Abstract
Benign fibro-osseous lesions of the craniofacial skeleton (BFOL) are a variant group of intraosseous disease processes that share similar microscopic features characterized by hypercellular fibroblastic stroma containing various combinations of bone or cementum-like tissue and other calcified structures [1–6]. Whereas some are diagnosable histologically, most require a combined assessment of clinical, microscopic and radiologic features. Some BFOL of the craniofacial complex are unique to that location whereas others are encountered in bones from other regions. Reactive, neoplastic, developmental and dysplastic pathologic processes are included under the rubric of BFOL and treatment varies from disease to disease. This review will discuss the clinical, microscopic and radiologic aspects of the more important types of BFOL of the craniofacial complex with updated information on underlying genetic and molecular pathogenic mechanisms of disease. Four main groups of BFOLs will be addressed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Fibrous Dysplasia
Fibrous dysplasia (FD) is a dysplastic skeletal anomaly in which normal bone is distorted and replaced by poorly organized and inadequately mineralized immature bone and fibrous tissue. The disease may affect multiple bones (polyostotic) or a single bone (monostotic). Polyostotic FD is less common and a few of these cases may also be associated with skin pigmentation and endocrine abnormalities, a condition known as the McCune Albright’s syndrome which is more common in female patients. The craniofacial skeleton may be involved in either of the two types of FD. Monostotic FD occurs in the craniofacial skeleton, particularly the maxilla and mandible, in 25 % of the cases [4]. The pathologic process in this anatomic site is not always strictly limited to one bone, but may extend by continuity across suture lines to involve adjacent bones, thus the commonly used notation monostotic in these cases is not always accurate, and the term craniofacial fibrous dysplasia is preferred [5].
FD is a disease of growing bones. Most cases are originally identified in children and adolescents. More than 80 % of craniofacial FD cases are diagnosed within the first two decades of life. Males and females are equally affected. Painless swelling of the facial bones with facial asymmetry is the first manifestation. Diffuse thickening of the bones with involvement of paranasal sinuses, orbits and the foramina of the base of the skull can produce a variety of symptoms, including headache, visual loss, proptosis, nasal obstruction, anosmia and hearing loss [4–6].
Radiographic Features
Radiographic appearance of the lesions depends on the stage of the disease. Early lesions tend to be radiolucent and as it progressively calcifies it becomes more opaque. Craniofacial lesions are typically mixed radiolucent/radio-opaque producing a characteristic “ground glass” appearance. The margins are ill defined and the lesional bone blends imperceptibly with the surrounding normal appearing bone [5–7] (Fig. 1). The paranasal sinuses may become obliterated, and the displacement of the orbit is a common feature.
a CT scan of fibrous dysplasia showing expansion of the mandible by a uniformly sclerotic lesion that blends with the surrounding bone; b immature woven bone trabeculae with no osteoblastic rimming, forming irregular structures resembling Chinese letters, in a fibrous stroma (×200); c higher magnification (×400)
Pathologic Features
Grossly, the affected bone is rubbery, compressible, grayish white tissue that has a gritty texture when cut with a scalpel. Microscopically, normal bone is replaced with a cellular fibroblastic stroma containing variable amounts of randomly dispersed irregular, usually delicate bone trabeculae that evolve directly from the stroma. The bone trabeculae are described as resembling Chinese script letters. Typically they are composed of immature woven bone, rich in osteoid, and not rimmed with osteoblasts [4, 5] (Fig. 2). Rarely, FD contains nodules of hyaline cartilage that vary from microscopic foci to larger grossly evident masses [8]. It has been suggested that the bone of craniofacial FD, unlike that of long bones, may undergo a process of maturation leading to lamellar bone formation [4–6].
a Panoramic radiograph of ossifying fibroma of the mandible. The tumor is expansive with well defined, corticated borders; b bone trabeculae and cementum-like structures dispersed in hypercellular fibrous stroma (×400); c Cementum-like calcified tissue and a well defined border with subjacent cortical bone (×200)
The diagnosis of FD, as in the case of other fibro-osseous lesion, could not always be established by microscopic examination alone, but is rather based, in addition, on clinical, radiographic and intra-operative information. FD affects children and young adults, unlike cemento-ossifying fibroma, which occurs in older adults. Radiographically, FD has ill-defined borders that blend gradually with the surrounding bone.
Genetics
Fibrous dysplasia is a nonhereditary condition caused by a dominant mutation affecting activation of a G protein subunit alpha (GS alpha) early in the course of development [9–12]. Post zygotic activating mutation of the GS alpha subunit leads to mosaic distribution of cells bearing constitutively active adenyl cyclase [9]. A somatic gain of function mutation in GNAS1 gene located at 20q 13.2–13.3 transcribing for GS alpha protein has been identified in all patients reported [9, 11, 12]. The point mutation results in substitution of the arginine residue at position 201, most often, into histidine or cysteine [9–12]. This mutation is identified in the McCune-Albrights Syndrome, isolated polyostotic fibrous dysplasia as well as monostotic fibrous dysplasia [9–12].
Constitutive activation of adenyl cyclase in the affected cells is believed to result in increased cell proliferation and inappropriate differentiation leading to over production of disorganized immature fibrotic bone in both polyostotic as well as monostotic fibrous dysplasia [10, 11]. Activation of adenyl cyclase may also be involved in hormonal hyperproduction and skin pigmentation in McCune-Albright Syndrome [10, 11].
Treatment and Prognosis
Many cases of craniofacial FD become quiescent after puberty. However, persistent growth in later life has been shown in multiple reports [13, 14]. Simple contouring of the affected bone back to normal dimension is usually an effective treatment. Retreatment may be required in small percentage of patients. Partial excision followed by grafting with normal autologous bone or acrylic implants may achieve reduction in the rate of recurrence [4, 13, 15].
Malignant degeneration has been reported in a few cases of FD, most of which are osteosarcomas and less frequently, fibrosarcoma, or chondrosarcoma. In the majority of these cases there was previous history of radiation therapy, which has been used in the past for treatment of FD [13, 16, 17]. Because of this risk, radiation therapy for FD is now strictly contraindicated. However, more recent reports show spontaneous sarcomatous transformation unrelated to radiation exposure in very rare cases [18, 19]. It is therefore prudent to keep patients with FD under long-term follow-up. Any patient showing clinical or radiographic evidence of change should undergo an adequate biopsy to rule out sarcomatous transformation.
Ossifying Fibroma
The term ossifying fibroma is used to describe a benign bone-producing fibrous neoplasm of the skeleton. Lesions that may differ in their clinical presentation, site of predilection, sex, age distribution, and microscopic appearance have been included under the umbrella rubric of ossifying fibroma. Ossifying fibroma of the craniofacial skeleton are separated into two main clinicopathologic entities:
-
1.
Ossifying fibroma of odontogenic origin (cemento-ossifying fibroma), and
-
2.
Juvenile ossifying fibroma, which is further divided into two distinct types:
-
A.
Trabecular juvenile ossifying fibroma (TrJOF)
-
B.
Psammomatoid juvenile ossifying fibroma (PsJOF)
-
A.
Familiarity with these distinct entities of ossifying fibroma is not merely of academic interest but can also be of value in distinguishing them from other fibro-osseous and non-fibro-osseous bone lesions, and thus influence their proper management and the outcome of treatment.
Cemento-Ossifying Fibroma (COF)
This benign odontogenic tumor has been variously called ossifying fibroma, cementifying fibroma, and cemento-ossifying fibroma. The latter is preferred because of its descriptive value and is used in the World Health Organization classification of head and neck tumors [20]. COF affect the tooth bearing areas of the mandible and maxilla.
The neoplastic cells elaborate bone and cementum and are believed to be derived from the progenitor cells of the periodontal membrane. These cells are capable of dual differentiation into fibroblasts, osteoblasts, and cementoblasts. COF is a distinctive jaw lesion that should not be confused with other craniofacial lesions that are also termed ossifying fibroma. The tumors present as painless expansion of the jaws, particularly the mandible. They can attain a very large size with considerable deformity, if untreated. The peak age of incidence is the third and fourth decades with a definite female predilection. The female to male ratio is as high as 5:1 [5, 20, 21].
Radiographic Features
The tumors are well defined and unilocular. They may be radiolucent or may show various degrees of opacification depending on the amount of calcified tissue present. In the mandible, larger lesions tend to expand inferiorly producing a characteristic downward bowing and thinning of the inferior border (Fig. 2). Displacement of surrounding teeth and root resorption may be seen [5, 6, 22, 23].
Pathologic Features
An important feature of COF is that it is well defined and can often be shelled out with relative ease from the surrounding bone. Grossly the tumor is submitted in one piece or in large fragments that are yellowish tan, which may be hemorrhagic, and feels gritty, when cut with a scalpel.
Microscopically the tumor is well defined and may be encapsulated. It is composed of hypercellular fibroblastic stroma with sparse collagen fibers and blood vessels, and containing variable amounts of calcified structures. The stromal fibroblastic cells show hyperchromatic nuclei. Mitosis is not easily found. The calcified structures are composed of variable amounts of osteoid or bone and lobulated basophilic masses of cementum-like tissue resembling the cementicles that are normally found in the periodontal membrane. These structures may coalesce and form curvilinear trabeculae which may be acellular [5, 6, 21, 23] (Fig. 2).
The ratio of the bone to the cementum-like tissue varies in different lesions. In some tumors one or the other type of the calcified tissue may dominate. Osteoblastic rimming of the bone trabeculae is evident. Polarized light microscopy reveals both woven and lamellar bone. The cementum-like tissue is often woven and may show a characteristic quilted pattern [5, 6, 21, 23].
Genetics
Few studies aimed at identifying specific genetic alterations in COF have so far been reported. Pimenta et al. [24] showed three novel mutations in HRPT2 gene in two of three COFs. One of the patients also had a germ-line mutation. Paradoxically, using RT-PCR the authors were unable to identify the mutations in mRNA transcripts of the gene. HRPT2 gene is a tumor suppressor that is implicated in the autosomal dominant hyperparathyroidism-jaw-tumor familial cancer syndrome (HPT-JT) (see below). Parafibromin protein is a product of HRPT2 that is believed to be involved in cell cycle regulation by interfering with cyclin D1 expression [25]. It has also been shown that COF lacks GNAS gene mutation characteristic of fibrous dysplasia [26, 27].
Differential Diagnosis (COF vs. FD)
COF is a radiographically well defined lesion of the jaws affecting predominantly female patients in the third and fourth decades of life. Unlike fibrous dysplasia, COF can be shelled out or curetted from the surrounding bone with relative ease. FD can affect any part of the craniofacial skeleton predominantly in children and young adults. FD has ill-defined borders that blend with the surrounding bone.
Treatment and Prognosis
COF is a slow growing benign neoplasm. It can be surgically excised conservatively by curettage or enucleation, with no recurrences in most cases. Untreated tumors can attain a massive size and may require en-block resection. Sarcomatous transformation has not been documented [4–6, 23].
Juvenile Ossifying Fibromas (JOF)
The term JOF has been used in the literature to describe two clinically and pathologically distinct entities: trabecular juvenile ossifying fibroma (TrJOF) and psammomatoid juvenile ossifying fibroma (PsJOF). These tumors have also been referred to as juvenile active ossifying fibroma and juvenile aggressive ossifying fibroma [28–30].
Trabecular Juvenile Ossifying Fibroma
TrJOF predominantly affects children and adolescents. The mean age range is 8.5–12 years [29]. Males and females are equally affected. The maxilla and mandible are the most common sites. The maxilla is more frequent than the mandible. Extragnathic occurrence is extremely rare [28–31]. Clinically, the lesion is characterized by progressive and sometimes rapid expansion of the affected bone. In the maxilla, obstruction of the nasal passages and epistaxis may occur.
Radiographic Features
The tumor is expansive and fairly well demarcated, with cortical thinning and possible perforation. The lesion shows various degrees of radiolucency or opacity depending on the amount of calcified tissue produced (Fig. 3). A ground-glass as well as multilocular appearance has been described [29–31].
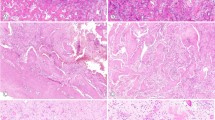
a CT scan of trabecular juvenile ossifying fibroma of the maxilla. The lesion is expansive with ground glass appearance and corticated border; b trabecular juvenile ossifying fibroma showing cellular osteoid trabeculae in spindle cell rich stroma (×400); c aggregates of osteoclast-like giant cells (×400)
Pathologic Features
Grossly the tumor is described as yellowish white and gritty. Microscopically it is unencapsulated and shows infiltrative growth pattern into the surrounding bone. It has a characteristic loose architecture with hypercellular stroma composed of spindle cells with little collagen production. Osteoid develops directly from the fibrous stroma and forms long slender strands that have been likened to paint brush strokes. Irregular mineralization takes place at the center of the strands resulting in the production of immature bone trabeculae that are devoid of osteoblastic rimming and do not show evidence of maturation (Fig. 3). Aggregates of osteoclastic giant cells are typically found in the stroma (Fig. 3). Occasional mitosis may be observed. Aneurysmal bone cyst formation has been reported in some cases [28–31].
Treatment and Prognosis
Multiple recurrences have been reported following conservative excision [29]. Eventual complete cure could be achieved without resorting to radical excision. Malignant transformation has not been reported.
Psammomatoid Juvenile Ossifying Fibroma
PsJOF affects predominantly the extragnathic craniofacial bones. The lesions are particularly centered on periorbital frontal and ethmoid bones [29]. The average age of incidence varied in different studies from 16 to 33 years. However, the age range is wide and cases have been reported in patients as young as 3 months and as old as 72 years [5, 29, 31], and there is no gender predilection. Clinically, PsJOF manifests as a bony expansion that may involve the orbit or nasal bones and sinuses. Expansion of the tumor may result in proptosis, visual symptoms, and nasal obstruction.
Radiographic Features
Radiographically, PsJOF presents as a round well defined osteolytic lesion. Sclerotic changes may impart it with a ground glass appearance (Fig. 7) [29, 32, 33]. The lesion may range in size from 2 to 8 cm in diameter and may appear multiloculated on CT scans. Areas of low density due to cystic changes may be noted [29, 34].
Pathologic Features
Grossly, the tumor is yellowish white and gritty. On microscopic examination, the tumor is unencapsulated and is significant for multiple small uniform ossicles (psammomatoid bodies) imbedded in cellular stroma composed of spindle and stellate shaped cells (Fig. 4) [5, 28, 29]. The psammomatoid bodies are basophilic and bear some resemblance to dental cementum. At the periphery of the lesion these structures may coalesce and form bone trabeculae. Cystic degeneration and aneurysmal bone cyst (ABC) formation may occur. It is believed by the author that reported cases of sudden aggressive growth in both TrJOF and PsJOF may be due to ABC formation.
Genetics
A study of 3 cases of “cemento-ossifying fibroma of the orbit”, most likely PsJOF, as evidenced by review of published representative histopathologic sections, demonstrated non random chromosome break points at Xq26 and 2q33 resulting in (X;2) translocations [41]. In a very recent study, a group of French researchers using qPCR identified MDM2 gene amplification in 9 of 13 (69 %) cases of Juvenile ossifying fibroma, both trabecular and psammomatoid types [42]. The prevalence of MDM2 amplification in juvenile ossifying fibroma was significantly higher than that observed in craniofacial fibrous dysplasia (p < 0.004) and conventional gnathic ossifying fibroma (p < 0.001). MDM2 amplification was not associated with immunohistochemical overexpression of MDM2 protein. In contrast, in a control group of low grade osteosarcoma and liposarcoma the MDM2 amplification was associated with overexpression in all 15 cases.
Diagnosis and Differential Diagnosis
Confusion in the literature between TrJOF and PsJOF is mainly due to the common use of the term JOF to describe these two clinically and pathologically distinct lesions. Microscopically the former is characterized by trabecular bone formation while in the latter the produced bone shows a characteristic psammomatoid pattern. PsJOF has a definite sit predilection to the periorbital bones, whereas TrJOF primarily affects the jaws. The latter also has a younger average age of incidence.
Treatment and Prognosis
Recurrence, even after definitive surgery, has been reported and multiple recurrences were observed after long follow up periods [5, 29, 35]. Malignant transformation has not been reported.
Cemento-Osseous Dysplasia
Cemento-osseous dysplasias are non-neoplastic fibro-osseous lesions that affect the tooth-bearing areas of the jaws. Two main types are recognized: localized and generalized, the former includes periapical cemento-osseous dysplasia (PCOD) and focal cemento-osseous dysplasia (FCOD), the latter is termed florid cemento-osseous dysplasia (FlCOD) which denotes an extensive process with multifocal involvement of the jaws by lesional tissue with the same microscopic appearance as is encountered with PCOD and FCOD. Ideally these lesions should be identified clinically and radiographically without the need for a biopsy. Indeed, surgical intervention is contraindicated, because a simple biopsy, particularly in the case of FlCOD can result in persistent local infection and pain with complicated clinical course [4, 6].
Periapical and Focal Cemento-Osseous Dysplasia
PCOD is a reasonably well-defined clinical-radiological entity, predominantly involving the apical areas of vital mandibular incisors. FCOD affects the tooth-bearing areas of the posterior jaws, particularly in sites of former extraction [36]. The two lesions share common radiographic and pathologic features. PCOD, also known as periapical cemental dysplasia and periapical cementoma is a relatively common presumably dysplastic disorder. It typically affects the periapical area of the mandibular anterior teeth in middle aged black female patients. The lesions are asymptomatic and are usually discovered on routine radiographic examination.
Radiographic Features
The early lesions present as small periapical radiolucencies affecting the mandibular anterior teeth in the case of PCOD. A similar but isolated lesion affecting the posterior quadrant of the jaws, especially the mandible, is seen in the case of FCOD. Continued mineralization results in heavily calcified radio-opaque areas (Fig. 5) [4, 6].
The Microscopic features of PCOD and FCOD are analogous to those of FlCOD and will be discussed together with that entity.
Florid Cemento-Osseous Dysplasia
This condition usually presents in middle age or older black women. It is asymptomatic and typically discovered incidentally on routine radiographic examination [4, 6, 37, 38]. In most instances, the disease affects the mandible bilaterally and may or may not show concomitant maxillary involvement. Most of the patients with FlCOD are more than 45 years old, although it has been reported in younger patients.
Radiographic Features
A characteristic radiographic appearance is extensive sclerotic areas surrounded by radiolucent zone and involving the posterior quadrants of both mandible and maxilla bilaterally, in a symmetric fashion (Fig. 5).
Pathologic Features
Both localized cemento-osseous dysplasia and FlCOD have analogous microscopic features. The lesions are composed of fibrous stroma containing foci of cementum, osteoid, or bone (Fig. 6). More advanced lesions show increased mineralization and in the case of FlCOD large, dense, hypocellular sclerotic masses which may form. Development of simple bone cysts in FlCOD is known to occur [39, 40].
Diagnosis and Differential Diagnosis
It is of importance to know that, unlike inflammatory and neoplastic lesions, COD are asymptomatic and not associated with pain or expansion of the affected area of the jaws. Jaw metastasis of some carcinomas such as those of the breast and prostate, may induce osteoblastic activity and may show radiographic features similar to COD. However, metastatic jaw lesions are usually associated with pain, looseness of teeth, and paraesthesia of the lip. A medical history of prostate or breast carcinoma should prompt a biopsy of a suspicious jaw lesion.
Treatment and Prognosis
Ideally, COD should be identified clinically and radiographically, and not subjected to surgical intervention.
Ossifying Fibromas Associated with Systemic Genetic Disorders
A group of benign fibro-osseous lesions affecting the jaws and microscopically described as ossifying fibromas or cemento-ossifying fibromas are manifestations of systemic genetic disorders. These are rare and not very well defined conditions. The following are examples that are gaining more recognition:
-
1.
Hyperparathyroidism-jaw tumor syndrome
-
2.
Familial gigantiform cementoma
-
3.
Gnathodiaphysial dysplasia/fragile bone syndrome with fibro-osseous jaw lesions
Hyperparathyroidism-Jaw Tumor Syndrome (HPT-JT)
HPT-JT is an autosomal dominant syndrome with high but incomplete penetrance and variable expression. It is characterized by primary hyperparathyroidism (PHPT) with multiple parathyroid adenomas occurring at an early age with increased risk for parathyroid carcinoma, fibro-osseous jaw lesions, and renal cysts or tumors [25, 43, 44]. The jaw tumors may be multiple and affect the mandible and maxilla [45, 46] where they have been variably described as ossifying fibroma, cementifying fibroma, and cemento-ossifying fibroma. The tumors occur during adolescence or early adulthood, and they persist and may grow after parathyroidectomy and restoration of a normal serum parathyroid hormone level [45, 47, 48].
Radiographic Features
From a number of reported cases it appears that the jaw tumors are more common in the mandible than the maxilla and may be bilateral. The tumors affect the tooth bearing areas and may extend into the mandibular ramus. They are described as expansive, lytic lesions that may be unilocular or multilocular. They may be radiolucent, radio-opaque or a combination of both features. Resorption of roots of the affected teeth is reported [44–49].
Pathologic Features
Microscopically, the lesions are well defined but unencapsulated (Fig. 7). They are identical to cemento-ossifying fibroma and are composed of hypercellular fibroblastic stroma containg variable amounts of calcifying structures that may form woven bone trabeculae or cementum-like structures [44–49].
Genetics
HPT-JT syndrome has been mapped to chromosome 1 at the q21–q31 region. The gene HRPT2 located in this region is a tumor suppressor gene encoding for parafibromin protein [25, 50]. It has been shown that over expression of parafibromin inhibits cell proliferation and blocks expression of cyclin D1, a key cell cycle regulator [25]. Mutations in the HRPT2 result in truncated, inactive protein [44].
Treatment and Prognosis
The tumors are treated surgically usually for cosmetic purposes. Recurrence is common, may be multiple, and may occur after correction of the hyperparathyroid state. No malignant transformation has been reported [46, 47, 51].
Familial Gigantiform Cementoma (FGC)
FGC is a rare form of ossifying fibroma. The tumors present as multifocal/multiquadrant expansive lesions of the jaws which can be massive and cause remarkable facial deformity. No other bones are affected. Autosomal dominant inheritance is seen among some cases whereas others are “familial”. Among the few cases that have been reported, the gene appears to have a high level of penetrance with variable expressivity. The condition has been described in families in different parts of the world including the United States, Italy, Korea, and the Philippines [52–56]. Lesions arise during childhood and progressively expand to cause facial deformity during early adult years. Sporadic cases without any heritable features have been also been reported.
Radiographic Features
Gigantiform cementomas are restricted to the jaws and may arise in two, three or all four quadrants. The lesions present as markedly expansive masses of the maxilla and mandible that are well circumscribed presenting as radiolucent areas containing radiopaque calcifications. They commonly cross the midline of the jaws [6, 54, 55] (Fig. 8).
a CT scan of the skull of a patient with familial gigantiform cementoma. Massive expansive masses of the maxilla and mandible with well circumscribed borders presenting as radiolucent areas containing radiopaque calcifications; b microscopic features of FGC are analogous to those of cemento-ossifying fibroma. Cementum-like tissue formed of hypocellular basophilic and curvilinear structures and immature bone trabeculae; c are dispersed in hypercellular fibroblastic stroma composed of monomorphic appearing spindle shaped fibroblasts and collagen fibers
Pathologic Features
The microscopic features of FGC are analogous to those of cemento-ossifying fibroma. Hypercellular fibroblastic stroma with monomorphic appearing spindle shaped fibroblasts and collagen fibers are seen. Dispersed throughout are mineralized structures of immature bone trabeculae and cementum like tissue. The latter is formed of hypocellular basophilic and curvilinear structures resembling cementicles that are normally seen in the periodontal ligament (Fig. 8). Under polarized light, Sharpy’s fibers are seen to project radially from these spheroidal deposits [6, 52–55].
Genetics
FGC is transmitted as an autosomal dominant trait that is fully penetrant but with variable expressivity [6, 52–54]. Molecular studies to characterize specific mutations are currently unavailable. Conditions that combine typical FGC phenotype and disorders of the extragnathic skeleton, particularly long bone fragility have been described under different designations. Recently the term Gnathodiaphysial dysplasia (GDD) was proposed as a name for this entity [57]. A specific mutation has been identified as causative in these cases [58] (see below). Whether or not FGC and GDD are genetically related is currently not known.
Treatment and Prognosis
Surgical management of FGC is a challenge due to rapid growth of the lesions and extensive involvement of the jaws. Simple cosmetic recontouring procedures result in recurrences, which may be multiple and occasionally at a more accelerated rate [53–55]. Extensive resection followed by massive reconstruction has been successful in some cases [54, 55].
Gnathodiaphysial Dysplasia (GDD)
Several reports of patients showing typical features gigantiform cementomas associated with extragnathic skeletal abnormalities have appeared in the literature. The bone abnormalities are variably described as osteopenia, osteogenesis imperfecta, fragile and brittle bone [57–63]. As early as 1969, Akasaka et al. [64] from Japan reported familial cases of systemic bone disease that they named Hereditary gnathodiaphysial sclerosis. The term Gnathodiaphysial dysplasia was first coined by Riminucci et al. [65], which describes cemento-ossifying fibromas of the jaws associated with multiple fractures, bowing and cortical thickening of the tubular bone. The authors documented that their cases lacked GNAS1 mutation characteristic of fibrous dysplasia.
Radiographic Features
The gnathic lesions in GDD have been variably described. In some cases the lesions are expansive radiolucent with radiopaque areas that closely resemble those seen in FGC (Fig. 8) [62, 65, 66]. They affect both maxilla and mandible bilaterally. Other cases present as multiple sclerotic areas of the tooth-bearing areas of the jaws [57, 59, 61] or as a unilateral expansive multilocular lesion [60].
Radiographic features of the extragnathic bone include osteopenia, demineralization, trabecular coarsening, diaphysial cortical thickening and bowing of the femora and tibiae [57–59, 61, 62, 65, 66].
Pathologic Features
Lesions of the jaws in GDD are analogous to those described in FGC. They are generally described as cemento-ossifying fibromas with immature bone and lobulated calcified masses in cell rich fibroblastic stroma [57, 58, 61–63, 65] (Fig. 9).
Jaw lesions in gnathodiaphysial dysplasia are analogous to those described in FGC (see Fig. 8)
Genetics
GDD is an autosomal dominant generalized skeletal syndrome. For several years, the exact cytogenetic and molecular genetics of this clinicopathologic entity remained unknown. In 2004, a novel GDD1 gene was found by Tsutsumi et al. [67] to be mutated in the original Japanese family and also in an African American family. The GDD1 gene, also known as TMEM16E or anoctamin 5 (ANO5) is mapped to a locus on chromosome 11p14.3–15.1 [57, 67]. It encodes a 913 amino-acid protein containing eight putative transmembrane-spanning domains. It is believed that cellular localization of GDD1 protein to the endoplasmic reticulum suggests a role in regulation of intracellular calcium homeostasis [67]. The high levels of GDD1 protein expression in normal cardiac and skeletal muscle tissue as well as in growth plate chondrocytes and osteoblasts in bone suggests an important role for GDD1 in the development of the musculoskeletal systems [67, 68].
Two missense mutations (C356R and C356G) in GDD1 have been identified in two GDD families. Both mutations occur at the cysteine residue at position 356 of ANO5 [67]. An additional novel missense mutation (p.Thr513Ile) has also been identified recently in a large Italian family with clinicopathologic features of GDD [58].
Treatment and Prognosis
Surgical management and prognosis of the gnathic lesions in GDD are analogous to those described for FGC. They are characterized by multiple, rapid local recurrences following cosmetic surgery.
References
Waldron CA, Giansanti JS. Benign fibro-osseous lesions of the jaws: a clinical radiologic-histologic review of sixty-five cases I. Oral Surg Oral Med Oral Pathol. 1973;35:190–201.
Waldron CA, Giansanti JS. Benign fibro-osseous lesions of the jaws: a clinical radiologic-histologic review of sixty-five cases II. Oral Surg Oral Med Oral Pathol. 1973;35:340–50.
Hamner JE III, Scofield HH, Cornyn J (1968) Benign fibro-osseous lesions of periodontal membrane origin. An analysis of 249 cases. Cancer. 1968;22:861–78.
Waldron CA. Fibro-osseous lesions of the jaws. J Oral Maxillofac Surg. 1993;51(8):828–35.
El-Mofty S. Bone lesions. In: Gnepp D, editor. Diagnostic surgical pathology of the head and neck, 2nd ed. Philadelphia: Saunders, Elsevier; 2009. p. 729–84.
Eversole R, Su L, El-Mofty S. Benign fibro-osseous lesions of the craniofacial complex: a review. Head Neck Pathol. 2008;2:177–202.
Kransdorf MJ, Moser RP Jr, Gilkey FW. Fibrous dysplasia. Radiographics. 1990;10(3):519–37.
Ishida T, Dorfman HD. Massive chondroid differentiation in fibro-osseous dysplasia of bone (fibrocartilagenous dysplasia). Am J Surg Pathol. 1993;17:924–30.
Lumbroso S, Paris F, Sultan C. McCune-Albright syndrome: molecular genetics. J Pediatr Endocrinol Metab. 2002;15(Suppl 3):875–82.
Marie PJ, de Pollak C, Chanson P, et al. Increased proliferation of osteoblastic cells expressing the activating Gs alpha mutation in monostotic and polyostotic fibrous dysplasia. Am J Pathol. 1997;150:1059–69.
Marie PJ. Cellular and molecular basis of fibrous dysplasia. Histol Histopathol. 2001;16:981–8.
Lietman SA, Ding C, Levine MA. A highly sensitive polymerase chain reaction method detects activating mutations of the GNAS gene in peripheral blood cells in McCune-Albright syndrome or isolated fibrous dysplasia. J Bone Joint Surg Am. 2005;87:2489–94.
Stompro BE, Wolf P, Haghighi P. Fibrous dysplasia of bone. Am Fam Phys. 1989;39(3):179–84.
Ricalde P, Horswell BB. Craniofacial fibrous dysplasia of the fronto-orbital region: a case series and literature review. J Oral Maxillofac Surg. 2001 Feb;59(2):157–67; discussion 67–8.
Moore AT, Buncic JR, Munro IR. Fibrous dysplasia of the orbit in childhood. Clinical features and management. Ophthalmology. 1985;92(1):12–20.
Barat M, Rybak LP, Mann JL. Fibrous dysplasia masquerading as chronic maxillary sinusitis. Ear Nose Throat J. 1989 Jan;68(1):42, 4–6.
Yabut SM Jr. Kenan S, Sissons HA, Lewis MM. Malignant transformation of fibrous dysplasia. A case report and review of the literature. Clin Orthop Relat Res. 1988;228:281–9.
Huvos A. Bone tumors: diagnosis, treatment, and prognosis. 2nd ed. Philadelphia: W B Saunders; 1991.
Ruggieri P, Sim FH, Bond JR, Unni KK. Malignancies in fibrous dysplasia. Cancer. 1994;73(5):1411–24.
Slootweg P, El-Mofty S. Ossifying Fibroma. In: Barnes L, Eveson J, Reichart P, Sidronsky D, editors. Pathology and genetics head and neck tumors. Lyon: IARC Press; 2005. p. 319–20.
Eversole LR, Leider AS, Nelson K. Ossifying fibroma: a clinicopathologic study of sixty-four cases. Oral Surg Oral Med Oral Pathol. 1985;60(5):505–11.
Eversole LR, Merrell PW, Strub D. Radiographic characteristics of central ossifying fibroma. Oral Surg Oral Med Oral Pathol. 1985;59(5):522–7.
El-Mofty SK. Cemento-ossifying fibroma and benign cementoblastoma. Semin Diagn Pathol. 1999;16(4):302–7.
Pimenta FJ, Silveria LFG, Tavares GC, Silva AC, Perdigao PF, et al. HRPT2 gene alterations in ossifying fibroma of the jaws. Oral Oncol. 2006;42:735–9.
Woodard GE. Lin L, Zhang J-H, Agarwal SK, Marx SJ, Simond FS. Parafibromin, product of the hyperparathyroidism-jaw tumor syndrome gene HRPT2, regulates cyclin D1/PRAD expression. Oncogene. 2005;24:1272–6.
Toyosawa S, Yuki M, Kishino M, Ogawa Y, Ueda T, et al. Ossifying fibroma vs fibrous dysplasia of the jaws: molecular and immunological characterization. Mod Pathol. 2007;20:389–96.
Patel MM, Wilkey JF, Abdelsayed R, D’Silva N, Malchoff C, et al. Analysis of GNAS mutations in cemento-ossyfying fibroma and cemento-osseous dysplasia. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;109:739–43.
Slootweg P, El-Mofty S. Ossifying Fibroma. In: Barnes L, Eveson J, Reichart P, Sidronsky D, editors. Pathology and genetics head and neck tumors. Lyon: IARC Press; 2005. p. 319–20.
El-Mofty S. Psammomatoid and trabecular juvenile ossifying fibroma of the craniofacial skeleton: two distinct clinicopathologic entities. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;93(3):296–304.
Slootweg PJ, Muller H. Juvenile ossifying fibroma. Report of four cases. J Craniomaxillofac Surg. 1990;18(3):125–9.
Slootweg PJ, Panders AK, Koopmans R, Nikkels PG. Juvenile ossifying fibroma. An analysis of 33 cases with emphasis on histopathological aspects. J Oral Pathol Med. 1994;23(9):385–8.
Margo CE, Weiss A, Habal MB. Psammomatoid ossifying fibroma. Arch Ophthalmol. 1986;104(9):1347–51.
Margo CE, Ragsdale BD, Perman KI, Zimmerman LE, Sweet DE. Psammomatoid (juvenile) ossifying fibroma of the orbit. Ophthalmology. 1985;92(1):150–9.
Khoury NJ, Naffaa LN, Shabb NS, Haddad MC. Juvenile ossifying fibroma: CT and MR findings. Eur Radiol. 2002;12(Suppl 3):S109–13.
Marvel JB, Marsh MA, Catlin FI. Ossifying fibroma of the mid-face and paranasal sinuses: diagnostic and therapeutic considerations. Otolaryngol Head Neck Surg. 1991;104(6):803–8.
Summerlin DJ, Tomich CE. Focal cemento-osseous dysplasia: a clinicopathologic study of 221 cases. Oral Surg Oral Med Oral Pathol. 1994;78:611–20.
Melrose RJ, Abrams AM, Mills BG. Florid osseous dysplasia. A clinical-pathologic study of thirty-four cases. Oral Surg Oral Med Oral Pathol. 1976;41(1):62–82.
El-Mofty SK. Lesions of the head and neck. In: Wick M, Humphrey P, Ritter J, editors. Pathology of pseudoneoplastic lesions. Philadelphia: Lippincott—Raven; 1997. p. 69–96.
Mupparapu M, Singer SR, Milles M, Rinaggio J. Simultaneous presentation of focal cemento-osseous dysplasia and simple bone cyst of the mandible masquerading as a multilocular radiolucency. Dentomaxillofac Radiol. 2005;34(1):39–43.
Wakasa T, Kawai N, Aiga H, Kishi K. Management of florid cemento-osseous dysplasia of the mandible producing solitary bone cyst: report of a case. J Oral Maxillofac Surg. 2002;60(7):832–5.
Sawyer JR, Tryka AF, Bell JM, et al. Nonrandom chromosome breakpoints at Xq26 and 2q33 characterize cemento-ossifying fibromas of the orbit. Cancer. 1995;76:1853–9.
Tabareau-Delalande F, Collin C, Gomez-Brouchet A, Bouvier C, Decouvelaere A-V, et al. Chromosome 12 long arm rearrangement covering MDM2 and RASAL1 is associated with aggressive craniofacial juvenile ossifying fibroma and extracranial psammomatoid fibro-osseous lesions. Mod Pathol. 2014;. doi:10.1038/modpathol.2014.80.
Shattuck T, Valimaki S, Obara T, Gaz RD, Clark OH, et al. Somatic and germ-line mutations of HRPT2 gene in sporadic parathyroid carcinoma. N Eng J Med. 2003;349:1722–9.
Iacobone M, Masi G, Barzon L, Porzionato A, Macchi V, et al. Hyperparathyroidism-jaw tumor syndrome: a report of three large kindred. Langenbecks Arch Surg. 2009;394:817–25.
Kenneth S, Pollick H. jaw lesions in familial hyperparathyroidism. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1971;31:502–10.
Rosen IB, Palmer JA. Fibro-osseous tumors of the facial skeleton in association with primary hyperparathyroidism: an endocrine syndrome r coincidence? Am J Surg. 1981;142:494–8.
Aldred MJ, Talacko AA, Savarirayan R, Murdolo V, Mills AE, et al. Dental findings in a family with hyperparathyroidism-jaw tumor syndrome and novel HPRT2 gene mutation. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101:212–8.
Szabo J, Heath B, Hill VM, Jackson CE, Zarbo RJ, et al. Hereditary hyperparathyroidism-jaw tumor syndrome; the endocrine tumor gene HRPT2 maps to chromosome 1q21-q31. Am J Hum Genet. 1995;56:944–50.
Warnakulasuriya S, Markwell BD, Williams DM. Familial hyperparathyroidism associated with cementifyingfibromas of the jaws in two siblings. Oral Surg Oral Med Oral Pathol. 1985;59:269–74.
Carlson AL, Smith CL. Primary hyperparathyroidism and jaw tumor syndrome; a novel mutation in HRPT2 gene. Endocr Pract. 2008;14:743–7.
Abdulla AG, O’Leary EM, Isorena JP, Diaz MFP, Yeh MW. Recurrent hyperparathyroidism and novel nonsense mutation in a patient with hyperparathyroidism-jaw tumor syndrome. Endocr Pract. 2013;19:e134–7.
Agazzi C, Belloni L. Gli odontomi duri dei mascellari contributo clinico-rontgenologico e anatomo-microscopico con particolare riguardo alle formle ad estensione e alla comparsa familiare. Arch Ital Otol. 1953;64(suppl 16):3–102.
Young SK, Markowitz R, Sullivan S, Seal TW, Hirsci R. Familial gigantiform cementoma; classification and presentation of a large pedigree. Oral Surg Oral Med Oral Pathol. 1989;68:740–747.
Abdelsayed RA, Eversole LR, Singh BS, Scarbrough FE. Gigantiform cementoma; clinicopathologic presentation of 3 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;91:438–44.
Shah S, Huh KH, Yi WJ, Heo MS, Lee SS, Choi SC. Follow up findings of recurrent gigantiform cementoma of a female child. Skeletal Radiol. 2012;41:341–6.
Finical SJ, Kane WJ, Clay RP, Bite U. Familial Gigantiform cementoma. Plastic Recon Surg. 1999;103:949–54.
Tsutsumi S, Kamata N, Maruoka Y, Ando M, Tezuka O, et al. Autosomal dominant Gnathodiaphyseal dysplasia maps to chromosome11p14.3-15.1. J Bone Miner Res. 2003;18:413–8.
Marconi C, Binello PB, Badiali G, Caci E, Cusano R, et al. A novel missense mutation in ANO5/TMEM516E is causative for Gnathodiaphyseal dysplasia in a large Italian pedigree. Eur J Hum Genet. 2013;21:613–9.
Levin LS, Wright JM, Byrd DL, Greenway G, Dorst JP, et al. Osteogenesis imperfeacta with unusual skeletal lesions: report of three families. Amer J Med Genet. 1985;21:257–69.
Shibahara T, Noma H, Yamane G-Y, Hashimoto S. Large cementifying fibroma in a patient with osteogenesis imperfecta. J Oral Maxillofac Surg. 1996;54:1016–9.
Nishimora G, Haga N, Ikeuchi S, Yamaguchi T, Aoki K, Yamato M. Fragil bone syndrome associated with craniognathic fibro-osseous lesions and abnormal modeling of the tubular bones; report of two cases with review of literature. Skeletal Radiol. 1996;25:717–22.
Moshref M, Khojastch A, Kazemi B, Roudsari MV, Varshowaz M, Eslami B. Autosomal dominant gigantiform cementoma associated with bone fractures. Am J Med Genet Part A. 2008;146A:644–8.
Rossbach HC, Leston D, lacson A, Ruas E, Salazar P. Familial gigantiform cementoma with brittle bone disease, pathologic fractures, and osteosarcoma: a possible explanation of an ancient mystery. Pediatr Blood Cancer 2005;44:390–6.
Akaska Y, Nakajima T, Koyama K, Furuya K, Misuka Y. Familial cases of new systemic bone disease, hereditary gnathodiaphysial sclerosis. Nippon Seigeka Gakkai Zasshi. 1996;43:381–94.
Riminucci M, Collins MT, Corsi A, Boyde A, Murphey MD, et al. Gnathodiaphyseal dysplasia; a syndrome of fibro-osseous lesions of the jaw bones, bone fragility, and long bone bowing. J Bone Miner Res. 2001;16:1710–8.
Ahluwalia J, Ly JQ, Norman E, Costello RF Jr, Beall DP. Gnathodiaphyseal dysplasia. Clin Imag. 2007; 31:67–9.
Tsutsumi S, Kamata N, Vokes TJ, Maruoka Y, Nakakuki K, et al. The novel gene encoding transmembrane protein is mutated in gnathodiaphyseal dysplasia (GDD). Am J Hum Genet. 2004;74:1255–61.
Mizuta K, Tsutsumi S, Inoue H, Sakamoto Y, Miyataki K, et al. Molecular characterization of GDD1/TMEM16E, the gene product responsible for autosomal dominant gnathodiaphyeal dysplasia. BBRC. 2007;357:126–32.
Acknowledgments
The national and international community of Oral and Head and Neck pathologists are particularly grateful for Lewis Roy Eversole role in founding this Journal and for acting as its first co-Editor-In-Chief.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is dedicated to Lewis Roy Eversole DDS, MSD, MA: a generous teacher, dedicated scholar and esteemed colleague and friend. His vast and seminal contributions to the field of Oral and Maxillofacial Pathology and particularly to the fascinating subject of fibro-osseous lesions of the maxillofacial skeleton are acknowledged.
Rights and permissions
About this article
Cite this article
El-Mofty, S.K. Fibro-Osseous Lesions of the Craniofacial Skeleton: An Update. Head and Neck Pathol 8, 432–444 (2014). https://doi.org/10.1007/s12105-014-0590-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12105-014-0590-0