Abstract
Purpose
The aim of this study was to assess the diagnostic performance of 18F-Fluoride positron emission tomography (PET) or positron emission tomography/computed tomography (PET/CT) compared with bone scintigraphy (BS) planar or BS planar and single photon emission computed tomography (SPECT) in evaluating patients with metastatic bone tumor.
Materials and methods
We performed a meta-analysis of all available studies addressing the diagnostic accuracy of 18F-Fluoride PET, 18F-Fluoride PET/CT, BS planar, and BS planar and SPECT for detecting the metastatic bone tumor. We determined sensitivities and specificities across studies, calculated positive and negative likelihood ratios, and drew summary receiver operating characteristic curves using hierarchical regression models. We also compared the effective dose and cost-effectiveness estimated by data from the enrolled studies between 18F-Fluoride PET or PET/CT and BS planar or BS planar and SPECT.
Results
When comparing all studies with data on 18F-Fluoride PET or PET/CT, sensitivity and specificity were 96.2% [95% confidence interval (CI) 93.5–98.9%] and 98.5% (95% CI 97.0–100%), respectively, on a patient basis and 96.9% (95% CI 95.9–98.0%) and 98.0% (95% CI 97.1–98.9%), respectively, on a lesion basis. The Az values of 18F-Fluoride PET or PET/CT were 0.986 for the patient basis and 0.905 for the lesion basis, whereas those of BS or BS and SPECT were 0.866 for the patient basis and 0.854 for the lesion basis. However, the estimated effective dose and average cost-effective ratio were poorer for 18F-Fluoride PET or PET/CT than those of BS planar or BS planar and SPECT.
Conclusion
18F-Fluoride PET or PET/CT has excellent diagnostic performance for the detection of metastatic bone tumor, but the estimated effective dose and average cost-effective ratio are at a disadvantage compared with BS planar or BS planar and SPECT.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The presence of bone metastasis is an important prognostic factor in patients with cancer because bone is a common site of distant metastasis in patients with advanced stage. Bone metastasis causes much of the morbidity and disability in patients with cancer because of recent advances in treatment regimens. Proper evaluation of bone metastasis and early detection of occult bone metastasis is essential for correct treatment decisions and improved outcome. Bone scintigraphy (BS) and magnetic resonance imaging (MRI) play important roles in detecting occult bone metastases that are missed by physical examination. However, the sensitivity of BS is not satisfactory because of limited spatial resolution [1]. Although the diagnostic accuracy of whole body MRI with diffusion-weighted sequences to detect metastatic bone tumor is acceptable, this technique is available only for limited clinical studies to detect the occult bone metastasis [2].
Positron emission tomography (PET) with the use of the radiolabeled fluoride analog 18F-Fluoride has been applied in the assessment of bone metastasis in a variety of malignancies [3]. The accumulation of 18F-Fluoride in fluorapatite of osteoblastic and osteolytic lesions reflects increased blood flow and bone turnover because 18F-Fluoride ion can be exchanged with hydroxy groups in hydroxyapatite crystal. The overall accuracy of 18F-Fluoride PET has been favorable to detect bone metastasis using pathology as the reference standard. It has been suggested that 18F-Fluoride PET might be more accurate than BS in identifying bone metastasis because it is considered to have greater spatial resolution [4, 5]. Furthermore, the increasing use of integrated positron emission tomography/computed tomography (PET/CT) reveals that this modality is useful for the detection of bone metastasis, because it can provide information on 18F-Fluoride avidity and morphologic changes in lesions [6].
The diagnostic performance of 18F-Fluoride PET or PET/CT to detect bone metastasis is more accurate than that of BS [4–6]. However, results from previous studies have limited external validity because single studies are inconclusive due to small sample size, comparison of various combinations, and the use of a variety of methods for determining the diagnostic performance of 18F-Fluoride PET or PET/CT. The aim of our study was to undertake a meta-analysis of all available studies and address the diagnostic performance of 18F-Fluoride PET or PET/CT in evaluating bone metastasis in cancer patients.
Materials and methods
Data sources eligibility
Two reviewers searched Medline (from 1966 to November, 2009), SCOPUS, and Biological Abstracts. We used a search algorithm based on a combination of the terms: (1) 18F-Fluoride, 18F-Fluoride PET, or 18F-Fluoride PET/CT, (2) bone scintigraphy, and (3) bone metastasis and metastatic bone tumor. We applied no language restrictions. The two reviewers independently assessed potentially relevant citations for inclusion, and disagreements were resolved by consensus. Referenced articles of the retrieved studies were screened for additional studies. Investigators of eligible studies were contacted to ask about supplemental data when information relevant to the meta-analysis was missing. We excluded studies with verification bias including patients with non-solid tumors such as hematologic malignancies. Studies using 18F-Fluoride PET or PET/CT, or BS for evaluation of status after treatment, including recurrence, were excluded. Studies that contained patients whose diagnoses lacked standard reference regardless of contact with the authors or the presence of concomitant diseases were excluded.
Data extraction
Two reviewers extracted data from eligible studies independently and resolved any issues by consensus. We recorded author names, journal, year of publication, country of origin, number of patients, age, inclusion and exclusion criteria, study design, injected dose, imaging camera, technical characteristics and protocol of imaging, data type (patient- or lesion-based), number of reviewers who assessed and interpreted the results of imaging, definition of positive test result (qualitative or quantitative), and reference standard. The numbers of true-positive, false-positive, true-negative, false-negative, and equivocal findings for each modality were also recorded for both patient- and lesion-based series.
The effect of radiation exposure
We estimated the patient’s radiation doses in both 18F-Fluoride PET or PET/CT and BS (planar and/or single photon emission computed tomography, SPECT) from the available data of extracted articles. Effective doses from the CT portion were calculated from the simulation spreadsheet software ImPACT [7]. Because the CT tube current was automatically controlled using an auto exposure control system, the radiation doses were different depending on the body region. Therefore, we calculated the effective doses for the head, chest, and abdominal regions separately using ImPACT, and added these values to obtain the effective dose for the whole body [8, 9]. Absorbed dose and effective dose in each organ and tissue from radiopharmaceuticals were obtained from the International Commission on Radiological Protection (ICRP) publication 80 [10].
Cost-effectiveness
In all extracted studies, cost-effectiveness was compared by each modality: BS planar and/or SPECT, 18F-Fluoride PET, and 18F-Fluoride PET/CT. Expected effectiveness was defined as the proportion of correctly diagnosed patients. Direct costs were referred to the perspective of Japanese and American Hospitals. Expected costs were estimated in Japanese-yen (\) for the year of 2010 official charge for BS. Expected costs were also calculated in US $ for the year of 2010 based on CMS Medicare rate for BS. Since 18F-Fluoride is not reimbursed by Japanese insurance, CMS Medicare or private insurers in the USA, hospital charges were estimated with reference to 18F-FDG PET or PET/CT by the published ranges for official charges or the CPT codes. Average cost-effectiveness ratios were calculated by dividing expected costs by expected effectiveness, which was the accuracy of the included studies [11]. These are demonstrated as US $ and Euro (EUR) referring to the respective exchange rate on 4 February 2010.
Statistical analysis
Data on the diagnostic performance of images studies were combined quantitatively across eligible studies. We combined sensitivities and specificities across studies to estimate the weighted mean values using an inverse of variance of sensitivity and specificity from each study as a weight. To obtain the overall diagnostic accuracy of each modality for all combined studies, the analyses addressed the diagnosis of bone metastasis per patient and per lesion. The summary receiver operating characteristic (SROC) curve was estimated using a linear regression model with weighted least squared method for the logarithms of sensitivity, and specificity was made to show the summary trade-off between sensitivity and specificity across the eligible studies and the summary likelihood ratios. The effective doses between 18F-Fluoride PET or PET/CT and BS planar or BS were compared by Student’s t test. A p value less than 0.05 was considered indicative of statistical significance.
Results
Our literature search yielded 35 articles; 24 were excluded upfront after reading the abstract because they did not contain any diagnostic information. Thus, 11 articles were available for our analyses that represented a total of 425 patients. Of these 11 studies, data on patients were available in 8 for BS planar or BS planar and SPECT and 10 for 18F-Fluoride PET or PET/CT, and data on lesions in 5 for BS planar or BS planar and SPECT and 11 for 18F-Fluoride PET or PET/CT. A total of 350 patients were analyzed for the diagnostic accuracy to detect metastatic bone tumor on a patient basis, while a total of 255 patients were analyzed on a lesion basis which included 1,164 lesions evaluated by 18F-Fluoride PET and/or PET/CT and 474 lesions evaluated by BS planar or BS planar and SPECT.
Two of the 11 studies (18%) were performed using only 18F-Fluoride PET or PET/CT without comparison with BS planar or BS planar and SPECT. Four of 11 studies (36%) were stratified by histology of the primary tumor: lung carcinoma and prostate carcinoma in 2 studies each. Five studies (45%) stated that they were prospective. The evaluation of study results was stated to have been done in a qualitative manner in all studies, whereas one study stated explicitly that evaluation was also performed by quantitative method using active ratio of lesion. Reference standard consisted of other imaging studies including CT, MRI, radiography, 18F-Fluorodeoxyglucose (18F -FDG) PET, clinical follow-up, and biopsy. However, one study did not comment on the method of reference standard. After contacting the corresponding author for this study, we were informed that follow-up CT and MRI had been used as the reference standard. Information regarding the technical characteristics of imaging, inclusion, and exclusion criteria is summarized in Table 1.
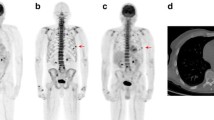
Independent estimates and likelihood ratios are demonstrated in Table 2. When comparing all studies with data on 18F-Fluoride PET or PET/CT, sensitivity and specificity were 96.2 and 98.5%, respectively, on a patient basis and 96.9 and 98.0%, respectively, on a lesion basis. However, in studies stratified by PET and PET/CT, sensitivity and specificity remained high. Sensitivity of BS changed according to the use of planar alone or planar plus SPECT and according to the use of patient- or lesion-based analyses. However, the specificity of BS estimates was similar to those of 18F-Fluoride PET or PET/CT. The SROC curves and the Forest plot of odds ratio showed excellent diagnostic performance of 18F-Fluoride PET and PET/CT studies combined for the patient- and lesion-based analyses and considerably good performance in combined studies of BS planar and SPECT (Figs. 1, 2, 3).
Summary receiver operating characteristic (SROC) curve for the diagnostic performance of 18F-Fluoride PET or PET/CT (a) and BS and/or SPECT (b) for a patient basis. The size of the circles indicates the weight of each study. The area under the SROC curve (Az value) is 0.986 for 18F-Fluoride PET or PET/CT and 0.866 for BS and/or SPECT
Summary receiver operating characteristic (SROC) curve for the diagnostic performance of 18F-Fluoride PET or PET/CT (a) and BS and/or SPECT (b) for a lesion basis. The size of the circles indicates the weight of each study. The area under the SROC curve (Az value) is 0.905 for 18F-Fluoride PET or PET/CT and 0.854 for BS and/or SPECT
Our literature research revealed that the effective doses by injected 18F-Fluoride ranged from 2.7 to 15.0 mSv, whereas these values ranged from 4.2 to 5.7 mSv for BS studies. Five of 11 studies were evaluated by PET/CT comprising three scanner types. The effective dose from the CT portion of PET/CT ranged from 8.4 to 13 mSv. Therefore, the effective dose of 18F-Fluoride PET or PET/CT calculated from these studies ranged from 2.7 to 28.0 mSv. Effective doses of 18F-Fluoride PET or PET/CT were significantly higher than those of BS planar or BS planar and SPECT (p = 0.005).
In Japan, the costs of PET or PET/CT per study are ¥75,000 and ¥86,250, respectively. A total of 96.3% of all patients were correctly diagnosed from the included studies on a patient basis. If the total product of 18F-Fluoride were covered by each institution, the average cost per study would be at least ¥77,882 for PET and ¥89,564 for PET/CT. When Tc-99m-methyl-diphosphate (MDP) of 740 MBq is used, the average costs per study for BS planar or BS planar and SPECT are ¥28,399 and ¥30,044, respectively. Since a total of 73.5% of all patients were correctly diagnosed in the included studies, the average cost-effective ratio would be ¥38,638 for BS planar and ¥40,876 for BS planar and SPECT, respectively. The average cost per study in US was estimated by the published ranges for the CPT codes. For 18F-Fluoride PET or PET/CT, the average cost per study ranged from US $1,000 to 1,500. The average cost-effective ratio ranged from US $1,038 to 1,558 (1,437–2,157 EUR). Similarly, the average cost per study was 297 US$ by CMS Medicare for BS planar or BS planar and SPECT. The average cost-effective ratio would be US $404 (559 EUR) per study for BS planar or BS planar and SPECT.
Discussion
When compared with those of BS planar and/or SPECT, the diagnostic performance of 18F-Fluoride PET or PET/CT was excellent in detecting the metastatic bone tumor. Meta-analysis of the data allowed us to investigate how 18F-Fluoride PET or PET/CT can contribute to the diagnosis of metastatic bone tumor.
Based on the results of this meta-analysis, the performance of 18F-Fluoride PET or PET/CT is satisfactory because only a low percentage of false-negative or -positive result is found. Reflecting the high accuracy of 18F-Fluoride PET or PET/CT, a higher detection rate of degenerative lesions may lead to an increasing rate of false-positive results [6, 15].
Thus, there is possible evidence to support the use of 18F-Fluoride PET or PET/CT to detect metastatic bone tumor. Some possible explanations for this failure of 18F-Fluoride PET or PET/CT to detect metastatic bone tumor include the close anatomic proximity of bone metastasis to degenerative structures of bone that are visualized with 18F-Fluoride PET or PET/CT and the size of occult bone metastases which may be below the spatial resolution of 18F-Fluoride PET or PET/CT. However, we should also note that the performance of other diagnostic methods such as whole-body MRI with diffusion-weighted sequences was equal to those of 18F-Fluoride PET or PET/CT [2].
Atomic Energy of Canada Limited (AECL) has announced that the supply of technetium preparation must be reduced because of repairs being made to a heavy water leak at the reactor in Chalk River, Ontario, Canada. Most countries importing technetium preparations have to restrict the numbers of BS for detecting metastatic bone tumor for the time being. Our results of meta-analysis revealed that the diagnostic performance of 18F-Fluoride PET or PET/CT was excellent to detect the metastatic bone tumor. Therefore, we can substitute 18F-Fluoride PET or PET/CT with BS until the supply of technetium preparations is restored.
Current advances in diffusion-weighted MR imaging have facilitated the detection of metastatic bone tumor with high accuracy. Nemeth et al. [22] described an MRI protocol using diffusion-weighted sequences in which the detectability of metastatic bone tumor was improved compared with conventional MRI. However, this technique is insensitive for detecting lesions with sclerotic osseous reaction, and is not available for whole-body imaging at one time. Technical advances in whole-body MRI will enable us to use diffusion-weighted sequences for detecting the metastatic bone tumor in the near future.
The included studies revealed that the effective dose of 18F-Fluoride PET or PET/CT ranged from 2.7 to 28.0 mSv. Some side effects, including a decrease in sperm count, may appear if the patient is exposed to a radiation dose of 542 mSv at one time [8]. However, effective doses of 18F-Fluoride PET or PET/CT were significantly higher than those of BS planar or BS planar and SPECT. Therefore, deterministic effects should be avoided by reducing the dose of 18F-Fluoride and by low-dose CT portion of PET/CT because screening of bone metastasis is generally performed at an interval of approximately 6 months or 1 year, and the exposure is not of an acute nature.
Although our estimates of the cost of 18F-FDG PET or PET/CT were based on the hospital charge of 18F-FDG PET or PET/CT based on the official charge for medicine or CMS Medicare, the average cost-effective ratio ranged from ¥77,882 to ¥89,564 (US $1,038–1,558 or 1,437–2,157 EUR). In contrast, the average cost-effective ratio ranged from ¥38,638 to ¥40,876 (US $404 or 559 EUR) per study for BS planar or BS planar and SPECT. Regarding the high expense of surgery, which may be avoided by more accurate diagnostic procedures, the additional cost of BS planar or BS planar and SPECT or 18F-FDG PET or PET/CT seems reasonable. However, our estimates were based on limited data of 18F-FDG PET or PET/CT. Since resource prices differ in other countries, further studies are needed for false positive or negative interpretation by an uncritical use of 18F-FDG PET or PET/CT.
The limitations of the present study include source of heterogeneity (publication bias) which results in systematic differences in effect size estimates derived from small versus large studies. The available data are consistent with great improvement in sensitivity with 18F-Fluoride PET or PET/CT over BS planar or BS planar and SPECT in the studies enrolled. Although the confidence intervals include a low sensitivity for BS planar or BS planar and SPECT, the number of BS planar and SPECT studies was limited. Thus, the potential incremental diagnostic benefit still leaves a large percentage of false negatives on BS planar and SPECT. The inclusive criteria showed a wide variety of histologic diagnoses in some of the studies. However, 18F-Fluoride PET or PET/CT is considered to more sensitively detect bone metastasis with sclerotic osseous reaction than those with lytic destruction. Studies that included only tumors with a tendency to develop sclerotic bone metastasis may influence the diagnostic accuracy of this meta-analysis. There was a risk of subjective interpretation because the interpretation of 18F-Fluoride PET or PET/CT was performed by two reviewers qualitatively in all studies, but the presence/absence of blinding was unclear. In the definition of bone metastasis, most studies lacked not only histologic confirmation, but also direct comparison with whole-body MRI. However, biopsies of multiple lesions in one patient were not substantial, and whole-body MRI was limited to clinical use in the entire study period. Further validation studies using 18F-Fluoride PET or PET/CT compared with whole-body MRI are needed in larger populations. The cost-effectiveness of 18F-Fluoride PET or PET/CT for the detection of metastatic bone tumor has to be systematically re-considered.
In conclusion, our study provided evidence to support the possible application of 18F-Fluoride PET or PET/CT to detect metastatic bone tumors. BS planar or BS planar and SPECT appear to have limited sensitivity but similar specificity to detect metastatic bone tumor both on a patient and lesion basis. Further research is required to determine whether there is indeed an incremental diagnostic improvement with 18F-Fluoride PET or PET/CT over other imaging methods with consideration of radiation dose, cost-effectiveness, and potential complications against the yield of information.
References
Ghanem N, Uhl M, Brink I, Schäfer O, Kelly T, Moser E, et al. Diagnostic value of MRI in comparison to scintigraphy, PET, MS-CT and PET/CT for the detection of metastases of bone. Eur J Radiol. 2005;55:41–55.
Goudarzi B, Kishimoto R, Komatsu S, Ishikawa H, Yoshikawa K, Kandatsu S, et al. Detection of bone metastases using diffusion weighted magnetic resonance imaging: comparison with 11C-methionine PET and bone scintigraphy. Magn Reson Imaging. 2010 (in press).
Vallabhajosula S. (18)F-labeled positron emission tomographic radiopharmaceuticals in oncology: an overview of radiochemistry and mechanisms of tumor localization. Semin Nucl Med. 2007;37:400–19.
Cook GJ, Fogelman I. Detection of bone metastases in cancer patients by 18F-fluoride and 18F-fluorodeoxyglucose positron emission tomography. Q J Nucl Med. 2001;45:47–52.
Grant FD, Fahey FH, Packard AB, Davis RT, Alavi A, Treves ST. Skeletal PET with 18F-fluoride: applying new technology to an old tracer. J Nucl Med. 2008;49:68–78.
Even-Sapir E, Mishani E, Flusser G, Metser U. 18F-Fluoride positron emission tomography and positron emission tomography/computed tomography. Semin Nucl Med. 2007;37:462–9.
ImPACT. CT patient dosimetry Excel spreadsheet (version 0.99v, 17 June 2004). http://www.impactscan.org/.
Murano T, Tateishi U, Iinuma T, Shimada N, Daisaki H, Terauchi T, et al. Evaluation of the risk of radiation exposure from new 18FDG PET/CT plans versus conventional x-ray plans in patients with pediatric cancers. Ann Nucl Med. 2010;24(4):261–7.
Jones D, Shrimpton P. NRPB-SR250: normalised organ doses for X-ray computed tomography calculated using Monte Carlo techniques. National Radiological Protection Board. 1993.
International Commission on Radiological Protection. 1990 recommendations of the International Commission on Radiological Protection. ICRP publication 60. Annals of the ICRP, vol 21, issue 1–3. Oxford: Elsevier; 1991.
Hetzel M, Arslandemir C, König HH, Buck AK, Nüssle K, Glatting G, et al. F-18 NaF PET for detection of bone metastases in lung cancer: accuracy, cost-effectiveness, and impact on patient management. J Bone Miner Res. 2003;18:2206–14.
Hoh CK, Hawkins RA, Dahlbom M, Glaspy JA, Seeger LL, Choi Y, et al. Whole body skeletal imaging with [18F]fluoride ion and PET. J Comput Assist Tomogr. 1993;17:34–41.
Hoegerle S, Juengling F, Otte A, Altehoefer C, Moser EA, Nitzsche EU. Combined FDG and [F-18]fluoride whole-body PET: a feasible two-in-one approach to cancer imaging? Radiology. 1998;209:253–8.
Schirrmeister H, Guhlmann A, Kotzerke J, Santjohanser C, Kühn T, Kreienberg R, et al. Early detection and accurate description of extent of metastatic bone disease in breast cancer with fluoride ion and positron emission tomography. J Clin Oncol. 1999;17:2381–9.
Schirrmeister H, Guhlmann A, Elsner K, Kotzerke J, Glatting G, Rentschler M, et al. Sensitivity in detecting osseous lesions depends on anatomic localization: planar bone scintigraphy versus 18F PET. J Nucl Med. 1999;40:1623–9.
Schirrmeister H, Glatting G, Hetzel J, Nüssle K, Arslandemir C, Buck AK, et al. Prospective evaluation of the clinical value of planar bone scans, SPECT, and (18)F-labeled NaF PET in newly diagnosed lung cancer. J Nucl Med. 2001;42:1800–4.
Even-Sapir E, Metser U, Flusser G, Kollender Y, Lerman H, Lievshitz G, et al. Assessment of malignant skeletal disease: initial experience with 18F-fluoride PET/CT and comparison between 18F-fluoride PET and 18F-fluoride PET/CT. J Nucl Med. 2004;45:272–8.
Even-Sapir E, Metser U, Mishani E, Lievshitz G, Lerman H, Leibovitch I. The detection of bone metastases in patients with high-risk prostate cancer: 99mTc-MDP Planar bone scintigraphy, single- and multi-field-of-view SPECT, 18F-fluoride PET, and 18F-fluoride PET/CT. J Nucl Med. 2006;47:287–97.
Beheshti M, Vali R, Waldenberger P, Fitz F, Nader M, Loidl W, et al. Detection of bone metastases in patients with prostate cancer by 18F fluorocholine and 18F fluoride PET-CT: a comparative study. Eur J Nucl Med Mol Imaging. 2008;35:1766–74.
Kawaguchi M, Tateishi U, Shizukuishi K, Suzuki A, Inoue T. F-18 fluoride uptake in bone metastasis: morphologic and metabolic analysis on integrated PET/CT. Ann Nucl Med. 2010;24(4):241–7.
Iagaru A, Mittra E, Yaghoubi SS, Dick DW, Quon A, Goris ML, et al. Novel strategy for a cocktail 18F-fluoride and 18F-FDG PET/CT scan for evaluation of malignancy: results of the pilot-phase study. J Nucl Med. 2009;50:501–5.
Nemeth AJ, Henson JW, Mullins ME, Gonzalez RG, Shaefer PW. Improved detection of skull metastasis with diffusion-weighted MR imaging. Am J Neuroradiol. 2007;28:1088–92.
Acknowledgments
The authors thank the Japanese Society of Nuclear Medicine for their vulnerable assistance of data interpretation and also thank Kengo Ito, MD, Kimiichi Uno, MD, and Seigo Kinuya, MD for their helpful suggestions. This study was supported in part by grants from Scientific Research Expenses for Health and Welfare Programs and the Grant-in-Aid for Cancer Research from the Ministry of Health, Labour.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tateishi, U., Morita, S., Taguri, M. et al. A meta-analysis of 18F-Fluoride positron emission tomography for assessment of metastatic bone tumor. Ann Nucl Med 24, 523–531 (2010). https://doi.org/10.1007/s12149-010-0393-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12149-010-0393-7