Abstract
Objective
To study the clinical profile of dengue fever and its outcome in children with application of revised WHO classification and to identify risk factors for severe dengue.
Methods
This study was a prospective observational study of children diagnosed with dengue from July 2012 through February 2013 at a tertiary care hospital in Bangalore, Karnataka (South India).
Results
Eighty one children including 55(67.9 %) boys and 26(32.1 %) girls were diagnosed with dengue. Mean age of presentation was 8 y. Vomiting (60.5 %), pain abdomen (32 %), headache (30.9 %), myalgia (23.5 %) and bleeding manifestations (16 %) were the common presenting complaints. Facial puffiness (63 %), hepatomegaly (51.9 %), ascites (48.1 %), pleural effusion (39.5 %) and petechiae (14.8 %) were noted during examination. Dengue NS1 antigen, IgM, IgG were positive in 66.7 %, 29.6 % and 18.5 % of cases respectively.
Investigations showed hemoconcentration in 72.8 %, leucopenia (34.5 %), thrombocytopenia (82.7 %), abnormal liver function test (LFT) (33.3 %). USG abdomen was suggestive of dengue in 66.7 % and gall bladder edema was noted in 53.1 %. Two patients died out of the total 81 patients with mortality rate of 2.5 %. Number of cases classified as Dengue without warning signs (D), Dengue with warning signs (DW) and Severe Dengue (SD) were 48.1 %, 27.2 % and 24.7 % respectively.
Conclusions
Children between 5 and 15 y were most affected by dengue fever. Pain abdomen and vomiting were most common presenting symptoms. Ascites, plerural effusion, hepatomegaly, gall bladder wall thickening and abnormal LFT were found significantly high in severe dengue cases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Dengue is a vector borne viral infection and its incidence has increased by 30 fold over the last 50 y with increasing geographic distribution [1]. India being recognized as an endemic country for dengue, had recorded a maximum number of cases during 2012 and Karnataka state was the second highest. Uncontrolled growth in population, unplanned rapid urbanization and inadequate waste management, as currently happening in the city of Bangalore, have been cited as the reasons for outbreak of dengue. Children younger than 15 y of age are at highest risk for severe disease and death [2]. The manifestations of dengue fever vary from being asymptomatic to dengue shock syndrome and differ from epidemic to epidemic with atypical manifestations reported more frequently. Early recognition of dengue fever is important as delay in the treatment results in morbidity and mortality. Dengue fever is classified according to revised WHO classification as Dengue without Warning signs (D), Dengue with warning signs (DW) and Severe Dengue (SD). The present study describes the clinical features and outcome of dengue fever in children during its outbreak in 2012 admitted to a tertiary care hospital in Bangalore, Karnataka (South India). As the cases were classified according to the revised classification, symptoms, signs and investigations were evaluated for predicting the severity of dengue disease accordingly.
Material and Methods
The present prospective observational study was conducted at Sapthagiri Institute of Medical Sciences, Bangalore, Karnataka from July 2012 through February 2013. All children who presented with symptoms of fever, myalgia, arthralgia, headache, vomiting, pain abdomen and bleeding manifestations with confirmed blood tests for dengue infection were included in the study.
All clinically suspected patients irrespective of duration of illness were subjected to both Dengue NS1 antigen test (by immunochromatography method, Rapid Dengue Day 1 test) and Dengue IgM, IgG antibody test done by the same method.
History and examination findings of all the cases were recorded on the proforma on the day of admission and monitored for further progression of the disease. Laboratory investigations included complete blood count, liver function tests, coagulation profile with serum electrolytes and blood sugar monitoring in severe cases. Simultaneously, USG abdomen and chest radiograph were done in all the patients to look for evidence of plasma leakage.
Patients were classified according to revised WHO criteria and managed accordingly. Clinical features and laboratory parameters were analysed for frequencies and their predictability to identify severe forms of dengue as per the new criteria.
Data was analyzed by SPSS software version 16.0 and different groups were compared with chi-square test. Logistic regression was applied to identify significant risk factors for severe dengue. Study was approved by the Institutional Ethical Committee.
Results
Eighty one children were diagnosed to have dengue fever during the study period; 55(67.9 %) were boys and 26 (32.1 %) girls with a ratio of 2:1. Higher percentage of boys (65 %) had severe dengue compared to girls. Majority of children were from urban areas (65.4 %).
Commonest age group was between 5 and 15 y with mean age of presentation at 8 y. Table 1 shows distribution of age with respect to severity of dengue fever. Severe dengue was more commonly seen in children between 10 and 15 y (55 %) which is however statistically not significant.
Fever was present universally in all patients with mean duration of illness at presentation of 4.6 d. Complaints with which patients presented were vomiting (60.5 %), pain abdomen (32 %), headache (30.9 %), myalgia (23.5 %), bleeding manifestations (16 %) and joint pain (2.5 %). Epistaxis and gastrointestinal bleeding (malena) were the common bleeding manifestations noted along with petechiae, ecchymotic patches, gum bleeding, prolonged bleeding from IV injection site, hematuria and fresh GI bleed. Tourniquet test was positive in 24 % of cases.
Other complaints included respiratory distress, seizures and altered sensorium. CNS manifestations were noted in 5 patients out of whom 2 patients had seizures.
Table 2 shows the frequency of symptoms and signs in dengue fever observed during the study period. Shock was the presenting feature in 18.5 % of patients and icterus was noted in 2.5 % of patients. Though pleural effusion was predominantly seen on right side, bilateral effusion was also commonly seen with only one patient presenting with isolated left sided pleural effusion. Erythematous macular rash with facial flushing was present in 28.4 %. Many patients were noted to have bradycardia and prurits during recovery phase.
Depending upon above symptoms and signs and following investigations, 48.1 % of cases were classified as Dengue without warning signs (D), 27.2 % as Dengue with warning signs (DW) and 24.7 % of cases as Severe Dengue (SD). There was a high rate of admission of dengue without warning signs in the present case series mainly because of parental anxiety.
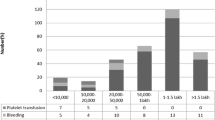
Dengue NS1 antigen test was positive in 66.7 % of cases, IgM in 29.6 % and Dengue IgG (along with either IgM or NS1 antigen) in 18.5 % cases. Out of total NS1 antigen positive cases (54), 88 % of cases were detected within 5 d of onset of illness. Three cases were positive on day 1 but positive response was noted as late as 9th day of illness. IgM positive response was noted between a period of 3 d to 15 d of onset of illness whereas IgG was positive between 2 d and 15 d. Anemia was noted in 14.8 % of patients whereas 72.8 % had evidence of hemoconcentration with mean packed cell volume (PCV) of 37.5 %. Thrombocytopenia was present in 82.7 % with 6.2 % of patients having counts less than 20,000/mm3 but majority of cases had platelet counts between 50,000 and 100,000. Figure 1 shows distribution of platelets with respect to severity of dengue cases. Sixty percent of patients in severe dengue had counts less than 20,000. Surprisingly in the present study none of the patients with platelet counts less than 20,000 had bleeding manifestations while 33.3 % of patients had bleeding manifestations with platelet count between 20,000 and 50,000 and 23.1 % had bleeding manifestations with platelets between 50,000 and 1 lakh.
USG abdomen showed features suggestive of dengue in 66.7 % of cases with gall bladder wall thickening seen significantly high in severe dengue cases (p value < 0.001). Liver function test was abnormal in 33.3 % of total patients whereas 80 % of severe dengue cases had abnormal LFT which is statistically significant (p value < 0.001). Prolonged prothrombin time (PT) and activated partial thromboplastin time (APTT) were seen in 9.9 %. Table 3 shows investigative profile in all the categories of dengue fever. On application of logistic regression of various risk factors discussed for severe dengue it was found out that ascites [95%CI 2.026–1934.986, p value 0.0181] and abnormal LFT [95%CI 2.564–124.072 p value 0.004] were more significantly associated with severe dengue. Table 4 shows values obtained in logistic regression of various risk factors.
Blood component therapy was used in 24.7 % cases with 15 patients being transfused with platelets, 7 patients with plasma and 2 patients with whole blood. Though not indicated as per WHO guidelines, all patients with counts less than 20,000 received platelets transfusion while 50 % of patients between 20,000 and 50,000 platelets were transfused due to bleeding manifestations. Patients who continued to be in shock inspite of receiving sufficient crystalloids were transfused with plasma whereas 2 patients who had anemia and continued to bleed received whole blood transfusion.
Inotropes were used in 4.9 % of cases out of which one patient died due to refractory shock. Mortality rate was 2.5 % with the death of two patients.
Discussion
The present study was conducted from July 2012 through February 2013 at Sapthagiri hospital, tertiary referral center, Bangalore. Eighty one children were diagnosed with dengue either based on NS1 antigen test or IgM and IgG antibody tests.
Common age group was between 5 and 15 y with mean age of presentation at 8 y in accordance with other studies [3]. During the study period 3 infants were diagnosed with dengue fever who presented with irritability, diarrhea and decreased intake of feeds but one infant had severe dengue with respiratory distress, petechiae, ecchymosis and prolonged PT and APTT.
Boys to girls ratio was 2:1 with severe dengue cases presenting in higher percentage in boys (65 %) which is in contrast to the observation made in other studies [4, 5]. Though WHO has reported shift of dengue to rural areas, in the present study still the patients were predominantly from urban area.
As observed in the study done by Wang et al. [6] arthralgia and myalgia were relatively less common complaints in children compared to adults whereas pain abdomen (32.5 %) and vomiting (60.5 %) constituted the more common presenting symptoms and seen more commonly in severe dengue patients, which was also statistically significant (p < 0.001). Malena and epistaxis were commonest bleeding manifestations noted which is similar to observation made in the study by Ahmed et al. [7].
Respiratory distress requiring supplementary oxygen was noted in 4 patients due to massive ascites and pleural effusion. CNS involvement was seen in 5 patients who presented with drowsiness, altered sensorium and convulsions. Investigations showed hyponatremia, hypoglycemia and abnormal LFT indicating encephalopathy like picture. Though encephalitis was suspected in one patient further investigations could not be done as the patient expired. One case of febrile seizures was also seen. As the involvement of CNS system in dengue fever is recognized more frequently, there should be a high index of suspicion of dengue in patients presenting with neurological manifestations in endemic areas [8, 9].
Facial puffiness (85 %), ascites (90 %), hepatomegaly (80 %) and pleural effusion (75 %) were significantly high (P < 0.001) in severe dengue compared to dengue fever with or without warning signs. Presence of above signs will guide in predicting the severity of illness as noted in other studies as well [10, 11] .
Presence of hemoconcentration (72.8 %), thrombocytopenia (82.7 %) and leucopenia gave important clues towards diagnosis of dengue fever. None of the patients with platelet count less than 20,000 had bleeding manifestations indicating that bleeding is not related to degree of thrombocytopenia as noted in other studies [12]. Liver enzymes (SGOT and SGPT) were raised in 33.3 % with average values between 100 and 400 IU/L and 80 % of severe dengue cases had abnormal LFT as noted in other studies [13]. Presence of ascites and abnormal LFT were more significantly associated with severe dengue. Both hyperglycemia and hypoglycemia were seen in severe dengue patients.
Ninety percent of severe dengue cases had features suggestive of dengue on USG Abdomen with gall bladder wall thickening (statistically significant) which is similar to observation made by Colbert et al. [14]. It is also noted by Chatterjee et al. that sonographical changes appear even before the serological tests become positive (as early as 3rd day) [15].
Among the two patients who died, one had refractory shock and the other patient was suspected to have encephalitis.
In the present study around 64.2 % of cases were exclusively positive only for NS1 antigen indicating higher sensitivity of NS1 antigen test in detecting dengue fever early during the onset of disease and it may also indicate higher rate of primary infection in the index case series. Combination of NS1 and IgM detection in samples during first few days is recommended to increase the dengue diagnostic sensitivity [16, 17]. IgG is the dominant immunoglobulin in secondary dengue infection which is detectable at high levels even in acute phase and IgM levels are significantly lower in secondary dengue infection than primary ones and may be undetectable in some cases [1]. However in the present case series IgG was present along with either IgM (in majority of cases) or with NS1 antigen (1 case).
Revised WHO classification was applied to categorize the patients. Dengue presents as a spectrum of disease instead of a distinct phase as in the earlier classification which has affected clinical management and triage of patients [18]. Patients presenting with CNS manifestations and respiratory distress in severe dengue were included in the present study; this could not be done in the earlier classification. Till date there has been only one Indian study which has applied new classification [19]. While there were overlapping symptoms and signs between dengue with and without warning signs, guidelines for identifying severe dengue are very clear and beneficial in managing patients who require emergency care. Though in this study the authors have not compared revised WHO classification with traditional WHO classification (1997) it is considered to be sensitive for the diagnosis of severe dengue but lacks in specificity especially pathological entity as the traditional scheme [18, 20].
Limitations of the present study are unavailability of dengue serotype information causing the outbreak and relatively small number of patients. So a larger multicenter study is advisable in future to get acquainted with revised WHO classification and to know feasibility of its application.
Conclusions
Children between 5 and 15 y were most affected by dengue fever with majority of cases from urban areas. Pain abdomen and vomiting were more common presenting symptoms with increased tendency for involvement of CNS was noted. Ascites, plerural effusion, hepatomegaly, gall bladder wall thickening and abnormal LFT were found significantly high in severe dengue cases which can be used as possible markers of severe dengue.
References
Dengue: Guidelines for diagnosis, treatment, prevention and control. World Health Organization. Geneva, Switzerland: WHO; 2009.
Division of Vector Borne Infectious Disease. Dengue fever. Atlanta, Ga: Centers for Disease Control and Prevention; 2008.
Mittal H, Faridi MM, Arora SK, Patil R. Clinicohematological profile and platelet trends in children with dengue during 2010 epidemic in north India. Indian J Pediatr. 2012;79:467–71.
Kulkarni MJ, Sarathi V, Bhalla V, Shivpuri D, Acharya U. Clinico-epidemiological profile of children hospitalized with dengue. Indian J Pediatr. 2010;77:1103–7.
Anders KL, Nguyet NM, Chau NVV, Hung NT, Thuy TT, Lien le B, et al. Epidemiological factors associated with dengue shock syndrome and mortality in hospitalized dengue patients in Ho Chi Minh city, Vietnam. Am J Trop Med Hyg. 2011;84:127–34.
Wang CC, Lee IK, Su MC, Lin HI, Huang YC, Liu SF, et al. Differences in clinical and laboratory characterstics and disease severity between children and adults with dengue viral infection in Taiwan, 2002. Trans R Soc Trop Med Hyg. 2009;103:871–7.
Ahmed S, Arif F, Yahya Y, Rehman A, Abbas K, Ashraf S, et al. Dengue fever outbreak in Karachi 2006-a study of profile and outcome of children under 15 years of age. J Pak Med Assoc. 2008;58:4–8.
Soares CN, Cabral-Castro MJ, Peralta JM, de Freitus MR, Zalis M, Puccioni-Sohler M. Review of etiologies of viral meningitis and encephalitis in a dengue endemic region. J Neurol Sci. 2011;303:75–9.
Jackson ST, Mullings A, Bennett F, Khan C, Gordon-Strachan G, Rhoden T. Dengue infection in patients presenting with neurological manifestations in a dengue endemic population. West Indian Med J. 2008;57:373–6.
Gupta V, Yadav TP, Pandey RM, Singh A, Gupta M, Kanaujiya P, et al. Risk factors of dengue shock syndrome in children. J Trop Pediatr. 2011;57:451–6.
Chacko B, Subramanian G. Clinical, laboratory and radiological parameters in children with dengue fever and predictive factors for dengue shock syndrome. J Trop Pediatr. 2008;54:137–40.
Joshi R, Baid V. Profile of dengue patients admitted to a teritiary care hospital in Mumbai. Turk J Pediatr. 2011;53:626–31.
Jagdishkumar K, Jain P, Manjunath VG, Umesh L. Hepatic involvement in dengue fever in children. Iran J Pediatr. 2012;22:231–6.
Colbert JA, Gordon A, Roxelin R, Silva S, Silva J, Rocha C, et al. Ultrasound measurement of gall bladder thickening as a diagnostic and prognostic indicator for severe dengue in pediatric patients. Pediatr Infect Dis J. 2007;26:850–2.
Chatterjee R, Mysore A, Ahya K, Shrikande D, Shedabale D. Utility of sonography in clinically suspected dengue. Pediatr Infect Dis. 2012;4:107–11.
Guzman MG, Jaenisch T, Gaczkowski R, Ty Hang VT, Sekaran SD, Kroeger A, et al. Multi-country evaluation of the festivity and specificity of 2 commercially available NS1 ELISA assays for dengue diagnosis. PLoS Negl Trop Dis. 2010;4:e811.
Arya SC, Agarwal N, Parikh SC, Agarwal S. Simultaneous detection of dengue NS1 antigen, IgM plus IgG and platelet enumeration during an outbreak. Sultan Qaboos Univ Med J. 2011;11:470–6.
Hadinegoro SR. The revised WHO dengue case classification: does the system need to be modified? Paediatr Int Child Health. 2012;32:33–8.
Prasad D, Kumar C, Jain A, Kumar R. Accuracy and applicability of revised WHO classification (2009) of dengue in children seen at a teritiary healthcare facility in northern India. Infection. 2013;41:775–82.
Narvez F, Gutierrez G, Perez MA, Elizendo D, Nuñez A, Balmaseda A, et al. Evaluation of the traditional and revised WHO classification of dengue disease severity. PLoS Negl Trop Dis. 2011;5:e1397.
Acknowledgments
The authors would like to thank Mr. Narasimha Murthy, Statistician, Sapthagiri Institute of Medical Sciences, Bangalore for his immense help in preparing the statistics of the study.
Contributions
KSS: Conceived the idea, designed the study, collected the data, entered data, did analysis, wrote first draft, approved the final manuscript and shall act as guarantor of the study; RS: Reviewed and edited the manuscript.
Conflict of Interest
None.
Source of Funding
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sahana, K.S., Sujatha, R. Clinical Profile of Dengue Among Children According to Revised WHO Classification: Analysis of a 2012 Outbreak from Southern India. Indian J Pediatr 82, 109–113 (2015). https://doi.org/10.1007/s12098-014-1523-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12098-014-1523-3