Abstract
Two studies were designed to examine the role of self-compassion on sleep quality. One hundred and forty-two participants completed a one-time survey in which they reported their trait level self-compassion, sleep quality assessment and perceived stress over last month. Mediation analysis using regression and bootstrapping indicated that self-compassion was positively related to sleep quality assessment, and this relationship was mediated by perceived stress. Higher levels of self-compassion were associated with lower levels of perceived stress, and the latter were linked to better sleep. A 2-week diary study with a subsample of fifty-nine participants was followed to examine the effect of self-compassion on sleep outcomes within and between individual on a daily basis. Participants rated their stressor of the day before bed and sleep quality upon awakening. Multilevel models supported the positive effect of self-compassion on everyday sleep outcomes. Specifically, self-compassion buffered the negative effect of daily stressor on sleep latency. Experiencing stressful events during the day were associated with taking a longer time to fall asleep at night, except for participants with higher levels of self-compassion. Higher levels of self-compassion were also indirectly associated with a better mood and more alertness upon awakening. Self-compassion could benefit sleep quality both through the buffering effect and the indirect effect.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sleep is a vital physiological process for the overall health of human beings. Poor sleep quality is highly correlated with various diseases, medical costs, accident proneness, as well as indirect costs related to work absenteeism (Luyster set al. 2012). Research has demonstrated that poor sleep quality can be caused by psychosocial stress, such as negative life events, occupational stress, prenatal maternal stress, and posttraumatic stress (Jackowska et al. 2011; Steptoe et al. 2003, 2008). Self-compassion has recently been found to have a positive effect on coping with stress (Allen and Leary 2010; Arch et al. 2014). Therefore, investigating the benefits of self-compassion on stress-related poor sleep quality is worthwhile.
Self-compassion has been defined by Neff (2003b) as treating oneself with warmth and non-judgmental understanding when confronting suffering, failure, or inadequacy. According to Neff’s definition, self-compassion has three main components: self-kindness versus self-judgment, common humanity versus isolation, and mindfulness versus over-identification. A self-compassionate person would acknowledge negative feelings when making mistakes or facing frustration, and recognize that others may suffer from or experience the same situations. Therefore, some researchers have claimed that self-compassion could act as a valuable coping mechanism (Allen and Leary 2010). Researchers have found that when confronting unpleasant events or negative cognitions, self-compassion could serve as a moderator that buffers against negative self-feelings and depression (Brion et al. 2014; Leary et al. 2007; Wong and Mak 2013). Individuals with higher levels of self-compassion also exhibited lower interleukin-6 response when exposed to a standardized laboratory stressor (Breines et al. 2014). Beyond the buffering effect of self-compassion when facing specific stressors, researchers have also found self-compassion could help to decrease the overall perceived stress level (Bluth et al. 2016; Neff and Germer 2013; Sirois et al. 2015b). Sirois et al. (2015) found that self-compassion negatively correlated with perceived stress level in chronic illness samples, although this correlation could be mediated by coping styles. Furthermore, intervention studies have shown that trainings in self-compassion could decrease perceived stress levels in both adult and adolescent samples (Bluth et al. 2016; Neff and Germer 2013). Although, to our knowledge, there has not been a study directly examining the mediating role of perceived stress between self-compassion and well-being, it is proposed that self-compassion could positively influence well-being by decreasing the perceived stress level.
Self-compassion has been demonstrated to be associated with different aspects of psychological well-being, such as positive affect, life satisfaction, and adaptive functioning (Allen and Leary 2010; Neff et al. 2007, 2008). Recently, the potential positive effect of self-compassion on physical health has become increasingly popular within the literature (Hall et al. 2013). Self-compassion has been found to be associated with health-promoting behaviors (Sirois 2015; Sirois et al. 2015a; Terry et al. 2013). For people with chronic diseases, having more self-compassion could alleviate the emotional impact of these illnesses and promote a more active lifestyle (Brion et al. 2014). Training in self-compassion can also reduce daily smoking, especially for smokers with low motivation (Kelly et al. 2010).
Sleep is one of the main indicators for health. The research on self-compassion has expanded from psychological well-being to physical health, but the role of self-compassion on sleep has not yet been well studied. There have been only a few correlational studies that examined the relationship between self-compassion and sleep as of now (Kemper et al. 2015; Marques et al. 2016; Teixeira et al. 2016). These studies found that sleep was correlated with self-compassion in various samples. However, these studies are all correlational design, and the correlation between self-compassion and sleep is much smaller than the correlation between stress and sleep (Kemper et al. 2015), other mechanisms beyond correlation should be studied.
Although there is very limited literature on the relationship between self-compassion and sleep, accumulating evidence has suggested that mindfulness has benefits for improving sleep quality. Dispositional mindfulness is correlated with sleep quality in various samples (e.g., Garland et al. 2013; Howell, Digdon and Buro 2010; Howell et al. 2008). Intervention studies using Mindfulness-Based Stress Reduction or other therapies that incorporated mindfulness components found evidence of improving sleep quality (Carlson and Garland 2005; Hubbling et al. 2014; Ong et al. 2012). While mindfulness is one component in the overall concept of self-compassion, it is likely that self-compassion alone could contribute to improving sleep quality as well. Additional studies are needed to examine the highly possible effect of self-compassion on sleep and its functioning mechanism and therefore provide information for future interventions for sleep problems.
The present study examines the relationship between self-compassion and sleep. We also aim to separate the everyday stressor and the one-time measure general perceived stress by a survey study and a diary study. In the survey study, the correlational association among self-compassion, perceived stress, and sleep quality would be examined. Within the diary study, the effect of self-compassion and general perceived stress on the relationship between daily stressor and daily sleep outcomes would be examined. Based on previous studies, we established our hypotheses: (H1) self-compassion has an indirect effect on sleep. Self-compassion reduces perceived stress level, and the later improves sleep quality. (H2a) Self-compassion has a moderating effect on sleep by buffering the negative effects of the daily stressor, and (H2b) the moderating effect of self-compassion on sleep may be mediated by perceived stress. These hypotheses are illustrated in our conceptual model Fig. 1.
Study 1
Method
Participants
A total of 142 college students participated in this study. Among them, 62 were males, 78 were females, and 2 participants did not report their gender. The age ranged from 18 to 32, with a mean of 20.07 and a standard deviation of 2.36. There was also one missing value in age.
Procedure
Participants were recruited via the Human Participants Pool in the Department of Psychology and in-class announcements. The first round of data collection recruited 83 participants. They completed a one-time survey and received one course credit for their participation. The second round of data collection recruited 59 participants. Besides the one-time survey, they also completed a 14-day sleep diary and received two course credits. The survey data of 142 participants were used in study 1.
Measures
Self-Compassion
Neff (2003a) developed a self-report measurement to assess trait levels of self-compassion—the Self-Compassion Scale, which has been the most widely used measurement in assessing self-compassion. The short form of SCS was developed by Raes et al. (2011), which has been found to have the same level of reliability and factorial structure as the original scale. In this study, the short form of the self-compassion scale was used to assess the participants’ self-compassion (SC; Raes et al. 2011). The short form scale contains 12 items. Participants were asked to indicate how often they behave in the stated way on a five-point Likert scale ranging from one (almost never) to five (almost always). For example, one of these statements was, “I try to see my failings as part of the human condition.” Items 1, 4, 8, 9, 11, and 12 were reverse coded. The Cronbach’s alpha for the entire sample was found to be 0.756. Higher scores indicate high levels of self-compassion.
Perceived Stress
The Perceived Stress Scale (PSS; Cohen et al. 1983) was used to measure the level of stress that participants perceived. The scale includes 10 items. Participants were asked to indicate how often they felt or thought a certain way during the last month on a five-point scale from zero (never) to five (very often). An example of the questions asked is, “in the last month, how often have you been upset because of something that happened unexpectedly?” Items 4, 5, 7, and 8 were reverse coded. The Cronbach’s alpha for the entire sample was found to be 0.770. Higher scores indicate high levels of perceived stress.
Sleep Quality
The Pittsburgh Sleep Quality Index (PSQI; Buysse et al. 1989) was used to assess sleep quality over a 1-month interval. The questionnaire includes 19 self-reported items and creating 7 components including subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleeping medication, and daytime dysfunction. The seven components produce a total score, as an effective measure of overall sleep quality. The first reported Cronbach’s alpha for this questionnaire is 0.83, and the alpha for this sample is 0.72. Higher scores in PSQI indicate a poorer overall sleep quality.
Data Analyses
The correlations among SC, PSS, and PSQI were evaluated, and then multiple regressions were used to examine the mediating hypothesis (H1). Specifically, three regression models were examined (Baron and Kenny 1986). First, PSQI was regressed on SC, then PSS was regressed on SC, and finally, PSQI was regressed on both SC and PSS. A significant effect of SC on PSQI and PSS, as well as a significant effect of PSS on PSQI would be essential to support the mediating hypothesis. Moreover, a bootstrapping method recommended by Preacher and Hayes (2008) was also used to confirm the proposed mediating effect. The correlation, regression, and bootstrapping mediation analysis were all conducted using SPSS 24.0.
Results
Descriptive statistics for PSQI, PSS, and SC were as followed. The mean of PSQI is 6.67, with a standard deviation of 2.68 and a range from 0 to 13. A PSQI global score of five or greater indicates a “poor” sleeper. The current sample covers a wide range of participants from good sleepers to poor sleeper. The mean of PSS is 18.33, with a standard deviation of 5.87 and a range from 5 to 34. The mean of SC is 3.2, SD = 0.62, ranged from 1.67 to 4.67. Correlation analysis among PSQI, PSS, and SC indicated that PSQI positively correlated with perceived stress, r = .34, p < .001, and negatively correlated with self-compassion, r = −.23, p < .01. Perceived stress also negatively correlated with self-compassion, r = −.59, p < .001.
Regression analysis was used to investigate the hypothesis that PSS mediates the effect of SC on PSQI. Gender and age were controlled. Table 1 shows the results of regression analysis. The main effect of SC on PSQI was significant, b = − 0.079, 95% CI = [− 0.139, − 0.019], β= − .218, p = .010. The main effect of PSS on PSQI was also significant, b = 0.146, 95% CI = [0.070, 0.222], β = 0.321, p < .001. The main effect of SC on PSS was significant as well, b = − 0.450, 95% CI = [− 0.556, − 0.344], β = − .567, p < .001. When both SC and PSS were used to predict PSQI, the effect of SC became not significant, b = − 0.019, 95% CI = [− 0.092, 0.053], β= − .054, p = .596. This result suggested that PSS mediated the effect of SC on PSQI, supporting H1. We also tested the interaction effect between SC and PSS, b = − 0.201, 95% CI = [− 0.638, 0.237], β = − 0.074, p = .366, indicating that the final model should not include the interaction effect. According to the main effect only model, approximately 12.2% of the variance in PSQI was accounted for by the predictors, R2 = 0.122.
The indirect effect of SC on PSQI was also tested with 5000 bootstrap resamples (Preacher and Hayes 2008). The indirect effect was significant, b = 0.0671, SE = 0.0226, p < .01, 95% bootstrap confidence intervals are [− 0.1143, −0.0264]. The association between self-compassion and PSQI was significantly mediated by perceived stress.
Discussion
This study examined the relationship among self-compassion, perceived stress, and sleep quality through a survey study. The results supported our hypothesis that self-compassion could affect sleep quality through perceived stress. A lower level of SC was related to a higher level of PSS and therefore was associated with higher PSQI score which indicated worse sleep. However, the moderation role of self-compassion was not supported in the survey study.
Study 2
Method
Participants
As mentioned previously, 59 participants among the 142 participants were also asked to complete a 14-day sleep diary. In this diary study sample, 18 were males, 40 were females, and one did not provide their gender. The age ranged from 18 to 29, with one missing value, an average of 19.5 and a standard deviation of 1.93. Among the 59 diary study participants, 25 have no missing value on all variables during the 14 days, 23 have at least 6 days of complete data, and the other 11 have more missing values.
Procedure
After completing the self-compassion, perceived stress, and PSQI scales, the participants in the diary study also completed a 14-day sleep diary. The diary was identical for each day of the 14 days. Each day of the diary included the self-report on any stressful events as well as day activities such as exercise and caffeine consumption that may have occurred and self-reported sleep outcomes the following morning. In this study, daytime activities are not included in data analysis in order to focus on the stress-sleep relationship.
Measures
Daily Stressor
Participants were first asked whether they experienced a disruptive event that day, and if their answer is yes, they rated how stressful the event was on a one to five Likert scale. Therefore, the variable daily stressor is coded from zero to five, with zero indicating no stressor occurred, and one to five indicating the stressfulness of the event when it did occur.
Sleep Outcomes
The diary questions on sleep latency, sleep quality, mood, and alertness were used as the sleep outcomes. Every morning, participants reported how long it took them, in minutes, to get to sleep the night prior to filling out the questionnaire as sleep latency, and rated the overall sleep quality, their mood on final wakening, and alertness on final wakening on a one to five Likert scale.
Data Analyses
The diary data of the 59 participants on the daily stressor and sleep outcomes were merged with their data from the survey study. Self-reported sleep outcomes from diary entries (DV) were predicted by daily stressor (IV), as well as the one-time measures SC and PSS (moderator and mediator). Multilevel models were used on the multilevel data, where daily observations (level 1) were nested within persons (level 2). The interaction between the two levels was also examined. The model is specified as follows:
-
Level 1: Sleep = β0 + β1 × stressor + ε
-
Level 2:β0 = γ00 + γ01 × SC + γ02 × PSS
β1 = γ10 + γ11 × SC + γ12 × PSS
The model parameter γ10 stands for the fixed main effect of stressor, γ01 and γ02 stand for the fixed main effect of SC and PSS on sleep outcome. The parameter γ11 indicates the interaction effect between SC and stressor, and the parameter γ12 indicates the interaction effect between PSS with stressor. A significant γ11 or γ12 would support our second hypothesis. Specifically, a significant γ11 will support H2a, and a significant γ12 will support H2b. This multilevel model was implemented using the lmer function in the lme4 package (Bates et al. 2015) in R (R Core Team 2017).
Results
The multilevel model on stressor and sleep variables was conducted. Level 1 is within-subject, daily stressor was used to predict daily sleep outcomes. We also controlled the effect of weekends. We defined Friday night and Saturday night as weekend, and other nights as weekdays. Level 2 is between-subject, one-time measures SC and PSS were used to predict the intercept (main effect) and slope (interaction effect) of the level 1 model. The diary questions on sleep quality, sleep latency, mood, and alertness upon waking up were analyzed separately as sleep outcomes.
Sleep Quality and Sleep Latency
Multilevel models were conducted to examine the effect of the stressor, self-compassion, and perceived stress on sleep quality and sleep latency separately. As shown in Table 2, the interaction between PSS and the daily stressor is significant on sleep quality, supporting H2b, and indicating that perceived stress moderated the effect of the daily stressor on sleep quality. Given a certain amount of daily stressor, a higher overall perceived stress would result in poor sleep whereas a low level of perceived stress would not. Since weekends had no significant main or interaction effect on sleep quality, we did not include it as a predictor for sleep quality.
The interaction between SC and daily stressor is significant on sleep latency, supporting H2a, and indicating that self-compassion moderated the effect of stressor on sleep latency. A high self-compassion score can reduce the negative effect of stressor on sleep latency. Given a certain amount of daily stressor, persons with high self-compassion would not have sleep latency while persons with low self-compassion would have more sleep latency. There was also a significant three-way interaction between SC, daily stressor, and weekends, suggesting that the moderating effect of SC was stronger during weekends than during weekdays.
Figure 2 illustrated the moderating effect of perceived stress and self-compassion. As shown in the figure, a high perceived stress enhances the negative effect of the stressor on sleep quality, and a high self-compassion score reduces the effect of the stressor on sleep latency.
The moderating effect of perceived stress and self-compassion. Note: the lines in the left plot were created by the regression equation sleep quality = stressor + PSS + stressor × PSS with PSS replaced by its mean M, M-1SD, and M+1SD. The lines in the right plot were created by the regression equation sleep latency = stressor + SC + stressor × SC with SC replaced by its mean M, M-1SD, and M+1SD
Mood and Alertness upon Awakening
Four models were tested to examine the effect of stressor, self-compassion, and perceived stress on mood and alertness upon awakening separately. The variable weekends had no main or interaction effect; therefore, we did not include it in the result report. As shown in Table 3, daily stressor does not have a significant effect on these outcomes, but SC has an effect on them. When PSS was inputted into the model, the significant effect of SC disappeared, indicating that SC indirectly influenced mood and alertness via the mediator PSS, supporting H1. All the interaction effects are not significant. These results are consistent with our findings in study 1.
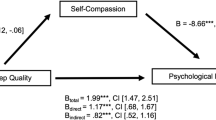
Figure 3 summarized the findings in two studies. In sum, self-compassion influences sleep in two ways: (1) help shorten sleep latency when facing a stressor, (2) reduce perceived stress and therefore reduce the negative effect of a stressor on sleep quality, and improve mood and alertness upon waking up.
Discussion
The diary study found that self-compassion works differently in regard to the different sleep outcomes. It may indirectly influence sleep by reducing perceived stress, and it may buffer the negative effect of a stressor on sleep.
For outcomes that are directly related to sleep, such as sleep quality and sleep latency, the moderation model (H2a and H2b) is supported. Self-compassion moderated the negative influences of a daily stressor on sleep outcomes, directly (moderation) or indirectly via perceived stress (mediated moderation). For people with high self-compassion, which is associated with low perceived stress, a daily stressor did not impact sleep latency or sleep quality; while for people with low self-compassion, which is also associated with high perceived stress, the stressor was linked with more sleep latency and low sleep quality.
For outcomes that are more related to emotion, such as mood and alertness upon waking up, the mediation model (H1) is supported. Self-compassion had an indirect effect through the mediator perceived stress. High self-compassion is associated with less perceived stress and therefore yielded better mood and more alertness. Any daily stressor did not have a significant effect on those emotion related sleep outcomes.
It is worth mentioning that for self-reported outcomes on subjective feelings, i.e., sleep quality, mood, and alertness upon waking up, self-compassion took effect mostly through the mediating role of perceived stress. Self-compassion helps reduce the perceived stress, and then a lower perceived stress level is associated with better mood and alertness in the morning, and improves stress-related poor sleep quality. By contrast, sleep latency, a relative objective behavior outcome, the moderating effect of self-compassion did not need to go through perceived stress.
General Discussion
This study strongly supported the protective role of self-compassion from stress-related poor sleep quality. Self-compassion directly buffered the effect of daily stressors on sleep latency and indirectly buffered the negative effect of stressors on sleep quality by reducing general perceived stress. This study enriches the literature by twofold. First, it begins to fill in the gap within the literature between self-compassion and sleep. Second, it examined the mechanism of self-compassion on sleep by using a daily diary study, and all possible roles of self-compassion were examined so that a comprehensive model can be developed.
The findings of this study are consistent with previous findings that self-compassion is associated with better sleep (Kemper et al. 2015; Marques et al. 2016; Teixeira et al. 2016), and extended it by finding that the observed positive effect actually was mediated by perceived stress, which clarified the functioning mechanism of the relationship between self-compassion and sleep quality.
The findings supported that self-compassion could play as a moderator and buffer the negative effect of daily stressor. This result reaffirms the multiple empirical and theoretical findings that self-compassion can serve as a coping mechanism and buffer many kinds of negative events on multiple psychological and physical well-being outcomes in general (Allen and Leary 2010; Brion et al. 2014; Leary et al. 2007), and more importantly, this study further expanded the literature by confirming self-compassion as a buffer specifically between stressor and sleep outcomes.
This study differentiated daily stressor from perceived stress and found self-compassion function differently toward them. A daily stressor is more of a measure on an individual’s actual experience. Therefore, self-compassion cannot change the stressor but instead help reduce its negative consequences. Perceived stress is more of a measure on a subjective perception, and self-compassion helps reduce it. There have been studies reporting that insomnia sufferers and healthy sleepers reported equivalent numbers of minor daily stressful life events, but insomnia sufferers rated the impact of the daily stressor higher than good sleepers (Morin et al. 2003). This indicates insomniacs may overanalyze negative life events. This is congruent with the cognitive-behavioral model of insomnia, which presents that emotional, cognitive, and physiologic hyperarousal were central mediating features of poor sleep (Morin 1993). Therefore, researchers have made effort to explore the effect of novel intervention in treating insomnia, such as mindfulness (Blake et al. 2016; Ong et al. 2012). Accumulating evidence has shown that mindfulness-based interventions can help improve sleep (Carlson and Garland 2005; Hubbling et al. 2014). The findings of this study, although not aimed to be an intervention study, suggest that interventions based on self-compassion may be another effective method of treatment. The buffering effect of self-compassion and its indirect effect through perceived stress may be the mechanism under self-compassion and sleep.
According to DSM-5 (American Psychiatric Association 2013), difficulty in falling asleep is a main indicator of insomnia, so the finding that self-compassion has direct effect on sleep latency is very valuable. Besides buffering the negative effect of daily stressor, self-compassion directly reduced sleep latency (see Table 2, the main effect of SC on sleep latency). This result suggested that intervention based on self-compassion may at least improve sleep latency directly, with or without confronting stressful events. However, individuals may overestimate sleep latency compared with objective assessment, and patients with insomnia tend to be especially poor at estimating sleep latency (Baker et al. 1999). Therefore, findings in this study still need to be validated with objective polysomnographic data.
Limitations and Future Directions
There are several limitations that limit the interpretation of the findings. First, all sleep outcomes were self-reported. As mentioned previously, subject reported sleep outcome is different from an objective assessment. Furthermore, individuals who are willing and able to track their sleep quality may be different from those who are not. Future studies can attempt to use objective assessment to record sleep outcomes. Second, this study is limited by a university student sample. The findings need to be examined in more general populations, especially in a community or working sample as well as from clinical samples. Third, the sample size is relatively small for a regression analysis and multilevel modeling. However, considering the daily dairy nature of the study, it is costly to follow participants for two full weeks. If possible, future studies can use a larger sample size to enhance the findings here. Last, this study only examined the stress-related poor sleep. The potential roles of self-compassion between other predictors and poor sleep were not examined in this study, such as pregnancy, shift work, large traumatic events, and others. In the future, more studies can be conducted with those samples and situations, and the information may help in designing targeted interventions.
References
Allen, A. B., & Leary, M. R. (2010). Self-compassion, stress, and coping. Social and Personality Psychology Compass, 4(2), 107–118.
American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders: DSM-5. Washington, D.C: American Psychiatric Association.
Arch, J. J., Brown, K. W., Dean, D. J., Landy, L. N., Brown, K. D., & Laudenslager, M. L. (2014). Self-compassion training modulates alpha-amylase, heart rate variability, and subjective responses to social evaluative threat in women. Psychoneuroendocrinology, 42, 49–58.
Baker, F. C., Maloney, S., & Driver, H. S. (1999). A comparison of subjective estimates of sleep with objective polysomnographic data in healthy men and women. Journal of Psychosomatic Research, 47(4), 335–341.
Baron, R. M., & Kenny, D. A. (1986). The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology, 51, 1173–1182.
Bates, D., Maechler, M., Bolker, B., & Walker, S. (2015). Fitting linear mixed-effects models using lme4. Journal of Statistical Software, 67(1), 1–48.
Blake, M., Waloszek, J. M., Schwartz, R., Murray, G., Dahl, R. E., Bootzin, R., et al. (2016). The SENSE study: post intervention effects of a randomized controlled trial of a cognitive-behavioral and mindfulness-based group sleep improvement intervention among at-risk adolescents. Journal of Consulting and Clinical Psychology, 84(12), 1039–1051.
Bluth, K., Gaylord, S. A., Campo, R. A., Mullarkey, M. C., & Hobbs, L. (2016). Making friends with yourself: a mixed methods pilot study of a mindful self-compassion programs for adolescents. Mindfulness, 7, 479–492.
Breines, J. G., Thoma, M. V., Gianferante, D., Hanlin, L., Chen, X., & Rohleder, N. (2014). Self-compassion as a predictor of interleukin-6 response to acute psychosocial stress. Brain, Behavior, and Immunity, 37, 109–114.
Brion, J. M., Leary, M. R., & Drabkin, A. S. (2014). Self-compassion and reactions to serious illness:the case of HIV. Journal of Health Psychology, 19(2), 218–229.
Buysse, D. J., Reynolds III, C. F., Monk, T. H., Berman, S. R., & Kupfer, D. J. (1989). The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Journal of Psychiatric Research, 28(2), 193–213.
Carlson, L. E., & Garland, S. N. (2005). Impact of mindfulness-based stress reduction (MBSR) on sleep, mood, stress, and fatigue symptoms in cancer outpatients. International Journal of Behavioural Medicine, 12(4), 278–285.
Cohen, S., Kamarck, T., & Mermelstein, R. (1983). A global measure of perceived stress. Journal of Health and Social Behavior, 24(4), 385–396.
Garland, S. N., Campbell, T., Samuels, C., & Carlson, L. E. (2013). Dispositional mindfulness, insomnia, sleep quality and dysfunctional sleep beliefs in post-treatment cancer patients. Personality and Individual Differences, 55(3), 306–311.
Hall, C. W., Row, K. A., Wuensch, K. L., & Godley, K. R. (2013). The role of self-compassion in physical and psychological well-being. The Journal of Psychology, 147(4), 311–323.
Hubbling, A., Reilly-Spong, M., Kreitzer, M. J., & Gross, C. R. (2014). How mindfulness changed my sleep: focus groups with chronic insomnia patients. BMC Complementary and Alternative Medicine, 14(1), 50.
Howell, A. J., Digdon, N. L., & Buro, K. (2010). Mindfulness predicts sleep-related self-regulation and well-being. Personality and Individual Differences, 48(4), 419–424.
Howell, A. J., Digdon, N. L., Buro, K., & Sheptycki, A. R. (2008). Relations among mindfulness, well-being, and sleep. Personality and Individual Differences, 45(8), 773–777.
Jackowska, M., Dockray, S., Hendrickx, H., & Steptoe, A. (2011). Psychosocial factors and sleep efficiency: discrepancies between subjective and objective evaluations of sleep. Psychosomatic Medicine, 73(9), 810–816.
Kelly, A. C., Zuroff, D. C., Foa, C. L., & Gilbert, P. (2010). Who benefits from training in self-compassionate self-regulation? A study of smoking reduction. Journal of Social and Clinical Psychology, 29(7), 727–755.
Kemper, K. J., Mo, X., & Khayat, R. (2015). Are mindfulness and self-compassion associated with sleep and resilience in health professionals? The Journal of Alternative and Complementary Medicine, 21(8), 496–503.
Leary, M. R., Tate, E. B., Adams, C. E., Batts Allen, A., & Hancock, J. (2007). Self-compassion and reactions to unpleasant self-relevant events: the implications of treating oneself kindly. Journal of Personality and Social Psychology, 92(5), 887–904.
Luyster, F. S., Strollo, P. J., Zee, P. C., & Walsh, J. K. (2012). Sleep: a health imperative. Sleep, 35(6), 727–734.
Marques, M., Pereira, A. T., Freitas, V., Bento, E., Azevedo, J., Xavier, S., et al. (2016). Self-compassion and insomnia at pregnancy. European Psychiatry, 33, S268–S268.
Morin, C. M. (1993). Insomnia: Psychological Assessment and Management. New York: The Guilford Press.
Morin, C. M., Rodrigue, S., & Ivers, H. (2003). Role of stress, arousal, and coping skills in primary insomnia. Psychosomatic Medicine, 65, 259–267.
Neff, K. D. (2003a). Self-compassion: an alternative conceptualization of a healthy attitude toward oneself. Self and Identity, 2(2), 85–101.
Neff, K. D. (2003b). The development and validation of a scale to measure self-compassion. Self and Identity, 2(3), 223–250.
Neff, K. D., & Germer, C. K. (2013). A pilot study and randomized controlled trial of the mindful self-compassion program. Journal of Clinical Psychology, 69(1), 28–44.
Neff, K. D., Kirkpatrick, K. L., & Rude, S. S. (2007). Self-compassion and adaptive psychological functioning. Journal of Research in Personality, 41(1), 139–154.
Neff, K. D., Pisitsungkagarn, K., & Hsieh, Y. P. (2008). Self-compassion and self-construal in the United States, Thailand, and Taiwan. Journal of Cross-Cultural Psychology, 39(3), 267–285.
Ong, J. C., Ulmer, C. S., & Manber, R. (2012). Improving sleep with mindfulness and acceptance: a metacognitive model of insomnia. Behaviour Research and Therapy, 50(11), 651–660.
R Core Team. (2017). R: a language and environment for statistical computing. In R Foundation for Statistical Computing, Vienna, Austria URL https://www.R-project.org/.
Preacher, K. J., & Hayes, A. F. (2008). Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods, 40(3), 879–891.
Raes, F., Pommier, E., Neff, K. D., & Van Gucht, D. (2011). Construction and factorial validation of a short form of the self-compassion scale. Clinical Psychology & Psychotherapy, 18(3), 250–255.
Sirois, F. M. (2015). A self-regulation resource model of self-compassion and health behavior intentions in emerging adults. Preventive Medicine Reports, 2, 218–222.
Sirois, F. M., Kitner, R., & Hirsch, J. K. (2015a). Self-compassion, affect, and health-promoting behaviors. Health Psychology, 34(6), 661–669.
Sirois, F. M., Molnar, D. S., & Hirsch, J. K. (2015b). Self-compassion, stress, and coping in the context of chronic illness. Self and Identity, 14(3), 334–347.
Steptoe, A., Kunz-Ebrecht, S., Owen, N., Feldman, P. J., Willemsen, G., Kirschbaum, C., & Marmot, M. (2003). Socioeconomic status and stress-related biological responses over the working day. Psychosomatic Medicine, 65(3), 461–470.
Steptoe, A., O'Donnell, K., Marmot, M., & Wardle, J. (2008). Positive affect, psychological well-being, and good sleep. Journal of Psychosomatic Research, 64(4), 409–415.
Teixeira, I., Simões, S., Marques, M., Espírito-Santo, H., & Lemos, L. (2016). Self-criticism and self-compassion role in the occurrence of insomnia on college students. European Psychiatry, 33, S268–S268.
Terry, M. L., Leary, M. R., Mehta, S., & Henderson, K. (2013). Self-compassionate reactions to health threats. Personality and Social Psychology Bulletin, 39(7), 911–926.
Wong, C. C., & Mak, W. W. (2013). Differentiating the role of three self-compassion components in buffering cognitive-personality vulnerability to depression among Chinese in Hong Kong. Journal of Counseling Psychology, 60(1), 162–169.
Acknowledgements
We thank all the participants who participated in the study.
Funding
This work was funded by the MOE (Ministry of Education) Project of Humanities and Social Science (16YJCZH107) and the National Natural Science Foundation of China (31700961).
Author information
Authors and Affiliations
Contributions
YH: designed and executed the study, conducted data analyses, and wrote the paper. YW: designed and executed the study and wrote the paper. YS: collaborated with data collection. JA and SP: collaborated with data collection and the editing of the final manuscript.
Corresponding author
Ethics declarations
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of Texas State University Human Institutional Review Board and the Department of Psychology of Sun Yat-sen University Human Subject Review Boards, as well as with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in this study.
Conflict of Interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Hu, Y., Wang, Y., Sun, Y. et al. Diary Study: the Protective Role of Self-Compassion on Stress-Related Poor Sleep Quality. Mindfulness 9, 1931–1940 (2018). https://doi.org/10.1007/s12671-018-0939-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12671-018-0939-7