Abstract
Purpose
Chronic obstructive pulmonary disease (COPD) is characterized by airflow limitation which is not fully reversible. Despite the heterogeneity of COPD, its diagnosis and staging is currently based solely on forced expiratory volume in 1 s (FEV1). FEV1 does not explain the underlying pathophysiology of airflow limitation. The relationship between FEV1, symptoms and emphysema extent is weak. Better diagnostic tools are needed to define COPD. Tomographic lung scintigraphy [ventilation/perfusion single photon emission tomography (V/P SPECT)] visualizes regional V and P. In COPD, relations between V/P SPECT, spirometry, high-resolution computed tomography (HRCT) and symptoms have been insufficiently studied. The aim of this study was to investigate how lung function imaging and obstructive disease grading undertaken using V/P SPECT correlate with symptoms, spirometric lung function and degree of emphysema assessed with HRCT in patients with COPD.
Methods
Thirty patients with stable COPD were evaluated with the Medical Research Council dyspnoea questionnaire (MRC) and the clinical COPD questionnaire (CCQ). Spirometry was performed. The extent of emphysema was assessed using HRCT. V/P SPECT was used to assess V/P patterns, total reduction in lung function and degree of obstructive disease.
Results
The total reduction in lung function and degree of obstructive disease, assessed with V/P SPECT, significantly correlated with emphysema extent (r = 0.66–0.69, p < 0.0001) and spirometric lung function (r = 0.62–0.74, p < 0.0005). The correlation between emphysema extent and spirometric lung function was weaker. No correlation between MRC, CCQ and objective measurements was found.
Conclusion
V/P SPECT is sensitive to early changes in COPD. V/P SPECT also has the possibility to identify comorbid disease. V/P SPECT findings show a significant correlation with emphysema extent and spirometric lung function. We therefore recommend that scintigraphic signs of COPD, whenever found, should be reported. V/P SPECT can also be used to categorize the severity of functional changes in COPD as mild, moderate or severe.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Chronic obstructive pulmonary disease (COPD) is a preventable and treatable disease characterized by airflow limitation that is not fully reversible [1, 2]. COPD is a leading and increasing cause of morbidity and mortality [3]. Cigarette smoking, which causes inflammation in the lungs, is the most frequently encountered risk factor [2]. In patients with COPD, the inflammatory response is accentuated and small airways become persistently inflamed [4]. Chronic airflow limitation is caused by a combination of airway disease and parenchymal destruction (emphysema), the relative extent of which varies among patients [2]. COPD also leads to decreased gas transfer. The vascular system is affected, with an increased risk of ischaemic heart disease, congestive heart failure (CHF), pulmonary vascular changes and pulmonary embolism (PE) [5–7]. Hence, in patients with COPD, morphological and physiological changes, as well as disease manifestations such as dyspnoea, productive cough and exacerbations are heterogeneous [3].
Despite this extensive heterogeneity, the definition and severity of COPD is currently assessed with forced expiratory volume in 1 s (FEV1) alone [1, 2]. FEV1 measures the degree of airflow limitation but provides no information about the underlying pathophysiology. It is accepted that staging based only on FEV1 cannot capture and explain the complex clinical consequences of COPD [1, 8].
High-resolution computed tomography (HRCT) may provide morphological information about the extent of emphysema, its type and localization, but gives no functional evaluation. HRCT is not routinely recommended in COPD patients and correlation with FEV1 is weak [2, 9, 10]. Different questionnaires are used as a complement to assess symptoms, dyspnoea and functional state in COPD [11–13]. These scales predict prognosis, but correlate poorly with FEV1 [11, 14, 15]. Better tools to understand and categorize different phenotypes of COPD are requested [16].
Lung scintigraphy visualizes the distribution of ventilation and perfusion in the lungs. It is used primarily to detect PE but other conditions such as COPD, pneumonia and CHF may also be identified [17–19]. Despite the benefits of being able to delineate pathophysiological changes in COPD, at present lung scintigraphy is only recommended for emphysema patients where lung volume reduction procedures are being considered [1]. The introduction of three-dimensional ventilation/perfusion single photon emission tomography (V/P SPECT) has improved diagnostic accuracy in PE and facilitated recognition of other cardiopulmonary diseases [20–24]. Recently, Technegas, an ultrafine dispersion of 99mTc-labelled carbon particles, has been shown to be the aerosol of choice in COPD [25].
The role of V/P SPECT in the evaluation of COPD patients remains undefined. It may provide valuable information about functional abnormalities in COPD and so contribute to the classification of different phenotypes and to severity staging of COPD.
The aim of this study was to investigate how lung function imaging and obstructive disease grading undertaken with V/P SPECT correlate with symptoms, spirometric lung function and degree of emphysema assessed with HRCT in patients with COPD.
Materials and methods
Patients
After approval from the regional Ethics Review Board at Lund University, 30 consecutive patients were recruited from the hospital COPD outpatient clinic (for patient characteristics see Table 1). They had moderate to very severe COPD according to the Global Initiative for Obstructive Lung Disease classification [2]. All patients were clinically stable and free from exacerbation for at least 6 weeks prior to inclusion in the study. All patients were under optimized pharmacological treatment.
To avoid interpretation bias, the V/P SPECT images of the 30 patients with COPD were included with examination results of 33 other patients who had been clinically referred for V/P SPECT. Suspected PE was the most common reason for referral among these patients, 28 of whom had no known obstructive lung disease. These patients were only examined with V/P SPECT and were only used to include a full range of disease severity and patients with confounding disorders.
Symptoms
Dyspnoea was evaluated using the Medical Research Council (MRC) questionnaire, routinely used for grading the effect of breathlessness on daily activities [12]. It has been related to other measures of health status and prognosis [11, 14]. The MRC scale is graded from 1 to 5 and ranges from: not troubled by breathlessness except on strenuous exercise (1) to breathless when dressing or undressing (5) [12].
The clinical COPD questionnaire (CCQ) was used to measure symptoms and functional state. It has been validated for studies of clinical control in COPD patients [13]. The 10-item CCQ is self-administered and patients are instructed to recall symptoms experienced during the previous week. Each item is scored from 0 to 6 and the total CCQ score is then calculated by dividing the total sum by the number of items. Thus, CCQ ranges from 0 (very good control) to 6 (extremely poor control).
Spirometry and diffusion capacity for CO
FEV1, vital capacity (VC), total lung capacity (TLC), residual volume (RV), functional residual capacity (FRC) and diffusion capacity for carbon monoxide (DLCO) were measured using a body plethysmograph (MasterScreen Body/Diffusion; Viasys Healthcare). Spirometry was quality controlled according to the American Thoracic Society guidelines [26] and performed in accordance with Swedish Board for Accreditation and Conformity Assessment (SWEDAC) accreditation, fulfilling the requirements in ISO/IEC 17025. All measured values were expressed as % of predicted (e.g. %FEV1). The absolute ratio of FEV1/VC was also presented. The value of VC represents the best of forced VC (FVC) and slow VC.
HRCT
HRCT scanning, covering the whole lung, was performed with the patients in the supine position, using a multidetector CT scanner. Transaxial images, 1 mm thick, were reconstructed with the lung algorithm; 28 of 30 patients were examined with HRCT.
HRCT images were visually assessed with focus on emphysema type, its location and extent. The emphysema extent was scored as a percentage of the total lung volume (EmphysemaHRCT). Other findings such as bronchiectasis, thickening of bronchial wall and mucus plugs were also identified but not further analysed in this study. The review was performed by an experienced chest radiologist, blinded to V/P SPECT results.
V/P SPECT
V/P SPECT was performed according to the guidelines of the European Association of Nuclear Medicine (EANM) [17], as previously described [22, 27], fulfilling the requirements in ISO/IEC 17025. In short, a large field of view dual-head gamma camera with a low-energy all-purpose collimator was used. Acquisition was performed in a 64 × 64 matrix, zoomed to a pixel size of 6.8 mm with 128 projections over 360°. Sixty-four steps, each of 10 s duration, were used for the ventilation study, and of 5 s duration for the perfusion study. Total acquisition time was approximately 20 min which was well tolerated by all patients. V/P SPECT was performed as a 1-day protocol. The examination started with the inhalation of Technegas (Cyclomedica Ltd.) until 30 MBq had reached the lungs. Thereafter, ventilation tomography followed. After that, without patient movement and in carefully maintained supine position, 100–120 MBq of 99mTc-labelled macroaggregates of human albumin (Malinckrodt Medical BV) was slowly injected intravenously. Then, perfusion tomography was performed. The effective dose for this protocol is 1.8 mSv [25]. After reconstruction, V/P SPECT images were prepared for blinded review by an independent technologist.
Evaluation of V/P SPECT images
All V/P SPECT images were independently reviewed by two experienced physicians in accordance with a previously described scoring protocol [25]. A training session with the two physicians was held to achieve consistency of scoring. The physicians were blinded to all patient information. Ventilation images were visually reviewed first to evaluate three qualitative parameters: the unevenness of regional ventilation, central hot spots (i.e. deposition of aerosol in major and intermediate conductive airways) and peripheral hot spots (i.e. focal deposition of aerosol in distal airways). Each of these three parameters was graded from 0 (none) to 10 (very high). Thereafter, ventilation and perfusion images were reviewed together. The presence of regionally reduced ventilation and/or perfusion were assessed and described as matched (reduction in V = reduction in P), mismatched (P < V) or reverse mismatched (V < P) in accordance with the EANM guidelines [17]. The extent of V/P defects was expressed as a percentage of the total lung volume [28]. The total sum of the V/P defects was used to estimate the extent of total reduction in lung function (TotRedV/P SPECT) [28]. In accordance with other COPD terminology, the physicians graded the degree of obstructive disease (ObstrV/P SPECT), if present, as mild (approximately affecting < 20% of the lung function), moderate (20–50% approx.) or severe (> 50%). The physicians were permitted to use intermediate steps, e.g. mild-moderate. V/P SPECT images were finally reviewed according to clinical routine, assessing the presence of PE, CHF or other cardiopulmonary disease [19, 21, 22].
Statistics
The Spearman rank correlation test was used to calculate correlations between V/P SPECT, MRC, CCQ, spirometry and EmphysemaHRCT. The two-tailed Mann-Whitney U test was used for comparison of differences between groups. The null hypothesis was rejected when p < 0.05.
Results
Symptoms
The distribution of MRC and CCQ scores is shown in Fig. 1 and Table 1. Moderate correlation was seen between the MRC dyspnoea scale and the CCQ (r = 0.62, p < 0.001). Otherwise, no correlations were found between the two clinical questionnaires and spirometric parameters, V/P SPECT values or EmphysemaHRCT (Table 2).
HRCT
In 27 of 28 patients, HRCT showed signs of emphysema with a mean extent of 36% of the lung volume. Correlations between EmphysemaHRCT and other study parameters are shown in Table 2. With increasing EmphysemaHRCT, a moderate correlating decrease in FEV1/VC (r = −0.56, p = 0.002) (Fig. 2d), %FEV1/VC (r = −0.47, p = 0.012) and %DLCO (r = −0.42, p = 0.028) was seen. A moderate correlating increase in %TLC was observed (r = 0.50, p = 0.007). No significant correlation with %FEV1 was found.
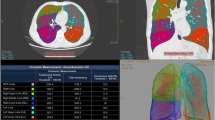
V/P SPECT
Among V/P SPECT variables, strong to very strong correlation (r = 0.79–0.99, p < 0.0001) was seen between unevenness of Technegas distribution (as seen in Fig. 3), peripheral hot spots (as seen in Fig. 4), TotRedV/P SPECT, matched defects and ObstrV/P SPECT (as seen in Fig. 5). To avoid colinearity problems, further correlation analysis was restricted to TotRedV/P SPECT and ObstrV/P SPECT (Table 2).
Patient with emphysema, predominantly in upper lobes on HRCT (total emphysema extent: 50%). Severe obstructive ventilation pattern with absent ventilation and hot spots in small airways. Perfusion is not affected to the same degree (black arrows). Minor infiltrates in the middle lobe (white arrow) with corresponding ventilation and perfusion defect
Patient with centrilobular emphysema with an extent of 50% of the lung volume on HRCT. V/P SPECT shows severe obstructive pattern with uneven ventilation and perfusion and hot spot formation. Extensive areas with reverse as well as matched ventilation/perfusion defects are found. Better perfused areas correspond to areas which are well ventilated (black arrows) and to better preserved parenchyma on HRCT (white arrows). Other areas appearing as hot spots on ventilation images are poorly perfused (dotted arrows)
With increasing TotRedV/P SPECT, there was a correlating decrease in %FEV1 (r = −0.62, p = 0.0003), absolute FEV1/VC ratio (r = −0.74, p < 0.0001) (Fig. 2a, c) and %FEV1/VC (r = −0.70, p < 0.0001). A moderate to strong positive correlation was seen with EmphysemaHRCT (r = 0.69, p < 0.0001) (Figs. 2e and 6) as well as a weak to moderate correlating rise in %TLC and %RV.
Extensive emphysema affecting 70% of the lung volume on HRCT. V/P SPECT shows large areas with no or minimal ventilation and perfusion in emphysematous areas in both lungs. Ventilation and perfusion are best preserved within central anterior parts of the upper lobes, where there is still some preserved parenchyma on HRCT
The higher the ObstrV/P SPECT, there was a correlating decrease in %FEV1 (r = −0.64, p = 0.0001), absolute FEV1/VC ratio (r = −0.71, p < 0.0001) (Fig. 2b) and %FEV1/VC (r = −0.67, p < 0.0001). There was a significant correlation between EmphysemaHRCT and ObstrV/P SPECT (r = 0.66, p = 0.0001) (Figs.4, 5 and 6).
ObstrV/P SPECT was in median 2.25 (range 0.25–3) in the COPD patients compared to 0 (range 0–1.25) in the 28 patients without any known obstructive disease (p < 0.0001). Only 3 of the 28 patients without any previously known obstructive disease were scintigraphically categorized as having mild obstructive disease.
Minor mismatched perfusion defects (≤ 20%) were found in 10 of the 30 patients. In three of these cases, both physicians regarded the findings as consistent with PE, as they were of segmental character.
In four patients, a pattern with redistribution of perfusion to nondependent lung zones indicating CHF was seen [19]. Three of these patients had a history of either multiple myocardial infarctions with moderately decreased left ventricular function, known episodes of CHF or chronic atrial fibrillation.
Discussion
In patients with COPD, reduction of total lung function (TotRedV/P SPECT) and grade of obstructive disease (ObstrV/P SPECT) correlated well with both spirometric lung function and emphysema extent (EmphysemaHRCT). The correlation between EmphysemaHRCT and spirometric lung function was weaker.
The MRC dyspnoea and the CCQ scales showed no significant correlations either to spirometry, V/P SPECT or emphysema extent. MRC and CCQ can be used to predict morbidity and mortality when applied to populations, but already the developers of these scales found that the correlation to objective lung function tests, such as FEV1, was weak or absent [11, 13]. This is also seen within this sample of COPD patients. The degree of functional impairment, dyspnoea and symptoms apparently do not relate to absolute measures of lung function, but probably simply indicate the individual’s subjective experience of inability with his or her own habitual level as reference. The discrepancy between subjective symptoms and lung function impairment is also one of the reasons why COPD diagnosis often is delayed.
Increased resistance of small conducting airways and the emphysematous parenchyma destruction seen in COPD affect both regional ventilation and perfusion. As seen in this study and others, these V/P changes can be observed using lung scintigraphy (Figs. 3, 4, 5 and 6). This has previously been regarded mostly as a problem, obstructing interpretation of lung scintigraphy with regards to PE [29]. This attitude is undergoing a shift since the introduction of the three-dimensional V/P SPECT technique [17]. V/P SPECT offers great advantages over planar imaging [17, 20–24, 30, 31]. It has not only improved the diagnostic accuracy for PE but may also facilitate diagnosis of other cardiopulmonary diseases, like COPD and CHF [19, 21, 25]. Despite this, there are few systematic studies of how ventilation and perfusion patterns correlate to different phenotypes of COPD. It is clear that the potential of V/P SPECT to improve our understanding of the pathophysiology of COPD needs to be explored more fully [16]. This study is the first, to our knowledge, that systematically compares V/P SPECT with clinical symptoms, functional state, extent of emphysema and the degree of spirometric airway obstruction, as well as using V/P SPECT to identify comorbid disease.
COPD is today regarded as a treatable and preventable disease [1, 2]. Early detection is essential as it encourages people to give up smoking, which is the most effective way to prevent or delay airflow limitation in COPD [32]. FEV1 is a rather insensitive method in detecting airway changes in COPD as these mainly occur in small airways. Ventilation lung scintigraphy is a more sensitive indicator of obstructive lung disease than spirometric flow rates and lung volumes [33]. In previous studies, V/P SPECT has also shown to be more sensitive than HRCT in identifying small airway disease and emphysema [34, 35]. In the present study, this was confirmed and reduced lung function, as a sign of small airway disease, was identified with V/P SPECT even in regions with normal appearance on HRCT (Figs.2e and 3). The effective radiation dose from V/P SPECT is also considerably lower than the radiation dose from HRCT [30].
Different V/P abnormalities observed with lung scintigraphy in COPD and emphysema have been described in the literature, including general unevenness of radiopharmaceutical distribution, central and peripheral hot spots, mismatch, reverse mismatch and matched defects [33, 36]. These patterns are often simultaneously present in COPD, and the finding of high to very high correlations between them in our study is therefore not surprising. Further studies of the functional implications of these different V/P patterns may well increase our understanding of different phenotypes of COPD. Central hot spots have been associated with increased resistance in major and intermediate airways, disturbing the conductive flow and thus leading to impaction of radioaerosol particles (Fig. 5) [36]. This is seen in asthma and in COPD. In severe cases, the presence of central hot spots may make it difficult to evaluate peripheral parts of the lung. The use of Technegas has nearly eliminated this problem [25]. Peripheral hot spot formation is seen in uneven ventilation and is associated with small airway disease with obstruction of peripheral airways (Fig. 4) [36]. In severe COPD, well-functioning regions may sometimes appear as relative “hot spots” (Fig. 5), but actually represent areas with preserved and matched ventilation and perfusion.
Matched reduction of both ventilation and perfusion can be seen with parenchyma destruction in emphysema (Fig. 6), but can also be due to hypoxic vasoconstriction and diversion of blood flow from poorly ventilated areas. In our study, the extent of matched defects increased with increasing degree of emphysema. In this way both ventilation and perfusion are reduced and the V/P imbalance is somewhat buffered. This could be one explanation as to why analysis focusing on V/P ratio dispersion has not been able to separate different degrees of COPD [37].
We found that reverse mismatch (V < P) already can be present in mild COPD (Fig. 3). It can be a sign of airway disease with incomplete hypoxic vasoconstriction that could lead to shunting and hypoxaemia (Fig. 6) [38]. Reverse mismatch might also be seen in pneumonia [18].
Segmental mismatch (P < V) is the fundamental criterion for PE diagnosis [17]. Because PE is common among COPD patients, it is important to diagnose [6]. Three of the COPD patients in our study had findings consistent with PE and another seven COPD patients had mismatched defects of nonsegmental character. The findings of mismatch in small areas could represent PE but may also be caused by local vascular remodelling or vascular obliteration seen in COPD.
CHF is another common comorbidity in COPD patients that is important to diagnose [5]. In patients with COPD, the prevalence of CHF has been reported to be ≥ 20%, but the diagnosis is often missed due to overlapping symptoms [39]. Four COPD patients (13%) showed a scintigraphic pattern of CHF, which has been found to have a high positive predictive value [19]. According to patient records, three of four of these patients had either CHF or other known heart disease.
The sensitivity of V/P SPECT, as an indicator of airway obstruction, in combination with the moderate to strong correlations of TotRedV/P SPECT to spirometry and EmphysemaHRCT indicate a role for functional V/P SPECT imaging, as a bridge between spirometry and morphology in COPD. The grading of obstructive disease (ObstrV/P SPECT) used in this study strongly correlates to FEV1/VC and shows a substantial correlation to both %FEV1 and EmphysemaHRCT. In the COPD patients, where reduction of lung function is primarily caused by obstructive changes, ObstrV/P SPECT is very strongly correlated to TotRedV/P SPECT. However, the correlation between TotRedV/P SPECT and ObstrV/P SPECT in the patients without known obstructive disease is considerably lower (r = 0.39, p = 0.04). In these patients the reduced lung function, if present, is primarily caused by other conditions. As expected, there was also a significant difference in ObstrV/P SPECT between patients with COPD and those without obstructive disease. Worth mentioning is that only 3 of the 28 patients without known obstructive disease were classified as having mild obstructive disease by the blinded reviewers.
V/P SPECT has the unique possibility to image functional changes in regional ventilation and perfusion and to quantify the proportion of functional loss that is caused by matched, mismatched or reversed mismatched defects, respectively. This knowledge can be used to characterize different phenotypes of COPD, which is important, as the degree of airway obstruction and emphysema varies among patients. In this study, we also show that V/P SPECT gives the possibility not only to diagnose COPD but also to grade its severity. Furthermore, we show that V/P SPECT can be used to identify comorbid disease even in the presence of severe COPD.
Although larger studies are needed, our findings indicate the possibility to implement V/P SPECT in the diagnosis, staging and classification of COPD.
Conclusion
V/P SPECT is a sensitive method to detect early changes in COPD. V/P SPECT also has the possibility to identify comorbid disease. Functional V/P SPECT findings show moderate to strong correlations to morphological emphysema extent and spirometric lung function. We therefore recommend that scintigraphic signs of COPD, whenever found, should be reported. V/P SPECT can also be used to categorize the severity of functional changes in COPD as mild, moderate or severe.
References
Celli BR, MacNee W, ATS/ERS Task Force. Standards for the diagnosis and treatment of patients with COPD: a summary of the ATS/ERS position paper. Eur Respir J 2004;23:932–46.
Rabe KF, Hurd S, Anzueto A, Barnes PJ, Buist SA, Calverley P, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med 2007;176:532–55.
Mannino DM. COPD: epidemiology, prevalence, morbidity and mortality, and disease heterogeneity. Chest 2002;121:121S–6S.
Hogg JC, Chu F, Utokaparch S, Woods R, Elliott WM, Buzatu L, et al. The nature of small-airway obstruction in chronic obstructive pulmonary disease. N Engl J Med 2004;350:2645–53. doi:10.1056/NEJMoa032158.
Holguin F, Folch E, Redd SC, Mannino DM. Comorbidity and mortality in COPD-related hospitalizations in the United States, 1979 to 2001. Chest 2005;128:2005–11. doi:10.1378/chest.128.4.2005.
Stein PD, Beemath A, Meyers FA, Olson RE. Pulmonary embolism and deep venous thrombosis in hospitalized adults with chronic obstructive pulmonary disease. J Cardiovasc Med (Hagerstown) 2007;8:253–7.
Voelkel NF, Cool CD. Pulmonary vascular involvement in chronic obstructive pulmonary disease. Eur Respir J Suppl 2003;46:28s–32s.
Jones PW, Agusti AG. Outcomes and markers in the assessment of chronic obstructive pulmonary disease. Eur Respir J 2006;27:822–32.
Cerveri I, Dore R, Corsico A, Zoia MC, Pellegrino R, Brusasco V, et al. Assessment of emphysema in COPD: a functional and radiologic study. Chest 2004;125:1714–8.
Gelb AF, Hogg JC, Müller NL, Schein MJ, Kuei J, Tashkin DP, et al. Contribution of emphysema and small airways in COPD. Chest 1996;109:353–9.
Bestall JC, Paul EA, Garrod R, Garnham R, Jones PW, Wedzicha JA. Usefulness of the Medical Research Council (MRC) dyspnoea scale as a measure of disability in patients with chronic obstructive pulmonary disease. Thorax 1999;54:581–6.
Fletcher CM, Elmes PC, Fairbairn A, Wood CH. The significance of respiratory symptoms and the diagnosis of chronic bronchitis in a working population. Br Med J 1959;2:257–66.
van der Molen T, Willemse BW, Schokker S, ten Hacken NH, Postma DS, Juniper EF. Development, validity and responsiveness of the Clinical COPD Questionnaire. Health Qual Life Outcomes 2003;1:13.
Nishimura K, Izumi T, Tsukino M, Oga T. Dyspnea is a better predictor of 5-year survival than airway obstruction in patients with COPD. Chest 2002;121:1434–40.
Wolkove N, Dajczman E, Colacone A, Kreisman H. The relationship between pulmonary function and dyspnea in obstructive lung disease. Chest 1989;96:1247–51.
Mannino DM, Watt G, Hole D, Gillis C, Hart C, McConnachie A, et al. The natural history of chronic obstructive pulmonary disease. Eur Respir J 2006;27:627–43. doi:10.1183/09031936.06.00024605.
Bajc M, Neilly JB, Miniati M, Schuemichen C, Meignan M, Jonson B, et al. EANM guidelines for ventilation/perfusion scintigraphy: part 1. Pulmonary imaging with ventilation/perfusion single photon emission tomography. Eur J Nucl Med Mol Imaging 2009;36:1356–70.
Freeman LM, Krynyckyi B, Zuckier LS. Enhanced lung scan diagnosis of pulmonary embolism with the use of ancillary scintigraphic findings and clinical correlation. Semin Nucl Med 2001;31:143–57.
Jögi J, Palmer J, Jonson B, Bajc M. Heart failure diagnostics based on ventilation/perfusion single photon emission computed tomography pattern and quantitative perfusion gradients. Nucl Med Commun 2008;29:666–73.
Bajc M, Bitzén U, Olsson B, Perez de Sá V, Palmer J, Jonson B. Lung ventilation/perfusion SPECT in the artificially embolized pig. J Nucl Med 2002;43:640–7.
Bajc M, Olsson B, Palmer J, Jonson B. Ventilation/perfusion SPECT for diagnostics of pulmonary embolism in clinical practice. J Intern Med 2008;264:379–87.
Bajc M, Olsson CG, Olsson B, Palmer J, Jonson B. Diagnostic evaluation of planar and tomographic ventilation/perfusion lung images in patients with suspected pulmonary emboli. Clin Physiol Funct Imaging 2004;24:249–56.
Gutte H, Mortensen J, Jensen CV, von der Recke P, Petersen CL, Kristoffersen US, et al. Comparison of V/Q SPECT and planar V/Q lung scintigraphy in diagnosing acute pulmonary embolism. Nucl Med Commun 2010;31:82–6. doi:10.1097/MNM.0b013e3283336747.
Reinartz P, Wildberger JE, Schaefer W, Nowak B, Mahnken AH, Buell U. Tomographic imaging in the diagnosis of pulmonary embolism: a comparison between V/Q lung scintigraphy in SPECT technique and multislice spiral CT. J Nucl Med 2004;45:1501–8.
Jögi J, Jonson B, Ekberg M, Bajc M. Ventilation-perfusion SPECT with 99mTc-DTPA versus Technegas: a head-to-head study in obstructive and nonobstructive disease. J Nucl Med 2010;51:735–41. doi:10.2967/jnumed.109.073957.
Standardization of Spirometry, 1994 Update. American Thoracic Society. Am J Respir Crit Care Med 1995;152:1107–36.
Palmer J, Bitzén U, Jonson B, Bajc M. Comprehensive ventilation/perfusion SPECT. J Nucl Med 2001;42:1288–94.
Olsson CG, Bitzén U, Olsson B, Magnusson P, Carlsson MS, Jonson B, et al. Outpatient tinzaparin therapy in pulmonary embolism quantified with ventilation/perfusion scintigraphy. Med Sci Monit 2006;12:PI9–13.
Value of the ventilation/perfusion scan in acute pulmonary embolism. Results of the prospective investigation of pulmonary embolism diagnosis (PIOPED). The PIOPED Investigators. JAMA 1990;263:2753–9.
Bajc M, Neilly JB, Miniati M, Schuemichen C, Meignan M, Jonson B. EANM guidelines for ventilation/perfusion scintigraphy: part 2. Algorithms and clinical considerations for diagnosis of pulmonary emboli with V/P(SPECT) and MDCT. Eur J Nucl Med Mol Imaging 2009;36:1528–38.
Leblanc M, Leveillée F, Turcotte E. Prospective evaluation of the negative predictive value of V/Q SPECT using 99mTc-Technegas. Nucl Med Commun 2007;28:667–72.
Sundblad BM, Larsson K, Nathell L. Lung function testing influences the attitude toward smoking cessation. Nicotine Tob Res 2010;12:37–42. doi:10.1093/ntr/ntp170.
Taplin GV, Tashkin DP, Chopra SK, Anselmi OE, Elam D, Calvarese B, et al. Early detection of chronic obstructive pulmonary disease using radionuclide lung-imaging procedures. Chest 1977;71:567–75.
Satoh K, Nakano S, Tanabe M, Nishiyama Y, Takahashi K, Kobayashi T, et al. A clinical comparison between Technegas SPECT, CT, and pulmonary function tests in patients with emphysema. Radiat Med 1997;15:277–82.
Yokoe K, Satoh K, Yamamoto Y, Nishiyama Y, Asakura H, Haba R, et al. Usefulness of 99mTc-Technegas and 133Xe dynamic SPECT in ventilatory impairment. Nucl Med Commun 2006;27:887–92.
Santolicandro A, Ruschi S, Fornai E, Giuntini C. Imaging of ventilation in chronic obstructive pulmonary disease. J Thorac Imaging 1986;1:36–53.
Rodríguez-Roisin R, Drakulovic M, Rodríguez DA, Roca J, Barberà JA, Wagner PD. Ventilation-perfusion imbalance and chronic obstructive pulmonary disease staging severity. J Appl Physiol 2009;106:1902–8. doi:10.1152/japplphysiol.00085.2009.
Palmaz JC, Barnett CA, Reich SB, Krumpe PE, Farrer PA. Reverse ventilation–perfusion mismatch. Clin Nucl Med 1984;9:6–9.
Rutten FH, Cramer MJ, Lammers JW, Grobbee DE, Hoes AW. Heart failure and chronic obstructive pulmonary disease: an ignored combination? Eur J Heart Fail 2006;8:706–11. doi:10.1016/j.ejheart.2006.01.010.
Acknowledgements
This study was partially financed by the Region of Scania (ALF). The Clinical COPD questionnaire (CCQ) was used with kind permission from the author [13].
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jögi, J., Ekberg, M., Jonson, B. et al. Ventilation/perfusion SPECT in chronic obstructive pulmonary disease: an evaluation by reference to symptoms, spirometric lung function and emphysema, as assessed with HRCT. Eur J Nucl Med Mol Imaging 38, 1344–1352 (2011). https://doi.org/10.1007/s00259-011-1757-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-011-1757-5