Abstract
Objective
To evaluate correlation of transcutaneous bilirubin (TcB) measured at different body sites with serum total bilirubin (TSB) in early preterm infants.
Methods
This hospital based prospective comparative study was carried out in the Department of Pediatrics, SMS Medical College, Jaipur between April 2015 to March 2016. Early preterm infants with gestational age ≤ 34 weeks in whom clinical jaundice was significant mandating TSB measurement were included in the study. Study subjects who met the inclusion criteria were chosen consecutively. Neonates in whom phototherapy was already initiated and those with poor perfusion (capillary refill time > 3 s) were excluded from the study. All the measurements were carried out within first postnatal week. Transcutaneous bilirubin was measured from three sites: forehead, sternum and interscapular region and within 15 min of TcB measurement, blood samples were taken and serum bilirubin level was calculated.
Results
Correlation coefficients of transcutaneous bilirubin measured from forehead, sternum and interscapular sites were 0.82, 0.84 and 0.86 respectively. TcB measured from all the three sites correlated significantly with serum bilirubin (p < 0.001), but the correlation was best at interscapular site. Sensitivity, specificity and false negative rates were calculated with respect to starting phototherapy. Interscapular site had the highest sensitivity and lowest false negative rate (87.6 and 12.4% respectively) as compared to forehead (79.2 and 20.8% respectively) and sternum (87.1 and 12.9% respectively).
Conclusions
Transcutaneous bilirubin measurement is an acceptable method for identification of hyperbilirubinemia requiring treatment in early preterm newborns. The authors recommend interscapular region as a reliable site in infants of gestational age ≤34 wk for measuring transcutaneous bilirubin.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Jaundice is one of the most common conditions requiring medical attention in newborn infants. Approximately 60% of term and 80% of preterm babies develop jaundice in the first week of life [1]. Severe neonatal hyperbilirubinemia has been estimated to occur in up to 10% of newborns [2]. Usually, hyperbilirubinemia is a benign condition, but high levels of serum bilirubin for prolonged time period may permanently damage the globus pallidus, subthalamic nuclei, hippocampus, and oculomotor nucleus and other structures of the central nervous system causing kernicterus in the infant [3]. Preterm neonates are at increased risk for bilirubin encephalopathy and kernicterus as compared to term neonates, as a result of exaggerated neonatal red cell, hepatic, and gastrointestinal immaturity. The postnatal maturation of hepatic bilirubin uptake and conjugation may also be slower in premature infants. In addition, a delay in the initiation of enteral feedings so common in the clinical management of sick premature newborns may limit intestinal flow and bacterial colonisation resulting in further enhancement of bilirubin enterohepatic circulation. These developmental and clinical phenomena contribute to the greater degree and duration of neonatal jaundice in premature infants [4]. To prevent these complications and to do appropriate management such as phototherapy or blood exchange as soon as possible, all susceptible neonates with jaundice are checked for serum level of bilirubin.
Serum bilirubin estimation is an invasive method which requires drawing blood, and is also inconvenient because of technical difficulties in venous puncture, discomfort, pain, delay in results and parental stress; so it is important to reduce the number of draws and minimize the amount of blood the newborn loses due to blood draws [5,6,7].
Transcutaneous bilirubinometry (TcB) was originally developed as a potential replacement for invasive blood sampling. Earlier studies have obtained good correlation of TcB measurement, in term and late preterm babies, obtained from forehead and sternum as most common sites. The use of point-of-care TcB monitoring in early preterm neonates might enhance early detection of hyperbilirubinemia in this vulnerable population if these values correlate well with serum bilirubin values [8]. Interscapular site was also included in the present study considering the fact that unconjugated bilirubin is lipophilic and the interscapular site is among the earliest sites for fat deposition in the fetus [9].
Material and Methods
This hospital based prospective comparative study was carried out on patients admitted in the Department of Pediatrics, SMS Medical College, Jaipur between April 2015 to March 2016. Ethical clearance was obtained from institutional ethics committee before undertaking the study. Early preterm infants with gestational age ≤ 34 wk in whom clinical jaundice was significant mandating TSB measurement were included in the study. Study subjects who met the inclusion criteria were chosen consecutively. Neonates in whom phototherapy was already initiated and those with poor perfusion (capillary refill time > 3 s) were excluded from the study. Informed consent was obtained from the parents. All the measurements were carried out within first postnatal week. The gestational age of the neonates was determined by last menstrual period (LMP) if known, by antenatal USG or by Ballard method. Sample size for positive and negative predictive value, assuming TcB had a sensitivity of 80% in predicting the need to start phototherapy was generated. The sample size needed to demonstrate this with a power of 90% was 228. Transcutaneous bilirubin was measured from three sites: forehead, sternum and interscapular region using JM-103 bilirubinometer in accordance with the manufacturer instructions. An average of three consecutive readings from these sites were taken for evaluation. Within 15 min of measuring TcB, 0.5 ml of blood was collected via peripheral vein using aseptic technique, and sent to the laboratory promptly. The level of total serum bilirubin was determined by the diazo method. The decision to start phototherapy was based on TSB values according to guidelines mentioned in Manual of Neonatal Care, J. P. Cloherty 7th edition [10].
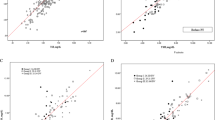
Age, sex, gestational age and anthropometry were recorded and mean, median and standard deviation was calculated. The correlation coefficient was then computed, a scatter diagram for TcB from different sites was plotted against TSB (Fig. 1), and absolute difference between TcB and TSB was computed.
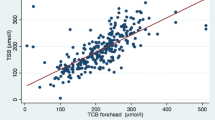
The sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV) and false positive rate for starting of phototherapy was calculated. Receiver operating characteristic (ROC) curve was generated and area under the curve was computed utilising the requirement of phototherapy according to TSB levels obtained.
Results
Two hundred twenty eight early preterm infants (gestational age ≤ 34 wk) were included in the present study. Their demographic characteristics are summarized in Table 1.
In 33(14%) patients, bilirubin level was measured within 24 h of birth, in 54(24%) patients, it was measured between 24 and 48 h and in rest 141(62%), it was measured after 48 h. Mean hours after birth at which serum bilirubin was calculated was 61.3±31.6.
Serum bilirubin in the study participants ranged from 4.4 mg/dL to 21.7 mg/dL. Median was 12.2 mg/dL. Mean±SD was 13±3.3 mg/dL. Out of 228 patients, 48(21%) had serum bilirubin <10 mg/dL, 131(57%) had serum bilirubin between 10 and 15 mg/dL and 49(22%) had serum bilirubin >15 mg/dL.
Correlation coefficients of transcutaneous bilirubin measured from forehead, sternum and interscapular sites were 0.82, 0.84 and 0.86 respectively. Transcutaneous bilirubin measured from all the three sites correlated significantly with serum bilirubin (p < 0.001), but the correlation was best at interscapular site. Differences between TSB and TcB values for forehead, sternum and interscapular site were − 5 to +6.3 mg/dL, −3.6 to +5.8 mg/dL and − 4.3 to +5.4 mg/dL respectively.
When patients were divided into two groups based on birth weight ≤ 1500 g and > 1500 g and correlation of TcB and TSB was calculated in each group, correlation was significant from all three sites in both groups (p < 0.001). Correlation of TcB obtained from forehead and sternum was better in >1500 g birth weight group as compared to ≤1500g group (0.84 and 0.85 vs. 0.76 and 0.81 respectively). At interscapular site, correlation was highest and similar in both groups (0.87 vs. 0.85).
With respect to starting phototherapy, sensitivity, specificity, PPV, NPV and false negative rates were calculated. Interscapular site had highest sensitivity and NPV and lowest false negative rate as compared to forehead and sternum (Table 2).
ROC curve was generated (Fig. 2) and area under the curve was calculated. Area under the curve for forehead, sternum and interscapular sites was 0.780, 0.770 and 0.781 respectively, which was comparable, though it was highest for interscapular site.
Discussion
Early diagnosis and management of neonatal jaundice in preterm infants is a challenge for physicians because of its potential to cause permanent encephalopathy. Immediate, accurate and painless evaluation of neonatal jaundice is highly desirable. Transcutaneous bilirubin measurement is a potentially useful method to achieve this goal. The authors attempted to calculate correlation of serum bilirubin levels and transcutaneous bilirubin measurements taken from forehead, sternum and interscapular site. They also assessed the validity of transcutaneous bilirubin measurement as a diagnostic tool to start phototherapy in early preterm infants.
The results of present study demonstrated a statistically significant correlation between the TcB values and TSB levels. The correlation coefficient of forehead TcB of 0.82 (p < 0.001) found in index study was higher than that described by other studies (Knüpfer et al. [11]: 0.73; De Luca et al. [12]: 0.79; Sajjadan et al. [13]: 0.56), but was lower as compared to findings of Yaser et al. [14] (r = 0.90). The discrepancy in correlation of forehead and total serum bilirubin found in different studies may be due to the fact that the forehead is continuously exposed to ambient light and has excessive hair, hence results vary from infant to infant. Measuring TcB over sternum seems to be also suitable for hyperbilirubinemia screening. The correlation coefficient of sternum TcB of 0.84 (p < 0.001) in present study was comparable to findings of other studies by Tan et al. [15] (r = 0.82); Szabo et al. [16] (r = 0.87); Schmidt et al. [17] (r = 0.79–0.92).
The interscapular site was also included in this study besides two commoner sites: forehead and sternum. There were two main reasons for including this site in present study: firstly, it is usually shielded from ambient light and secondly the interscapular area is one of the earliest sites of fat deposition in a newborn [9]. The correlation coefficient of interscapular TcB was 0.86 (p < 0.001). Previously, only one study by Yaser et al. [14] has evaluated this site for preterm neonates. The correlation between TSB and TcB obtained from interscapular site in their study was similar to present study (r = 0.86).
In the present study, authors also attempted to find out whether the correlation between TcB and TSB is affected by birth weight. For this, when they divided patients into two groups based on birth weight ≤ 1500 g and > 1500 g and correlation of TcB and TSB was calculated, significant correlation was found from all three sites in both groups (p < 0.001). Also, correlation of TcB obtained from forehead and sternum was better in >1500 g birth weight group as compared to ≤1500g birth weight group. At interscapular site, however, correlation was almost similar in both groups and it was better than forehead and sternum in less than ≤1500g group. So, authors concluded that interscapular site may be better for measuring bilirubin levels in both groups, and particularly in ≤1500g group. Karolyi et al. [18] studied correlation of TcB from sternum and TSB among neonates with birthweight <1500 g and they found this correlation to be 0.68 (p < 0.001). Kurokawa et al. [19] assessed the accuracy of transcutaneous bilirubin (TcB) measurements at 5 different body sites in Japanese very low birthweight (VLBW) infants and they found that TcB significantly correlated with TSB., but they did not compare it with neonates more than 1500 g. Baidee et al. [20] found that the TSB – TcB correlation coefficient increased with increasing gestational age and birth weight, which is similar to present study.
When authors compared the difference between TSB and TcBs’ from forehead and sternum, 66 (29%) of forehead and 45 (19.7%) of sternum TcB measurements overestimated while 15 (6.6%) of forehead and 18 (8%) of sternum TcB measurements underestimated TSB by >2 mg/dL. Similar to findings from present study, other studies using different transcutaneous bilirubinometers have also reported wide differences between TSB and TcBs’ measured over forehead and sternum (Knüpfer et al. [11], Schmidt et al. [17], De Luca et al. [12], Willems et al. [21], Yaser et al. [14]). The reason for this is not clear but it might have to do with light exposure to the forehead and scarcity of subcutaneous fat in the sternal area. At the interscapular site, in 50 (22%) patients, TcB overestimated while in 9 (4%) it underestimated TSB by >2 mg/dl.
The sensitivity of forehead transcutaneous bilirubin in identifying study participants in need of phototherapy in present study was 79.2% which is lesser than Knüpfer et al. [11] who found a sensitivity of 86.8% but similar to Yaser et al. [14] who found a sensitivity of 80.3%.
Yaser et al. [14] looked at sensitivity of the sternum transcutaneous bilirubin in determining need to initiate phototherapy and found this value to be 69.7%. In the present study, however, authors found better sensitivity at sternum (87.1%).
In the present study, the interscapular TcB had the highest sensitivity in identifying study participants in need of phototherapy (87.6%) and it wrongly labeled 12.4% of those in need of phototherapy. As compared to findings of Yaser et al. [14], who obtained 93.9% sensitivity at this site, the present values were lower, though comparable. The difference might be because of ethnic and racial variation.
The authors thus conclude that transcutaneous bilirubin measurement is an acceptable method for identification of hyperbilirubinemia requiring treatment in early preterm newborns. It can reduce the number of blood samplings, reducing neonatal and parental distress and medical care cost. Interscapular site had the highest sensitivity and lowest false negative rate, so authors recommend transcutaneous bilirubin measurements over interscapular region in infants of gestational age ≤34 wk as a reliable and accurate neonatal hyperbilirubinemia assessment test.
References
NICE Clinical Guidelines, No. 98. National Collaborating Centre for Women's and Children's Health (UK). London: RCOG Press; 2010.
Bhutani VK, Johnson L, Sivieri EM. Predictive ability of predischarge hour specific serum bilirubin for subsequent significant hyperbilirubinemia in healthy term and new-term newborns. Pediatrics. 1999;103:6–14.
Ip S, Chung M, Kulig J, et al; American Academy of Pediatrics Subcommittee on Hyperbilirubinemia. An evidence-based review of important issues concerning neonatal hyperbilirubinemia Pediatrics 2004;114:e130–53.
Cashore WJ. Bilirubin and jaundice in the micropremie. Clin Perinatol. 2000;27:171–9.
Facchini FP. Avaliação da variabilidade da dosagem transcutânea de bilirrubina pelo Bilicheck em neonatos. Rev Paul Pediatria. 2006;24:149–54.
Boo NY, Ishak S. Prediction of severe hyperbilirubinaemia using the Bilicheck transcutaneous bilirubinometer. J Paediatr Child Health. 2007;43:297–302.
Elias LS, Guinsburg R, Peres CA, Balda RC, Santos AM. Disagreement between parents and health professionals regarding pain intensity in critically ill neonates. J Pediatr. 2008;84:35–40.
Stillova L, Matasova K, Zibolen M, Stilla J, Kolarovszka H. Transcutaneous bilirubinometry in preterm neonates. Indian Pediatr. 2009;46:405–8.
Poissonnet CM, Burdi AR, Garn SM. The chronology of adipose tissue appearance and distribution in the human fetus. Early Hum Dev. 1984;10:1–11.
Cloherty JP, Eichenwald EC, Hansen AR, Stark AR. Manual of Neonatal Care, 7th ed. Philadelphia: Lippincott Williams & Wilkins; 2012. p. 325.
Knüpfer M, Pulzer F, Braun L, Heilmann A, Robel-Tillig E, Vogtmann C. Transcutaneous bilirubinometry in preterm infants. Acta Paediatr. 2001;90:899–903.
De Luca D, Zecca E, de Turris P, Barbato G, Marras M, Romagnoli C. Using BiliCheck for preterm neonates in a sub-intensive unit: diagnostic usefulness and suitability. Early Hum Dev. 2007;83:313–7.
Sajjadian N, Shajari H, Saalehi Z, Esphahani F, Alizadeh Taheri P. Transcutaneous bilirubin measurement in preterm neonates. Acta Med Iran. 2012;50:765–70.
Yaser A, Tooke L, Rhoda N. Interscapular site for transcutaneous bilirubin measurement in preterm infants: a better and safer screening site. J Perinatol. 2014;34:209–12.
Tan KL, Mylvaganam A. Transcutaneous bilirubinometry in preterm very low birthweight infants. Acta Paediatr Scand. 1988;77:796–801.
Szabo P, Wolf M, Bucher HU, Haensse D, Fauchère JC, Arlettaz R. Assessment of jaundice in preterm neonates: comparison between clinical assessment, two transcutaneous bilirubinometers and serum bilirubin values. Acta Paediatr. 2004;93:1491–5.
Schmidt ET, Wheeler CA, Jackson GL, Engle WD. Evaluation of transcutaneous bilirubinometry in preterm neonates. J Perinatol. 2009;29:564–9.
Karolyi L, Pohlandt F, Muche R, Franz AR, Mihatsch WA. Transcutaneous bilirubinometry in very low birthweight infants. Acta Paediatr. 2004;93:941–4.
Kurokawa D, Nakamura H, Yokota T, et al. Screening for hyperbilirubinemia in Japanese very low birthweight infants using transcutaneous bilirubinometry. J Pediatr. 2016;168:77–81.e1.
Badiee Z, Mohammadizadeh M, Shamee M. Diagnostic usefulness of transcutaneous bilirubinometry in very preterm newborns. Int J Prevent Med. 2012;3:262–5.
Willems WA, van den Berg LM, de Wit H, Molendijk A. Transcutaneous bilirubinometry with the Bilicheck in very premature newborns. J Matern Fetal Neonatal Med. 2004;16:209–14.
Acknowledgements
The authors acknowledge the contributions of their respective family members and hard working team of doctors and supporting staff of SMS Medical College and associated hospitals for supporting and encouraging them throughout in every possible way.
Author information
Authors and Affiliations
Contributions
All authors have contributed in designing the study, developing the methodology, collecting the data, performing the analysis, and writing the manuscript. KG will act as guarantor for this paper.
Corresponding author
Ethics declarations
Conflict of Interest
None.
Rights and permissions
About this article
Cite this article
Agrawal, G., Garg, K., Sitaraman, S. et al. Comparison of Diagnostic Accuracy of Different Sites for Transcutaneous Bilirubin Measurement in Early Preterm Infants. Indian J Pediatr 86, 32–37 (2019). https://doi.org/10.1007/s12098-018-2739-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12098-018-2739-4