Abstract
Purpose
The aim of this study was to assess the prognostic factors for treatment efficacy, and in particular the increase in serum thyroglobulin (Tg) level at the time of the first ablative radioiodine treatment, in patients with differentiated thyroid carcinoma (DTC).
Methods
A retrospective chart review was performed on 407 patients treated for DTC by total thyroidectomy and 131I ablation between 1995 and 2002, and examined 5–12 months later with diagnostic 131I whole-body scan and serum Tg measurement after thyroid hormone treatment withdrawal. At the time of the ablative radioiodine treatment, serum Tg level was determined just before 131I administration (TgD0) and 5 days later (TgD5); Tg variation was expressed as the ratio TgD5/TgD0. At the first post-ablation follow-up examination, unsuccessful ablation was defined by a Tg level ≥2 ng/ml and/or abnormal 131I uptake.
Results
Ablation was unsuccessful in 51 patients. Univariate analysis showed high TgD0 level, low TgD5/TgD0 ratio extrathyroidal invasion, 131I uptake in the neck (excluding the thyroid bed) during the ablative treatment and distant metastases to be significantly associated with unsuccessful ablation. On logistic multivariate analysis, TgD0 level <5 ng/ml and TgD5/TgD0 ratio ≥20 were independently associated with successful ablation. A receiver operating characteristic curve analysis determined that a TgD5/TgD0 ratio greater than 20 had a 97% positive predictive value for successful ablation. When both TgD0 and TgD5/TgD0 ratio were considered, that is, TgD0 <5 ng/ml or TgD0 ≥5 ng/ml but TgD5/TgD0 ratio >20, ablation was unsuccessful in only 12/301 patients.
Conclusion
Our data show that the TgD5/TgD0 ratio may be used as a new prognostic indicator of 131I treatment efficacy in patients with DTC.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The long-term prognosis (in terms of survival) of papillary and follicular differentiated thyroid cancer (DTC) is known to be very good [1, 2]. The value of serum thyroglobulin (Tg) measurement in the follow-up of DTC is well recognized [3–9]. In particular, after near-total or total thyroidectomy and just before ablative radioiodine treatment, an elevated serum Tg level after thyroid hormone treatment withdrawal has been shown to have a high predictive value for persistent cervical disease or distant metastases [10, 11]. In a previous study, conducted in a small population of patients, we reported that an increase in serum Tg level during ablative radioiodine treatment (3.7 GBq) appeared to be a good predictor of treatment efficacy [12].
The aim of this study was to evaluate, in a large cohort of consecutive patients treated for DTC, the initial prognostic factors for treatment efficacy, and in particular the relevant cut-off value for the increase in serum Tg level at the time of ablative radioiodine treatment.
Materials and methods
Subjects
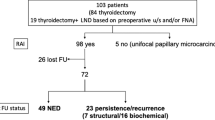
Between January 1995 and September 2002, 540 patients with DTC were referred to our institution for ablative radioiodine treatment. All patients had undergone near-total or total thyroidectomy. Diagnostic 131I whole-body scan (131I-WBS) and serum Tg measurement after thyroid hormone treatment withdrawal were usually performed 6–12 months after 131I ablation. For various reasons, 133 patients were not included in the study: 62 with anti-Tg antibodies, 17 with a TSH below 25 mIU/l at the time of the ablative radioiodine treatment, 44 in whom diagnostic 131I-WBS and serum Tg measurement 6–12 months after the ablative radioiodine treatment were either not performed (n=18) or were performed after rhTSH stimulation (n=26), 3 with missing Tg measurements and 7 in whom lymph node dissection (n=6) or bone metastasis surgery (n=1) was performed between 131I therapy and follow-up examination.
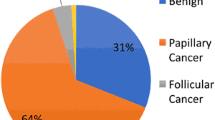
The study population comprised 302 females and 105 males, aged 9–81 years (mean 46) at the time of thyroidectomy. The histological DTC subtype was papillary in 329 cases (81%) and follicular in 78 cases (19%). Fourteen patients were found to have distant metastases at the time of the first radioiodine treatment (bone in four cases, lung in eight cases and both lung and bone in two cases).
Ablative radioiodine treatment
Patients were referred for radioiodine therapy 1–16 months (median 3.4 months) after thyroidectomy. L-Thyroxine treatment was discontinued 6 weeks before ablative radioiodine treatment and replaced by triiodothyronine for 4 weeks. Triiodothyronine was stopped 2 weeks before radioiodine therapy. On day 0 (D0), an ablative dose of 131I (3.7 GBq) was administered. On day 5 (D5), 131I-WBS was performed, using a dual-head gamma camera (DST-XL, Sopha Medical Vision, France) equipped with high-energy collimators. Spot views were obtained for 10 min and radioiodine cervical uptake was quantified.
TSH and Tg measurements
Blood samples were drawn on day 0 (immediately before the administration of an ablative dose of 131I) and on day 5. Serum TSH measurement was performed on day 0. Serum Tg was measured on day 0 and day 5 in a radioimmunoassay (Cis Bio International, France) with a lower detection limit of 0.2 ng/ml. Serum anti-Tg auto-antibodies were measured on day 0 by an immunoradiometric assay method (Cis Bio International, France; normal range <70 IU/ml). Variation between pre- (D0 Tg level) and post-therapeutic (D5 Tg level) serum Tg levels was expressed as the ratio TgD5/TgD0. Given the assay sensitivity of 0.2 ng/ml, the ratio was calculated only when TgD5 and TgD0 were both greater than 0.2 ng/ml.
Follow-up examination
The first post-ablation follow-up examination was performed 5–12 months (mean 7.3 months) after 131I thyroid ablation. This follow-up examination consisted of a diagnostic 131I-WBS and serum Tg measurement after thyroid hormone withdrawal. Blood samples for serum TSH and Tg assays were drawn before 131I administration (111 MBq). 131I-WBS was performed 3 days later. Patients were classified into two groups :
-
1.
Unsuccessful ablation: Tg level ≥2 ng/ml and/or abnormal 131I uptake in a pattern evocative of residual or metastatic disease
-
2.
Successful ablation: Tg level <2 ng/ml
Statistical analysis
Using logistic regression, 11 variables were tested for their association with unsuccessful ablation by univariate analysis: sex, age at diagnosis, TgD0 level, TgD5/TgD0 ratio, histological subtype (follicular or papillary), tumour size, number of tumour foci (one, two or more), extrathyroidal extension, abnormal uptake evocative of cervical lymph node metastases on the 131I-WBS performed 5 days after the ablative dose, and presence and location of distant metastases. Variables with 0.05<p≤0.20 were further analysed by multiple logistic regression with backward elimination of variables so as to identify a small set of variables with independent prognostic significance. A p value <0.05 was considered statistically significant. Statistical analysis was performed using SPSS statistical software (SPSS, Inc., Chicago, IL).
Results
At the time of ablative radioiodine treatment, TgD0 ranged from 0 to 9,663 ng/ml (median 3.8) and the TgD5/TgD0 ratio, calculated in 364 cases, ranged from 0.3 to 301.6 (median 14.8). At the follow-up examination, successful ablation was observed in 356/407 (87.5%) patients. In 51 patients with unsuccessful ablation, the serum Tg level ranged from 2.1 to 4,286 ng/ml (median 5.1), with abnormal diagnostic 131I-WBS in 18 cases.
Variables significantly associated with unsuccessful ablation by univariate analysis are reported in Table 1. The results of the logistic multivariate regression analysis are summarised in Table 2. We observed that both a TgD5/TgD0 ratio ≥20 and a TgD0 level <5 ng/ml were independently associated with successful ablation even after testing a term of interaction between these two variables. A receiver operating characteristic curve analysis determined that a TgD5/TgD0 ratio ≥20 had a 97% positive predictive value for successful ablation (Table 3).
As in our experience ablation is successful in most patients with a TgD0 level <5 ng/ml, we defined a subgroup of patients with an initial good prognosis, including those with a TgD0 level <5 ng/ml (n=238) and those with a TgD0 level ≥5 ng/ml but a TgD5/TgD0 ratio ≥20 (n=63). All in all, among the 301 patients of this subgroup, ablation was unsuccessful in only 12 (4%) patients. Firstly, unsuccessful ablation was observed in only 7 (2.9%) of the 238 patients with TgD0 <5 ng/ml (Table 3). All seven of these patients had a TgD5/TgD0 ratio <20, ranging from 0.85 to 9.11 (mean 3.22). In five of the seven, no recurrence was observed during follow-up (mean follow-up 35.5 months, range 7–72). The two other patients had widely invasive Hürthle cell carcinomas and TgD0 levels of 3.4 and 1.7 ng/ml, respectively. Their serum Tg levels remained detectable (5.1 and 2.5 ng/ml, respectively) at the follow-up examination and they received a second dose of 3.7 GBq 131I, with no uptake observed on the post-therapeutic 131I-WBS. Complementary imaging by neck ultrasonography and 18F-FDG PET/CT demonstrated residual disease in the thyroid bed in one patient and the presence of lung metastases in both patients. Secondly, among the 63 patients who presented a TgD0 level ≥5 ng/ml but a TgD5/TgD0 ratio ≥20, unsuccessful ablation was observed in five patients. Their TgD0 level ranged from 5.5 to 24 ng/ml (mean 15.0) and was always lower at the follow-up examination, ranging from 4.3 to 9.8 ng/ml (mean 6.5). One patient presented bone metastases on the initial post-therapeutic 131I-WBS and afterwards received iterative 131I therapy. The serum Tg level of the four other patients progressively decreased and they were considered free of disease after prolonged follow-up (mean follow-up 50.7 months, range 25–73 mo).
Discussion
Our data suggest that the magnitude of the increase in serum Tg level during the 131I ablative treatment is an important and independent prognostic factor for successful ablation. Four other prognostic factors were identified by multivariate analysis: low TgD0 level, no extrathyroidal invasion on pathology, female gender and absence of distant metastases.
We hypothesised that the importance of the increase in serum Tg after radioiodine therapy could be related to the 131I uptake in residual thyroid tissue and radiation-induced cellular damage, as previously described with external radiotherapy [13, 14]. We determined a threshold for the TgD5/TgD0 ratio which could distinguish patients with successful ablation from those with unsuccessful ablation. To avoid overlooking persistent disease, we favoured high specificity (90%) and high predictive value for successful ablation (97%), thus accepting a low sensitivity (44%).
Identification of patients with successful ablation was improved by considering both the TgD5/TgD0 ratio and TgD0, as compared with the TgD0 level alone. According to different studies, TgD0 values ranging from 2.5 to 69.7 ng/ml can reflect the presence of metastases, although it remains difficult to distinguish Tg production by thyroid remnants from metastatic Tg production [8, 10, 15–18]. Thus a TgD0 level <5 ng/ml or a TgD0 level ≥5 ng/ml associated with a TgD5/TgD0 ratio ≥20 was noted in 301/407 patients (74%) of our population and predicted patient outcome correctly in 289 cases (96%), while failing to identify only 12 patients with unsuccessful ablation. Moreover, long-term follow-up of these 12 patients showed persistent disease in only three cases.
In the subgroup of 106 patients with an initial less favourable prognosis, as defined by our criteria (i.e. TgD0 ≥5 ng/ml and TgD5/TgD0 <20), clinical features and evolution of serum Tg level during the follow-up were not studied. Indeed, we considered that the relationship between TgD0 level or TgD5/TgD0 ratio and long-term prognosis would be obscured by the bias introduced by the heterogeneity of subsequent medical care, which included at least another radioiodine treatment, external radiation therapy and/or surgery in 50 cases.
The estimated amount of residual thyroid tissue was not included in statistical analysis because our patients had undergone total thyroidectomy and median cervical uptake of 131I was 1.7%, suggesting that residual tissue did not usually exceed 5 g. Furthermore, serum TgD0 level and cervical uptake of 131I did not correlate and precise assessment of remnant volume by ultrasonography is difficult in the postoperative period.
In conclusion, an increase in the serum Tg level during ablative radioiodine treatment in patients with DTC should be considered to be a new independent prognostic factor for 131I treatment efficacy. By combining it with known prognostic factors, it may be possible to predict successful ablation in the majority of patients with DTC, with a rather low risk of missing persistent disease.
References
Schlumberger MJ. Diagnostic follow-up of well-differentiated thyroid carcinoma: historical perspective and current status. J Endocrinol Invest 1999;22 (11 Suppl):3–7
Dean DS, Hay ID. Prognostic indicators in differentiated thyroid carcinoma. Cancer Control 2000;7:229–39
Mazzaferri EL, Kloos RT. Clinical review 128: current approaches to primary therapy for papillary and follicular thyroid cancer. J Clin Endocrinol Metab 2001;86:1447–63
Cailleux AF, Baudin E, Travagli JP, Ricard M, Schlumberger M. Is diagnostic iodine-131 scanning useful after total thyroid ablation for differentiated thyroid cancer? J Clin Endocrinol Metab 2000;85:175–8
Mazzaferri EL, Kloos RT. Is diagnostic iodine-131 scanning with recombinant human TSH useful in the follow-up of differentiated thyroid cancer after thyroid ablation? J Clin Endocrinol Metab 2002;87:1490–8
Toubeau M, Touzery C, Arveux P, Chaplain G, Vaillant G, Berriolo A, et al. Predictive value for disease progression of serum thyroglobulin levels measured in the postoperative period and after 131I ablation therapy in patients with differentiated thyroid cancer. J Nucl Med 2004;45:988–94
Menendez Torre E, Lopez Carballo MT, Rodriguez Erdozain RM, Forga Llenas L, Goni Iriarte MJ, Barberia Layana JJ. Prognostic value of thyroglobulin serum levels and 131I whole-body scan after initial treatment of low-risk differentiated thyroid cancer. Thyroid 2004;14:301–6
Roelants V, Nayer PD, Bouckaert A, Beckers C. The predictive value of serum thyroglobulin in the follow-up of differentiated thyroid cancer. Eur J Nucl Med 1997;24:722–7
Baudin E, Do Cao C, Cailleux AF, Leboulleux S, Travagli JP, Schlumberger M. Positive predictive value of serum thyroglobulin levels, measured during the first year of follow-up after thyroid hormone withdrawal, in thyroid cancer patients. J Clin Endocrinol Metab 2003;88:1107–11
Ronga G, Filesi M, Ventroni G, Vestri AR, Signore A. Value of the first serum thyroglobulin level after total thyroidectomy for the diagnosis of metastases from differentiated thyroid carcinoma. Eur J Nucl Med 1999;26:1448–52
Hall FT, Beasley NJ, Eski SJ, Witterick IJ, Walfish PG, Freeman JL. Predictive value of serum thyroglobulin after surgery for thyroid carcinoma. Laryngoscope 2003;113:77–81
Muratet JP, Giraud P, Daver A, Minier JF, Gamelin E, Larra F. Predicting the efficacy of first iodine-131 treatment in differentiated thyroid carcinoma. J Nucl Med 1997;38:1362–8
Cramp WA, Yatvin MB, Harms-Ringdahl M. Recent developments in the radiobiology of cellular membranes. Acta Oncol 1994;33:945–52
Ramakrishnan N, McClain DE, Catravas GN. Membranes as sensitive targets in thymocyte apoptosis. Int J Radiat Biol 1993;63:693–7
Grunwald F, Menzel C, Fimmers R, Zamora PO, Biersack HJ. Prognostic value of thyroglobulin after thyroidectomy before ablative radioiodine therapy in thyroid cancer. J Nucl Med 1996;37:1962–4
Lin JD, Huang MJ, Hsu BR, Chao TC, Hsueh C, Liu FH, et al. Significance of postoperative serum thyroglobulin levels in patients with papillary and follicular thyroid carcinomas. J Surg Oncol 2002;80:45–51
Filesi M, Signore A, Ventroni G, Melacrinis FF, Ronga G. Role of initial iodine-131 whole-body scan and serum thyroglobulin in differentiated thyroid carcinoma metastases. J Nucl Med 1998;39:1542–6
Lima N, Cavaliere H, Tomimori E, Knobel M, Medeiros-Neto G. Prognostic value of serial serum thyroglobulin determinations after total thyroidectomy for differentiated thyroid cancer. J Endocrinol Invest 2002;25:110–5
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bernier, MO., Morel, O., Rodien, P. et al. Prognostic value of an increase in the serum thyroglobulin level at the time of the first ablative radioiodine treatment in patients with differentiated thyroid cancer. Eur J Nucl Med Mol Imaging 32, 1418–1421 (2005). https://doi.org/10.1007/s00259-005-1866-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-005-1866-0