Abstract
Objective
The utility of serum thyroglobulin (Tg) level, 3 days after radioactive iodine (RAI) therapy, was assessed as a means of predicting successful ablation of thyroid remnant in patients with postoperative thyroid cancer.
Methods
A total of 152 patients with thyroid cancer (mean age = 44.9 ± 13.7 year) undergoing RAI therapy after total thyroidectomy were included. Levels of TSH-stimulated Tg prior to ablation (stimTg) and serum Tg sampled immediately after RAI therapy (Day 3) were measured (immTg). ImmTg samples were collected during patient hospital visits for scheduled follow-up of radioiodine scans. Successful ablation was determined by the second time stimulated Tg levels (≤1 ng/ml) and negative radioiodine uptake at thyroid bed after 6.1 ± 1.1 months of RAI therapy. Univariate and multivariate analyses were done for immTg, stimTg, change in Tg levels (deltaTg: immTg − stimTg), immTg:stimTg ratio (ratioTg), and other potential clinical and pathologic markers of successful ablation.
Results
Of selected laboratory variables, ratioTg was a significant predictor of successful ablation. StimTg, tumor diameter, metastatic lymph node (LN) numbers, lymphatic invasion were possible clinical markers of successful ablation by univariate analysis. By multivariate analysis, ratioTg (odds ratio = 7.851), stimTg (odds ratio = 16.819), metastatic LN numbers (odds ratio with stimTg = 6.732) proved significant results. Furthermore, combining high ratioTg and low stimTg provided added predictive value.
Conclusions
High ratioTg (reflecting extensive release of Tg to the blood after RAI therapy) and low stimTg (reflecting small remnant thyroid tissue) constitute the indices of successful ablation after RAI therapy. Immediate Tg level could give an useful information on RAI ablation of postoperative thyroid remnant.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Radioiodine (RAI) therapy after total or near-total thyroidectomy is an effective means of ablating postoperative remnants of thyroid tissue. By eliminating normal thyroid tissue, tumor recurrence or metastasis are easily monitored using follow-up RAI scans and serum thyroglobulin (Tg) level. In addition, microscopic foci of cancer or minor recurrences may be eradicated by the initial RAI therapy [1]. Successful remnant ablation after total thyroidectomy is recommended in high-risk groups, such as large thyroid cancer involving extrathyroidal extension or metastasis (regional or remote) [2, 3], to improve patient outcomes [4, 5].
Unfortunately, RAI therapy is not always successful at first attempt. In about 20–30 % of patients, the initial RAI therapy did not reach the successful ablation [6], so repeated RAI therapy or other treatment options are needed [7]. Consequently, markers to predict successful ablation might help ensure proper patient care. The level of TSH-stimulated Tg (stimTg) obtained prior to RAI therapy has been a well-known predictor of successful ablation [8–10]. However, false-negative results are common with recurrent or metastatic thyroid cancer [11], needing better predictive marker. Other parameters, such as a high Tg to TSH × 24-h 131I uptake ratio [12], stage of thyroid cancer [9], extrathyroidal tumor extension [13], and lymph node or distant metastasis [5] have also been insisted for successful ablation predictor with some controversies.
In theory, exposure to 131I should eradicate normal thyroidal tissue in a few days, resulting in destruction of cellular membrane integrity. As consequences, the stored Tg in thyroid follicle enter the blood, and induces high blood level of Tg. A recent retrospective study by Bernier et al. [14], evaluating Tg levels 5 days after RAI therapy (TgD5), indicated that the ratio of post- to pre-therapeutic values (TgD5:TgD0) can be a predictive marker. It has been proposed that Tg levels immediately after RAI therapy may predict the successful ablation of remnant thyroid tissue. However, no following research is conducted as far as we know.
Given the half-life of serum Tg (65 h) [15] and competing scheduling issues (i.e., follow-up scans), we examined serum levels of Tg immediately (Day 3) after RAI therapy (immTg). We compared other pathologic and clinical variables for prediction of successful remnant thyroid ablation. The purpose was to find a reliable predictor of successful ablation in Korean patients following surgery for thyroid cancer.
Materials and methods
Patient selection
From March 2011 to June 2013, 152 thyroid cancer patients (female:male = 112:40; mean age = 44.9 ± 13.7 year) undergoing RAI therapy [mean RAI dose = 4.0 ± 1.1 GBq (108.6 ± 28.5 mCi)] and post-therapeutic follow-up scans (131I or 123I) at our institute were studied. The study design was approved by the Institutional Review Board (IRB) at out institute. Total thyroidectomy had been done for differentiated thyroid cancer (papillary thyroid cancer, 144; follicular thyroid cancer, 8). Mean diameter of primary tumors was 1.6 ± 1.1 cm (range 0.2–7.0), with mean metastatic lymph node (LN) number found at surgery was 5.7 ± 7.1 (range 0–46) (Table 1). Patients with distant metastases were excluded. As potential indices of successful ablation, stimTg [TSH-stimulated (>30 mU/L) serum Tg prior to RAI therapy] and immTg [serum Tg immediately (Day 3) after RAI therapy] were measured. The change in Tg levels (deltaTg: immTg–stimTg) and immTg:stimTg ratio (ratioTg) were also included as possible predictive markers.
Measurement of laboratory variables
Serum thyroid stimulating hormone (TSH) levels were determined by immunoradiometric assay (IRMA) (TSH-CTK-3, DiaSorin, Saluggia, Italy), with analytic sensitivity (AS) and functional sensitivity (FS) of 0.04 and 0.07 mU/L, respectively. The cut-point for TSH, above which corresponding stimTg levels were acceptable, was 30 mU/L. Brahms kits (RIA Tg-plus; Berlin, GmbH, Hennigsdorf, Germany) were used to measure immTg and stimTg (AS, 0.08 ng/ml; FS, 0.2 ng/ml) and serum autoantibodies to thyroglobulin (anti-TgAb) (AS, 5.5 U/ml; FS < 20 U/ml). The inclusion criteria of stimTg was ≥0.2 ng/ml, which was the least detectable range. The exclusion criteria of anti-TgAb was ≥100 U/mL, to exclude the effect of stimTg and ImmTg.
Whole body scan
131I whole body scan was performed 3 days after oral ingestion of 131I. Thyroid hormone replacement therapy was discontinued in all patients 4 weeks prior to scans, and all of the patients met the elevated TSH level (>30 mU/L) at the time of scanning. A large field-of-view gamma camera (ON 410, Ohio Nuclear, Solon, OH, USA) with medium-energy parallel-hole collimator was used. A 20 % symmetric window was centered at 364 keV. Anterior images of the neck, chest, and abdomen were obtained, and a minimum of 100,000 counts was collected per image. After the whole body scan, thyroid replacement therapy was restarted. Follow-up scan was performed in the same way 3 days after ingestion of 131I [1.11 GBq (30 mCi)] or 123I [148 MBq (4 mCi)]. A 20 % symmetric window was centered at 159 keV for 123I whole body scan.
Final assessment of remnant ablation
Successful ablation (n = 81) was defined as follows: no remnant tissue on follow-up 131I or 123I scans and the second time stimulated Tg ≤ 1 ng/ml at 6.1 ± 1.1 months after RAI therapy. Patients not satisfying both conditions (n = 71) were believed to have remnant thyroid tissue.
Clinical variables
Clinical variables, including age, gender (F vs. M) and RAI dose were analyzed as potential predictive markers. Age and RAI dose were grouped to continuous parameters, and gender was allocated to categorical parameter.
Pathologic variables
Tumor largest diameter and metastatic LN numbers (which were found at surgery) were added as pathologic variables. In addition, the status (boolean: no or yes) of possible predictive factors (lymphatic invasion, multicentricity, blood vessel invasion, extrathyroidal extension, resection margins, and BRAF mutation), tumor pathology (FTC vs. PTC) were also assessed.
Statistical analysis
Independent-samples T test and receiver operation characteristic (ROC) curve analysis were done to find statistically significant (p < 0.05) and statistical trend (0.05 ≤ p < 0.1) parameters, and determined area under the curve (AUC), p value, cut-off value, sensitivity (%), and specificity (%). Odds ratio (OR) and p value of each categorical parameters were generated via Chi square analysis. Multivariate analysis was used to assess significant variables and establish OR. Statistical significance was set at p < 0.05. All computations relied on standard software using SPSS (Version 18.0; SPSS Inc., Chicago, IL, USA) and MedCalc (Version 12.2; MedCalc Inc., Mariakerke, Belgium).
Results
Univariate analysis
Small number of metastatic LN numbers (p < 0.001) and high ratioTg (p < 0.001) served to predict successful ablation with statistical significance (Table 2). ROC curve analysis indicated the following: (1) 70.4 % sensitivity and 85.9 % specificity for stimTg (cut-off ≤ 2.0, AUC = 0.828, p < 0.001); and (2) 59.3 % sensitivity and 85.9 % specificity for ratioTg, (cut-off ≥ 12.0 AUC = 0.785, p < 0.001) (Table 3). By Chi square analysis, statistical significance was identified to negative lymphatic invasion of thyroid cancer in predicting successful ablation (p = 0.001) (Table 4).
Multivariate analysis
RatioTg, stimTg, gender, tumor largest diameter, lymphatic invasion and metastatic LN numbers were parameters to multivariate analysis. Continuous variables (ratioTg, stimTg, and mLN count) were stratified by cut-off values, according to ROC curve analysis. Of six candidate variables, ratioTg (OR = 7.851, p < 0.001), stimTg (OR = 16.819, p < 0.001), metastatic LN numbers [OR = 3.028 (with ratioTg, p = 0.018), 6.732 (with stimTg, p < 0.001)] showed significance in predicting successful ablation (Table 5).
Combination of ratioTg and stimTg for remnant ablation prediction
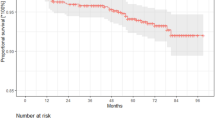
High ratioTg or low stimTg combined value (defined either positive as successful ablation) showed higher sensitivity (91.4 %, 74/81), negative predictive value (88.5 %, 54/61), accuracy (84.2 %, 128/152), and Kappa index (0.680) than each parameters. High ratioTg and low stimTg combined value (defined both positive as successful ablation) showed greater specificity (95.8 %, 68/71) and positive predictive value (91.2 %, 31/34) than each parameters (Table 6; Fig. 1).
Additional value of ratioTg for prediction of successful ablation. Intense uptake of remnant tissue was detected in the initial 131I whole body scan (a) and successful ablation was observed in following scan (b). ImmTg and stimTg was 336.7 and 14.1 ng/ml, respectively. RatioTg was was 23.8 and the 2nd time stimulated Tg was normalized to 0.1 ng/ml
Discussion
High ratioTg (immTg:stimTg ratio) was valuable in predicting successful ablation after RAI treatment. High ratioTg showed the highest specificity of all variables assessed. By multivariate analysis, high ratioTg displayed statistical significance as a marker of successful ablation, in addition to low stimTg and small numbers of metastatic LNs; and predictive value was strengthened by combining ratioTg and stimTg.
Generally, stimTg is used to predict successful remnant ablation [9], judging RAI therapy response [13], detecting tumor recurrence [16, 17], forecasting disease recurrence [18, 19], anticipating prognosis [20, 21] and more. There have been a number of studies demonstrating that pre-ablation stimTg is a predictive marker of thyroidal remnants, and our findings do support this contention [13].
However, false-positive and false-negative rates of pre-ablation stimTg are about 30 %, respectively [9]. Tg is a large (660 kDa) protein with more than 20 epitopes. And because the antibodies of conventional kits are different, serum Tg determinations may vary accordingly [22]. In external quality control data (Korean), we found that Tg levels generated via immunoradiometric assay (IRMA) have about 10 % coefficient of variance. Since Tg is a normal component of thyroid follicular cell, but not a conventional tumor marker like carcinoembryonic antigen (CEA) and alpha-fetoprotein (α-FP), serum Tg level might show higher false-positive and negative results in detecting residual or recurrent thyroid cancer.
The basis for the predictive value of ratioTg is detailed in a study of external radiotherapy, describing the damage suffered by residual thyroidal tissue [23, 24]. Thyroid tissue apoptosis after radiotherapy induces destruction of membrane integrity. As a result, storaged Tg release at the thyroid tissue after radiation results in high level of serum Tg at acute phase. In the same way, high ratioTg corresponds with early response to RAI therapy. High ratioTg means early release of storaged Tg at remnant thyroid tissue, which means early thyroid tissue destruction and good response of RAI therapy. Hence, ratioTg is an index of RAI therapeutic response with high specificity, while stimTg is a marker of residual thyroid tissue irrespective of RAI therapy in theory. We think that ratioTg is superior to stimTg as a predictive marker for successful ablation and expect it to be similarly investigated in cases of metastatic thyroid cancer.
Compared with an earlier study by Bernier et al. [14], our design was advantageous in terms of patient scheduling and accessibility (Day 3). Samples for immTg were collected when patients presented for 131I post-therapeutic scans. To our knowledge, only one study [14] has focused on serum Tg immediately following RAI therapy previously and showed the similar results with our study. Comparative study according to the sampling date of serum Tg (Day 3 vs. Day 5) immediately following RAI therapy is needed in the future.
As in our work, numbers of metastatic LN were seen as a predictive marker in a previous univariate analysis [5]. Our study also supports the previous study. However, the validity of metastatic LN numbers predicts remnant ablation has been debated. Additional research is needed to elucidate the potential benefit of predicting RAI therapy response.
Our study does have limitations. The many variables analyzed may have clouded our results to some degree, and due to the retrospective nature of clinical and pathologic assessment, some desired parameters (such as capsular invasion) could not be included for the lack of data. In addition, differences of serum TSH level before and 3 days after the RAI therapy could be a confounding factor. While our patients showed no statistical differences of TSH measurement between before RAI therapy (104.6 ± 66.0 mU/L, range 32.3–434.0) and 3 days after RAI therapy (119.8 ± 64.8 mU/L, range 32.8–480.0), the effect of TSH should be considered in the future study. Finally, the patient subgroups studied were relatively small. A prospective analysis is warranted to better determine the merit of immTg in managing thyroid cancer.
In conclusion, high ratioTg and low stimTg showed most significant results for prediction of remnant ablation and ratioTg showed the additional value in combination with stimTg. The reason for prediction of remnant ablation by high ratioTg might be early response of thyroid follicular cell damage. We expect ratioTg to be routine work up for prediction of successful remnant ablation. Thus, serum level of immediate Tg could give an useful information on RAI ablation of postoperative thyroid remnant.
References
Verburg FA, Dietlein M, Lassmann M, Luster M, Reiners C. Why radioiodine remnant ablation is right for most patients with differentiated thyroid carcinoma. Eur J Nucl Med Mol Imaging. 2009;36:343–6.
Pacini F, Schlumberger M, Harmer C, Berg GG, Cohen O, Duntas L, et al. Post-surgical use of radioiodine (131I) in patients with papillary and follicular thyroid cancer and the issue of remnant ablation: a consensus report. Eur J Endocrinol. 2005;153:651–9.
Cooper DS, Doherty GM, Haugen BR, Kloos RT, Lee SL, Mandel SJ, et al. Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid. 2009;19:1167–214.
Sawka AM, Thephamongkhol K, Brouwers M, Thabane L, Browman G, Gerstein HC. Clinical review 170: a systematic review and metaanalysis of the effectiveness of radioactive iodine remnant ablation for well-differentiated thyroid cancer. J Clin Endocrinol Metab. 2004;89:3668–76.
Verburg FA, de Keizer B, Lips CJ, Zelissen PM, de Klerk JM. Prognostic significance of successful ablation with radioiodine of differentiated thyroid cancer patients. Eur J Endocrinol. 2005;152:33–7.
Karam M, Gianoukakis A, Feustel P, Cheema A, Postal E, Cooper J. Influence of diagnostic and therapeutic doses on thyroid remnant ablation rates. Nucl Med Commun. 2003;24:489–95.
Paeng JC, Kang KW, Oh SW, Chung JK. Alternative medical treatment for radioiodine-refractory thyroid cancers. Nucl Med Mol Imaging. 2011;45:241–7.
Vaisman A, Orlov S, Yip J, Hu C, Lim T, Dowar M, et al. Application of post-surgical stimulated thyroglobulin for radioiodine remnant ablation selection in low-risk papillary thyroid carcinoma. Head Neck. 2010;32:689–98.
Kendler DB, Vaisman F, Corbo R, Martins R, Vaisman M. Preablation stimulated thyroglobulin is a good predictor of successful ablation in patients with differentiated thyroid cancer. Clin Nucl Med. 2012;37:545–9.
Sawka AM, Orlov S, Gelberg J, Stork B, Dowar M, Shaytzag M, et al. Prognostic value of postsurgical stimulated thyroglobulin levels after initial radioactive iodine therapy in well-differentiated thyroid carcinoma. Head Neck. 2008;30:693–700.
Park EK, Chung JK, Lim IH, Lee DS, Lee MC, Cho BY. Recurrent/metastatic thyroid carcinomas false negative for serum thyroglobulin but positive by posttherapy I-131 whole body scans. Eur J Nucl Med Mol Imaging. 2009;36:172–9.
Verkooijen RB, Rietbergen D, Smit JW, Romijn JA, Stokkel MP. A new functional parameter measured at the time of ablation that can be used to predict differentiated thyroid cancer recurrence during follow-up. Eur J Endocrinol. 2007;156:41–7.
Tamilia M, Al-Kahtani N, Rochon L, Hier MP, Payne RJ, Holcroft CA, et al. Serum thyroglobulin predicts thyroid remnant ablation failure with 30 mCi iodine-131 treatment in patients with papillary thyroid carcinoma. Nucl Med Commun. 2011;32:212–20.
Bernier MO, Morel O, Rodien P, Muratet JP, Giraud P, Rohmer V, et al. Prognostic value of an increase in the serum thyroglobulin level at the time of the first ablative radioiodine treatment in patients with differentiated thyroid cancer. Eur J Nucl Med Mol Imaging. 2005;32:1418–21.
Vrndic OB, Savin SB, Mijatovic LC, Djukic AA, Jeftic ID, Simonovic STZ. Concentration of thyroglobulin and thyroglobulin-specific autoantibodies in patients with differentiated thyroid cancer after treatment with radioactive iodine 131. Lab Med. 2011;42:27–31.
Mazzaferri EL, Robbins RJ, Spencer CA, Braverman LE, Pacini F, Wartofsky L, et al. A consensus report of the role of serum thyroglobulin as a monitoring method for low-risk patients with papillary thyroid carcinoma. J Clin Endocrinol Metab. 2003;88:1433–41.
Eustatia-Rutten CF, Smit JW, Romijn JA, van der Kleij-Corssmit EP, Pereira AM, Stokkel MP, et al. Diagnostic value of serum thyroglobulin measurements in the follow-up of differentiated thyroid carcinoma, a structured meta-analysis. Clin Endocrinol (Oxf). 2004;61:61–74.
Pelttari H, Valimaki MJ, Loyttyniemi E, Schalin-Jantti C. Post-ablative serum thyroglobulin is an independent predictor of recurrence in low-risk differentiated thyroid carcinoma: a 16-year follow-up study. Eur J Endocrinol. 2010;163:757–63.
Toubeau M, Touzery C, Arveux P, Chaplain G, Vaillant G, Berriolo A, et al. Predictive value for disease progression of serum thyroglobulin levels measured in the postoperative period and after (131)I ablation therapy in patients with differentiated thyroid cancer. J Nucl Med. 2004;45:988–94.
Webb RC, Howard RS, Stojadinovic A, Gaitonde DY, Wallace MK, Ahmed J, et al. The utility of serum thyroglobulin measurement at the time of remnant ablation for predicting disease-free status in patients with differentiated thyroid cancer: a meta-analysis involving 3947 patients. J Clin Endocrinol Metab. 2012;97:2754–63.
Lin JD, Huang MJ, Hsu BR, Chao TC, Hsueh C, Liu FH, et al. Significance of postoperative serum thyroglobulin levels in patients with papillary and follicular thyroid carcinomas. J Surg Oncol. 2002;80:45–51.
Gibelli B, Tredici P, De Cicco C, Bodei L, Sandri MT, Renne G, et al. Preoperative determination of serum thyroglobulin to identify patients with differentiated thyroid cancer who may present recurrence without increased thyroglobulin. Acta otorhinolaryngol Ital. 2005;25:94–9.
Ramakrishnan N, McClain DE, Catravas GN. Membranes as sensitive targets in thymocyte apoptosis. Int J Radiat Biol. 1993;63:693–701.
Nishiyama K, Kozuka T, Higashihara T, Miyauchi K, Okagawa K. Acute radiation thyroiditis. Int J Radiat Oncol Biol Phys. 1996;36:1221–4.
Acknowledgments
This research was supported by the National Research Foundation of Korea (NRF), funded by the Ministry of Science, ICT and Future Planning (No. 2011-0030680).
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kim, Yi., Im, HJ., Paeng, J.C. et al. Serum thyroglobulin level after radioiodine therapy (Day 3) to predict successful ablation of thyroid remnant in postoperative thyroid cancer. Ann Nucl Med 29, 184–189 (2015). https://doi.org/10.1007/s12149-014-0927-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12149-014-0927-5