Abstract
Treatment of somatostatin receptor-positive tumors with radiolabeled somatostatin analog is a promising option. Several phase I and phase II studies done at a few centers around the world reported encouraging results with [90Y-DOTA-Tyr3]-octreotide (DOTATOC) and/or [177Lu-DOTA-Tyr3-Thr8]-octreotate (DOTATATE). The current article is a selective review of patients who were treated mainly with 90Y-DOTATOC after failure with conventional therapy. The aim is to provide an updated comprehensive evaluation of the overall effectiveness of 90Y-DOTATOC therapy in patients with somatostatin-positive tumors. Review of several studies revealed an objective response rate ranging from 20 to 28% for all neuroendocrine tumors (NET)s. For gastroenteropancreatic-NET (GEP-NET), the response rate was found to be consistently better in the range 28–38%. Overall, the cumulative response rate was found to be 24%. An important issue in peptide receptor radionuclide therapy (PRRT) is the dose–response relationship and finding the correct dose of 90Y-DOTATOC that will achieve an optimum tumor kill. Nephrotoxicity was common but could be minimized by taking adequate renal protective measures. In conclusion, PRRT remains a good option in patients with inoperable and/or metastatic NETs particularly of GEP origin. Over a decade of experience with 90Y-DOTATOC proves that it is still an effective tool for the treatment of large infiltrative NETs with achievement of objective radiological responses in nearly a quarter and disease stabilization in more than half the patients studied so far.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Neuroendocrine tumor (NET)s constitute a heterogeneous group of tumors that originate from the diffuse endocrine system such as the pituitary, the parathyroids, adrenal medulla, endocrine islets within glandular tissue (thyroid or pancreatic) and cells disseminated between exocrine cells, such as endocrine cells of the digestive and respiratory tracts [1]. Gastroenteropancreatic (GEP)-NETs in particular, arise from the neuroendocrine cells found in the pancreas, the gut and its derivatives like the bronchial tree [2]. The great majority are either benign or relatively slow growing (well differentiated NETs) but some may be aggressive and highly malignant (poorly differentiated NETs) [1]. The clinical manifestation of NETs depend on whether the tumor is functioning or non-functioning. Functioning tumors present clinically with symptoms related to overproduction of hormones and amines, while non-functioning tumors produce and secrete peptides that do not cause any distinct symptoms but may present with large abdominal masses with pressure symptoms [3, 4]. In general, malignant NETs and syndromes have poor prognosis and aggressive multimodality treatment is required for primary and metastatic tumors that continue to grow [1, 3] and cause symptoms. Treatment is mainly aimed at reducing hormone overproduction by these tumors. This is considered very important because mortality in NETs is often due to the effects of peptide hypersecretion rather than tumor progression [5]. Surgical removal or debulking of the primary or metastatic tumor mass is often the initial approach even though it is reported to be effective in <5% of all patients [6, 7]. This is due to the fact that 90% of patients have metastatic disease at the time of presentation [8]. Other treatment modalities are biotherapy, chemotherapy, peptide receptor-targeted therapy and tumor embolization. Each of these treatment options are applicable in specific clinical settings and has variable outcomes.
The discovery that most NETs overexpress receptors for peptide hormones has been a major breakthrough for development of somatostatin analog-derived radiopeptides for therapy. Somatostatin analogs are synthetic peptides with a longer half life than native peptides (2 vs. 90 min) but with the capacity to exert most of the biological actions of the native peptide [9]. In 1994, the diagnostic radiolabeled peptide [111In-DTPA] octreotide (OctreoScan, 111In-pentetreotide) was approved by the FDA for scintigraphy of patients with NETs [10] and it quickly became established as the standard practice for localization and staging of NETs in many centers. The selective uptake of this compound in tumors that expressed somatostatin receptors led to its subsequent use in higher doses for targeted radiotherapy. Many trials by several groups [11, 12] reported symptomatic improvement, but eventually the Auger particles emitted from the 111In coupled peptide proved to be inadequate in shrinking tumor size. This led to the search for analogs with higher affinity profiles that can be linked to beta-emitting radionuclides for better targeting and destruction of tumors. Consequently, a number of somatostatin analogs were constructed, which used dodecane tetraacetic acid derivative (DOTA) as the chelator to link the octreopeptide to a β-emitting therapeutic radionuclide such as 90Y and/or 177Lu. The first promising DOTA-chelated somatostatin analog was conjugated in 1996 [13]. DOTA provides a stronger bond between 90Y and the octreotide resulting in a more stable complex [14]. The resulting 90Y-DOTA-Tyr3-octreotide is currently known generically as 90Y-edotreotide (also referred to in literature as SMT-487 or 90Y-DOTATOC [2]. This compound has an increased affinity for somatostatin receptor 2 (sstr2) expressed by most NETs.
Peptide receptor radionuclide therapy (PRRT) with 90Y-DOTATOC is the most extensively studied radiopeptide in adults with NETs. Majority of the therapy trials were carried out in Basel (Switzerland), Milan (Italy), Rotterdam (Netherlands), including multicenter trials with Germany, Brussels, Belgium and USA. A number of review articles have also been published focusing on the various treatment options. The current article is a selective review of patients who were mainly treated with 90Y-DOTATOC after failure with conventional therapy. The aim of this review is to provide an updated comprehensive evaluation of the overall effectiveness of 90Y-DOTATOC therapy in patients with somatostatin receptor-positive tumors.
Method
Selected published literature on 90Y-DOTATOC therapy of NETs was obtained by hand searching through peer-reviewed journals, through electronic bibliographic databases and also through personal communication. Medline search through PubMed was accessed online several times to identify and download relevant articles. To narrow down the recovery of citations to those that fit the research question, specific text words such as 90Y-DOTATOC, 90Y-DOTA-Tyr3-octreotide, somatostatin receptor therapy, PRRT and NETs were used. In addition, author name, journal and publication types were also entered to filter the search. An experienced and authorized librarian accessed password restricted databases through the central library to find relevant articles. Bibliographies of key full text articles already retrieved were used to find even more relevant sources. These articles were carefully reviewed to identify the total number of cases and the different type of tumors treated with 90Y-DOTATOC. Though the focus was mainly on 90Y-DOTATOC therapy of NETs, two papers in which the patients were treated with 177 Lu-DOTATATE after failure of 90Y-DOTATOC therapy were also included in the review. The protocols used, activities administered, frequency and severity of the toxicities encountered and the response to therapy reported by different centers were summarized to obtain a comprehensive data of the outcome of patients treated with 90Y-DOTATOC. Findings obtained from the aggregation of results were discussed in the framework of patient/tumor characteristics, dose administration and objective responses to 90Y-DOTATOC therapy.
Patient characteristics and protocol for PRRT
Several clinical phase I and phase II trials with 90Y-DOTATOC therapy were carried out in centers mainly in Europe and in USA. The cumulative number of patients included in the analysis from 13 centers is shown in Table 1. A total of 774 patients were treated, of which 291 were male and 241 were female while in 242 patients the gender was not specified. The mean age was 41.25 years. Specific tumor types were GEP-NETs in 526 patients and NETs of other organs and/or unknown primary tumors in 248 patients. All patients received 90Y-DOTATOC therapy after failure and/or unsuitability of conventional modes of treatment. At baseline before PRRT, majority of the patients had progressive disease while others had symptomatic stable disease. The foremost criteria for selection were patients with residual or recurrent disease that showed positive uptake with somatostatin receptor scintigraphy. Patient eligibility mandated a sufficiently high uptake of tracer in the target tissues because it has been shown to correlate directly with tumor regression after therapy [15]. Baseline clinical examination and laboratory investigations were done which included routine hematology, liver and kidney function parameters. Generally, the pre-requisites of the treatment were normal blood count parameters (WBC >2,500/dl; hemoglobin >10 g/dl; platelets >100,000/dl) and normal serum creatinine <1.5 mg/dl, plus Karnofsky Performance Score ≥50. There was considerable variation in the selection of patients, activity of 90Y-DOTATOC and the types of protocol used. As per radiation protection regulation, all patients were hospitalized for 2–3 days for the procedure. After labeling of DOTATOC with 90Yttrium, the labeling yield and the radiopharmaceutical purity were checked for acceptability. The required 90Y-DOTATOC activity was then measured for each patient according to the different laboratory protocol and practice. Generally, the measured activity of 90Y-DOTATOC was administered slowly by intravenous route over 20–30 min in 100 ml physiological saline. Single or multiple cycles of the measured dose of 90Y-DOTATOC at 6–9 weeks intervals were given. While it is desirable to target the tumors with as high a dose as possible, the risk of radiation damage to the bone marrow and especially to the kidneys need special consideration. Precautionary measures to avert bone marrow complication included careful selection of patients in whom the bone marrow has not been compromised by previous therapies. For kidney protection, most trials used amino acids such as lysine ± arginine infusion immediately before, during or right after therapy at different concentrations and combinations. Some centers obtained dosimetry of the kidneys and planned the treatment aiming not to exceed 27 Gy to the kidneys.
Evaluation of response to therapy was made both clinically and by combination of CT, MRI, ultrasonography and nuclear medicine (111In-pentetreotide or FDG-PET) imaging. Blood count and chemistry, chromogranin A measurement in some centers, and tumor specific hormonal examinations were performed to assess response. The WHO and/or SWOG (South west Oncology Group) standard criteria was used to assess response to therapy in most centers. The SWOG criteria is defined as follows: complete response (CR) is total regression of all known lesions for at least 1 month; partial response (PR) is regression of all known lesions by more than 50%; Minor Response (MR) is regression of all known lesions by 25–50%; stable disease (SD) is no change in lesion size; Progressive Disease (PD) is increase of all known lesions by 25% or more. Clinical responses were also determined in some centers by a scoring system. Side effects of 90Y-DOTATOC were documented using the WHO toxicity grade criteria.
Clinical studies
The first successful therapeutic use of 90Y-DOTATOC was published from the School of Medicine, Basel, Switzerland in 1997 [16]. The group treated a patient with somatostatin receptor-positive abdominal metastases of a neuroendocrine carcinoma of unknown localization and reported good response with symptomatic relief. The following year [17], results of 10 more patients treated with 90Y-DOTATOC was published. Stability of the disease and partial remission were obtained in these patients with advanced somatostatin receptor-positive tumors who received multiple treatments 2 to 3 months apart without renal protection. The same group from Basel [18] reported the outcome of 90Y-DOTATOC therapy in a larger number of 29 patients in their phase I clinical study. The mean cumulative dose of 6.12 GBq (165 mCi)/m2 was divided over four cycles. Half the patients did not get renal protection with amino acid infusion. Twenty (69%) of the 29 patients showed evidence of SD, two (7%) had PR, four (14%) had MR and three (10%) had PD. The overall response rate was 21% when both partial and minor responses were considered. Renal toxicity was observed in four of the five cases who received more than 7,400 MBq/m2 without renal protection. Two patients who had received cumulative doses of 8,903–7,611 MBq/m2 90Y-DOTATOC had stable renal insufficiency and two patients who had received cumulative doses 8,788 and 8,924 MBq/m2 required hemodialysis. Radiation induced thrombotic microangiopathy was identified on kidney biopsy samples from these patients. Maximum dose tolerated in this trial was 6 GBq/m2 with kidney protection. Two of these five patients also exhibited anemia and thrombocytopenia grades 2–4 necessitating treatment.
Paganelli et al. [19] published the results of 20 patients treated with 90Y-DOTATOC in the same year. Their protocol consisted of 3 treatment cycles with dose escalation beginning at 1.1 GBq (30 mCi) per cycle in the first group of five individuals and ending at 2.2 GBq (60 mCi) per cycle in the last group of five. The response rate was MR/SD in 11 (55%), CR/PR in four (20%) and PD in 5 (25%) patients. No major hematological toxicity (grade 3 and 4) were reported with doses ranging 3.3 to 4.4 GBq. The majority patients had no acute kidney toxicity, although two patients showed grade 1 and one patient who received cumulative dose of 3.3 GBq had delayed grade 2 toxicity.
In 2001, the group from Basel [20] published the results of their phase II trial on 41 patients with neuroendocrine GEP and other NETs. The treatment consisted of a total 6,000 MBq/m2 90Y-DOTATOC administered over 4 cycles at intervals of 6 weeks. All patients had renal protection with amino acid infusions. Treatment had to be stopped in 2 patients after the second cycle due to tumor progression. The treatment response showed evidence of CR in one (2%) patient, PR in nine (22%), SD in 25 (61%) patient and PD in 6 (15%) patients. The overall objective response was 24%, but for GEP-NET the response rate was higher (36%). In four patients, CT showed elimination of all liver metastases. One patient who had been bedridden because of neuroendocrine spinal metastases achieved marked improvement in neurological function. However, eight of the 41 patients (20%) died within a median follow up of 15 months (range 2–26 months) after therapy from causes that were not related to 90Y-DOTATOC administration. The overall survival at 24 months including the 95% confidence interval was calculated to be 76 ± 16%. Lymphocytopenia and anemia were observed which returned to baseline after 3–4 weeks. Renal toxicity was not observed in any of these patients who had renal protection and received cumulative dose less than 7,400 MBq/m2 of 90Y-DOTATOC.
In a subsequent study, the same group [21] treated 39 patients with progressive NET with a higher (total 7.4 GBq (200 m Ci)/m2) dose of 90Y-DOTATOC given under enhanced renal protection. The patients all received an additional 2,000 ml amino acid infusion for renal protection within 2.5 h after 90Y-DOTATOC bolus injection. The high activity was well tolerated with remarkable clinical benefit and objective response. The results showed CR in two (5%), PR in seven (18%), SD in 27 (69%) and PD in three (8%). The over all tumor response was 23%. In 13 patients with endocrine pancreatic tumors the response rate was 38%. Clinical improvement of symptoms was found in 63% patients. In these patients with advanced disease at the time of initiating the therapy, 92% patients could be stabilized (CR, PR or SD). Lymphocytopenia and anemia grade 1-3 that occurred after therapy was reversible within 3–4 weeks. Delayed renal toxicity was observed in one patient in the form of increased serum level of creatinine 5 months after therapy while in rest of the patients it remained normal during and after treatment within the median follow up of 6 months.
Paganelli et al. [22] reported their results on 30 patients treated with three cycles of up to 2.59 GBq of 90Y-DOTATOC per cycle (total 7.77 GBq) without renal protection. Complete or partial tumor mass reduction occurred in 7 (23%) of patients, while 19 (64%) had SD and 4 (13%) had PD. No major acute undesirable reactions were observed after 90Y-DOTATOC injection up to 2.59 GBq per cycle. Grade-2 renal toxicity was observed 6 months later in one patient after total dose of 3.33 GBq.The cumulative radiation dose to the kidneys was found to be the limiting factor with high dose. Median duration of response was 18 months.
The same group from Milan [23] treated 87 patients with higher activities of 90Y-DOTATOC ranging from 7.4 to 20.2 GBq/m2 with no major adverse effects in doses up to 5.55 GBq/cycle. Amino acid infusion was given for renal protection. Complete remission was found in four (5%), PR in 20 (23%), stable disease in 43 (49%) and progressive disease in 17 (20%), while three (3%) patients could not be evaluated. The objective response for the whole group was 28%. No major acute reactions were observed up to the activity of 5.55 GBq per cycle. The dose limiting was bone marrow toxicity and the maximum tolerated dose was defined as 5.18 GBq.
Further experience with 90Y-DOTATOC therapy on a large number of patients was reported by the same group from the European Institute of Oncology [24]. They investigated the potential therapeutic applications of 90Y-DOTATOC by performing a thorough dosimetric study in 18 patients who were administered 111In-DOTATOC to estimate the absorbed doses during 90Y-DOTATOC administration. Then they moved on and treated an overall number of 256 patients with 90Y-DOTATOC. These patients were mostly recruited in two distinct protocols with and without the administration of kidney protecting agents. The first group of 30 patients were treated without kidney protection with 3 cycles of escalating doses from 1.11 to 2.59 GBq per cycle at 8 wks interval. The objective response in this group was reported to be 23%. There were no major acute reactions or renal toxicity within the short period of follow up. The second group of 40 patients received 2 cycles of 90Y-DOTATOC starting from 2.96 GBq up to 5.55 GBq activities per cycle under renal protection. The objective therapeutic response in this group was 21%. Among the total number of 256 patients studied in the above center, 111 of the patients had a cumulative activity ranging from 7.4 GBq and 21.3 GBq (200–576 mCi) in two or more sessions. In a mean follow-up of 15 months the objective response rate in this group was 27%. Complete response was found in 6 (5%), PR in 24 (22%), stable disease in 54 (49%) and progressive disease in 17 (20%) while in 5 (4%) patients, the response could not be evaluated.
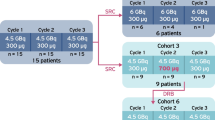
Another multicenter phase I study [25] was carried out to define the maximal tolerated single and 4 cycle dose of 90Y-DOTATOC in 42 patients with progressive and stable NETs. Before treatment, all patients underwent PET scan with 86Y-DOTATOC to predict the renal exposure expected with 90Y DOTATOC. The cumulative radiation dose to the kidneys was limited to 27 Gy. All patients received amino acids infusion concomitantly with 90Y DOTATOC administration. The activity was given in 4 cycles of escalating doses repeated every 6 to 9 weeks. The cumulative dose ranged from 1.7 to 27 GBq (47 to 733 mCi) without reaching the maximum tolerable dose. Of the 32 patients who could be evaluated, three (9%) had PR, four (13%) had minor and mixed response, 17 (53%) were stable and 8 (25%) had progressive disease. Complete symptomatic cure occurred in two of two insulinoma and one of one gastrinoma patients. Sixteen (50%) patients had symptomatic improvement. The renal toxicity was mild in this study.
A collaborative study from the research groups in Basel and in Milan [26] also attempted to find out the maximum tolerated dose of 90Y-DOTATOC per cycle in association with amino acid infusion. Forty patients in eight groups received two cycles of 90Y-DOTATOC with the activity increasing by 0.37 GBq per group. The activity started from 2.96 and terminated at 5.55 GBq, while the dose of the peptide ranged from100 to 150 μg. To protect the kidneys, the cumulative dose was limited to ~27 Gy, plus amino acid infusion was given in different combinations. There was grade 3 hematological toxicity in 43% patients but no renal toxicity was observed. Overall, one (2.5%) patient with medullary thyroid carcinoma had complete response, seven (17.5%) patients had partial remission, 18 (45%) patients had stable disease, 13 (32.5%) patients had progressive disease while in one (2.5%) patient the response could not be evaluated. Over all the objective response was 20%. When GEP-NETs were considered separately the objective response was 28.5% with six out of 21 patients with GET-NET showing tumor regression.
In a subsequent review, Bodei et al. [27] detailed the results of 141 patients treated for different types of NET. The patients were treated with cumulative activities ranging from 7.4 to 26.4 GBq 90Y-DOTATOC divided into 2–16 cycles at 4–6 weeks apart. The objective response (PR + CR) was 26%. An overall clinical benefit was observed in 76% patients who had progressive disease and in 32% patients who had stable disease at the time of treatment. Most of the patients who responded (69.7%) had GEP-NET.
Long-term follow-up and survival data on 58 patients treated with 90Y-DOTATOC for advanced GEP-NET was published by Valkema et al. [28]. At baseline, 47 of the 58 patients had progressive disease, 36 of whom were symptomatic. There were 52 patients with liver metastasis of which 16 were in the ‘end stage’ and six patients without liver metastasis of which 2 were in the ‘end stage’. A dose-escalating protocol with 0.73–3.80 GBq/m2 in four equal cycles (cumulative 8.20–14.90 GBq/m2) or two to three single dose escalation of 3.60–9.30 GBq/m2 (cumulative 7.20–12.90 GBq/m2) were administered without reaching the maximum tolerated single dose. The cumulative radiation dose to kidneys was limited to 27 Gy. All patients had concomitant amino acid infusions for renal protection. The overall results were PR in five (9%), minor response in seven (12%), stable disease in 29 (50%) and progressive disease in 17 (29%). Full individual treatment was possible only in 52 patients because of death/withdrawal of consent and/or disease progression in six others. Patients who had stable disease at baseline had a significantly better overall survival rate than patients with progressive disease at baseline. Overall 33 (57%) patients experienced some improvement in their disease status; including conversion from progressive disease into stable disease and improvement from stable disease to minor response. Three patients had dose-limiting toxicity (liver toxicity, thrombocytopenia grade 4 and myeloblastic syndrome in each of the three). The median overall survival was 36.7 months.
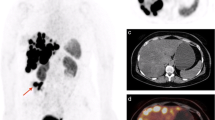
In another study [29], 90Y-DOTATOC was used as frontline therapy in 20 patients who had advanced histologically or cytologically proven progressive metastatic NET not suitable for primary resection. All patients received 90Y-DOTATOC as initial treatment in two or more cycles repeated at 8–10 weeks interval. The cumulative dose of 90Y-DOTATOC was 7.4 GBq/m2. Six patients were later switched to therapy with 177Lu-DOTATOC due to tumor relapse and/or due to small size and multilocularity of the neoplastic lesions. The follow-up period was from 6 to 36 months (median 19.9 months). In the evaluation of 14 patients with 90Y-DOTATOC therapy alone, three (21.4%) patients had PR, eight (57.14%) had stable disease and three (21.4%) had progressive disease. The objective response was 21%. The therapy further allowed the surgical resection of large metastatic deposits in two patients.
Forrer et al. [30] from Basel, Switzerland studied the efficacy and safety of 90Y-DOTATOC in activities ranging from 162 to 200 mCi/m2 administered to 116 patients with metastatic NET. The results showed complete response in five (4%), PR in 26 (23%), stable disease including minor response in 72 (62%) and progressive disease in 13 (11%). In 57 patients, the quality of life (QoL) was assessed with the National Cancer Institute-Common Toxicity Criteria (NCI-CTC). Symptomatic response according to the NCI-CTC scoring system revealed a significant reduction of carcinoid symptoms in 83% patients with diarrhea, 46% patients with flushes, 63% patients with wheezing and in 75% patients with pellagra. The reduction of tumor-related pain was also significant, allowing the patients to either stop pain medication or shift to lower potency analgesics. The same group examined the efficacy of radiolabeled DOTATOC in 28 patients with surgically incurable metastatic paragangliomas and pheocytochromas [31]. In 25 patients, 90Y-DOTATOC alone was used for therapy in a total activity of 200 mCi/m2 body surface while in three patients, first one cycle of 90Y-DOTATOC 100 mCi/m2 body surface was given, followed by 200 mCi/m2 of 177Lu-DOTATOC. The three patients who received 177Lu DOTATOC all suffered from predominantly small metastasis (<2 cm). Of the 28 patients, two could not complete the treatment due to progression of disease during therapy. Of the 26 who completed the treatment, the response rate showed two partial remissions, five minor responses; two patients showed a mixed response (some lesions were bigger and some smaller), 13 had stable disease after former progression; and four patients remained progressive. The treatment was well tolerated. Even though the efficacy was less than that reported with GEP-NET, the mean 18 months duration of response observed in this group with advanced paragangliomas was remarkable compared to the median duration of between 9 and >36 months for NET. In a more recent publication, the benefit of PRRT in a small homogenous group of five patients with advanced stages of NET was shown by Muros et al. [32]. After the failure of all kinds of conventional therapy, these patients were treated with 90Y DOTATOC with activities ranging from 45 to 200 mCi in 2–3 consecutive cycles with an interval of 3–4 months. The patients also received a continuous infusion of amino acids positively charged with different combinations of l-lysine and/or l-arginine. Three patients were treated with 90Y-DOTATOC alone while two patients received both 90Y DOTATOC and 177Lu DOTATATE in different cycles. The patient follow-up ranged from 20 to 37 months. In this study, response to therapy was assessed using the response evaluation criteria in solid tumors (RECIST), post-treatment survival time and QoL using Karnofsky performance index. All patients survived for >20 months after treatment (mean survival time was 28 months). Three patients were alive after 20, 27 and 37 months. Partial response was observed in one patient, stable disease in three and disease progression in the fifth patient. A good-to-excellent post treatment QoL was observed in all patients with a mean Karnofsky score of 75%. All patients experienced significant increase in appetite and weight with disappearance of carcinoid syndrome. Two of the patients returned to their usual work activity.
Aggregation of result from several of the above studies is shown in tabular form. The dose schedule and activities of 90Y-DOTATOC administered to the patients are shown in Table 2 and the response achieved to therapy is given in Table 3. The objective response rate for all somatostatin-positive tumors treated with 90Y-DOTATOC was 24%. For GEP-NET, the response rate was found to be consistently better in the range 28–38%.
Adverse effects of therapy
Acute effects
The immediate side effects encountered after 90Y-DOTATOC administration were mostly reported as mild and tolerable. Nausea, vomiting and flushing (grades 1–3) were common and frequently attributed to amino acid infusion. Vague, difficult to locate symptoms in the form of flushing in patients with carcinoid syndrome, warm sensation, paraesthesia and gastric heaviness were reported in patients treated by Bodei et al. [26] and one patient with pancreatic insulinoma required co-infusion of 5% glucose solution. Clinical manifestation of acute toxicity such as skin reaction, allergy or fever was not observed in any of the trials. However, as a consequence of irradiation some patients frequently experienced asthenia in the first week following therapy [27].
Hematological toxicity
The maximum tolerated dose for hematologic toxicity was reported as 5.18 GBq [22, 26]. Hematological toxicity of different grades according to NCI-CTC and/or WHO criteria were found in almost all the studies. Anemia, lymphocytopenia, thrombocytopenia and pancytopenia ranging from grades 1 to 4 were reported. These values usually returned to baseline after a few weeks but occasionally may require blood transfusion [18, 22, 29]. Late hematological toxicity in the form of myeloblastic syndrome has also been reported 2 years after the start of PRRT and/or chemotherapy [28, 33]. In general, patients who started with anemia and thrombocytopenia of lower grade exhibited higher grades of hematological toxicity [20] after therapy.
Renal toxicity
The kidneys are considered the dose-limiting organ in PRRT with 90Y-DOTATOC because of potential interstitial irradiation that can occur from tubular peptide re-absorption. Positively charged amino acids, e.g. l-lysine and l-arginine, have been demonstrated to competitively inhibit the proximal tubular re-absorption of the radiopeptide, resulting in a potential reduction in renal dose [27]. Bodei et al. [26] used amino acid infusion in different combinations in 40 patients. The first 16 patients received 20 g lysine and 40 g arginine each in 1 l physiological saline over 3–4 h before DOTATOC. Next 14 pts received 10 g lysine and 20 g arginine in 500 ml saline each over 1–2 h prior to therapy. Next 10 patients received 10 g lysine and 15 g arginine in 500 ml saline over 1 h before therapy and 15 g lysine in 750 ml saline over 2 h after therapy. Transient elevation of serum BUN and creatinine occurred in two patients but permanent renal toxicity was not observed in any patient over a 3–30 months follow-up (median 19 month) period. The effect of amino acid infusion was observed in the biodistribution study showing reduction of kidney uptake of 111In-DOTATOC. Since the volume of the kidneys play a crucial role in the absorbed dose to the organ [34], it is often recommended to adapt an individual dose scheme. Individual dosimetry can be performed both by 111In-DOTATOC and 86Y-DOTATOC. Though 86Y-DOTATOC is ideal and a perfect surrogate of 90Y for dosimetry studies, the disadvantage is that, it is not widely available and has a decay characteristic that requires elaborate correction algorithm. In comparison, 111In-DOTATOC is readily available and pre-therapeutic dosimetry can be done on planar scintigraphic images for effective treatment with 90Y-DOTATOC [35]. Renal toxicity was found to be mild with individualized (renal) dosimetry and co-infusion of protective amino acids when renal radiation dose is limited to <27 Gy [33]. Conventional dosimetry, however, does not always correlate with renal toxicity observed in patients treated with 90Y-DOTATOC [36]. In one study, Bodei et al. [37] studied the biological effective dose (BED) to the kidneys using the Linear-Quadratic Model for radionuclide therapy and observed a BED threshold of 28 Gy for renal toxicity in patients with risk factors such as hypertension and diabetes and a threshold 40 Gy for those without risk factors.
In a large number of patients studied by the European Institute of Oncology [23, 24], only mild reversible grade 1 renal toxicity was observed. They have determined that infusion of lysine ± arginine before and after therapy can give around 30% protection in a way that the maximum cumulative activity of 90Y-DOTATOC could be set in the range 12–18 GBq. Valkema et al. [28] reported dose-limiting toxicity in two patients. They observed 15% per year decline in creatinine clearance in nine patients and end stage renal disease in two patients. Forrer et al. [30] found, grade 4 renal toxicity in one patient requiring hemodialysis. All trials agreed on the kidneys being the dose-limiting organs with repeated administration of 90Y-DOTATOC.
Other side effects
Tumor-associated pain and weakness was experienced by some patients with bone and/or liver metastasis requiring the need for morphine administration in a few patients [20]. Carcinoid syndrome (grades 1–4) was also observed (despite octreotide medication) in the form of diarrhea, vomiting, intermittent flushes, wheezing/dyspnoea and pellagra [20, 21]. In general liver toxicity was low and grade 3 hepatic toxicity was observed in very few patients [28, 33].
Discussion
The molecular basis of PRRT lies in the ability of the synthetically developed somatostatin analogs to selectively bind with endogenous somatostatin receptors expressed in enhanced levels by particular tumor cells. One of the most successful analogs developed so far is DOTATOC [13], which can be labeled with a high energy beta emitter at elevated specific activities of up to 55.5–62.9 GBq μmol [24]. The increased specificity of DOTATOC for sstr2 receptors and the radiotherapeutic effects of the compound when labeled with 90Y were demonstrated pre-clinically in the rat CA20948 tumor model a decade ago by Stolz et al. [38].
In clinical studies, the effects of 90Y-DOTATOC therapy as the effects of any other anti-cancer therapy is variable, being dependent on size of the tumors, stage of the disease, differentiation of the tumor cells and other factors [39]. Taking into consideration, all the variability inherent in the different studies from different centers reviewed here, the cumulative objective response (including CR, PR and MR) was found to be 24%. The rate of complete remission with disappearance of all tumors was only 5% (36/774). This is not surprising because 90Y-DOTATOC therapy is mostly performed in patients with inoperable or metastasized NETs and at a stage that is less favorable for complete remission. Majority of the patients were in progressive stage of the disease before initiation of PRRT and though the rate of complete remission was very low, disease stabilization of up to 54% was observed. This is quite remarkable in a patient population with advanced disease and no other treatment options.
Of note is the increased effectiveness of PRRT in GEP-NET compared to other NETs. Among the many sstr2-positive tumors that were treated, the response rate of GEP-NET to PRRT was found to be consistently better (28–38%) than that obtained for other NETs. In NETs of other organs, the success rate of PRRT was found to be widely variable. In patients with somatostatin receptor-positive small cell lung cancer, therapy with 90Y-DOTATOC in a pilot study showed no objective response [40]. In a phase II trial on metastatic medullary thyroid carcinoma, response to 90Y-DOTATOC therapy was found to be associated with long-term survival benefit justifying its intensified use in patients who are responsive [41]. In another recent study, 90Y-DOTATOC and 177Lu DOTATOC therapy in patients with inoperable paraganglioma and pheochromocytomas though less effective than in GEP was nevertheless found to be remarkable with a mean 18 months duration of response [31].
An important issue in PRRT is the dose–response relationship and finding the correct dose of 90Y-DOTATOC that will achieve an optimum tumor kill. Previous animal studies have indicated that high absorbed doses to tumor lesions (>80–100 Gy) would result in a high percentage of cure and that this dose range should be reached in humans at activities of at least 7.4 GBq [24, 33]. Although remarkable responses and disease stabilization were achieved in patients receiving cumulative doses of >7.4 GBq/m2, there were also increased (≥grade 3) toxicity to the kidneys [24]. Waldherr et al. [21], however, did not find significant improvement in tumor response when the total dose was increased from 6 to 7.4 GBq/m2. Dosimetric studies show that the spleen has a higher predicted dose (range 1.5–19.4 mGy/MBq) than the kidneys (range 1.06–10.3 mGy/MBq) [42]. Nonetheless, the kidneys appear to be the critical dose-limiting organs. Even though the threshold absorbed dose for renal toxicity using conventional external radiotherapy is set at ~25 Gy, the dose to the kidneys may be higher with repeated administration of injected yttrium. Therefore, measures to reduce renal toxicity are strongly recommended in most trials. Positively charged amino acids have been shown to competitively inhibit renal tubular re-absorption and retention of 90Y-DOTATOC by renal interstitial cells, allowing administration of higher activities [18, 22, 26, 43, 44]. But the fact remains that despite this precaution, there is a median annual decline in creatinine clearance of 7.3% so that the loss of renal function may become clinically evident 1–5 years after 90Y-DOTATOC therapy in some patients [45]. Pre-existing risk factors such as hypertension and diabetes can also contribute to renal loss [37]. The large variability in individual renal uptake and wide inter patient differences in kidney side effects therefore justifies individualized dosimetry before administration of therapeutic doses of 90Y-DOTATOC [36]. Bone marrow depression is another very common side effect but fortunately it is usually transient. So, while there is no contraindication in administrating higher doses of 90Y-DOTATOC to patients with low myelotoxicity, it may be a limiting factor in patients with reduced bone marrow reserve secondary to myelotoxic chemotherapy or radiotherapy to bone [20, 26]. An interesting and innovative way to reduce systemic toxicity would be by radiopeptide brachytherapy. Recently recurrent high grade gliomas were successfully treated by local administration of 1,660–2,220 MBq of 90Y-DOTATOC with only minor side effects. In this approach, 98 Gy/GBq was delivered to residual tumor tissue with only 2.8 Gy/GBq exposures to the kidneys [46]. Theoretically, the same strategy applied on a larger extra cerebral setting of somatostatin receptor-positive tumors that are localized and easily accessible would allow the delivery of a higher concentration of 90Y-DOTATOC activity to the target tumor with marked reduction in toxicity.
Another promising agent currently being applied for PRRT is the 177Lu-labeled somatostatin analog DOTATATE, which has a ninefold higher affinity for the somatostatin receptor subtype 2 compared to DOTATOC [47]. This compound demonstrated the highest tumor uptake of all tested octreotide analogs so far, not only in rats but also in patients with NET with excellent tumor to kidney ratio [48]. Striking differences in the radiotherapeutic effects of 177Lu-DOTATATE and 90Y-DOTATOC in tumors of different sizes were also observed [33]. Even though there are as yet no prospective clinical studies directly comparing the efficacy and performance of 90Y-DOTATOC to 177Lu-DOTATATE, study in animals with various tumor sizes have shown that combined use of 90Y-DOTATOC and 177Lu-labeled octreotate therapy achieved better tumor remission than either 90Y or 177 Lu-labeled octreotate alone.
In conclusion, PRRT has a significant role in the treatment of NETs that express sstr2 receptors. With regard to 90Y-DOTATOC, clinical experience gained for over a decade proves that it is still a powerful agent for targeting large infiltrative NETs in selected patients. An objective response achieved in nearly a quarter of the patients treated so far bears testimony to this fact. In addition, symptomatic improvement and stability of the disease obtained in more than half of the patients treated with 90Y-DOTATOC justifies its use even in end stage disease. Nevertheless, a multidisciplinary approach aimed at early diagnosis of NETs and timely intervention with appropriate therapy is desirable for a more satisfactory outcome.
References
Kaltsas GA, Papadogias D, Makras P, Grossman AB. Treatment of advanced neuroendocrine tumors with radiolabelled somatostatin analogues. Endocr Relat Cancer. 2005;12:683–9.
Khanna G, Bushnell D, O’Dorisio MS. Utility of radiolabelled somatostatin receptor analogues for staging/restaging and treatment of somatostatin receptor-positive pediatric tumors. Oncologist. 2008;13:382–9.
Öberg K. Management of neuroendocrine tumors. Ann Oncol. 2004;15:iv293–8.
Bieligk S, Jaffe BM. Islet cell tumors of the pancreas. Surg Clin North Am. 1995;75:1025–40.
Öberg K. Advances in chemotherapy and biotherapy of endocrine tumors. Curr Opin Oncol. 1998;10:58–65.
Higgins GA, Recant L, Fischman AB. The glucagonoma: surgically curable diabetes. Am J Surg. 1979;137:142–8.
Prinz RA, Dorsch TR, Lawrence AM. Clinical aspects of glucagons producing islet cell tumors. Am J Gastroenterol. 1981;76:125–31.
Raut C, Kulke M, Glickman J, Swanson RS, Ashley SW. Carcinoid tumors. Curr Probl Surg. 2006;43:383–450.
De Herder WW, Hofland LJ, Van Der Lely AJ, Lambert SW. Somatostatin receptors in gastroentero-pancreatic neuroendocrine tumors. Endocr Relat Cancer. 2003;10:451–8.
De Jong M, Kwekkeboom D, Valkema R, Krenning EP. Radiolabelled peptides for tumor therapy: current status and future directions. Eur J Nucl Med. 2003;30:463–9.
McCarthy KE, Woltering EA, Antony LB. In situ radiotherapy with 111In-pentreotide State of the art and perspectives. Q J Nucl Med. 2000;44:88–95.
Antony LB, Woltering EA, Espenan GD, Cronin MD, Maloney TJ, McCarthy KE. Indium 111-pentetreotide prolongs survival in gastroenteropancreatic malignancies. Semin Nucl Med. 2002;32:123–32.
Béhé M, Heppeler A, Maecke HR. New somatostatin analogs for SPET and PET. Eur J Nucl Med 1996;23:1144 (abstract).
Van Essen M, Krenning EP, De Jong M, Valkema R, Kwekkeboom DJ. Peptide receptor radionuclide therapy with radiolabelled somatostatin analogues in patients with somatostatin receptor positive tumors. Acta Oncol. 2007;46:723–34.
Kwekkeboom DJ, Bakker WH, Kam BL, Teunissen JJM, Kooij PPM, de Herder WW, et al. Treatment of patients with gastro-enteropancreatic (GEP) tumors with the novel radiolabelled somatostatin analogue [177LuDOTA(0), Tyr(3) octreotide. Eur J Nucl Med Mol Imaging. 2003;30:417–22.
Otte A, Jermann E, Béhé M, Goetze M, Bucher HC, Roser HW, et al. DOTATOC: A powerful new tool for receptor mediated radionuclide therapy. Eur J Nucl Med. 1997;24:792–6.
Otte A, Mueller-Brand J, Dellas S, Nitzsche EU, Herrmann R, Maecke HR. Ytterium-90-labelled somatostatin-analogue for cancer treatment. Lancet. 1998;351:417–8.
Otte A, Herrmann R, Heppeler A, Behe M, Jermann E, Powell P, et al. Yttrium-90 DOTATAC first clinical results. Eur J Nucl Med. 1999;26:1439–47.
Paganelli G, Zoboli S, Cremonesi M, Mäcke HR, Chinol M. Receptor-mediated radionuclide therapy with 90Y-DOTA-D-Phe1-Tyr3-Octreotide: preliminary report in cancer patients. Cancer Biother Radiopharm. 1999;14:477–83.
Waldherr C, Pless M, Maecke HR, Haldemann A, Mueller-Brand J. The clinical value of [90Y-DOTA]-D-Phe1-Tyr3-octreotide (90Y-DOTATOC) in the treatment of neuroendocrine tumors: a clinical phase II study. Ann Oncol. 2001;12:941–5.
Waldherr C, Schumacher T, Maecke HR, Schirp U, Forrer F, Nitzsche EU, et al. Tumor response and clinical benefit in neuroendocrine tumors after 7.4 GBq 90Y-DOTATOC. J Nucl Med. 2002;43:610–6.
Paganelli G, Zoboli S, Cremonesi M, Bodei L, Ferrari M, Grana C, et al. Receptor mediated radiotherapy with 90Y-DOTA-D-Phe1-Tyr3-octreotide. Eur J Nucl Med. 2001;28:426–34.
Paganelli G, Bodei L, Junak DH, Rocca P, Papi S, Sierra ML, et al. 90Y-DOTA-D-Phe1-Tyr3-octreotide in therapy of neuroendocrine malignancies. Biopolymers (Peptide Science). 2002;66:393–8.
Chinol M, Bodei L, Cremonesi M, Paganelli G. Receptor-mediated radiotherapy with 90Y-DOTA-Dphe1-Tyr3- octreotide: the experience of the European Institute of Oncology Group. Semin Nucl Med. 2002;32:141–7.
Valkema R, Jamar F, Bakker WH, Norenberg J, Smith C, Stolz B, et al. Safety and efficacy of [Y-90-DOTA, Tyr(3)]octreotide (Y-90-SMT487;OCTREOTHERTM) peptide receptor radionuclide therapy (PRRT): preliminary results of a phase-I study (abstract OS-248). Eur J Nucl Med. 2001;28(Suppl):1025P.
Bodei L, Cremonesi M, Zoboli S, Grana C, Bartolomei M, Rocca P, et al. Receptor-mediated radionuclide therapy with 90Y-DOTATOC in association with amino acid infusion: a phase I study. Eur J Nucl Med. 2003;30:207–16.
Bodei L, Cremonesi M, Grana C, Rocca P, Bartolomei M, Chinol M, et al. Receptor radionuclide therapy with 90Y-[DOTA]0-Tyr3-Octreotide (90Y-DOTATOC] in neuroendocrine tumors. Eur J Nucl Med Mol Imaging. 2004;31:1038–46.
Valkema R, Pauwels S, Kvols LK, Barone R, Jamar F, Bakker WH, et al. Survival and response after peptide receptor radionuclide therapy with [90Y-DOTA0 Tyr3] octreotide in patients with advanced gastroenteropancreatic neuroendocrine tumors. Semin Nucl Med. 2006;36:147–56.
Frilling A, Weber F, Saner F, Bockisch A, Hofmann M, Mueller-Brand J, et al. Treatment with 90Y- and 177Lu-DOTATOC in patients with metastatic neuroendocrine tumors. J Surg. 2006;140(6):968–77.
Forrer F, Waldherr C, Maecke HR, Mueller-Brand J. Targeted radionuclide therapy with 90Y-DOTATOC in patients with neuroendocrine tumors. Anticancer Res. 2006;26:703–8.
Forrer F, Riedweg I, Maecke HR, Mueller-Brand J. Radiolabeled DOTATOC in patients with advanced paraganglioma and pheochromocytoma. Q J Nucl Med Mol Imaging. 2008;52:334–40.
Muros MA, Varsavsky M, Rozas PI, Valdivia J, Delgado JR, Forrer F, et al. Outcome of treating advanced neuroendocrine tumours with radiolabelled somatostatin analogues. Clin Transl Oncol. 2009;11:48–53.
De Jong M, Valkema R, Jamar F, Kvols LK, Kwekkeboom DJ, Breeman APW, et al. Somatostatin receptor-targeted radionuclide therapy of tumors: preclinical and clinical findings. Semin Nucl Med. 2002;32:133–40.
Konijnenberg MW. Is the renal dosimetry for [90Y-DOTA 0, Tyr3] octreotide accurate enough to predict thresholds for individual patients? Cancer Biother Radiopharm. 2003;18(4):619–25.
Forrer F, Mueller-Brand J, Maecke H. Pre-therapeutic dosimetry with radiolabelled somatostatin analogues in patients with advanced neuroendocrine tumors. Eur J Nucl Med Mol Imaging. 2005;32:511–2.
Barone R, Borson-Chazot F, Valkema R, Walrand S, Chauvin F, Gogou L, et al. Patient-specific dosimetry in predicting renal toxicity with (90)Y-DOTATOC: relevance of kidney volume and dose rate in finding a dose-effect relationship. J Nucl Med. 2005;46:99S–106S.
Bodei L, Cremonesi M, Ferrari M, Pacifici M, Grana CM, Bartolomei M, et al. Long-term evaluation of renal toxicity after peptide receptor radionuclide therapy with 90Y-DOTATOC and 177Lu-DOTATATE: the role of associated risk factors. Eur J Nucl Med Mol Imaging. 2008;35:1847–56 (epub 22 Apr 2008; erratum in Eur J Nucl Med Mol Imaging. 2008;35:1928).
Stolz B, Weckbecker G, Smith-Jones PM, Albert R, Raulf F, Bruns C. The somatostatin receptor-targeted radiotherapeutic [90Y]-DOTA-D-Phel-Tyr3-octeotide([90Y]-SMT487) eradicates experimental rat pancreatic CA 20948 tumors. Eur J Nucl Med. 1998;25:668–74.
Gotthardt M, Dijkgraaf I, Boerman OC, Oyen WJG. Nuclear Medicine imaging and therapy of neuroendocrine tumors. Cancer Imaging. 2006;6:S178–84.
Pless M, Waldherr C, Maecke H, Buitrago C, Herrmann R, Mueller-Brand J. Targeted radiotherapy for small cell lung cancer using 90Yttrium-DOTATOC, an Yttrium-labeled somatostatin analogue: a pilot trial. Lung Cancer. 2004;45:365–71.
Iten F, Müller B, Schindler C, Rochlitz C, Oertli D, Mäcke HR, et al. Response to [90Yttrium-DOTA]-TOC treatment is associated with long-term survival benefit in metastasized medullary thyroid cancer: a phase II clinical trial. Clin Cancer Res. 2007;13:6696–702.
Cremonesi M, Ferrari M, Bodei L, Tosi G, Paganelli G. Dosimetry in peptide radionuclide receptor therapy: a review. J Nucl Med. 2006;47:1467–75.
Smith MC, Liu J, Chen T, Schran H, Yeh CM, Jamar F, et al. OctreoTher: ongoing early clinical development of a somatostatin-receptor-targeted radionuclide antineoplastic therapy. Digestion. 2000;62((Suppl 1)):69–72.
Cybulla M, Weiner SM, Otte A. End-stage renal disease after treatment with 90Y-DOTATOC. Eur J Nucl Med. 2001;28:1552–4.
Valkema R, Pauwels SA, Kvols LK, Kwekkeboom DJ, Jamar F, de Jong M, et al. Long-term follow-up of renal function after peptide receptor radiation therapy with (90)Y-DOTA(0), Tyr(3)-octreotide and (177)Lu-DOTA(0), Tyr(3)-octreotate. J Nucl Med. 2005;46:83S–91S.
Heute D, Kostron H, Guggenberg EV, Ingorokva S, Gabriel M, Dobrozemsky G, et al. Response of recurrent high-grade glioma to treatment with 90Y-DOTATOC. J Nucl Med. 2010;51:397–400.
Reubi JC, Schar JC, Waser B, Wenger S, Heppeler A, Schmitt JS, et al. Affinity profiles for human somatostatin receptor subtypes SST1–SST5 of somatostatin radiotracers selected for scintigraphic and radiotherapeutic use. Eur J Nucl Med. 2000;27:273–82.
Kwekkeboom DJ, Bakker WH, Kooj PP, Konijnenberg MW, Srinivasan A, Erion JL, et al. [177Lu-DOTA0, Tyr3] octreotate: comparison with [111In-DTPAo] octreotide in patients. Eur J Nucl Med. 2001;28:1319–25.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nisa, L., Savelli, G. & Giubbini, R. Yttrium-90 DOTATOC therapy in GEP-NET and other SST2 expressing tumors: a selected review. Ann Nucl Med 25, 75–85 (2011). https://doi.org/10.1007/s12149-010-0444-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12149-010-0444-0