthermore, the CT volumes (%) and SPECT functional lung contributions (ventilation % and perfusion %) per lobe were compared in 53 subjects. CT volumes overestimated the contribution of the upper lung lobes and underestimated the contribution of the lower lung lobes to the overall function, as shown in Fig. 4.
In our patients, we found heterogeneous and patchy distribution patterns of ventilation, central or peripheral “hot spots,” and segmental or nonsegmental defects. In most cases, the lung perfusion distribution pattern showed a decrease or deficit, and sometimes, a compensatory response pattern with a simultaneous increase in perfusion in undamaged areas of the lung was seen. There were three different matching patterns in patients with COPD and asthma, including matched (preserved in V = preserved in P), mismatched (P < V), and reverse mismatched (V < P). In COPD patients, there were 163 segments of matched defects, 43 segments of mismatched defects, and 100 segments of reverse mismatched defects. In the asthma patients, there were 252 segments of matched defects, 69 segments of mismatched defects, and 93 segments of reverse mismatched defects. In addition, 13 COPD patients had all three distribution patterns together, 4 patients had matched defects and reverse mismatched defects, 21 asthma patients had all three distribution patterns together, and 2 had matched defects and reverse mismatched defects. Last, most patients presented with all three distribution patterns simultaneously, as shown in Fig. 5.
Figure 6: V/P SPECT imaging shows the distribution of pulmonary function in a 67-year-old male with GOLD4. Due to diffuse emphysema in both lungs, there is increased translucency in both lungs. Disturbed lung texture and increased parenchymal density in the middle lobe of the right lung and the upper lobe of the left lung were seen on the CT images. However, on the V/P SPECT images, almost only the middle lobe of the right lung retains pulmonary ventilation, and pulmonary perfusion is diffusely reduced, with a compensatory increase in the middle lobe of the right lung. A-C and D-F, coronal, sagittal and transverse, respectively; A-C1-3, CT imaging, ventilation SPECT imaging and fusion imaging, respectively; D-F1-3, CT imaging, perfusion SPECT imaging and fusion imaging, respectively
Discussion
This study combined two examination techniques that quantify airway remodeling and lung function changes in COPD and asthma with the help of Q-lung analysis software and Philips Nebula data processing software. With the advanced image software, we found differences between HRCT parameters and SPECT/CT parameters among the disease severity groups in asthma and COPD (Table 2). And a moderate to strong correlation was found between V/P SPECT parameters and partial PFTs and HRCT parameters. In addition, the correlations between the CT lung function parameters and V/P SPECT parameters were stronger than the CT bronchial parameters (Table 3).
Both asthma and COPD patients have varying degrees of airway remodeling at the lung segment and sub-segment levels, with airway remodeling evident in the lung segments in asthma and in the lung sub-segments in COPD, consistent with the pathogenesis of bronchial changes predominantly in the proximal bronchi in asthma and in the distal bronchi in COPD [31, 32]. In patients with COPD, WA increased and airway LA decreased with increasing severity, whereas in patients with asthma, WA increased but LA did not decrease, which is consistent with the earlier findings of Yasutaka et al. [33] Patients with asthma mainly present with bronchial inflammation and pulmonary ventilation dysfunction [34], while COPD mainly presents with parenchymal lung changes [35]. Compared to asthma, emphysema was more severe in each lobe of COPD. The EI of severe—very severe COPD was different from asthma, mainly in the upper and lower lobes of the right lung. A comparison between V/P SPECT/CT parameters of different severity in COPD and asthma revealed that OG, PLVF, and PLPF were among the indicators to differentiate the severity of asthma and COPD disease.
There were significant correlations between OG, PLVF, and PLPF and the PFT parameters, and each had the strongest correlation with FEV1 (r = − 0.901, r = 0.915, and r = 0.836, respectively). Notably, FEV1 was an independent predictor of respiratory disease. As the degree of obstruction increased and the preserved lung function decreased, the corresponding values for the PFT parameters decreased, the severity of the disease became more severe, and the degree of airflow limitation also became more severe. The study by Jögi et al.[22] showed moderate correlations between the obstruction grade (r = − 0.64), preserved lung function (r = 0.63), and FEV1. Compared to the study by Jögi et al. that predominantly analyzed patients with GOLD 2 and 3, we included asthmatic patients and more patients with GOLD 3 and 4. Although most previous studies on SPECT in the respiratory system have focused on COPD and involved SPECT-related parameters (usually including only those reflecting the degree of pulmonary ventilation and airway obstruction), few studies have included patients with asthma and COPD. The stronger correlation between SPECT and FEV1 may be related to disease severity and the more realistic assessment of the degree of airway obstruction and total preserved lung function with V/P SPECT/CT in patients with higher grading. In a study by Bajc et al. [24], the V/P SPECT-related parameters significantly correlated with emphysema extent (r = 0.66–0.69, p < 0.0001), consistent with our findings (Table 3). Low-to-moderate correlations between OG, PLVF, PLPF and most of the CT bronchial parameters were found in this study. The correlations were more significant in the pulmonary segment bronchus (Table 3).
The present study also found a strong correlation between PLPF, PLVF, and OG. To some extent, the degree of impaired pulmonary perfusion can highly reflect the degree of impaired pulmonary ventilation, presumably due to an efficient mechanism of the pulmonary vascular system matching perfusion to ventilation to maintain narrow distributions of V/P and thus maintain effective gas exchange. The deterioration of the ventilation to perfusion distribution reflects the structural changes affecting the airways and blood vessels [36]. Masiero et al.[37] confirmed that the degree of perfusion deficit in COPD is related to the degree of airflow limitation. Therefore, for patients with chronic airway disease for whom it is challenging to perform pulmonary ventilation imaging or spirometry, lung perfusion imaging alone can, to a certain extent, evaluate the severity of the disease and preserve lung function. Lung lobar parameters, including the percentages of ventilation, perfusion, and volume of each lobe, did not correlate with the PFTs, indicating that regional lobe functional parameters do not reflect changes in global lung function.
In contrast to the supine position required for CT scanning, the volume estimates of regional lobar contribution from CT scans may not be representative of actual lobar contributions during daily life because most human waking activities are performed in the upright position. Our study revealed that CT volumes overestimated the contribution of the upper lung lobes and underestimated the contribution of the lower lung lobes to overall function, consistent with the findings of Bailey et al. [38], expanding the disease spectrum. In diseased lungs, the functional contribution of different lobes and segments to overall ventilation and perfusion may be heterogeneous. However, V/P SPECT/CT allows for accurate delineation of individual lung lobes using CT images and is used to determine the relative functional contribution of ventilated and perfused lobes to overall lung function. Thus, the quantification parameters by SPECT/CT showed promise as an objective measure to predict the impact on function from surgical procedures and assessment of lung function for guiding localized treatments, e.g., lung volume reduction surgery or endobronchial valves in COPD, radio-ablation of airways, and responsiveness to mepolizumab in asthma [39,40,41].
Patients with COPD and asthma have a predominance of matched and reverse mismatched deficits, followed by mismatched deficits. SPECT/CT is more helpful in understanding the heterogeneity of the disease and can be used to characterize different phenotypes of COPD and asthma than other means of examination. Ventilation defects are usually more prominent than perfusion defects, even in mild patients, which leads to a reverse mismatched pattern. As the lungs attempt to match blood flow to ventilation to maintain optimal gas exchange efficiency, precapillary pulmonary vascular smooth muscle reflex contraction, or extrinsic vascular compression, ventilation abnormalities may lead to perfusion defects; this is a matched deficit [37, 42]. There is no clear explanation for mismatched defects (nonthromboembolic abnormalities). However, the disturbance of this relationship and the resulting heterogeneity are thought to be the leading cause of hypoxemia in most lung diseases and correlate with the severity of the disease [43, 44].
Our study expanded the spectrum of V/P SPECT/CT in respiratory diseases, including more SPECT-related parameters than previous studies, and compared its correlation with traditional pulmonary function parameters and CT pulmonary function and CT bronchial parameters. However, this study also had several limitations. First, the number of patients included in this study was insufficient, which may have affected the interpretation of more specific indicators. More extensive studies will be needed to overcome this issue. Second, although studies have confirmed the value of V/P SPECT/CT in the monitoring and prognostic assessment of the treatment response in COPD and asthma, this study did not follow up on this included cohort of patients. Further prospective studies are needed to confirm whether V/P SPECT/CT provides a basis for disease prognosis and treatment response, as well as for developing new therapeutic approaches and evaluation indicators.
Conclusions
Quantitative assessment of ventilation and perfusion abnormalities and the degree of pulmonary functional loss by V/P SPECT/CT shows promise as an objective measure to assess the severity of disease and lung function to guide localized treatments. There are differences between HRCT parameters and SPECT/CT parameters among the disease severity groups in asthma and COPD, which may enhance, to some extent, the understanding of complex physiological mechanisms in asthma and COPD. And the V/P SPECT parameters correlate to the partial PFTs and HRCT parameters. By assessing the distribution pattern of regional ventilation/perfusion and can be used as an alternative examination for patients with difficulty performing spirometry.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
NICE Evidence Reviews Collection. Evidence reviews for the length of corticosteroid use during exacerbations: Chronic obstructive pulmonary disease in over 16s: diagnosis and management: Evidence review J. London: National Institute for Health and Care Excellence (NICE) Copyright © NICE 2019; 2019.
Qaseem A, Wilt TJ, Weinberger SE, Hanania NA, Criner G, van der Molen T, et al. Diagnosis and management of stable chronic obstructive pulmonary disease: a clinical practice guideline update from the American College of Physicians, American College of Chest Physicians, American Thoracic Society, and European Respiratory Society. Ann Intern Med. 2011;155:179–91.
Labaki WW, Rosenberg SR. Chronic obstructive pulmonary disease. Ann Intern Med. 2020;173:Itc17-itc32.
Hogg JC, Timens W. The pathology of chronic obstructive pulmonary disease. Annu Rev Pathol. 2009;4:435–59.
Lapperre TS, Postma DS, Gosman MM, Snoeck-Stroband JB, ten Hacken NH, Hiemstra PS, et al. Relation between duration of smoking cessation and bronchial inflammation in COPD. Thorax. 2006;61:115–21.
Zhou-Suckow Z, Duerr J, Hagner M, Agrawal R, Mall MA. Airway mucus, inflammation and remodeling: emerging links in the pathogenesis of chronic lung diseases. Cell Tissue Res. 2017;367:537–50.
Hogg JC, Chu F, Utokaparch S, Woods R, Elliott WM, Buzatu L, et al. The nature of small-airway obstruction in chronic obstructive pulmonary disease. N Engl J Med. 2004;350:2645–53.
Su Y, Han W, Kovacs-Kasa A, Verin AD, Kovacs L. HDAC6 activates ERK in airway and pulmonary vascular remodeling of chronic obstructive pulmonary disease. Am J Respir Cell Mol Biol. 2021;65:603–14.
Park SW, Lim MN, Kim WJ, Bak SH. Quantitative assessment the longitudinal changes of pulmonary vascular counts in chronic obstructive pulmonary disease. Respir Res. 2022;23:29.
Pauwels RA, Buist AS, Calverley PM, Jenkins CR, Hurd SS. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. NHLBI/WHO Global Initiative for Chronic Obstructive Lung Disease (GOLD) Workshop summary. Am J Respir Crit Care Med. 2001;163:1256–76.
Wang C, Xu J, Yang L, Xu Y, Zhang X, Bai C, et al. Prevalence and risk factors of chronic obstructive pulmonary disease in China (the China Pulmonary Health [CPH] study): a national cross-sectional study. Lancet. 2018;391:1706–17.
Papi A, Brightling C, Pedersen SE, Reddel HK. Asthma. Lancet. 2018;391:783–800.
Fahy JV. Type 2 inflammation in asthma—present in most, absent in many. Nat Rev Immunol. 2015;15:57–65.
Kasahara K, Shiba K, Ozawa T, Okuda K, Adachi M. Correlation between the bronchial subepithelial layer and whole airway wall thickness in patients with asthma. Thorax. 2002;57:242–6.
Song WJ, Kang MG, Chang YS, Cho SH. Epidemiology of adult asthma in Asia: toward a better understanding. Asia Pac Allergy. 2014;4:75–85.
Koster TD, Klooster K, Ten Hacken NHT, van Dijk M, Slebos DJ. Endobronchial valve therapy for severe emphysema: an overview of valve-related complications and its management. Expert Rev Respir Med. 2020;14:1235–47.
Vestbo J, Hurd SS, Agustí AG, Jones PW, Vogelmeier C, Anzueto A, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med. 2013;187:347–65.
Battaglia S, den Hertog H, Timmers MC, Lazeroms SP, Vignola AM, Rabe KF, et al. Small airways function and molecular markers in exhaled air in mild asthma. Thorax. 2005;60:639–44.
Nuttall AGL, Velásquez W, Beardsmore CS, Gaillard EA. Lung clearance index: assessment and utility in children with asthma. Eur Respir Rev. 2019;28: 190046.
Şerifoğlu İ, Ulubay G. The methods other than spirometry in the early diagnosis of COPD. Tuberk Toraks. 2019;67:63–70.
Jarenbäck L, Ankerst J, Bjermer L, Tufvesson E. Flow-volume parameters in COPD related to extended measurements of lung volume, diffusion, and resistance. Pulm Med. 2013;2013: 782052.
Bajc M, Markstad H, Jarenbäck L, Tufvesson E, Bjermer L, Jögi J. Grading obstructive lung disease using tomographic pulmonary scintigraphy in patients with chronic obstructive pulmonary disease (COPD) and long-term smokers. Ann Nucl Med. 2015;29:91–9.
Satoh K, Nakano S, Tanabe M, Nishiyama Y, Takahashi K, Kobayashi T, et al. A clinical comparison between Technegas SPECT, CT, and pulmonary function tests in patients with emphysema. Radiat Med. 1997;15:277–82.
Jögi J, Ekberg M, Jonson B, Bozovic G, Bajc M. Ventilation/perfusion SPECT in chronic obstructive pulmonary disease: an evaluation by reference to symptoms, spirometric lung function and emphysema, as assessed with HRCT. Eur J Nucl Med Mol Imaging. 2011;38:1344–52.
Qin S, Yu X, Ma Q, Lin L, Li Q, Liu H, et al. Quantitative CT analysis of small airway remodeling in patients with chronic obstructive pulmonary disease by a new image post-processing system. Int J Chron Obstruct Pulmon Dis. 2021;16:535–44.
Graham BL, Steenbruggen I, Miller MR, Barjaktarevic IZ, Cooper BG, Hall GL, et al. Standardization of spirometry 2019 update. An Official American Thoracic Society and European Respiratory Society technical statement. Am J Respir Crit Care Med. 2019;200:e70–88.
Bajc M, Schümichen C, Grüning T, Lindqvist A, Le Roux PY, Alatri A, et al. EANM guideline for ventilation/perfusion single-photon emission computed tomography (SPECT) for diagnosis of pulmonary embolism and beyond. Eur J Nucl Med Mol Imaging. 2019;46:2429–51.
Jögi J, Jonson B, Ekberg M, Bajc M. Ventilation-perfusion SPECT with 99mTc-DTPA versus Technegas: a head-to-head study in obstructive and nonobstructive disease. J Nucl Med. 2010;51:735–41.
Bajc M, Olsson CG, Olsson B, Palmer J, Jonson B. Diagnostic evaluation of planar and tomographic ventilation/perfusion lung images in patients with suspected pulmonary emboli. Clin Physiol Funct Imaging. 2004;24:249–56.
Bajc M, Chen Y, Wang J, Li XY, Shen WM, Wang CZ, et al. Identifying the heterogeneity of COPD by V/P SPECT: a new tool for improving the diagnosis of parenchymal defects and grading the severity of small airways disease. Int J Chron Obstruct Pulmon Dis. 2017;12:1579–87.
Battaglia S, Mauad T, van Schadewijk AM, Vignola AM, Rabe KF, Bellia V, et al. Differential distribution of inflammatory cells in large and small airways in smokers. J Clin Pathol. 2007;60:907–11.
Hasegawa M, Nasuhara Y, Onodera Y, Makita H, Nagai K, Fuke S, et al. Airflow limitation and airway dimensions in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2006;173:1309–15.
Nakano Y, Müller NL, King GG, Niimi A, Kalloger SE, Mishima M, et al. Quantitative assessment of airway remodeling using high-resolution CT. Chest. 2002;122:271s-s275.
Pillai RA, Calhoun WJ. Introduction to asthma and phenotyping. Adv Exp Med Biol. 2014;795:5–15.
Davidson W, Bai TR. Lung structural changes in chronic obstructive pulmonary diseases. Curr Drug Targets Inflamm Allergy. 2005;4:643–9.
Sandek K, Bratel T, Lagerstrand L, Rosell H. Relationship between lung function, ventilation-perfusion inequality and extent of emphysema as assessed by high-resolution computed tomography. Respir Med. 2002;96:934–43.
Masiero PR, Menna-Barreto SS, Moreira MA, Mosmann MP, Mayer CM, Spiro BL. Perfused lung volume to thoracic gas volume ratio (perfused lung fraction) in patients with COPD and in controls. Nucl Med Commun. 2011;32:530–4.
Bailey DL, Farrow CE, Lau EM. V/Q SPECT-normal values for lobar function and comparison with CT volumes. Semin Nucl Med. 2019;49:58–61.
Wechalekar K, Garner J, Gregg S. Pre-surgical evaluation of lung function. Semin Nucl Med. 2019;49:22–30.
Kristiansen JF, Perch M, Iversen M, Krakauer M, Mortensen J. Lobar Quantification by Ventilation/Perfusion SPECT/CT in Patients with Severe Emphysema Undergoing Lung Volume Reduction with Endobronchial Valves. Respiration. 2019;98:230–8.
McDonald VM, Urroz PD, Bajc M, Rutherford N, Brooker B, Gibson PG. Imaging for precision medicine: can V-P SPECT measure mepolizumab response in asthma? Respirol Case Rep. 2021;9: e00717.
Weissmann N. Chronic obstructive pulmonary disease and pulmonary vascular disease. A comorbidity? Ann Am Thorac Soc. 2018;15:S278–81.
Frizzelli R, Lettieri C, Caiola S, Maulucci L, Pinzi C, Agostini F, et al. Unexplained hypoxemia in COPD with cardiac shunt. Respir Med Case Rep. 2022;37: 101661.
Amen EM, Becker EM, Truebel H. Analysis of V/Q-matching—a safety “biomarker” in pulmonary drug development? Biomarkers. 2011;16(Suppl 1):S5-10.
Acknowledgements
No potential conflicts of interest were disclosed.
Funding
The research was supported by the “1.3.5 Project for Disciplines of Excellence, West China Hospital, Sichuan University (ZYGD18016 and 2021HXFH033)”.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Xie, H., Zhao, Z., Zhang, W. et al. Quantitative analysis of lung function and airway remodeling using ventilation/perfusion single photon emission tomography/computed tomography and HRCT in patients with chronic obstructive pulmonary disease and asthma. Ann Nucl Med 37, 504–516 (2023). https://doi.org/10.1007/s12149-023-01848-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12149-023-01848-7