Abstract
Objective
To classify suspected dengue into dengue, dengue with warning signs and severe dengue, based on clinical features as per the revised WHO guidelines with special emphasis on serology.
Methods
It was a prospective cross-sectional study for five years from 2011–2016 in a tertiary care medical college hospital in Bangalore. All cases of fever of three to five days duration with symptoms like dengue were enrolled for the study. They were categorized into three groups as per the Revised WHO 2012 criteria. Laboratory parameters, serology, ultrasound abdomen and X-ray were done in almost all patients. Data was analysed by SPSS software, version 16, and different groups were compared with Chi square test.
Results
Five hundred sixty eight children were diagnosed to have dengue fever; 4.2% of the sample belonged to infancy. Majority were in the age group of 5–10 y (42.6%). Fever and flushing were present in majority of the children. Gastrointestinal bleed was more commonly seen in the severe dengue group. Dengue nonstructural protein antigen (NS1Ag) was positive in 78%, immunoglobulin M (IgM) in 15.8% and immunoglobulin G (IgG) in 14.6%. Children with IgG had more complications, though not statistically significant. Mortality was reported in 1.2%. Dengue serology helped to confirm the diagnosis, however did not help in patient management.
Conclusions
There is a considerable overlap in the symptomatology of dengue with warning signs and severe dengue. More studies are required on the severity and type of response to treatment in infants and obese adoloscents with severe dengue.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The incidence of dengue has increased by thirty-fold over the last fifty years [1]. It is endemic in more than 100 countries [2]. In South East Asian countries, dengue constitutes a major cause of pediatric morbidity and mortality [3]. Dengue fever is now classified into three categories as per the Revised WHO guidelines of 2012 into dengue without warning signs (D), with warning signs (DW) and severe dengue (SD) [4]. Patients with severe dengue and warning signs require hospital admission and those without, can be managed at home with oral rehydration solution and advice on when to return to the hospital [5]. This study was done in order to identify the early predictors of severe dengue and thereby reduce the morbidity and mortality. It will also help us to know the commonest age group affected with dengue in children for future vaccine recommendations.
Material and Methods
The present study was a cross-sectional observational study. It was conducted in a Medical college hospital from July 2011 through June 2016, in continuation with the pilot project done in 2012 [6]. All children who presented with fever of three–five days duration with clinical symptoms suggestive of dengue were included. A written consent was taken from the parents or guardian. History and clinical examination were noted. Laboratory investigations like complete hemogram, liver and renal function tests, X-ray and sonogram were done to aid the diagnosis. Bhat BioScan card test, a rapid sandwich immunochromatographic membrane test manufactured by Bhat Bio Tech India Limited for dengue was used to test nonstructural protein antigen (NS1Ag), immunoglobulin M (IgM) and immunoglobulin G (IgG) antibodies. The children were treated after categorization as per the WHO revised guidelines [4]. Data was analyzed by SPSS Software, version 20.0 and different groups were compared with Chi-square test. The study was approved by the hospital ethical committee.
Results
Over a period of five years, 568 children from infancy to adolescents, diagnosed clinically with dengue fever were enrolled in the study. Sixty-nine percent were seen between June to October which correlated with the rainy season. Among 568 children with dengue, infants comprised 4.2% (24 children). One hundred and forty four children (25.3%) were less than 5-y-old, 242 (42.6%) were in the age-group of 5–10 y and 182 (32%) were more than 10 y of age. Sixty six children (11.6%) were classified as dengue without warning signs, 308 (54.2%) were dengue with warning signs and 194 (34.2%) with severe dengue as shown in Fig. 1. Girls (237) accounted for 41% and the rest were boys.
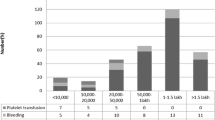
Table 1 depicts the clinical signs and symptoms frequently observed in present study. The proportions of symptoms like abdominal pain, vomiting, third space loss and hepatomegaly were significantly more in the SD group as compared to children diagnosed as D and DW (p < 0.01, significant). Chi square test was used as a test of significance of difference between proportions. Fever was noted in 552 (97.1%) patients, maculopapular erythematous rash in 126 (22%), flushing in all the children and hepatomegaly in 192 (33.8%). Other symptoms noted were abdominal pain (53.1%), vomiting (62.9%), cough (14.4%) and respiratory distress (10.9%). Bleeding manifestations were seen in 55 (9.6%) children, in the form of skin bleeds (54.5%), epistaxis (20%) GI bleed (20%) and hematuria (5.4%). Thirty six children had platelet counts less than 20,000, out of which only 11 had bleeding. Forty children, whose platelets were above 20,000, had significant bleeding. Central nervous system (CNS) involvement was seen in 5 patients in the form of drowsiness, severe headache, altered sensorium and convulsions. Hypotension was seen in 106 (18.69%) of 568, mostly in patients with SD (54.6%). Evidence of plasma leakage in the form of pleural effusion, ascites, edema of the dependent parts and facial puffiness were noted in almost all of SD and some of DW. Pruritis (20%) and bradycardia (21%) with a heart rate as low as 42 beats/ min were noted in patients during the recovery phase.
Hematocrit above 38 was noted in 264 out of 568 (46%) children. Thirty six children (6.3%) had platelets less than 20,000, 204 (35.9%) had between 21,000–50,000 and 236(41.5%) had between 50,000 to 100,000. X-ray chest showed pleural effusion in 168 (29.5%) children, right side more common than the left. Abdominal sonogram showed edema of gallbladder wall (65%), hepatomegaly (12.5%) and ascites in 71.6% of the children and they were more common in dengue with warning signs and severe dengue. Liver function test was abnormal in 30.6% with aspartate aminotranserase (AST) and alanine aminotranserase (ALT) in the range of 80–400 IU. Prothrombin time was abnormal in 0.18% and activated partial thromboplastin time in 0.7%.
Dengue NS1Ag was positive in 442 (78%), IgM in 90 (15.8%), and IgG in 82 (14.6%) of 568 children. Positive NS1Ag with no antibodies was seen in 363 (64%). In the study group, 70 (12.5%) were negative for dengue serology. Children who were IgG positive had more complications in the form of hypotension (18%) and bleeding (16%) as against 13% and 12% respectively in children with IgM positivity as shown in Fig. 2. Fifteen percent of children who were IgG positive required platelets as against 12% in children who were IgM positive. Vasopressor requirement was about 4%. Bleeding, as a clinical manifestation among IgG positive patients showed statistical significance (p < 0.05). Hypotension and requirement for platelet transfusion in IgG and IgM positive patients did not show any statistical significance (p > 0.05).
Seventy seven percent of SD i.e., 149 children were given intravenous fluids, 3–7 ml/kg/d depending on the response to treatment. Vasopressors were required in 23 patients of SD (11.8%). Blood component therapy was used in 125 of 568 children (22%). Platelets were given to children with counts less than 20,000, and with significant mucosal bleeding. Of the 125 children, platelets were transfused in 80 children (14% of 568) out of which 64 (32.9%) were from SD group. Fresh frozen plasma (FFP) was used in 23 children (11.8%) of severe dengue group. Four children required whole blood transfusion because of massive gastrointestinal bleed. Seven children died and all were adolescents. Five died due to refractory shock and multiorgan failure, one due to suspected encephalitis and the other due to severe GI bleeding. Five of the seven died within six to 24 h of admission. Mortality rate was 1.23% of the study group and 3.6% of the SD group.
Discussion
In the present study, the concentration of the cases was in the rainy and post monsoon period. This is significant from the community health view point, as effective preventive measures against Aedes aegypti can be implemented [7]. There was no significant difference in the incidence of dengue between boys and girls in present study as compared to the pilot study which showed a male preponderance [6, 8]. The age predominance was between 5 and 10 y, unlike the study done by Bhave et al., where the common age group was between 12 and 15 y [9]. In the present study, the percentage of children below 9 y constitute (72.7%) a huge majority. Pothapregada et al. in their study have observed the mean age of presentation as 6.9 y with a male female ratio of 1.2:1 [10]. A study by Hammond et al. differentiated the degree of severity in various age groups [11]. In the present study, diagnosis was mainly clinical with corroborative evidence of hematological, serological and radiological parameters. Clinical diagnosis is good enough to treat dengue in a resource poor setting like ours and timely escalation of supportive therapy plays a pivotal role for a better outcome [12]. In the present study, 4% were infants, in contrast to 20% in the study by Kabilan et al. [13]. This could be due to less clinical suspicion of dengue amongst infants. Among infants diagnosed with dengue fever in the study group, majority had fever, irritability and refusal of feeds. One infant with SD had prolonged jaundice and another infant had respiratory distress. All infants recovered without complications, unlike the study by Agarwal et al. in Delhi which reported 6% mortality among infants [14].
Arthralgia and myalgia were relatively less common presenting symptoms in index study similar to study by Wang et al. [15]. Fever and vomiting were common presenting symptoms in index study similar to a study by Aggarwal et al. [14]. Cough was seen in patients with pleural effusion and acute respiratory distress syndrome (ARDS). Hepatomegaly was more of a clinical finding. It did not correlate with the USG findings due to the radiologist observer bias and no standardized sonological age specific measurements for hepatomegaly in children.
Petechiae and skin bleeds were the most common bleeding manifestations similar to the study by de Souza et al. [16]. In the present study, epistaxis and malena were common mucosal bleeds similar to study by Ahmed et al. [17]. There was a significant overlap in the signs and symptoms of SD and DW. Younger age, persistent abdominal pain, tender hepatomegaly, signs of capillary leakage like ascites and pleural effusion, spontaneous bleeding, altered sensorium, seizures, oliguria and paralytic ileus were considered as early predictors of SD [18,19,20].
Hematocrit value of 38 was taken in accordance with Malaysian guidelines [16, 21]. There is no consensus on hematocrit for pediatric population in dengue and a variation of 20% from the basal values is taken significant [22]. Bleeding was seen mostly in patients whose platelet count were above 20,000. This shows that the platelet counts had no bearing with the bleeding tendency. Similar findings were noted by Joshi et al. [23]. Majority of the SD group had abnormal liver function test (LFT) similar to Jagadishkumar et al. who had abnormal LFT in 90% of the children with confirmed dengue, wherein AST was more impaired than ALT, owing to features of shock in dengue [24]. Sonogram showed ascites with gallbladder wall edema which was similar to the study by Colbert et al. [25]. The findings on ultrasound were more prominent in DW and SD patients.
The present study had a high percentage of children with NS1Ag positivity in contrast to Arya et al. who have shown a dengue serology positivity of 35.9% with negative serology (both dengue antibodies and NS1Ag) in 50% of the children [26]. It was because present patients were tested after day three of illness when the antibodies also start appearing. False positive NS1Ag can also occur in other viral fevers. Children with IgG positivity had more complications than IgM positivity suggesting that secondary dengue is more aggressive than the primary infection. However Lovera et al. have observed no difference in the frequency of dengue shock syndrome between primary and secondary infection [8]. The sensitivity can be increased by testing for both NS1Ag and IgM antibodies after day three of the illness and demonstrating rising titres at a later date.
Hypotension was seen in half of SD patients similar to studies by Bhave et al. (50%) and Pothapregada et al. (30%) [9, 10]. All non severe dengue cases (86.59%) recovered. The mortality rates in index study are comparable with other Indian studies [6, 9, 10, 12]. Lovera et al. have shown a mortality rate as low as 0.35% in their study with 12% intensive care unit (ICU) admissions [8].
The common age group was between 5 and 10 y in the index study. The currently available live attenuated tetravalent vaccine is recommended after 9 y of age in three doses at an interval of 6 mo. Efficacy against serotype 2 has been suboptimal with this vaccine. Seroconversion is lower if given in 2–5 y age group. There is an increased risk of hospital admissions in a small subset of patients [27, 28]. A new recombinant subunit vaccine with a three dose schedule at an interval of 0, 1 and 3 mo, effective in all age groups against all four serotypes, is still under trial and seems to be promising.
The number of infants in the present study group was less as dengue fever was less often suspected. Hence, high index of suspicion is required in infants during dengue season.
Conclusions
Children between 5 and 10 y were more commonly affected by dengue. Revised WHO criteria helps in categorizing patients and manage them effectively so as to reduce mortality and morbidity in dengue. Clinical assessment is more important to treat the illness. This context is relevant in our Indian settings with poor financial resources. More studies are needed in infants. It is a five year study in a single centre showing less mortality with early diagnosis. Clinical suspicion and early intervention helps in better management. In the present study, the percentage of children below 9 y constitute (72.7%) a huge majority. The currently available vaccine is for children above 9 y. The new vaccine under trial seems to be promising for the younger age group, which is more relevant for our set up.
Effective antivector measures during the rainy season, improving public awareness and introduction of dengue vaccine in younger age group will go a long way in the reduction of dengue menace in our country.
References
Dengue: Guidelines for Diagnosis, Treatment, Prevention and Control. Geneva: WHO; 2009.
Dengue, dengue haemorrhagic fever. Wkly Epidemiol Rec. 2000;75:193–6.
Cho-Min-Naing. Assessment of dengue hemorrhagic fever in Myanmar. Southeast Asian J Trop Med Public Health. 2000;31:636–41.
WHO. Handbook for Clinical Management of Dengue. Geneva, Switzerland: WHO; 2012.
Ingram PR, Mahadevan M, Fisher DA. Dengue management: practical and safe hospital-based outpatient care. Trans R Soc Trop Med Hyg. 2009;103:203–5.
Sahana KS, Ramabhatta S. Clinical profile of dengue among children according to revised WHO classification- analysis of a 2012 outbreak from southern India. Indian J Pediatr. 2015;82:109–13.
Ukey P, Bondade S, Paunipagar P, Powar R, Akulwar S. Study of seroprevalence of dengue fever in central India. Indian J Community Med. 2010;35:517–9.
Lovera D, de Cuellar MC, Araya S, et al. Clinical characteristics and risk factors of dengue shock syndrome in children. Pediatr Infect Dis J. 2016;35:1294–9.
Bhave S, Rajput CS, Bhave S. Clinical profile and outcome of dengue fever and dengue haemorrhagic fever in paediatric age group with special reference to WHO guidelines (2012) on fluid management of dengue fever. Int J Adv Res. 2015;3:196–201.
Pothapregada S, Kamalakannan B, Thulasingham M, Sampath S. Clinically profiling pediatric patients with dengue. J Glob Infect Dis. 2016;8:115–20.
Hammond SN, Balmaseda A, Perez L, et al. Differences in dengue severity in infants, children and adults in a 3-year hospital based study in Nicaragua. Am J Trop Med Hyg. 2005;73:1063–70.
Srigade V, Bingi K. Dengue-should we look for confirmation? Indian J Child Health. 2017;4:91–7.
Kabilan L, Balasubramanian S, Keshava SM, et al. Dengue disease spectrum among infants in the 2001 dengue epidemic in Chennai, Tamil Nadu, India. J Clin Microbiol. 2003;41:3919–21.
Aggarwal A, Chandra J, Aneja S, Patwari AK, Dutta AK. An epidemic of dengue hemorrhagic fever and dengue shock syndrome in children in Delhi. Indian Pediatr. 1998;35:727–32.
Wang CC, Lee IK, Su MC, et al. Differences in clinical and laboratory characteristics and disease severity between children and adults with dengue viral infection in Taiwan, 2002. Trans R Soc Trop Med Hyg. 2009;103:871–7.
Souza LJ, Pessanha LB, Mansur LC, et al. Comparison of clinical and laboratory characteristics between children and adults with dengue. Braz J Infect Dis. 2013;17:27–31.
Ahmed S, Arif F, Yahya Y, et al. Dengue fever outbreak in Karachi 2006 -- a study of profile and outcome of children under 15 years of age. J Pak Med Assoc. 2008;58:4–8.
Gupta V, Yadav TP, Pandey RM, et al. Risk factors of dengue shock syndrome in children. J Trop Pediatr. 2011;57:451–6.
Chacko B, Subramanian G. Clinical, laboratory and radiological parameters in children with dengue fever and predictive factors for dengue shock syndrome. J Trop Pediatr. 2008;54:137–40.
Pothapregada S, Kamalakannan B, Thulasingham M. Risk factors for shock in children with dengue fever. Indian J Crit Care Med. 2015;19:661–4.
Clinical Practice Guidelines. Management of dengue fever in children. Malaysia: Ministry of Health, Malaysia Academy of Medicine; 2004. MOH/P/PAK/95.04.
Elling R, Henneke P, Hatz C, Hufnagel M. Dengue fever in children. Pediatr Infect Dis J. 2013;32:1020–2.
Joshi R, Baid V. Profile of dengue patients admitted to a tertiary hospital in Mumbai. Turk J Pediatr. 2011;53:626–31.
Jagadishkumar K, Jain P, Manjunath VG, Umesh L. Hepatic involvement in dengue fever in children. Iran J Pediatr. 2012;22:231–6.
Colbert JA, Gordon A, Roxelin R, et al. Ultrasound measurement of gallbladder wall thickening as a diagnostic test and prognostic indicator for severe dengue on pedatric patients. Pediatr Infect Dis J. 2007;26:850–2.
Arya SC, Agarwal N, Parikh SC, Agarwal S. Simultaneous detection of NS1 antigen, IgM plus IgG and platelet enumeration during an outbreak. Sultan Qaboos Univ Med J. 2011;11:470–6.
Rothman AL, Ennis FA. Dengue vaccine: the need, the challenges and progress. J Infect Dis. 2016;214:825–7.
Hadinegoro SR, Arredondo-Garcia JL, Capeding MR, et al. Efficacy and long-term safety of a dengue vaccine in regions of endemic disease. New Engl Med. 2015;373:1195–206.
Acknowledgements
The authors would like to thank Dr. Vinod K Ramani, Associate Professor, Department of Community Medicine, Sapthagiri Instritute of Medical Sciences, Bengaluru and Mrs. Lavanya, Statistician, SIMS & RC for their help in analyzing data.
Author information
Authors and Affiliations
Contributions
SR continued the pilot project published earlier in 2011, compiled data, edited and submitted the manuscript. SP wrote the manuscript. NH and SVB collected the data. SR will act as guarantor for the paper.
Corresponding author
Ethics declarations
Conflict of Interest
None.
Source of Funding
None.
Rights and permissions
About this article
Cite this article
Ramabhatta, S., Palaniappan, S., Hanumantharayappa, N. et al. The Clinical and Serological Profile of Pediatric Dengue. Indian J Pediatr 84, 897–901 (2017). https://doi.org/10.1007/s12098-017-2423-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12098-017-2423-0