Abstract
While sinonasal intestinal type adenocarcinoma (ITAC) is defined by an intestinal phenotype, non-intestinal type adenocarcinoma (non-ITAC) is traditionally viewed as a diagnosis of exclusion, despite previous implication of a seromucinous phenotype and similarity to sinonasal seromucinous hamartomas (SSH). We performed a comparison of clinicopathologic and immunophenotypic features of ITAC, non-ITAC and SSH using traditional discriminatory markers and new markers of seromucinous differentiation. Twenty-three non-ITAC, 17 ITAC, and 5 SSH were retrieved (1987–2014). As expected, ITAC occurred predominantly in the nasal cavity in elderly patients (mean age 65 years) with a striking male predilection (15:2). Regardless of grade/subtype, all ITAC were invariably CK20 and CDX2 positive, and many (11/15) showed some CK7 positivity. Non-ITAC occurred in younger individuals (mean age 51 years) with a slight female predilection (male to female ratio: 10:13) and showed diverse morphologic patterns and grades, some with morphologic similarity to SSH. SSH occurred in younger individuals (mean age 33 years). Non-ITAC and SSH were invariably CK7 positive and CK20 negative, however, 4/22 non-ITAC and 2/5 SSH showed squamoid morular metaplasia that aberrantly expressed CDX2 and co-expressed nuclear β-catenin. Markers of seromucinous differentiation (S100, DOG1, and SOX10) were essentially absent in ITAC, but present to varying degrees in the majority of non-ITAC and all SSH. Thus, the term ‘seromucinous adenocarcinoma’ is the more appropriate designation for non-ITAC. Squamoid morules in non-ITAC and SSH may be an immunophenotypic pitfall given the aberrant CDX2 expression.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Primary non-salivary type sinonasal adenocarcinomas are rare malignancies. In a SEER database analysis of cases (1973–2006), they comprised only 13 % (n = 848) of all sinonasal carcinomas reported [1]. Currently, the most meaningful branch point in taxonomic categorization consists of separation of intestinal type adenocarcinomas (ITAC) and non-intestinal type sinonasal adenocarcinomas (non-ITAC).
ITAC are more common than non-ITAC and are often associated with occupational exposures including formaldehyde, wood, and leather dust [2–5]. The occupationally derived ITAC have a striking male predominance, predilection for the nasal cavity and ethmoid sinus and have a morphologic appearance that is similar to colonic tubulovillous adenomas and adenocarcinomas, hence their name. ITAC are also characterized by expression of intestinal type markers such as cytokeratin (CK) 20, CDX2, and villin, though they also frequently express cytokeratin 7 [6, 7]. About half of these recur locally, and lymph node and distant metastases are uncommon [2]. Prognosis depends on stage and histologic subtype/grade. Generally, low grade papillary-tubular patterned tumors have a much better outcome (3 year survival of 82 %) than high grade solid tumors (3 year survival of 36 %) [8].
On the other hand, less is understood about non-ITACs, which consist of adenocarcinomas that lack aforementioned intestinal morphology or immunophenotype and do not fall into named salivary gland carcinoma types. These encompass tumors described in the literature as: terminal tubulus adenocarcinoma [9], sinonasal tubulopapillary low-grade adenocarcinoma [10], low grade sinonasal adenocarcinoma [11], and seromucinous adenocarcinoma [12]. Unlike ITAC, an etiologic link with occupational/chemical exposure is not established.
The histogenesis/morphogenesis is not exactly clear. While often regarded as a surface mucosa derived tumor [11], some of its synonyms imply a seromucinous phenotype [9, 12]. They are generally substratified into low and high grade tumors. Low grade tumors are more frequent and have a very indolent course with recurrences in 25–30 % [11, 12] and only rare deaths from disease, while high grade tumors are very aggressive. In high grade tumors, considerable histologic diversity has been documented in subcategories described by Stelow et al. [13], some of which are definitively surface derived (i.e. ex Schneiderian papilloma). On the other end of the spectrum, morphologic overlap was noted between sinonasal seromucinous hamartomas (SSHs) and a subset of low grade non-ITAC, raising the possibility of a common pathogenesis [14, 15]. First reported in 1974 by Baillie and Batsakis [16], SSHs are rare lesions with a predilection for the posterior nasal septum, not unlike respiratory epithelial adenomatoid hamartoma. While SSH show a lobular architecture and do not infiltrate, the crowding of acini and typical absence of a delimiting myoepithelial cell layer may cause concern for malignancy. Interestingly, this potential relationship between at least a subset of non-ITAC and SSH would point to a seromucinous origin for the former.
This commonality can now be explored with the advent of new markers. Using the classic ‘intestinal type panel,’ both non-ITACs and SSH are expected to be negative for CK20 and CDX2, and positive for CK7. But surprisingly, in the largest series of SSHs to date, we had contributed one case that demonstrated focal CDX2 immunoreactivity in association with squamoid morules [14]. Since then we had noted this phenomenon in cases of non-ITAC. Thus, both entities share a similar pitfall in addition to morphologic similarities. In terms of less traditional markers in sinonasal adenocarcinomas, both SSH, and non-ITAC, particularly those designated as low grade tubulopapillary adenocarcinomas, are known to be S100 positive [14, 17]. But while S100 is variably expressed in normal seromucinous glands, it is not strictly a ‘seromucinous marker.’ Recent acinar/intercalated duct markers such as DOG1 [18] and SOX10 [19] show appeal in terms of addressing the question of whether a subset of non-ITAC are ‘seromucinous’ rather than surface derived. In order to identify this potential subcategory of non-ITAC with a seromucinous phenotype and determine the prevalence of this unique pitfall of aberrant CDX2 immunoreactivity with morular metaplasia in non-ITAC and SSH, we herein review our experience with our series of SSH, non-ITAC, and ITAC.
Materials and Methods
Case Selection
This study was approved by our Institutional Review Board (IRB#:PRO07050360). A total of 23 cases designated as “non-intestinal type adenocarcinoma,” “tubulopapillary adenocarcinoma,” or “adenocarcinoma, not otherwise specified,” 5 cases designated as “sinonasal seromucinous hamartomas”, and 21 cases designated as “ITAC” were retrieved from the pathology archives and consult files of UPMC (1987–2014). Fourteen cases of “sinonasal undifferentiated carcinoma” were retrieved as well for review for potential reclassification. Available clinical and demographic parameters were obtained. Cases not included for review in this study were: 6 cases of “carcinomas ex Schneiderian papillomas (reported from our institution previously)” [20], and 2 “clear cell/sinonasal renal cell like adenocarcinoma (one also reported previously by us)” [21].
Reclassification
Cases were re-reviewed to confirm diagnosis. ITAC were defined as primary adenocarcinomas of the sinonasal tract with morphologic and/or immunophenotypic evidence of intestinal differentiation. Non-ITAC were accepted if they showed predominantly glandular differentiation, did not fit into a salivary tumor category, and showed no evidence for intestinal or prominent neuroendocrine differentiation. While previously described apocrine/oncocytic-mucinous categories in high grade non-ITAC were acknowledged [13], these were excluded from analysis if encountered, since they were not likely candidates for a seromucinous phenotype. Cases with ‘blastomatous’ features were still included, only if predominantly glandular without a prominent neuroendocrine or stromal component. SSH were defined as bland glandular proliferations with a lobular pattern, non-infiltrative border and no evidence of papillary or true cribriform growth [14]. On re-review, four cases of non-ITAC were reclassified as follows: sinonasal undifferentiated carcinoma (2 cases), apocrine carcinoma (1 case), and adenoid cystic carcinoma with high grade transformation (1 case), and subsequently excluded from this study. Four cases of ITAC were reclassified as non-ITAC. None of the sinonasal undifferentiated carcinomas could be reclassified as adenocarcinoma for inclusion in the study. Thus, the final distribution of cases is as follows: 23 non-ITAC, 17 ITAC, and 5 SSH.
Histologic Assessment
All tumors were assigned a histologic grade. For ITAC, the Kleinsasser and Schroeder classification [8] was used for grading. Briefly well differentiated tumors with papillary growth and fairly monomorphic stratified nuclei (i.e. villous adenoma like) and scattered goblet cells were classified as papillary-tubular cylinder cell-I (PTCC-I), tumors with more infiltrative irregular tubuloglandular spaces and cytonuclear atypia were considered papillary-tubular cylinder cell-II (PTCC-II), and tumors with a solid predominant growth and pronounced cytonuclear atypia were considered papillary-tubular-cylinder cell-III (PTCC-III). Tumors with abundant mucin production reminiscent of a ‘colloid carcinoma’ were considered alveolar goblet cell (AGC) type. Tumors with predominant signet ring cell growth were designated as signet ring cell (SRC) type. Tumors with mixed morphology were considered transitional (Trans).
Non-ITAC were graded intuitively as there is currently no grading scheme for these tumors. Grade was thus a synthesis of cytonuclear atypia, mitoses and necrosis and was stratified into three tiers (low, intermediate, and high). Low grade tumors showed small, monomorphic, evenly spaced nuclei with smooth indistinct nuclear membranes, and inconspicuous nucleoli; mitotic rates were <2 mitoses per 10 high power fields, and there was no necrosis. Intermediate grade tumors had larger nuclei with some overlap and size variation, membrane irregularities and prominent nucleoli; mitotic rates were <5 mitoses per 10 high power fields, and only focal punctate necrosis was acceptable. High grade tumors had prominent nuclear size variation, membrane and chromatin irregularities; mitotic rates were 5 or more per 10 high power fields, and necrosis was fairly common. Additionally, tumors were categorized based on growth pattern. Major patterns were defined as follows: SSH-like (minimal deviation) tumors were defined as tumors with a lobular arrangement of small caliber tubules lined by cuboidal cells with rounded borders similar to SSH. However, unlike SSH, these tumors show confluent growth, focal cribriform, papillary growth and/or infiltration. Tubulopapillary tumors demonstrated the classic appearance described by Skalova et al. [10] and consisted of larger caliber tubules, cribriform areas and microcysts as well as varying degrees papillary growth with tumor cells ranging from cuboidal to columnar. Solid-cribriform tumors consisted of solid to compressed tubules or cribriform nests lined by cuboidal, columnar or polygonal cells. Tumors with mixed patterns were also documented separately. Additionally, other features (i.e. cystic change, calcifications, lymphoid stroma) were recorded separately.
Immunohistochemical Staining
Immunohistochemical staining was performed on cases with available material. Briefly, the studies were performed on 4-µm-thick sections of formalin-fixed, paraffin-embedded tissue using a Ventana autostainer (Ventana Medical Systems, Tucson, AZ, USA). Labeling was performed using the i-VIEW 20 diaminobenzamide (DAB) detection kit (Ventana Medical Systems, Tucson, AZ, USA) with a brown chromogen substrate for all antibodies except S100, which was labeled using ultraVIEW alkaline phosphatase (AP) red detection kit (Ventana Medical Systems, Tucson, AZ, USA). SOX10 was performed on a Leica BOND-III (Leica Microsystems Inc, Buffalo Grove, IL, USA) and visualized with Novocastra Bond Polymer Refine Red Detection (through Leica Microsystems). The antibodies, manufacturers, clones, and dilutions are listed in Table 1.
Results
Clinicopathologic Features
ITAC
The clinicopathologic features are summarized in Table 2. ITAC occurred in older individuals (mean age 65 years, range 35–92 years) with a striking male predilection (15:2). Nasal cavity was the most common site (13/17, 76 %). Other sites involved included ethmoid (2/17, 12 %), maxillary (1/17, 6 %), and frontal (1/17, 6 %) sinuses. Of note, there were no ITAC with sphenoid sinus involvement. In this series of ITAC, there were 4 PTCC-I, 6 PTCC-II, 2 PTCC-III, 4 AGC, and 1 Trans (Fig. 1). No pure SRC were noted but one PTCC-III recurred as SRC (Fig. 1d, e). The Trans ITAC was a mixture of PTCC-I and AGC.
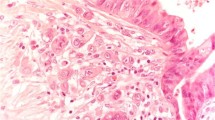
Morphologic spectrum of ITAC. a PTCC-I showing a predominantly papillary growth pattern (H&E, ×40), and stratification of fairly monomorphic nuclei resembling the appearance of a colonic adenoma (inset H&E, ×200). b PTCC-II showing a tubular and cribriform growth with stromal reaction similar to colorectal carcinoma (H&E, ×40), and more cytonuclear atypia and apoptotic debris (inset H&E, ×200). c AGC showing predominantly mucin filled spaces akin to a mucinous adenocarcinoma of colon (H&E, ×40), tumor nests are found floating in the mucin filled spaces (inset H&E, ×200). d PTCC-III showing a solid growth pattern and cytologic atypia (H&E, ×100). e Recurrence of same case showing SRC pattern instead (H&E, ×100)
Non-ITAC
Non-ITAC occurred on average almost two decades earlier (mean age 51 years: range 19–80) with a more even gender distribution (male to female ratio: 10:13). Nasal cavity was the most common site (13/23, 57 %), followed by maxillary (4/23, 17 %), and sphenoid (4/23, 17 %) sinuses. Cytonuclear grade distribution was as follows: low grade: 11/23 (48 %), intermediate grade: 5/23 (22 %), and high grade: (7/23, 30 %). The majority of tumors showed a tubulopapillary growth pattern (15/23, 65 %) with 9/15 (60 %) being low grade, 5/15 (33 %) being intermediate grade, and 1/15 (7 %) being high grade. Two of 23 cases (9 %) showed an SSH-like appearance with only focal confluent growth or infiltration, and both were low grade. Solid-cribriform tumors (4/23, 17 %) and tumors with mixed pattern (2/23, 9 %) were all high grade (Fig. 2). One of the mixed patterned tumors showed lower grade tubulopapillary areas, and higher grade tumors with prominent trabecular growth and rosette-like glands that were somewhat ‘blastomatous’ as described by Stelow et al. [13] (Fig. 2d, e). Four tubulopapillary tumors showed prominent cystic change, and four tubulopapillary tumors showed psammomatoid calcifications (Fig. 3a, b). Interestingly, one tumor showed a ‘Warthin like’ appearance with prominent lymphoplasmacytic stroma (Fig. 3c).
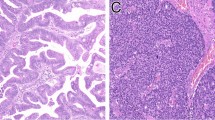
Morphologic spectrum of non-ITAC. a SSH-like (minimal deviation) non-ITAC showing a rounded tubulolobular growth similar to SSH, but with larger more confluent tumor nests (H&E, ×40). This tumor is low grade and composed of bland monomorphic tubules with almost no nuclear atypia (inset H&E, ×200). b Tubulopapillary non-ITAC showing columnar cells with nuclear stratification evident even at this magnification (H&E, ×40). This tumor is intermediate grade with nuclear membrane irregularities and prominent nucleoli with some mitotic activity (inset H&E, ×200). c Solid-cribriform non-ITAC with prominent central comedonecrosis (H&E, ×40). This tumor is high grade with prominent nuclear pleomorphism in addition to the necrosis (inset H&E, ×200). d Non-ITAC with tubulopapillary areas and intermediate nuclear grade (H&E, ×100). e The majority of this same case, however, showed solid ribbon like trabecular growth reported in ‘blastomatous’ tumors (H&E, ×100)
Variant morphologies in tubulopapillary non-ITAC. a Low grade tumor with micro and macrocystic change (H&E, ×100). b Low grade tumor with prominent psammoma-like calcifications (H&E, ×100). c Low grade tumor with lymphoplasmacytic infiltrates in papillae resembling those of salivary Warthin tumor (H&E, ×100)
SSH
SSH had a predilection for younger adults (mean age 33 years, range 14–66 years) with a female predilection (male:female ratio: 1:4). All cases occurred in the nasal cavity. In three cases of SSH, subsite was known and included: turbinate (2 cases) and nasal septum (1 case). One of the SSH from the turbinate was actually incidentally noted in a 38 year old female patient who underwent surgery for her contralateral non-ITAC. All cases demonstrated a lobular arrangement of tubules without areas of confluence, papillary, or infiltrative growth (Fig. 4a). One case showed respiratory epithelial adenomatoid hyperplasia like areas (Fig. 4b).
Identification of Morular Metaplasia
Interestingly, despite being adenocarcinomas fundamentally, squamoid or morular metaplasia was identified in a subset of cases, consisting of squamoid nests that showed none to focal keratinization. In some morules, cystic change or residual lumina were noted in the center (Fig. 5a). Morular metaplasia was noted in 4/22 (17 %) non-ITAC; two were SSH-like and low grade, one was solid-cribriform and high grade, and one was mixed (tubulopapillary and blastomatous) and high grade. Morules were noted in 2/5 (40 %) SSH as well (Fig. 5b), but no evidence of morular metaplasia was noted in any of the ITACs.
Immunophenotype in ITAC, Non-ITAC, and SSH
Immunophenotype is summarized in Table 3.
Classical Markers: CK7, CK20, CDX2, and p63
As expected, all ITAC stained were CK20 positive (15/15), CDX2 positive (13/13), and 11/15 (73 %) cases showed at least focal CK7 positivity. All tested non-ITAC (21/21) and SSH (5/5) were CK7 positive and CK20 negative (0/20 and 0/5 respectively) (Fig. 6a–l). However, CDX2 was noted in 3/20 (15 %) non-ITAC, and 2/4 (50 %) SSH, specifically in areas of morular metaplasia (Fig. 6m, n). Only one non-ITAC with morular metaplasia was CDX2 negative. Five of the CDX2 positive cases (3 non-ITAC and 2 SSH) with morular metaplasia were tested with β-Catenin and also showed nuclear accumulation corresponding to the morular areas (Fig. 6o).
Immunophenotype of ITAC, non-ITAC, and SSH using classical markers. a ITAC (H&E, ×40 showing. b CK20 (×100). c CDX2 (×100) positivity. d focal CK7 positivity (×100). e Intermediate grade tubulopapillary non-ITAC (H&E, ×40) showing. f CK20 (×100), and g CDX2 (×100) negativity, and h CK7 positivity (×100). i SSH (H&E, ×40) similarly showing j CK20 (×100), and k CDX2 (×100) negativity, and l CK7 positivity (×100). However, a subset of non-ITAC and SSH showed m squamoid morular metaplasia (H&E, ×100) which showed n CDX2 positivity in the morules (×200). o This corresponded to areas of nuclear accumulation of β-catenin (×200)
Aside from rare isolated weakly positive cells, p63 was negative in all ITAC tested (0/10). In non-ITAC, only 1/17 (6 %) cases showed significant p63, though still focal, positivity (muscle markers were negative, data not shown). All three SSH were negative for p63, though one case did show a few seromucinous glands with delimiting p63 positive basal/myoepithelial layer. In non-ITAC and SSH with morular metaplasia, scattered weakly p63 positive cells were occasionally noted in morules.
New “Seromucinous” Markers: S100, SOX10, DOG1
In normal sinonasal seromucinous glands, S100 was diffusely strongly positive in serous acini, weakly positive to negative in the mucous acini and excretory ducts. DOG1 showed moderate to intense apical luminal staining of serous acini with weaker staining in mucous acini and essential negativity in ducts. SOX10 showed a fairly even intensity across serous and mucous acini with loss in excretory ducts.
In tumors, none of the ITAC (0/10) were S100 positive. On the other hand, 14/19 (74 %) non-ITAC, and all (5/5) SSH showed at least focal S100 staining. Only one ITAC (1/10, 10 %) showed focal weak DOG1 apical luminal staining, while 13/19 (68 %) non-ITAC, and all tested (4/4) SSH showed at least focal apical luminal staining for DOG1. One case, a high grade tumor, showed some basolateral membranous or cytoplasmic staining as often seen in acinic cell carcinoma [18]. However, S100, and DOG1 were not entirely concordant in non-ITAC. Overall, 18/19 tumors expressed either DOG1 or S100 but only 9/19 cases co-expressed S100 and DOG1; five were DOG1 negative yet S100 positive, and four were DOG1 positive yet S100 negative.
SOX10 was only available on a limited number of cases but was present in 7/9 (78 %) non-ITAC, and the single SSH tested, and none of the ITAC (0/6). Within this limited set of non-ITAC, all nine cases were positive for either DOG1 or S100 or SOX10. Only 4/9 were positive for both SOX10 and S100. S100 was positive in one SOX10 negative case while SOX10 was positive in three S100 negative cases, and both SOX10 and S100 were negative in one case. In comparing SOX10 to DOG1, one case was DOG1 positive and SOX10 negative, one case negative for both DOG1 and SOX10, and only 5/9 cases were SOX10 and DOG1 positive. However, only 2/9 cases were triply positive for S100, DOG1, and SOX10.
Thus, at least one of the ‘seromucinous markers’ was expressed in the majority of non-ITAC, and all SSH. In general, low grade non-ITAC showed more diffuse and intense staining for these markers than intermediate and high grade non-ITAC. S100, DOG1, and SOX10 profiles for SSH and non-ITAC are demonstrated in Fig. 7.
Immunophenotype of SSH and non-ITAC using markers of seromucinous differentiation. a SSH (H&E, ×40) showing b S100 positivity in serous acini (×100), c DOG1 apical luminal staining mainly in serous acini (×100), and d SOX10 expression in all acini (×100). e Intermediate grade tubulopapillary non-ITAC (H&E, ×40) showing f focal S100 positivity (×100), g weak DOG1 apical luminal staining (×100), and h SOX10 positivity (×100)
Discussion
Even when excluding named salivary tumors, the diversity of sinonasal adenocarcinomas can be underestimated because of their rarity. In keeping with prior studies [2–4, 6], ITAC are distinct and are defined by an intestinal phenotype. However, we now confirm that a large subset of non-ITAC is indeed of seromucinous phenotype, highlighting similarities with their benign/hamartomatous counterpart, SSH. The implication then is that the working definition of non-ITAC can no longer be considered a diagnosis of exclusion [22].
Essentially all low-intermediate grade non-ITAC in the tubulopapillary and SSH like categories show positivity for at least one of the three seromucinous differentiation markers included in this study. As expected, all SSH expressed these markers quite extensively. This seromucinous immunoprofile for low-intermediate grade non-ITAC is not entirely surprising since many investigators have commented on the morphologic similarity to seromucinous glands [8, 12]. Furthermore, S100 positivity in low grade non-ITAC has been known for some time [10, 12, 15]. But even in this limited context, investigators have been reluctant to name S100 as supportive evidence for a seromucinous phenotype, perhaps justifiably so, given the breadth of expression of this marker in other cell types [10, 12]. Coupled with the morphologic features, the documentation of DOG1 and SOX10 in many of these tumors adds more certainty to this concept of seromucinous differentiation.
We initially described DOG1 as a marker of salivary acinar and intercalated duct differentiation in major salivary glands, though part of our validation included minor salivary sites as well [18]. The major difference in sinonasal glands is that the DOG1 staining, though fairly prominent in serous acini, is not as intense as in major salivary glands serous acini, likely given the differences in secretory function (DOG1 is implicated in saliva secretion through its function as a calcium activated chloride channel) [18]. Similarly, Ohtomo and colleagues [19] show a similar distribution of SOX10 in major salivary gland acini and intercalated ducts, though they did not specifically comment on the distribution at sinonasal sites. In our study we find that SOX10 remains fairly robust as a marker of seromucinous glands, quite similar to what is seen at major salivary sites. Both DOG1 and SOX10 when present in SSH and low-intermediate grade non-ITAC recapitulated the distribution seen in normal seromucinous glands.
Interestingly, the few high grade tumors in our study also showed some degree of seromucinous differentiation. Higher grade tumors, even when positive for a marker do however show attenuation of staining intensity and distribution. While this may seem a bit at odds with the schema for high grade non-ITAC put forth by Stelow et al. [13] where many tumors were reported to be of surface derivation, it must be noted that we did not encounter a pure blastomatous tumor in our archival search, and we avoided the oncocytic-mucinous (ex Schneiderian papilloma) category (which for the most part is technically squamoglandular), clear cell and apocrine tumors in order to enrich for high grade non-ITAC that may show seromucinous differentiation.
Despite the high prevalence of seromucinous markers in our non-ITAC, any statements on performance characteristics of each of these markers would be preliminary at best given the limited number of cases tested as well as variability in fixation and processing over this rather large timespan for these archival cases. SOX10 in particular seems profoundly affected by decalcification for example since only 16 cases were successfully stained.
An interesting and somewhat novel finding discovered in this survey of sinonasal adenocarcinomas is the presence of squamoid morular metaplasia. As noted previously, this phenomenon seems restricted to non-ITAC and SSH, suggesting a relationship only to the seromucinous phenotype. Morular metaplasia has been noted in several different lesional types including endometrial carcinoma, fetal type lung adenocarcinomas, pancreaticoblastoma, and (obviously) cribriform-morular variant of papillary thyroid carcinomas [17, 23–27]. Aside from the novelty, it does potentially result in a pitfall, since these morules show CDX2 reactivity. Taken out of morphologic context, the danger may be misinterpretation as evidence for intestinal differentiation. Tilson et al. [28] have recently noted this as an occasional problem, and demonstrate that CDX2 shows some degree of infidelity as a marker of intestinal phenotype when surveying a wide array of sinonasal tumors. Hence, this is yet another example of this, though it is fairly distinct and restricted to these morular areas. Thus with attention to morphologic distribution and demonstration of CK20 negativity, any potential dilemma is easily resolved. Additionally, as described in other sites, these morules typically show nuclear accumulation of β-Catenin. It is unexpected to find CDX2 in morules, but it may along with β-Catenin, play a role in squamous morula formation [29].
Finally, we did survey p63 in this series and this yielded some findings of minor importance. As expected, ITAC were essentially negative, though in non-ITAC we found a case with focal but noticeable p63 positivity even in non-morular, overtly glandular areas. However, this case was negative for muscle markers (data not shown). With modern staining protocols, it is apparent that p63 expression is not always restricted to basal, squamous or myoepithelial cells [30, 31]. While we did not perform p40 (ΔNp63) on this case as a more specific isoform selective immunostain, we suspect that the p63 staining in this non-ITAC represents this phenomenon. Regarding SSH, while the ductoacinar cells are uniformly negative we did identify one case with a focal delimiting myoepithelial cell layer. Thus in keeping with a recent report that not all SSH are devoid of myoepithelial cells [32].
In summary, sinonasal non-ITAC often shows seromucinous marker expression, including newer markers such as DOG1 and SOX10 and show phenotypic similarities to SSH. Low-intermediate grade tumors display this most prominently, but even some high grade tumors of the non-blastomatous, non-apocrine, non-oncocytic types are likely seromucinous. Thus, at least a subgroup of non-ITAC is defined by more than just the absence of intestinal phenotype. Both non-ITAC and SSH may show a peculiar morular metaplasia that may express CDX2 which may occasionally cause confusion.
References
Turner JH, Reh DD. Incidence and survival in patients with sinonasal cancer: a historical analysis of population-based data. Head Neck. 2012;34(6):877–85. doi:10.1002/hed.21830.
Barnes L. Intestinal-type adenocarcinoma of the nasal cavity and paranasal sinuses. Am J Surg Pathol. 1986;10(3):192–202.
Kleinsasser O, Schroeder HG. The pathology and clinical picture of adenocarcinoma of the nose after wood dust exposure. Strahlenther Onkol. 1989;165(6):437–40.
Franquemont DW, Fechner RE, Mills SE. Histologic classification of sinonasal intestinal-type adenocarcinoma. Am J Surg Pathol. 1991;15(4):368–75.
Batsakis JG, Mackay B, Ordonez NG. Enteric-type adenocarcinoma of the nasal cavity. An electron microscopic and immunocytochemical study. Cancer. 1984;54(5):855–60.
Cathro HP, Mills SE. Immunophenotypic differences between intestinal-type and low-grade papillary sinonasal adenocarcinomas: an immunohistochemical study of 22 cases utilizing CDX2 and MUC2. Am J Surg Pathol. 2004;28(8):1026–32.
Kennedy MT, Jordan RC, Berean KW, Perez-Ordonez B. Expression pattern of CK7, CK20, CDX-2, and villin in intestinal-type sinonasal adenocarcinoma. J Clin Pathol. 2004;57(9):932–7. doi:10.1136/jcp.2004.016964.
Kleinsasser O, Schroeder HG. Adenocarcinomas of the inner nose after exposure to wood dust. Morphological findings and relationships between histopathology and clinical behavior in 79 cases. Arch Otorhinolaryngol. 1988;245(1):1–15.
Kleinsasser O. Terminal tubulus adenocarcinoma of the nasal seromucous glands. A specific entity. Arch Otorhinolaryngol. 1985;241(2):183–93.
Skalova A, Cardesa A, Leivo I, Pfaltz M, Ryska A, Simpson R, et al. Sinonasal tubulopapillary low-grade adenocarcinoma. Histopathological, immunohistochemical and ultrastructural features of poorly recognised entity. Virchows Arch. 2003;443(2):152–8. doi:10.1007/s00428-003-0844-9.
Heffner DK, Hyams VJ, Hauck KW, Lingeman C. Low-grade adenocarcinoma of the nasal cavity and paranasal sinuses. Cancer. 1982;50(2):312–22.
Neto AG, Pineda-Daboin K, Luna MA. Sinonasal tract seromucous adenocarcinomas: a report of 12 cases. Ann Diagn Pathol. 2003;7(3):154–9.
Stelow EB, Jo VY, Mills SE, Carlson DL. A histologic and immunohistochemical study describing the diversity of tumors classified as sinonasal high-grade nonintestinal adenocarcinomas. Am J Surg Pathol. 2011;35(7):971–80. doi:10.1097/PAS.0b013e31821cbd72.
Weinreb I, Gnepp DR, Laver NM, Hoschar AP, Hunt JL, Seethala RR, et al. Seromucinous hamartomas: a clinicopathological study of a sinonasal glandular lesion lacking myoepithelial cells. Histopathology. 2009;54(2):205–13. doi:10.1111/j.1365-2559.2008.03198.x.
Jo VY, Mills SE, Cathro HP, Carlson DL, Stelow EB. Low-grade sinonasal adenocarcinomas: the association with and distinction from respiratory epithelial adenomatoid hamartomas and other glandular lesions. Am J Surg Pathol. 2009;33(3):401–8. doi:10.1097/PAS.0b013e3181874ee8.
Baillie EE, Batsakis JG. Glandular (seromucinous) hamartoma of the nasopharynx. Oral Surg Oral Med Oral Pathol. 1974;38(5):760–2.
Sekine S, Shibata T, Matsuno Y, Maeshima A, Ishii G, Sakamoto M, et al. Beta-catenin mutations in pulmonary blastomas: association with morule formation. J Pathol. 2003;200(2):214–21. doi:10.1002/path.1352.
Chenevert J, Duvvuri U, Chiosea S, Dacic S, Cieply K, Kim J, et al. DOG1: a novel marker of salivary acinar and intercalated duct differentiation. Mod Pathol. 2012;25(7):919–29. doi:10.1038/modpathol.2012.57.
Ohtomo R, Mori T, Shibata S, Tsuta K, Maeshima AM, Akazawa C, et al. SOX10 is a novel marker of acinus and intercalated duct differentiation in salivary gland tumors: a clue to the histogenesis for tumor diagnosis. Mod Pathol. 2013;26(8):1041–50. doi:10.1038/modpathol.2013.54.
Nudell J, Chiosea S, Thompson LD. Carcinoma ex-Schneiderian papilloma (malignant transformation): a clinicopathologic and immunophenotypic study of 20 cases combined with a comprehensive review of the literature. Head Neck Pathol. 2014;8(3):269–86. doi:10.1007/s12105-014-0527-7.
Bilodeau EA, Weinreb I, Antonescu CR, Zhang L, Dacic S, Muller S, et al. Clear cell odontogenic carcinomas show EWSR1 rearrangements: a novel finding and a biological link to salivary clear cell carcinomas. Am J Surg Pathol. 2013;37(7):1001–5. doi:10.1097/PAS.0b013e31828a6727.
Bhaijee F, Carron J, Bell D. Low-grade nonintestinal sinonasal adenocarcinoma: a diagnosis of exclusion. Ann Diagn Pathol. 2011;15(3):181–4. doi:10.1016/j.anndiagpath.2010.10.002.
Saegusa M, Okayasu I. Frequent nuclear beta-catenin accumulation and associated mutations in endometrioid-type endometrial and ovarian carcinomas with squamous differentiation. J Pathol. 2001;194(1):59–67. doi:10.1002/path.856.
Tanaka Y, Kato K, Notohara K, Nakatani Y, Miyake T, Ijiri R, et al. Significance of aberrant (cytoplasmic/nuclear) expression of beta-catenin in pancreatoblastoma. J Pathol. 2003;199(2):185–90. doi:10.1002/path.1262.
Hirokawa M, Kuma S, Miyauchi A, Qian ZR, Nakasono M, Sano T, et al. Morules in cribriform-morular variant of papillary thyroid carcinoma: immunohistochemical characteristics and distinction from squamous metaplasia. APMIS. 2004;112(4–5):275–82. doi:10.1111/j.1600-0463.2004.apm11204-0508.x.
Kurihara K, Shimizu S, Chong J, Hishima T, Funata N, Kashiwagi H, et al. Nuclear localization of immunoreactive beta-catenin is specific to familial adenomatous polyposis in papillary thyroid carcinoma. Jpn J Cancer Res. 2000;91(11):1100–2.
Nakatani Y, Masudo K, Miyagi Y, Inayama Y, Kawano N, Tanaka Y, et al. Aberrant nuclear localization and gene mutation of beta-catenin in low-grade adenocarcinoma of fetal lung type: up-regulation of the Wnt signaling pathway may be a common denominator for the development of tumors that form morules. Mod Pathol. 2002;15(6):617–24. doi:10.1038/modpathol.3880575.
Tilson MP, Gallia GL, Bishop JA. Among sinonasal tumors, CDX-2 immunoexpression is not restricted to intestinal-type adenocarcinomas. Head Neck Pathol. 2014;8(1):59–65. doi:10.1007/s12105-013-0475-7.
Wani Y, Notohara K, Saegusa M, Tsukayama C. Aberrant Cdx2 expression in endometrial lesions with squamous differentiation: important role of Cdx2 in squamous morula formation. Hum Pathol. 2008;39(7):1072–9. doi:10.1016/j.humpath.2007.07.019.
Bishop JA, Teruya-Feldstein J, Westra WH, Pelosi G, Travis WD, Rekhtman N. p40 (DeltaNp63) is superior to p63 for the diagnosis of pulmonary squamous cell carcinoma. Mod Pathol. 2012;25(3):405–15. doi:10.1038/modpathol.2011.173.
Rooper L, Sharma R, Bishop JA. Polymorphous low grade adenocarcinoma has a consistent p63+/p40− immunophenotype that helps distinguish it from adenoid cystic carcinoma and cellular pleomorphic adenoma. Head Neck Pathol. 2014;. doi:10.1007/s12105-014-0554-4.
Fleming KE, Perez-Ordonez B, Nasser JG, Psooy B, Bullock MJ. Sinonasal seromucinous hamartoma: a review of the literature and a case report with focal myoepithelial cells. Head Neck Pathol. 2012;6(3):395–9. doi:10.1007/s12105-012-0339-6.
Acknowledgments
We would like to thank the UPMC Research Histology and Immunohistochemistry Laboratory for their excellent technical support. We would also like to thank Mrs. Robyn Roche for her excellent secretarial support. Some of these findings were initially presented as a poster at the United States Canadian Academy of Pathology Meeting in 2012, Vancouver, BC, Canada. This work was supported in part by the Department of Veterans Affairs, BLSR&D. This work does not reflect the views of the US Government or the Department of Veterans Affairs.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Purgina, B., Bastaki, J.M., Duvvuri, U. et al. A Subset of Sinonasal Non-Intestinal Type Adenocarcinomas are Truly Seromucinous Adenocarcinomas: A Morphologic and Immunophenotypic Assessment and Description of a Novel Pitfall. Head and Neck Pathol 9, 436–446 (2015). https://doi.org/10.1007/s12105-015-0615-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12105-015-0615-3