Abstract
Objective
To investigate gentamicin pharmacokinetics in neonates with moderate-to-severe hypoxic-ischemic encephalopathy (HIE) who underwent therapeutic hypothermia (TH).
Methods
Data were collected retrospectively from infants admitted between January 2007 and February 2011. Gentamicin was given at 2.5 mg/kg/dose q12h intravenously. Infants not eligible for TH underwent therapeutic normothermia (TN). After reviewing the data which showed >85 % of infants undergoing TH had gentamicin trough concentration >2 µg/ml at steady state, the gentamicin level monitoring protocol was modified since March 2011.
Results
In the initial retrospective study, 15 TN infants were compared with 19 TH infants. There was significant difference in median gentamicin half-life (7.01 vs. 9.57 h). A higher proportion of infants in the TH group required dosage adjustment (8/15 vs. 17/19). After March 2011, gentamicin level taken 12-h post 1st dose was measured routinely and 18/22 infants had trough gentamicin levels >2 µg/ml. Their dosing intervals were extended to Q18h or beyond.
Conclusions
Infants with moderate-to-severe HIE who undergo TH may exhibit changes in the pharmacokinetic properties of gentamicin compared to infants who undergo TN. By measuring gentamicin level at 12-h after the first dose of 2.5 mg/kg/dose, appropriate dosing interval can be determined and the duration of exposure to toxic gentamicin level can be reduced.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Based on a better understanding of the pathogenesis of tissue damage following perinatal hypoxic-ischemia from the past 15 years’ research, modest brain cooling has been used to attenuate the cascade of events that contributes to brain injury. Large randomized controlled trials have demonstrated the benefits of therapeutic hypothermia (TH) in newborns with moderate to severe hypoxic-ischemic encephalopathy (HIE) after perinatal asphyxia [1–4]. However, knowledge on TH effects on other physiological functions, more specifically its effects on drug elimination, is limited.
Gentamicin has been one of the most commonly prescribed aminoglycosides for the treatment of neonates with suspected or documented early onset sepsis because of its broad spectrum of activity and extensive experience with its use [5]. Potential side effects include nephrotoxicity and ototoxicity [5–9]. Previous studies have evaluated extended-interval gentamicin dosing in neonates [10–14]. A recent meta-analysis had shown that therapeutic serum concentrations are achieved more often with extended interval dosing than with the traditional dosing, but there was no significant difference in clinical cure rate or toxicity [15].
Aminoglycosides are excreted unchanged by kidneys, with less than 1 % eliminated in feces. Compared to adults, glomerular filtration rate (GFR) is lower in newborns and is significantly lowered during the immediate post-asphyxial stage [16, 17] . In a retrospective clinical study, using a once daily gentamicin dosing protocol (4–5 mg/kg/dose), serum gentamicin concentrations in HIE infants undergoing TH were not significantly different from TN [18]. However, other studies revealed reduced gentamicin clearance in this group of infants [19, 20].
The aims of the present study were (i) to characterize the pharmacokinetic properties of gentamicin in neonates with HIE who underwent TN and TH, and (ii) to evaluate the impact of revised gentamicin level monitoring regimes on minimizing potential toxic drug exposure in these vulnerable infants.
Material and Methods
Data were collected retrospectively from infants admitted to the Level III Neonatal Intensive Care Unit at Children’s and Women’s Health Centre in Vancouver, Canada between January 2007 and February 2011. Eligible infants had moderate-to-severe HIE (Sarnat stage 2 or 3) and participated in the Infant Cooling Evaluation (ICE) study or fulfilled the clinical criteria for TH, as standard care, after 2008. The inclusion criteria for TH included: (i) gestational age ≥ 35 wk, (ii) moderate or severe encephalopathy as defined by the presence of seizures or the presence of signs in at least three of six categories defined in the Abbreviated Encephalopathy Table, and (iii) evidence of perinatal asphyxia by at least one of the following: (a) 5-min Apgar score of <5, (b) ongoing ventilation at 10 min of age, (c) pH < 7.00, base deficit >12 or lactate >5 mmol/L in cord arterial or arterial/venous/capillary gases within the 60 min of birth (d) within 6 h (before 2009) or 8 h of age (since 2009). Infants who underwent TN were infants in the control arm of the ICE study or those not eligible for TH because TH could not be started within 6 h (before 2009) or 8 h of age (from 2009 onwards). Blood cultures were taken and ampicillin and gentamicin were given on admission as empirical treatment for possible early-onset sepsis. Gentamicin dose was 2.5 mg/kg at 12 h intervals and infused as gentamicin 10 mg/ml (Sandoz Canada, Inc., Quebec, Canada), over 0.5 h.
Blood samples for measuring gentamicin concentrations were routinely collected within 0.5 h before and 0.5 h after the third dose. However, if impaired renal function was suspected, for pharmacokinetic analysis, two samples separated by at least 10 h were collected within a dosing interval. Gentamicin concentrations were measured using the Abbott AxSYM system, utilizing fluorescence polarization immunoassay technology (Abbott Laboratories Diagnostics Division, Abbott Park, IL, USA). Sawchuk and Zaske’s method was used to estimate the volume of distribution (Vd), elimination rate constant (Ke), half-life (t1/2), clearance (Cl), and peak concentration (Cmax) and trough concentration (Cmin) after 1st dose [21].
Basic demographic characteristics, including gestational age, birth weight, gender, 5-min Apgar score and birthplace, were extracted. Highest values of creatinine measured between 48 and 72 h of life were reported. Based on measured gentamicin trough and peak levels around the third dose which were considered as the steady state Cmax and Cmin., gentamicin t1/2, Vd, Ke, weight normalized Cl (L/h/kg), Cmax & Cmin after the first dose were calculated, and the need for dose adjustment due to elevated drug levels were recorded. Post infusion gentamicin peak level was not measured in three TH infants, therefore estimates of Vd and Cl were not available for these three infants, but their t1/2 and Ke were calculated, based on at least two measurements, separated by at least 10 h. In addition, the use of any inotropes during the first 72-h treatment period was recorded.
In the initial retrospective study from 2007 to February 2011, data revealed an unacceptable high proportion of infants undergoing TH had elevated gentamicin levels for a longer time period than those undergoing TN. The authors decided to have closer monitoring of gentamicin levels among these HIE infants. Since March 2011, blood samples for measuring gentamicin concentrations were collected at 12 h after the first dose. Based on this, if necessary, an adjusted gentamicin dose regime was recommended.
The SPSS 21.0 (SPSS Inc Chicago, IL) program was used for statistical analysis. Kruskal-Wallis test or Mann Whitney U-test (gestational age, birth weight, serum creatinine), Pearson Chi-square test or Fisher’s Exact test (outborn; HIE Stage III at initial assessment; Apgar score <5 at 5-min; gender; umbilical blood gas or first available blood gas with pH < 7; need for dosage adjustment) and Mann–Whitney U test (pharmacokinetics parameters) were used for analysis. A p-value < 0.05 was regarded as statistically significant.
Results
In the initial retrospective evaluation from 2007 to February 2011, a total of 48 infants were identified to have moderate-to-severe HIE during the study period and 14 infants were excluded (1 infant died before 6 h of age; 1 infant underwent extracorporeal membrane oxygenation; 1 infant had congenital anomalies; 11 infants had no gentamicin measurements because antibiotics were discontinued as culture results were negative at 48 h). A total of 15 infants undergoing TN and 19 infants undergoing TH were eligible for this analysis. Of the 15 patients in the TN group, 11 presented symptoms beyond the therapeutic window for cooling and one was from the control arm of ICE study. The other three were born in 2007, after ICE study, but before TH became the standard therapy.
There were no statistically significant differences in gestational age, birth weight, gender, proportion of outborn infants, proportion of infants with Apgar score less than 5 at 5-min of life, serum creatinine at 48–72 h of life and use of inotropes during the first 72-h period between groups (Table 1).
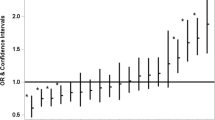
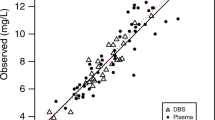
A comparison of pharmacokinetic parameters between these two groups (Tables 1 and 2) showed that there was no statistical difference in 48 to 72 h serum creatinine values but infants undergoing TH had longer gentamicin t1/2and lower weight normalized clearance (Cl/kg). Figures 1, 2 and 3 illustrate the measured and calculated pharmacokinetic parameters of each subject in both groups. The calculated serum gentamicin concentrations at 12 h post-infusion (i.e., prior to the second dose) were significantly higher in the TH group compared to the TN group. In the TH group, 17/19 subjects needed adjustments in gentamicin dosing because their measured trough levels around the third dose were >2 µg/ml, but only 8/15 subjects in the TN group required dose adjustment.
Using pharmacokinetic parameters obtained from TN and TH groups, theoretical profiles of gentamicin concentrations vs. time for different doses were calculated and are illustrated in Fig. 4. For the same dose, infants who were undergoing TH had a longer duration of gentamicin levels above 2 µg/ml compared to the TN group.
After the initial retrospective evaluation, 22 infants were identified having moderate to severe HIE and underwent TH from Mar 2011 through Feb 2012. There were no statistically significant differences in gestational age, birth weight, gender, proportion of outborn infants, proportion of infants with Apgar score <5 at 5-min of life and highest serum creatinine at 48–72 h of life, as compared to the TN and TH groups in the aforementioned patients (Table 1, Kruskal-Wallis test). The measured median trough gentamicin level 12-h after the first dose was 2.55 µg/ml (2.18, 3.30; 25th & 75th Percentiles respectively) (Fig. 3) and 19/22 (86.4 %) had gentamicin levels above 2 µg/ml, such that their dosage regimes needed to be revised from 2.5 mg/kg/dose q12h to 2.5 mg/kg/dose q18h or up to q36h. Both of these findings were similar to the results in the initial retrospective portion of the study.
Discussion
Aminoglycosides are widely used in the treatment of suspected early onset sepsis in neonates [5, 22]. It is crucial to use a suitable dosage regimen that will afford optimum serum concentrations. However, dosing with gentamicin in neonates is hampered by the inter- and intra-individual variability in the kinetic behavior of this antibiotic [23]. Aminoglycosides have a low therapeutic index; therefore, increased knowledge of their pharmacokinetics is essential [24]. Gentamicin trough concentrations greater than 2 µg/ml are associated with toxicity, and peak concentrations less than 5 µg/ml are associated with a reduced efficacy [24].
Aminoglycoside nephrotoxicity is associated with necrosis of the cells of the proximal tubule [25]. As a result, there is non-oliguric renal impairment and a reduction in glomerular filtration rate (GFR). Pre-existing renal impairment has been proposed to be one of the factors that aggravate clinical aminoglycoside toxicity [25] . Few studies found that gentamicin Cl is significantly reduced in asphyxiated neonates compared to healthy neonates and t1/2 is prolonged [19, 20, 26]. Hypothermia is associated with complex physiological changes, including a decrease in cardiac output. Studies in piglets have revealed that cardiac output and renal blood flow decrease with temperature, and renal blood flow decreases more than cardiac output [27]. The authors postulate that hypothermia, in addition to perinatal hypoxia, could lead to a further decrease in renal blood flow, glomerular filtration and consequently, excretion of gentamicin in infants with HIE who undergo TH. As a result, toxic levels of gentamicin in serum are reached, which leads to further nephrotoxicity and possible damage to the cochlea or the vestibular apparatus or both. Animal studies have yielded conflicting results regarding the effects of hypothermia after hypoxic-ischemia on the pharmacokinetics of gentamicin. These conflicting results could be related to variations in methodology such as, the degree of hypothermia, the duration of cooling and the choice of animals studied [27, 28].
The index study demonstrated that there were significant alterations in the pharmacokinetics of gentamicin during TH, including a prolongedt1/2, a significant reduction in gentamicin Cl, elevated Cmin at 12 h post 1st dose and an increased Cmax and Cmin at steady state. In authors’ initial retrospective analysis, infants undergoing TH (17/19) were more likely to have their gentamicin doses adjusted due to elevated trough levels. This is consistent with a recently published case–control study by Mark et al. that infants with HIE undergoing TH are associated with significant alterations in gentamicin pharmacokinetics [20]. In the population pharmacokinetic study focusing on full term infants diagnosed with HIE treated with TH, Frymoyer et al. also had similar findings [19]. Of interest, the reported pharmacokinetic parameters during TH by Mark et al.: t1/2 of 9.16 h, Ke of 0.08/h, clearance of 0.04 L/h/kg, and Vd of 0.46 L are very similar to present study’s findings: t1/2of 9.57 h, Ke of 0.072/h, Cl of 0.033 L/h/kg, and Vd of 0.41 L [20].
Once daily gentamicin dosing regimen of 4–5 mg/kg/dose has been adopted by many institutions. The general therapeutic goal of once daily gentamicin dosing is to achieve a peak concentration of 5–12 µg/ml and a trough concentration of <2 µg/ml. As suggested by NeoFax®, for gentamicin trough concentrations ≤1, 1.1 to 2.3 and 2.4 to 3.2 µg/ml, their corresponding suggested intervals are 24, 36 and 48 h [29]. Based on the volume of distribution and elimination half-life observed in this study, a daily dosing regimen of 4–5 mg/kg, theoretical serum gentamicin peak concentrations at steady state would be between 11 and 14 µg/ml and their levels would not reach <2 µg/ml for at least 25 h post infusion in infants receiving TH. Therefore, a reduction of dose or extension of dosing interval is required to minimize the potential for gentamicin-induced ototoxicity and nephrotoxicity. In fact, 5 mg/kg every 36-h gentamicin dosing in this group of infants has been proposed recently by Frymoyer et al. [30], while Mark et al. found that about 2/3rd of infants receiving 4 mg/kg of gentamicin required to extend their dosing interval from every 24-h to 36 or 48-h [20]. Smit et al. found about 1/3rd of the HIE infants treated with TH and a gentamicin dose of 4 mg/kg every 24-h results in permanent hearing loss and this is likely attributed to reduced gentamicin clearance [9].
Limitations of the present study are: small number of patients, retrospective nature of the study and potential differences in neonates undergoing TN and TH in the initial retrospective evaluation. Forteen out of 48 patients were not included because gentamicin was discontinued prior to measurement due to a low suspicion of sepsis. Regardless of the limitations, the fact that more than 80 % of infants undergoing TH required dosage regime revision in authors’ initial retrospective data could not be overlooked. Previously suggested dosing and monitoring (i.e., 2.5 mg/kg/dose and checking trough and peak levels of gentamicin around the third dose in Q12h regime, or 3 to 5 mg/kg/dose and monitor at 24-h in the single dose regime [18]) will result in a significant number of infants being exposed to toxic gentamicin levels >2 µg/ml for an extended period, which has shown to further increase the risk of permanent hearing impairment among the survivors of moderate or severe neonatal encephalopathy [9]. Using pharmacokinetic parameters obtained in this study, and measuring the gentamicin level at 12-h after the first dose of 2.5 mg/kg/dose can help to optimize the dosing regime in these vulnerable infants and reduce the duration of exposure to toxic gentamicin level.
Conclusions
Infants with moderate-to-severe HIE who underwent TH may exhibit changes in the pharmacokinetic properties of gentamicin compared to infants who underwent TN. A revision of the current recommended dose of gentamicin should be considered. By close monitoring of gentamicin levels in this population (measuring the level at 12-h after the first dose of 2.5 mg/kg/dose), appropriate dosing interval could be determined. Cautions should be applied with use of other renal-cleared medications during TH until further information is available.
References
Jacobs SE, Morley CJ, Inder TE, Stewart MJ, Smith KR, McNamara PJ, et al. Whole-body hypothermia for term and near-term newborns with hypoxic-ischemic encephalopathy: a randomized controlled trial. Arch Pediatr Adolesc Med. 2011;165:692–700.
Shankaran S, Laptook AR, Ehrenkranz RA, Tyson JE, McDonald SA, Donovan EF, et al. Whole-body hypothermia for neonates with hypoxic-ischemic encephalopathy. N Engl J Med. 2005;353:1574–84.
Azzopardi DV, Strohm B, Edwards AD, Dyet L, Halliday HL, Juszczak E, et al. Moderate hypothermia to treat perinatal asphyxial encephalopathy. N Engl J Med. 2009;361:1349–58.
Gluckman PD, Wyatt JS, Azzopardi D, Ballard R, Edwards AD, Ferriero DM, et al. Selective head cooling with mild systemic hypothermia after neonatal encephalopathy: multicentre randomised trial. Lancet. 2005;365:663–70.
Saez-Llorens X, McCracken GHJ. Clinical pharmacology of antibacterial agents. In: Remington JS, Klein JO, Wilson CB, Baker CJ, editors. Infectious diseases of the fetus and newborn infant. 6th ed. Philadelphia: Elsevier Saunders; 2006. p. 1223–67.
Smith CR, Lipsky JJ, Laskin OL, Hellmann DB, Mellits ED, Longstreth J, et al. Double-blind comparison of the nephrotoxicity and auditory toxicity of gentamicin and tobramycin. N Engl J Med. 1980;302:1106–9.
Moore RD, Smith CR, Lietman PS. Risk factors for the development of auditory toxicity in patients receiving aminoglycosides. J Infect Dis. 1984;149:23–30.
Brummett RE, Fox KE. Aminoglycoside-induced hearing loss in humans. Antimicrob Agents Chemother. 1989;33:797–800.
Smit E, Liu X, Gill H, Sabir H, Jary S, Thoresen M. Factors associated with permanent hearing impairment in infants treated with therapeutic hypothermia. J Pediatr. 2013;163:995–1000.
Begg EJ, Vella-Brincat JW, Robertshawe B, McMurtrie MJ, Kirkpatrick CM, Darlow B. Eight years’ experience of an extended-interval dosing protocol for gentamicin in neonates. J Antimicrob Chemother. 2009;63:1043–9.
Rao SC, Srinivasjois R, Hagan R, Ahmed M. 2011. Cochrane Database Syst Rev. 2011;11:CD005091.
Darmstadt GL, Miller-Bell M, Batra M, Law P, Law K. Extended-interval dosing of gentamicin for treatment of neonatal sepsis in developed and developing countries. J Health Popul Nutr. 2008;26:163–82.
Thureen PJ, Reiter PD, Gresores A, Stolpman NM, Kawato K, Hall DM. Once- versus twice-daily gentamicin dosing in neonates >/=34 Weeks’ gestation: cost-effectiveness analyses. Pediatrics. 1999;103:594–8.
Lundergan FS, Glasscock GF, Kim EH, Cohen RS. Once-daily gentamicin dosing in newborn infants. Pediatrics. 1999;103:1228–34.
Nestaas E, Bangstad HJ, Sandvik L, Wathne KO. Aminoglycoside extended interval dosing in neonates is safe and effective: a meta-analysis. Arch Dis Child Fetal Neonatal Ed. 2005;90:F294–300.
Bueva A, Guignard JP. Renal function in preterm neonates. Pediatr Res. 1994;36:572–7.
Svenningsen NW. Single injection polyfructosan clearance in normal and asphyxiated neonates. Acta Paediatr Scand. 1975;64:87–95.
Liu X, Borooah M, Stone J, Chakkarapani E, Thoresen M. Serum gentamicin concentrations in encephalopathic infants are not affected by therapeutic hypothermia. Pediatrics. 2009;124:310–5.
Frymoyer A, Meng L, Bonifacio SL, Verotta D, Guglielmo BJ. Gentamicin pharmacokinetics and dosing in neonates with hypoxic ischemic encephalopathy receiving hypothermia. Pharmacotherapy. 2013;33:718–26.
Mark LF, Solomon A, Northington FJ, Lee CK. Gentamicin pharmacokinetics in neonates undergoing therapeutic hypothermia. Ther Drug Monit. 2013;35:217–22.
Sawchuk RJ, Zaske DE. Pharmacokinetics of dosing regimens which utilize multiple intravenous infusions: gentamicin in burn patients. J Pharmacokinet Biopharm. 1976;4:183–95.
Edwards MS. Antibacterial therapy in pregnancy and neonates. Clin Perinatol. 1997;24:251–66.
Lanao JM, Calvo MV, Mesa JA, Martin-Suarez A, Carbajosa MT, Miguelez F, et al. Pharmacokinetic basis for the use of extended interval dosage regimens of gentamicin in neonates. J Antimicrob Chemother. 2004;54:193–8.
Pacifici GM. Clinical pharmacokinetics of aminoglycosides in the neonate: a review. Eur J Clin Pharmacol. 2009;65:419–27.
Gilbert DN, Leggett JE. Aminoglycosides. In: Mandell GL, Bennett JE, Dolin R, editors. Principles and practice of infectious diseases. 1. 7th ed. Philadelphia: Churchill Livingstone; 2010. p. 359–84.
Friedman CA, Parks BR, Rawson JE. Gentamicin disposition in asphyxiated newborns: relationship to mean arterial blood pressure and urine output. Pediatr Pharmacol (New York). 1982;2:189–97.
Koren G, Barker C, Bohn D, Kent G, Biggar WD. Influence of hypothermia on the pharmacokinetics of gentamicin and theophylline in piglets. Crit Care Med. 1985;13:844–7.
Satas S, Hoem NO, Melby K, Porter H, Lindgren CG, Whitelaw A, et al. Influence of mild hypothermia after hypoxia-ischemia on the pharmacokinetics of gentamicin in newborn pigs. Biol Neonate. 2000;77:50–7.
NeoFax®. Gentamicin Dosing Guideline: Truven Health Analytics Inc.; 2013.
Frymoyer A, Lee S, Bonifacio SL, Meng L, Lucas SS, Guglielmo BJ, et al. Every 36-h gentamicin dosing in neonates with hypoxic-ischemic encephalopathy receiving hypothermia. J Perinatol. 2013;33:778–82.
Acknowledgments
The authors would like to thank Dr. John Smyth and Ms. Ruth Milner for their expert comments.
Conflict of Interest
None.
Source of Funding
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ting, J.Y., Kwan, E., McDougal, A. et al. Pharmacokinetics of Gentamicin in Newborns with Moderate-to-Severe Hypoxic-Ischemic Encephalopathy Undergoing Therapeutic Hypothermia. Indian J Pediatr 82, 119–125 (2015). https://doi.org/10.1007/s12098-014-1527-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12098-014-1527-z