Abstract
A large number of studies have examined the association between depressive symptoms and sleep quality, however, the psychological mechanism underlying the association remains nebulous. Using moderated mediation analysis, the present study aimed to examine to what extent the association was mediated by rumination and whether the mediation effect was moderated by self-compassion. Self-reported measures on depressive symptoms, rumination, self-compassion, and sleep quality were collected from 564 college students. The results showed that (a) rumination mediated the association between depressive symptoms and sleep quality, and (b) self-compassion moderated the mediation effect. Specifically, the mediating effect of rumination was stronger for students with low self-compassion than those with high self-compassion. These findings suggest that self-compassion may be a useful intervention target for health care practitioners to evaluate and improve sleep quality for individuals suffering from depressive symptoms.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
People usually spend about one-third of their lifetime in sleeping, and good sleep quality is essential for the body to recover from weariness and regain physical and psychological energy (Opp 2009). Research suggests that an increasing number of people from young to old are experiencing sleep problems such as poor sleep quality (Hinz et al. 2017; Zhang et al. 2017). Due to a variety of internal (e.g., variable sleep schedules and poor sleep habits) and external factors (e.g., numerous challenges and environmental noise), college students have become one of the most vulnerable populations to various types of sleep disorders (Brown et al. 2002; Piro et al. 2018). Studies have indicated that sleep problems are very common among university students worldwide (e.g., Schlarb et al. 2017; Jiang et al. 2015). In China, for example, Li et al. (2018) found that prevalence of sleep disturbances in undergraduates was 25.7% across 76 studies involving 112,939 students. Moreover, a wealth of studies demonstrated that poor sleep quality was associated with several students’ physical and psychological health problems, such as somatic complaints (Schlarb et al. 2017), decreased accuracy of emotional memory recognition (Tempesta et al. 2015), dysfunctional social relationships (Carney et al. 2006), poor academic performance (Piro et al. 2018), and even suicide (Holdaway et al. 2018).
Considering the prevalence and negative impacts of poor sleep quality among college students, it is necessary to understand the potential risk factors for sleep quality. Past research has explored several potential risk factors (e.g., Amaral et al. 2018; Brown et al. 2002). Among them, depression was considered to be the most frequent and influential (Katz and McHorney 1998; Riemann et al. 2001), supported by both longitudinal studies (e.g., Roberts and Duong 2013) and meta-analysis research (e.g., Bao et al. 2017). For instance, Bao et al. (2017) suggested that depression increased risk by about 70% for onset and exacerbation of sleep disturbances.
Nevertheless, the previous research largely focused on the direct association between depressive symptoms and sleep quality; hence, the mechanism underlying this association is still unclear. In particular, there is a lack of empirical studies examining the mediating and moderating mechanisms involved in this relationship. To fill in this gap in the literature, the present study aimed to examine the potential mediating effect of rumination in the relationship between depressive symptoms and sleep quality and whether it is moderated by self-compassion. The study will shed light on the mechanism of how depressive symptoms influence sleep quality, which could be further used to inform the treatment for sleep problems.
The Mediating Role of Rumination between Depressive Symptoms and Sleep Quality
Rumination is conceptualized as passively and repetitively focusing on symptoms of distress and its possible causes and consequences without making active changes (Nolen-Hoeksema 1991). Indeed, rumination is essentially a deleterious action that manifests itself in additional negative thinking, undermines the ability to cope with problems, and results in negative and persistent thoughts about past, present, and future (Nolen-Hoeksema et al. 2010). Takano and Tanno (2009) argued that depression is characterized by accentuated self-focused attention, which may catalyze into maladaptive rumination. Furthermore, the metacognitive model (Wells 2009) considers that rumination, threat monitoring, and maladaptive coping behaviors are the components of Cognitive Attentional Syndrome (CAS) in depression wherein rumination is the central feature. Thus, depression could be an important vulnerability factor for rumination (Slavish and Graham-Engeland 2015). Longitudinal studies have shown that greater baseline depression predicted increase in rumination over time (Krause et al. 2018; Nolen-Hoeksema et al. 2007).
In addition, research showed that rumination played a significant role in the onset and continuance of insomnia (Stoia-Caraballo et al. 2008; Takano et al. 2012). According to the perseverative cognition hypothesis (Brosschot et al. 2006), rumination can induce sustained psycho-physiological arousal which can lead to short- and long-term disturbances during sleep. Empirical studies have found negative effects of rumination on sleep patterns among college students (Takano et al. 2012; Zawadzki et al. 2013) and young adults (Slavish and Graham-Engeland 2015; Winzeler et al. 2014). For instance, using a one-week daily sampling approach, Pillai et al. (2014) found that pre-sleep rumination was significantly associated with sleep onset latency. Several experimental studies also showed that rumination had a detrimental impact on sleep quality for students high in rumination (e.g., Guastella and Moulds 2007; Zoccola et al. 2009).
Considering that depressive symptoms are positively associated with rumination, and rumination is negatively associated with sleep quality, it is reasonable to hypothesize that rumination may mediate the relationship between depressive symptoms and sleep quality. Indeed, past research has shown that rumination mediates the effects of stress (Amaral et al. 2018) and negative affect such as depressed mood and loneliness (Slavish and Graham-Engeland 2015; Zawadzki et al. 2013) on sleep quality. Therefore, we hypothesized that increased depressive symptoms would increase rumination, which in turn decrease sleep quality (Hypothesis 1).
The Moderating Role of Self-Compassion
Although depression is a robust risk factor for sleep quality (e.g., Riemann et al. 2001), students may not be equally susceptible to sleep problems. For example, some individual traits may protect students from the negative impact of depressive symptoms on sleep quality, and one such trait is self-compassion. Different definitions for self-compassion have been available in the literature (e.g., Gilbert 2005; Neff 2003a). The one provided by Neff from a Buddhist framework is most popular. According to Neff, self-compassion refers to “being open to and moved by one’s own suffering, experiencing feelings of caring and kindness toward oneself, taking an understanding, nonjudgmental attitude toward one’s inadequacies and failures, and recognizing that one’s experience is part of the common human experience” (Neff 2003a, p. 224). There are three central components of self-compassion: self-kindness versus self-judgment (being loving and kindness toward oneself rather than being critical and harsh), a sense of common humanity versus isolation (the extent of individuals realizing everyone experiences these events rather than feeling isolated by their experiences), and mindfulness versus over-identification (using a balanced way to one’s thoughts and feelings rather than over-identifying them). By fostering the acceptance of reality, these components can enhance one’s capacity to respond to situations beyond sleep matters adaptively and functionally (Neff 2003a). Moreover, by inducing the feelings of being cared for, connected, and emotionally calm, self-compassion can promote one’s well-being (Gilbert 2005; Raes 2010).
For instance, growing empirical evidence from college students has shown that self-compassion is related to positive psychological outcomes such as relational well-being (Yarnell and Neff 2013), and is inversely correlated with negative psychological distress such as depression and anxiety (Neff 2003a; Raes 2010). Regarding the relationship between self-compassion and rumination, past research has consistently found that increased self-compassion was significantly associated with decreased rumination (Fresnics and Borders 2017; Johnson and O'Brien 2013; Neff 2003a; Raes 2010; Smeets et al. 2014). For example, Neff et al. (2007a) found that increased self-compassion after a one-month intervention saw a measurable decrease in rumination.
In addition to its positive effects on psychological outcomes, increasing self-compassion has recently been used as an important strategy to cope with negative emotions through fostering great awareness and understanding of emotions (Diedrich et al. 2014; Odou and Brinker 2014), and enhancing emotional flexibility (Beshai et al. 2018). For example, over a five-month treatment in which self-compassion was present, the participants showed diminished levels of depressive symptoms (Odou and Brinker 2015; Raes 2011). Similarly, Karl et al. (2018) suggested that self-compassion is associated with more adaptive responses to mood challenges in individuals with a history of depression. These findings indicated that self-compassion serves as a potentially important protective factor for depression (Wadsworth et al. 2018). Although prior research has not directly demonstrated the possible moderating role of self-compassion in the relationship between depressive symptoms and rumination, there has been some evidence from relevant studies that support this assumption (Ramel et al. 2004). For instance, self-compassion was negatively correlated to symptom-focused rumination in depressed outpatients (Krieger et al. 2013). After a daily self-compassion intervention for 1 week, patients with major depressive disorder reported a significant decrease in ruminative thoughts compared to those in a control condition (Butz and Stahlberg 2018). Therefore, we hypothesize that self-compassion would moderate the relationship between depressive symptoms and rumination such as depressive symptoms have a stronger effect on rumination for students with low self-compassion (Hypothesis 2).
The Current Study
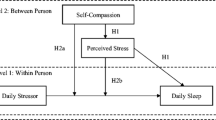
Based on the literature review presented above, this study aimed to test the psychological mechanism in the relationship between depressive symptoms and sleep quality among Chinese college students by testing a moderated mediation model (see Fig. 1). Overall, the present study examined (1) whether rumination mediates the influences of depressive symptoms on sleep quality, and (2) whether self-compassion moderates the mediating effect of rumination by modifying the link between depression and rumination.
Methods
Participants and Procedures
Participants were 564 college students from a public university in the Henan province of China. The mean age of the participants was 20.32 years (SD = 1.30, range = 17–24). Among them, 48.4% of them were females, 33.2% were freshmen, 28.2% were sophomores, 34% were juniors, and 4.6% were seniors. The survey was conducted in classrooms after informed consent was obtained from the participants or parents for three students who were under 18. The participants were informed that their responses would be kept anonymous and confidential, and they were free to withdraw at any time during the data collection. The investigation adopted the form of pen-paper, and the survey questions are presented in the same order across all participants (basic information such as age, gender, and grade, followed by the instrument battery). Trained data collectors administered the questionnaires using standard instructions. Participants were given approximately 15 min to complete the questionnaires. The completed questionnaires were checked and collected by data collectors. If there are omissions in required fields, data collectors asked participants to complete them and thereby resulting in no missing data. The Research Ethics Committee of the correspondence author’s institution approved this study.
Measures
Depressive Symptoms
Depressive symptoms were measured by the Beck Depression Inventory (BDI; Beck et al. 1961). The BDI consists of 21 items to assess various cognitive, affective, and somatic symptoms of depression. Participants rate their responses on a Likert-type scale from “0” to “3”. The total score was achieved by summing all responses, with higher scores indicating greater severity of depressive symptoms. The BDI has been widely used and validated for Chinese college students (e.g., Li et al. 2017; the internal consistency was .93). The Cronbach’s α in the present study was .89.
Sleep Quality
The Chinese version of the Pittsburgh Sleep Quality Index (PSQI; Liu et al. 1996) was used to estimate the level of subjective sleep quality. The PSQI comprises 18 items (e.g., “During the past month, when have you usually gone to bed at night?” and “During the past month, when have you usually gotten up in the morning?”), resulting in seven components such as sleep latency, sleep duration, habitual sleep efficiency. The seven component scores are summed to a total PSQI score (Buysse et al. 1989), with higher scores representing poorer subjective sleep quality. The PSQI has been widely used and validated for Chinese adolescents (e.g., Liu et al. 2018; the internal consistency was .76). The Cronbach’s α in the present study was .71.
Rumination
Rumination was measured by the Chinese version of Ruminative Response Scale (RRS; Yang et al. 2009), which is a subscale of the Response Styles Questionnaire (Nolen-Hoeksema 1991). It consists of 22 items scored on a Likert-type scale ranging from 1 (almost never) to 4 (almost always), with higher scores indicating a higher tendency for rumination. Example items include: “Go away by yourself and think about why you feel this way” and “Think about my friends will be tired of me and my problems.” The RRS has been used and validated for Chinese adolescents (e.g., Liu et al. 2018; the internal consistency was .92). The Cronbach’s α in the present study was .90.
Self-Compassion
Self-compassion was assessed with the Chinese version of Self-Compassion Scale (SCS; Chen et al. 2011; Neff 2003a). The SCS is a 26-item self-report inventory that consists of six different facets: self-kindness, self-judgment, common humanity, isolation, mindfulness, and over-identification. Sample items include: “I’m disapproving and judgmental about my own flaws and inadequacies” and “I try to see my failings as part of the human condition.” Participants answered each item on a 5-point Likert-type scale ranging from 1 (strongly disagree) to 5 (strongly agree), with higher scores indicating higher levels of self-compassion. The SCS has been used and validated for Chinese adolescents (e.g., Chu et al. 2018; the internal consistency was .82). The Cronbach’s α in the present study was .87.
Statistical Analyses
Data analyses were performed using SPSS 19.0. Descriptive statistics including means, SDs, and Pearson correlation coefficients were calculated for all variables. The potential presence of common method bias in the present study was also assessed. To test our hypotheses, we evaluated a moderated mediation model (see Fig. 1) using the SPSS macro PROCESS (Model 7; Hayes 2013). As shown in Fig. 1, the tested model included one independent variable (depressive symptoms), one mediator (rumination), one moderator (self-compassion), and one dependent variable (sleep quality). All variables were standardized to minimize multicollinearity. Thus the coefficients in the model represent standardized regression coefficients. The indirect effect of depressive symptoms on sleep quality through rumination was tested using nonparameteric boostrapping with 5000 boostrap samples.
Results
Common Method Bias
Following the procedure recommended by Podsakoff et al. (2012), Harman one-factor test was used to determine the extent to which correlations among the variables may have resulted from common method variance. The result showed that the first principal factor explained only 19.25% of the variance, indicating that there was no substantial common method bias.
Descriptive Statistics
Means, standard deviations, and correlations of the major variables are presented in Table 1. Both depressive symptoms and rumination were positively correlated with sleep quality (r = .47, .41, respectively, p < .01) and self-compassion was negatively correlated with sleep quality (r = − .09, p < .05). Depressive symptoms were positively correlated with rumination (r = .61, p < .01) and rumination was negatively correlated with self-compassion (r = − .20, p < .01). The correlation between depressive symptoms and self-compassion was non-significant (r = − .08, p > .05). Moreover, age was positively related to sleep quality (r = − .10, p < .05). On average, females reported significantly poorer sleep quality than males [t (562) = 3.03, p < .01]. As such, age and gender were controlled in the moderated mediation analysis.
Testing for Moderated Mediation Effect
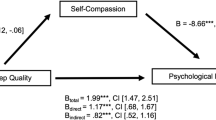
The result from the moderated mediation model is presented in Table 2 and Fig. 2. Depressive symptoms were positively associated with rumination (β = .61, p < .001), and rumination was positively associated with sleep quality (β = .19, p < .001). These results indicated a significant mediating effect of rumination in the relationship between depressive symptoms and sleep quality. In addition, there was a significant interaction effect between depressive symptoms and self-compassion on rumination (β = − .12, p < .001), suggesting that the relationship between depressive symptoms and rumination was moderated by self-compassion. Accordingly, the relationship between depressive symptoms and rumination was plotted when the levels of self-compassion were low (one SD below the mean) and high (one SD above the mean), respectively (see Fig. 3). Simple slope analysis showed that the positive association between depressive symptoms and rumination was stronger when self-compassion was low (β = .61, t = 6.02, p < .001), but weaker when self-compassion was high (β = .45, t = 3.70, p < .01). Consequently, the indirect effect of depressive symptoms on sleep quality via rumination was also stronger for college students with low self-compassion (β = .13, bootstrap 95% CI = [.07, .21]) than for those with high self-compassion (β = .09, bootstrap 95% CI = [.04, .14]). These results indicated that the mediating effect of rumination in the relationship between depressive symptoms and sleep quality was moderated by self-compassion. After accounting for the indirect effect of rumination, depressive symptoms were still positively related to sleep quality (β = .35, p < .01), indicating that rumination was only one of the mechanisms explaining the relationship between depressive symptoms and sleep quality.
Discussion
The present study conducted a moderated mediation analysis to explore the psychological mechanisms underlying the association between depressive symptoms and sleep quality. The results showed that the relationship between depressive symptoms and sleep quality was mediated by rumination, and self-compassion moderated the mediating effect of rumination by modifying the connection between depressive symptoms and rumination. Specifically, the mediating effect of rumination was stronger for students low in self-compassion than for those high in self-compassion.
The Mediating Role of Rumination between Depressive Symptoms and Sleep Quality
The result from the present study is consistent with the finding from the previous research that depressive symptoms are risk factors for sleep quality (e.g., Roberts and Duong 2013; Bao et al. 2017). We found that rumination mediated the relationship between depressive symptoms and sleep quality, supporting our first hypothesis. That is, depressive symptoms increase rumination, which in turn undermines sleep quality. This finding is in line with prior research revealing rumination mediated the relationships between risk factors and sleep quality (Amaral et al. 2018; Slavish and Graham-Engeland 2015). Rumination was considered as the consequence of early experiences of depressive symptoms (Nolen-Hoeksema 2004; Nolen-Hoeksema et al. 2007). During adolescence, those who are temperamentally prone to distress or experienced depression in childhood are more inclined to develop a ruminative response style. This response style is a key feature of the CAS activated in response to negative thoughts, beliefs, emotions, and symptoms (Nolen-Hoeksema 2004; Wells 2009). As adolescents grow older, rumination may become a habituated response style when facing distress or depression. Thus, how college students cope with depression during childhood and adolescence may explain the result that their depressive symptoms were positively related to rumination. In addition, depressive individuals who have a deficit in mood regulation skills may pay too much attention on distress and feel helpless to cope (Fabes et al. 1994). As a result, they often use the negative thoughts (e.g., rumination) activated by their depressed mood to interpret their current circumstances (Nolen-Hoeksema et al. 2010). For example, they would ask questions such as “Why this happens? Why I am sad?”. In the meanwhile, depressed people may also attempt to suppress their negative thoughts, which could result in rebounding of these thoughts, further increasing rumination (Wenzlaff et al. 1988).
Two theories may be used to explain the positive relationship between rumination and sleep quality. One is the Perseverative cognition hypothesis (Brosschot et al. 2006). According to the theory, by altering the immune system and neuroendocrine, or adopting maladaptive behaviors (e.g., substance abuse), rumination can induce a sustained psycho-physiological arousal which can further lead to short-term and long-term disturbances during sleep. The other is the response styles theory (Nolen-Hoeksema 1991), which says that when individuals are consistently engaged in rumination about symptoms, its possible causes, and consequences, without making any active changes, distress can be prolonged and heightened. This heightened distress can further lead to hyperarousal, increasing difficulty to fall asleep (Brosschot et al. 2006; Guastella and Moulds 2007).
The Moderating Role of Self-Compassion
The present study also found that the effect of depressive symptoms on sleep quality via rumination can be moderated by self-compassion. Specifically, the mediating effect of rumination was weaker for those with higher self-compassion. The finding supports our second hypothesis and is consistent with some prior studies suggesting self-compassion might be an important preventive factor against depression (Odou and Brinker 2015; Wadsworth et al. 2018).
The moderating role of self-compassion is mainly related to its psychological function. As an important human strength, self-compassion can foster kindness, equanimity, and feeling of inter-connectedness, hope and meaning when people are encountered with life’s stressful events (Neff et al. 2007b). Individuals high in self-compassion can gain a better understanding of his or her problems, weaknesses, and shortcomings, and experience more awareness and acceptance of difficult emotions (Leary et al. 2007). Presumably, a person with more self-compassion can respond to negative feelings with kindness and acknowledge that the experiences of imperfection and difficulties are part of human life (Krieger et al. 2015). At the same time, self-compassion allows one to take a balanced attitude towards his or her negative experiences, decreasing the chance of ruminate or suppress their negative thoughts and emotions (Neff et al. 2007a).
As a result, self-compassion has been used as an emotional regulation strategy (Neff 2003b) to transform negative feelings and thoughts into self-acceptance, thereby decreasing depression and enhancing positive outcomes such as life satisfaction and positive affect (Zessin et al. 2015). For example, Neff et al. (2005) found that students who were higher in self-compassion tend to cope with their negative feelings using adaptive emotion regulation strategies such as acceptance and positive reinterpretation. A meta-analysis by Zessin et al. (2015) also showed that self-compassion was positively related to emotional intelligence, suggesting self-compassion is a perceptive way to cope with difficult emotions. Thus, holding self-compassion in negative emotions is an adaptive way of dealing with difficulties in life, as it buffers individuals against the consequent negative emotions such as depressive symptoms.
Implications and Limitations
The present study shed light on how and when depressive symptoms influence sleep quality. The findings from the study have important practical implications for therapists and practitioners. First, given the mediating role of rumination, using strategies that can decrease rumination can be effective ways to improve sleep quality. For example, a metacognitive therapy (e.g., attentional training technique, detached mindfulness) developed by Wells (2009) seems promising. Wells (2009) demonstrated that the therapy mitigated the negative effects of the CAS and reduce depressive symptoms. This therapy could be used by practitioners to help depressed clients with a ruminative thinking style. Second, self-compassion would also be an attractive target for therapeutic interventions for students suffering from depressive symptoms, given the moderating role of self-compassion played in the pathway between rumination and depressive symptoms. Several intervention studies have shown that interventions focusing on self-compassion are effective in reducing negative outcomes such as depression and rumination (Finlay-Jones et al. 2017; Neff and Germer 2013; Smeets et al. 2014). For instance, Smeets et al. (2014) found that participants attending a 3-week self-compassion program designed for female college students increased their self-compassion, mindfulness, optimism, self-efficacy, and decreased their rumination and worry.
A few limitations of the study are worth mentioning. First, this study used a cross-sectional design, so that causation can not be made. Future research may valididate the results of this study through experimental studies and/or longitudinal studies. Second, only self-report data are used which may be contaminated by social desirability. To solve the problem, future research may collect data from multiple informants (e.g., parents and peers) and using multiple methods (e.g., randomized controlled trials). Third, the current study used convenience sampling, limiting to Chinese university population. Thus, caution should be taken when generalizing these findings to other populations. Future research should also consider a broader range of groups to increase its external validity. Finally, we tested self-compassion as a global construct. Many researchers (e.g., Brenner et al. 2017; Nerini et al. 2019) argued that self-compassion has two distinictive components: positive and negative components (i.e., self-coldness), and they may have differential impacts on mental health. For example, Brenner et al. (2018) found that self-compassion had a stronger association with well-being, whereas self-coldness had a stronger association with distress. Thus, the results of the present study might be inflated by the self-coldness subscale, and future research is warranted to explore the two components of self-compassion in the moderated mediation model separately.
References
Amaral, A. P., Soares, M. J., Pinto, A. M., Pereira, A. T., Madeira, N., Bos, S. C., Marques, M., Roque, C., & Macedo, A. (2018). Sleep difficulties in college students: The role of stress, affect and cognitive processes. Psychiatry Research, 260, 331–337. https://doi.org/10.1016/j.psychres.2017.11.072.
Bao, Y. P., Han, Y., Ma, J., Wang, R. J., Shi, L., Wang, T. Y., He, J., Yue, J. L., Shi, J., Tang, X. D., & Lu, L. (2017). Cooccurrence and bidirectional prediction of sleep disturbances and depression in older adults: Meta-analysis and systematic review. Neuroscience & Biobehavioral Reviews, 75, 257–273. https://doi.org/10.1016/j.neubiorev.2017.01.032.
Beck, A. T., Ward, C. H., Mendelson, M., Mock, J., & Erbaugh, J. K. (1961). An inventory for measuring depression. Archives of General Psychiatry, 4(6), 561–571. https://doi.org/10.1001/archpsyc.1961.01710120031004.
Beshai, S., Prentice, J. L., & Huang, V. (2018). Building blocks of emotional flexibility: Trait mindfulness and self-compassion are associated with positive and negative mood shifts. Mindfulness, 9(3), 939–948. https://doi.org/10.1007/s12671-017-0833-8.
Brenner, R. E., Heath, P. J., Vogel, D. L., & Credé, M. (2017). Two is more valid than one: Examining the factor structure of the self-compassion scale (SCS). Journal of Counseling Psychology, 64(6), 696–707. https://doi.org/10.1037/cou0000211.
Brenner, R. E., Vogel, D. L., Lannin, D. G., Engel, K. E., Seidman, A. J., & Heath, P. J. (2018). Do self-compassion and self-coldness distinctly relate to distress and well-being? A theoretical model of self-relating. Journal of Counseling Psychology, 65(3), 346–357. https://doi.org/10.1037/cou0000257.
Brosschot, J. F., Gerin, W., & Thayer, J. F. (2006). The perseverative cognition hypothesis: A review of worry, prolonged stress-related physiological activation, and health. Journal of Psychosomatic Research, 60(2), 113–124. https://doi.org/10.1016/j.jpsychores.2005.06.074.
Brown, F. C., Buboltz Jr., W. C., & Soper, B. (2002). Relationship of sleep hygiene awareness, sleep hygiene practices, and sleep quality in university students. Behavioral Medicine, 28(1), 33–38. https://doi.org/10.1080/08964280209596396.
Butz, S., & Stahlberg, D. (2018). Can self-compassion improve sleep quality via reduced rumination? Self and Identity, 17(6), 666–686. https://doi.org/10.1080/15298868.2018.1456482.
Buysse, D. J., Rd, R. C., Monk, T. H., Berman, S. R., & Kupfer, D. J. (1989). The Pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Research, 28(2), 193–213. https://doi.org/10.1016/0165-1781(89)90047-4.
Carney, C. E., Edinger, J. D., Meyer, B., Lindman, L., & Istre, T. (2006). Daily activities and sleep quality in college students. Chronobiology International, 23(3), 623–637. https://doi.org/10.1080/07420520600650695.
Chen, J., Yan, L. s., & Zhou, L. h. (2011). Reliability and validity of Chinese version of self-compassion scale. Chinese Journal of Clinical Psychology, 19(6), 734–736.
Chu, X. W., Fan, C. Y., Liu, Q. Q., & Zhou, Z. K. (2018). Cyberbullying victimization and symptoms of depression and anxiety among Chinese adolescents: Examining hopelessness as a mediator and self-compassion as a moderator. Computers in Human Behavior, 86, 377–386. https://doi.org/10.1016/j.chb.2018.04.039.
Diedrich, A., Grant, M., Hofmann, S. G., Hiller, W., & Berking, M. (2014). Self-compassion as an emotion regulation strategy in major depressive disorder. Behaviour Research and Therapy, 58, 43–51. https://doi.org/10.1016/j.brat.2014.05.006.
Fabes, R. A., Eisenberg, N., Karbon, M., Troyer, D., & Switzer, G. (1994). The relations of children’s emotion regulation to their vicarious emotional responses and comforting behaviors. Child Development, 65(6), 1678–1693. https://doi.org/10.1111/j.1467-8624.1994.tb00842.x.
Finlay-Jones, A., Xie, Q., Huang, X., Ma, X., & Guo, X. (2017). A pilot study of the 8-week mindful self-compassion training program in a Chinese community sample. Mindfulness, 9(3), 993–1002. https://doi.org/10.1007/s12671-017-0838-3.
Fresnics, A., & Borders, A. (2017). Angry rumination mediates the unique associations between self-compassion and anger and aggression. Mindfulness, 8(3), 554–564. https://doi.org/10.1007/s12671-016-0629-2.
Gilbert, P. (2005). Compassion: Conceptualisations, research and use in psychotherapy. London: Routledge.
Guastella, A. J., & Moulds, M. L. (2007). The impact of rumination on sleep quality following a stressful life event. Personality and Individual Differences, 42(6), 1151–1162. https://doi.org/10.1007/s12671-016-0629-2.
Hayes, A. F. (2013). Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. New York: The Guilford Press.
Hinz, A., Glaesmer, H., Brähler, E., Löffler, M., Engel, C., Enzenbach, C., Hegerl, U., & Sander, C. (2017). Sleep quality in the general population: Psychometric properties of the Pittsburgh sleep quality index, derived from a German community sample of 9284 people. Sleep Medicine, 30, 57–63. https://doi.org/10.1016/j.sleep.2016.03.008.
Holdaway, A. S., Luebbe, A. M., & Becker, S. P. (2018). Rumination in relation to suicide risk, ideation, and attempts: Exacerbation by poor sleep quality? Journal of Affective Disorders, 236, 6–13. https://doi.org/10.1016/j.jad.2018.04.087.
Jiang, X. L., Zheng, X. Y., Yang, J., Ye, C. P., Chen, Y. Y., Zhang, Z. G., & Xiao, Z. J. (2015). A systematic review of studies on the prevalence of insomnia in university students. Public Health, 129(12), 1579–1584. https://doi.org/10.1016/j.puhe.2015.07.030.
Johnson, E. A., & O'Brien, K. A. (2013). Self-compassion soothes the savage ego-threat system: Effects on negative affect, shame, rumination, and depressive symptoms. Journal of Social & Clinical Psychology, 32(9), 939–963. https://doi.org/10.1521/jscp.2013.32.9.939.
Karl, A., Williams, M. J., Cardy, J., Kuyken, W., & Crane, C. (2018). Dispositional self-compassion and responses to mood challenge in people at risk for depressive relapse/recurrence. Clinical Psychology & Psychotherapy, 25, 621–633.
Katz, D. A., & McHorney, C. A. (1998). Clinical correlates of insomnia in patients with chronic illness. Archives of Internal Medicine, 158(10), 1099–1107. https://doi.org/10.1001/archinte.158.10.1099.
Krause, E. D., Vélez, C. E., Woo, R., Hoffmann, B., Freres, D. R., Abenavoli, R. M., & Gillham, J. E. (2018). Rumination, depression, and gender in early adolescence: A longitudinal study of a bidirectional model. The Journal of Early Adolescence, 38(7), 923–946. https://doi.org/10.1177/0272431617704956.
Krieger, T., Altenstein, D., Baettig, I., Doerig, N., & Holtforth, M. G. (2013). Self-compassion in depression: Associations with depressive symptoms, rumination, and avoidance in depressed outpatients. Behavior Therapy, 44(3), 501–513. https://doi.org/10.1016/j.beth.2013.04.004.
Krieger, T., Hermann, H., Zimmermann, J., & Holtforth, M. G. (2015). Associations of self-compassion and global self-esteem with positive and negative affect and stress reactivity in daily life: Findings from a smart phone study. Personality and Individual Differences, 87, 288–292. https://doi.org/10.1016/j.paid.2015.08.009.
Leary, M. R., Tate, E. B., Adams, C. E., Batts Allen, A., & Hancock, J. (2007). Self-compassion and reactions to unpleasant self-relevant events: The implications of treating oneself kindly. Journal of Personality and Social Psychology, 92(5), 887–904. https://doi.org/10.1037/0022-3514.92.5.887.
Li, H., Fu, R., Zou, Y., & Cui, Y. (2017). Predictive roles of three-dimensional psychological pain, psychache, and depression in suicidal ideation among Chinese college students. Frontiers in Psychology, 8, 1550. https://doi.org/10.3389/fpsyg.2017.01550.
Li, L., Wang, Y. Y., Wang, S. B., Zhang, L., Li, L., Xu, D. D., Ng, C. H., Ungvari, G. S., Cui, X. L., Liu, Z. M., Li, S. D., Jia, F. J., & Xiang, Y. T. (2018). Prevalence of sleep disturbances in Chinese university students: A comprehensive meta-analysis. Journal of Sleep Research, 27(3), e12648. https://doi.org/10.1111/jsr.12648.
Liu, X. C., Tang, M. Q., Hu, L., Wang, A. L., Wu, X. G., Zhao, G. F., et al. (1996). The study on the reliability and validity of Pittsburgh sleep quality index. Chinese Journal of Psychiatry, 29, 103–107.
Liu, Q. Q., Zhou, Z. K., Yang, X. J., Kong, F. C., Sun, X. J., & Fan, C. Y. (2018). Mindfulness and sleep quality in adolescents: Analysis of rumination as a mediator and self-control as a moderator. Personality and Individual Differences, 122, 171–176. https://doi.org/10.1016/j.paid.2017.10.031.
Neff, K. D. (2003a). The development and validation of a scale to measure self-compassion. Self and Identity, 2(3), 223–250. https://doi.org/10.1080/15298860309027.
Neff, K. (2003b). Self-compassion: An alternative conceptualization of a healthy attitude toward oneself. Self and Identity, 2(2), 85–101. https://doi.org/10.1080/15298860309032.
Neff, K. D., & Germer, C. K. (2013). A pilot study and randomized controlled trial of the mindful self-compassion program. Journal of Clinical Psychology, 69(1), 28–44. https://doi.org/10.1002/jclp.21923.
Neff, K. D., Hsieh, Y.-P., & Dejitterat, K. (2005). Self-compassion, achievement goals, and coping with academic failure. Self and Identity, 4(3), 263–287. https://doi.org/10.1080/13576500444000317.
Neff, K. D., Kirkpatrick, K. L., & Rude, S. S. (2007a). Self-compassion and adaptive psychological functioning. Journal of Research in Personality, 41(1), 139–154. https://doi.org/10.1016/j.jrp.2006.03.004.
Neff, K. D., Rude, S. S., & Kirkpatrick, K. L. (2007b). An examination of self-compassion in relation to positive psychological functioning and personality traits. Journal of Research in Personality, 41(4), 908–916. https://doi.org/10.1016/j.jrp.2006.08.002.
Nerini, A., Matera, C., Di Gesto, C., Policardo, G. R., & Stefanile, C. (2019). Exploring the links between self-compassion, body dissatisfaction, and acceptance of cosmetic surgery in young Italian women. Frontiers in Psychology, 10. https://doi.org/10.3389/fpsyg.2019.02698.
Nolen-Hoeksema, S. (1991). Responses to depression and their effects on the duration of depressive episodes. Journal of Abnormal Psychology, 100(4), 569–582. https://doi.org/10.1037/0021-843X.100.4.569.
Nolen-Hoeksema, S. (2004). The response styles theory. In C. Papageorgiou & A. Wells (Eds.), Depressive rumination: Nature, theory, and treatment of negative thinking in depression (pp. 107–123). Chichester: Wiley.
Nolen-Hoeksema, S., Stice, E., Wade, E., & Bohon, C. (2007). Reciprocal relations between rumination and bulimic, substance abuse, and depressive symptoms in female adolescents. Journal of Abnormal Psychology, 116(1), 198–207. https://doi.org/10.1037/0021-843X.116.1.198.
Nolen-Hoeksema, S., Wisco, B. E., & Lyubomirsky, S. (2010). Rethinking rumination. Perspectives on Psychological Science, 3(5), 400–424. https://doi.org/10.1111/j.1745-6924.2008.00088.x.
Odou, N., & Brinker, J. (2014). Exploring the relationship between rumination, self-compassion, and mood. Self and Identity, 13(4), 449–459. https://doi.org/10.1080/15298868.2013.840332.
Odou, N., & Brinker, J. (2015). Self-compassion, a better alternative to rumination than distraction as a response to negative mood. The Journal of Positive Psychology, 10(5), 447–457. https://doi.org/10.1080/17439760.2014.967800.
Opp, M. R. (2009). Sleeping to fuel the immune system: Mammalian sleep and resistance to parasites. BMC Evolutionary Biology, 9(1), 8. https://doi.org/10.1186/1471-2148-9-8.
Pillai, V., Steenburg, L. A., Ciesla, J. A., Roth, T., & Drake, C. L. (2014). A seven day actigraphy-based study of rumination and sleep disturbance among young adults with depressive symptoms. Journal of Psychosomatic Research, 77(1), 70–75. https://doi.org/10.1016/j.jpsychores.2014.05.004.
Piro, R. S., Alhakem, S. S. M., Azzez, S. S., & Abdulah, D. M. (2018). Prevalence of sleep disorders and their impact on academic performance in medical students/University of Duhok. Sleep and Biological Rhythms, 16(1), 1–8. https://doi.org/10.1007/s41105-017-0134-6.
Podsakoff, P. M., Mackenzie, S. B., & Podsakoff, N. P. (2012). Sources of method bias in social science research and recommendations on how to control it. Annual Review of Psychology, 63, 539–569. https://doi.org/10.1146/annurev-psych-120710-100452.
Raes, F. (2010). Rumination and worry as mediators of the relationship between self-compassion and depression and anxiety. Personality and Individual Differences, 48(6), 757–761. https://doi.org/10.1016/j.paid.2010.01.023.
Raes, F. (2011). The effect of self-compassion on the development of depression symptoms in a non-clinical sample. Mindfulness, 2(1), 33–36. https://doi.org/10.1007/s12671-011-0040-y.
Ramel, W., Goldin, P. R., Carmona, P. E., & Mcquaid, J. R. (2004). The effects of mindfulness meditation on cognitive processes and affect in patients with past depression. Cognitive Therapy and Research, 28(4), 433–455. https://doi.org/10.1023/B:COTR.0000045557.15923.96.
Riemann, D., Berger, M., & Voderholzer, U. (2001). Sleep and depression—Results from psychobiological studies: An overview. Biological Psychology, 57(1–3), 67–103. https://doi.org/10.1016/s0301-0511(01)00090-4, 103.
Roberts, R., & Duong, H. T. (2013). Depression and insomnia among adolescents: A prospective perspective. Journal of Affective Disorders, 148(1), 66–71. https://doi.org/10.1016/j.jad.2012.11.049.
Schlarb, A. A., Claßen, M., Hellmann, S. M., Vögele, C., & Gulewitsch, M. D. (2017). Sleep and somatic complaints in university students. Journal of Pain Research, 10, 1189–1199. https://doi.org/10.2147/JPR.S125421.
Slavish, D. C., & Graham-Engeland, J. E. (2015). Rumination mediates the relationships between depressed mood and both sleep quality and self-reported health in young adults. Journal of Behavioral Medicine, 38(2), 204–213. https://doi.org/10.1007/s10865-014-9595-0.
Smeets, E., Neff, K., Alberts, H., & Peters, M. (2014). Meeting suffering with kindness: Effects of a brief self-compassion intervention for female college students. Journal of Clinical Psychology, 70(9), 794–807. https://doi.org/10.1002/jclp.22076.
Stoia-Caraballo, R., Rye, M. S., Pan, W., Kirschman, K. J. B., Lutz-Zois, C., & Lyons, A. M. (2008). Negative affect and anger rumination as mediators between forgiveness and sleep quality. Journal of Behavioral Medicine, 31(6), 478–488. https://doi.org/10.1007/s10865-008-9172-5.
Takano, K., & Tanno, Y. (2009). Self-rumination, self-reflection, and depression: Self-rumination counteracts the adaptive effect of self-reflection. Behaviour Research and Therapy, 47(3), 260–264. https://doi.org/10.1016/j.brat.2008.12.008.
Takano, K., Iijima, Y., & Tanno, Y. (2012). Repetitive thought and self-reported sleep disturbance. Behavior Therapy, 43(4), 779–789. https://doi.org/10.1016/j.beth.2012.04.002.
Tempesta, D., De, G. L., Natale, V., & Ferrara, M. (2015). Emotional memory processing is influenced by sleep quality. Sleep Medicine, 16(7), 862–870. https://doi.org/10.1016/j.sleep.2015.01.024.
Wadsworth, L. P., Forgeard, M., Hsu, K. J., Kertz, S., Treadway, M., & Björgvinsson, T. (2018). Examining the role of repetitive negative thinking in relations between positive and negative aspects of self-compassion and symptom improvement during intensive treatment. Cognitive Therapy and Research, 42(3), 236–249. https://doi.org/10.1007/s10608-017-9887-0.
Wells, A. (2009). Metacognitive therapy for anxiety and depression. Washington, DC: The Guilford Press.
Wenzlaff, R. M., Wegner, D. M., & Roper, D. W. (1988). Depression and mental control: The resurgence of unwanted negative thoughts. Journal of Personality and Social Psychology, 55(6), 882–892. https://doi.org/10.1037/0022-3514.55.6.882.
Winzeler, K., Voellmin, A., Schäfer, V., Meyer, A. H., Cajochen, C., Wilhelm, F. H., & Bader, K. (2014). Daily stress, presleep arousal, and sleep in healthy young women: A daily life computerized sleep diary and actigraphy study. Sleep Medicine, 15(3), 359–366. https://doi.org/10.1016/j.sleep.2013.09.027.
Yang, J., Ling, Y., Xiao, J., & Yao, S. Q. (2009). The Chinese version of ruminative responses scale in high school students: Its reliability and validity. Chinese Journal of Clinical Psychology, 17(1), 27–28.
Yarnell, L. M., & Neff, K. D. (2013). Self-compassion, interpersonal conflict resolutions, and well-being. Self and Identity, 12(2), 146–159. https://doi.org/10.1080/15298868.2011.649545.
Zawadzki, M. J., Graham, J. E., & Gerin, W. (2013). Rumination and anxiety mediate the effect of loneliness on depressed mood and sleep quality in college students. Health Psychology, 32(2), 212–222. https://doi.org/10.1037/a0029007.
Zessin, U., Dickhäuser, O., & Garbade, S. (2015). The relationship between self-compassion and well-being: A meta-analysis. Applied Psychology. Health and Well-Being, 7(3), 340–364. https://doi.org/10.1111/aphw.12051.
Zhang, H. S., Li, Y., Mo, H. Y., Qiu, D. X., Zhao, J., Luo, J. L., Lin, W. Q., Wang, J. J., & Wang, P. X. (2017). A community-based cross-sectional study of sleep quality in middle-aged and older adults. Quality of Life Research, 26(3), 923–933. https://doi.org/10.1007/s11136-016-1408-1.
Zoccola, P. M., Dickerson, S. S., & Lam, S. (2009). Rumination predicts longer sleep onset latency after an acute psychosocial stressor. Psychosomatic Medicine, 71(7), 771–775. https://doi.org/10.1097/PSY.0b013e3181ae58e8.
Funding
The Key Specialist Projects of Shanghai Municipal Commission of Health and Family Planning (ZK2015B01).
The Programs Foundation of Shanghai Municipal Commission of Health and Family Planning (201540114).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Ethics Approval
The Ethics Committee of Psychological Research at East China Normal University, Shanghai, China.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bian, XH., Hou, XL., Zuo, ZH. et al. Depression and sleep quality among Chinese college students: The roles of rumination and self-compassion. Curr Psychol 41, 4242–4251 (2022). https://doi.org/10.1007/s12144-020-00946-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12144-020-00946-3