Abstract
Anaplastic lymphoma kinase (ALK) rearrangement is detected in 3–7% of patients with non-small-cell lung cancer. Crizotinib is an ALK inhibitor, which was approved in 2011 for the treatment of ALK-positive lung cancer. Despite the initial enthusiasm, most of the patients develop resistance within the first year of treatment. The main mechanisms are secondary mutations and bypass track activation. Moreover, crizotinib has low penetration into the central nervous system. The need to overcome these limitations has led to the development of second-generation inhibitors that have better effectiveness against crizotinib-resistant mutations and brain metastases. Ceritinib and alectinib are the only approved drugs of this group. Many ongoing trials try to define the most appropriate agent for the treatment of ALK-positive lung cancer depending on the responsible mechanism. This review focuses on the current data regarding the potential mechanisms of resistance to ALK inhibitors and the strategies to overcome it.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lung cancer is the second most common cancer and the leading cause of cancer death worldwide [1]. It is estimated that in 2016, in the United States of America, 224.390 new cases and 158.080 deaths will occur [2]. Non-small-cell lung cancer (NSCLC) accounts for 85–90% of cases and chemotherapy was the standard treatment for it until recently [3]. However, over the last decade, this approach has changed thanks to the advances in molecular analysis, the identification of oncogenic drivers that are responsible for lung cancer, and the development of targeted therapies [4]. The first big change happened in 2004 when it was described that patients with activating mutations in the epidermal growth factor receptor (EGFR) gene respond dramatically to EGFR tyrosine kinase inhibitors (TKIs), such as gefitinib, erlotinib and afatinib [5]. Then, in 2007, it was discovered that 3–7% of patients with adenocarcinoma carry an anaplastic lymphoma kinase (ALK) rearrangement. For these patients, ALK inhibitor crizotinib is the appropriate treatment choice [6].
Targeted therapies increased the progression-free survival (PFS) and overall survival (OS) in these groups and started a new era in the treatment of lung cancer [7]. Despite the initial enthusiastic outcomes, it became clear very soon that the development of acquired resistance is the main limitation to these therapies [8]. This review describes how ALK inhibitors (such as crizotinib) work, the discovery of second- and thirrd-generation inhibitors (ceritinib, alectinib, brigatinib, lorlatinib), the mechanisms of resistance, and the ways to overcome it.
Methods
The data were collected through published reviews, case reports, articles and studies with publication date from 2007 to 2016. The MEDLINE and the Journal of Thoracic Oncology were our primary databases and the main citations searched were ALK rearrangement, ALK-positive non-small-cell lung cancer, crizotinib, ceritinib, alectinib, mechanisms of resistance to ALK inhibitors, brain metastases in ALK-positive non-small-cell lung cancer. We excluded publications that were not written in English.
ALK rearrangement and its role in lung cancer
Anaplastic lymphoma kinase protein belongs to the insulin receptor tyrosine kinase family. It is encoded by the ALK gene which is located on chromosome 2p23. As other receptors, it has an extracellular ligand-binding part, a transmembrane helix and an intracellular domain that is responsible for the kinase activation [9]. It was first detected as part of the fusion protein NPM–ALK in a translocation between chromosomes 2 and 5, associated with anaplastic large cell lymphoma [10]. Based on experiments on mice, ALK protein normally participates in the development of the nervous system [11]. The most common ALK mutation is rearrangement which disrupts the normal structure of the gene. As a result, a fusion gene is formed and encodes a fusion ALK protein. This kind of translocation has been associated with oncogenesis as it has been found in different types of cancer, such as lymphoma, neuroblastoma and NSCLC [12].
With regard to NSCLC, the first reference was made in 2007 when the EML4–ALK fusion protein was identified in a patient with lung adenocarcinoma [13]. The fusion protein arises from an inversion within the chromosome 2 and has many variants depending on the fusion point within the EML4 gene. It leads to constant activation of the kinase and the signaling pathways and, consequently, to oncogenesis [14]. ALK rearrangement is described in 3–7% of NSCLCs. Every patient with lung adenocarcinoma should now be tested for it using fluorescence in situ hybridization (FISH) analysis, although it is more common among younger, female patients with a history of no (or light) smoking, and no EGFR or KRAS mutations [15, 16]. The central nervous system (CNS) is the most common site of metastasis in ALK-positive NSCLC, with frequency from 25 to 40% [17, 18].
Crizotinib
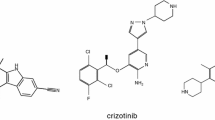
ALK fusion protein is an excellent target in lung cancer treatment because of its oncogenic role, as it was initially proved in preclinical models [19]. Clinical trials had the same promising results when crizotinib was tested. Crizotinib (PF-02341066, Xalkori, Pfizer Inc) is an oral, ATP-competitive, small-molecule, selective inhibitor targeting ALK and c-Met tyrosine kinase. In particular, it inhibits the phosphorylation of ALK when it is activated at nanomolar concentrations [20]. In the phase I PROFILE 1001 [21] and phase II PROFILE 1005 [22] trials, the overall response rate (ORR) was about 60% leading to the accelerated approval of crizotinib for patients with ALK-rearranged, locally advanced or metastatic NSCLC [23]. The approval was granted by Food and Drug Administration (FDA) in 2011. Two more studies showed the superiority of crizotinib over standard chemotherapy in ALK-positive NSCLC. In the phase III PROFILE 1007 trial, patients, who had received platinum-based chemotherapy as first-line treatment and had disease progression, were randomly administered crizotinib or chemotherapy (pemetrexed or docetaxel). In the first group, the RR was 65% and the PFS was 7.7 months, while, in the second group, the results were 20% and 3.0 months, respectively. There was no difference in OS for both arms. Patients that were treated with chemotherapy were able to receive crizotinib after disease progression. This led to a high crossover rate between the two groups and, most likely, to the similar results in OS [24]. The same benefit was demonstrated in the phase III PROFILE 1014 trial. Previously untreated patients were randomly assigned to receive crizotinib or chemotherapy (platinum plus pemetrexed). The RR in the first group was higher (74 vs 45%), as were the PFS (10.9 vs 7.0 months). There was again no significant difference in OS due to the patient crossover from the chemotherapy to the crizotinib arm [25]. In a year, we expect the results of the phase III PROFILE 1029 trial which compares crizotinib with chemotherapy as first-line treatment in patients from eastern Asia [26] (Table 1).
Mechanisms of resistance to crizotinib
Despite the fact that the targeted therapies have introduced a new era in lung cancer treatment, they have a large limitation: the development of resistance [27]. Patients who receive crizotinib experience resistance to the drug within the first year [28]. This was first described in 2010 when a patient with ALK-rearranged NSCLC taking crizotinib had disease progression after 5 months of treatment. A sample of his pleural effusion was obtained, in which two novel mutations, L1196M and C1156Y, were detected and proved to be responsible for the lack of response to the drug [29]. The mechanisms of resistance can be divided into two main categories: ALK dominant, when ALK signaling is still important, and ALK non-dominant, when there is no connection to ALK [30]. The first group includes secondary mutations (31% frequent), copy number gain (CNG-13%), and their combination (6%). The second group includes bypass tracks that are activated (50% frequent) [31].
Apart from the acquired resistance, the primary resistance to crizotinib is also worth considering. The initial RR is about 60%, which accounts for the lack of response in some patients. Some possible explanations are the different variants of the EML4–ALK fusion protein or the false-positive diagnoses of ALK translocation [32]. Another type of resistance is the disease progression only in CNS and not in other organs as crizotinib does not penetrate the blood–brain barrier sufficiently [33].
ALK dominant mechanisms
Secondary mutations in the ALK gene are the main mechanisms of this group as it happens in the treatment with EGFR TKIs [34]. It has already been mentioned that mutations L1196M and C1156Y were the first to be detected. L1196M, in particular, changes the ATP-binding domain and does not allow crizotinib to inhibit ALK, acting as a gatekeeper mutation [35]. More than ten similar mutations have been identified, of which the most common are L1152R [36], G1202R, S1206Y, 1151Tins [37], G1269A [38], F1174L [39], G1269S, L1198P, and D1203N [40].
Anaplastic lymphoma kinase amplification due to copy number gain is another way of developing resistance, which occurs alone or in combination with secondary mutations [41]. Finally, the loss of ALK rearrangement as a possible mechanism is yet to be proved, as the detection of ALK is influenced by many factors [42].
ALK non-dominant mechanisms
In this category, the activation of alternative signaling pathways and the mutations in genes not connected with ALK are the responsible mechanisms of resistance to crizotinib. The most common are the activation of the EGFR pathway, as shown by the increased levels of EGFR phosphorylation in biopsy specimens after crizotinib therapy [8, 43], the mutations in the KRAS gene [38], and the amplification of the KIT gene [37]. There are, also, some rarer mechanisms, such as activation of the ErbB family, activation of the insulin-like growth factor receptor 1 (IGF-1R) pathway, epithelial–mesenchymal transition induced by hypoxia, autophagy [31], mutations in CD74-ROS1 [44], activation of the HER family [45] and, of course, in some cases, no apparent cause can be found. Finally, a case of ALK-rearranged NSCLC transformed into an SCLC was recently reported. This mechanism is known to be responsible for developing resistance to EGFR inhibitors [46].
Second-generation ALK inhibitors
The previously described limitations to crizotinib therapy showed the need for development of second-generation ALK inhibitors for NSCLC. This category includes ceritinib (LDK 378, Zykadia, Novartis) and alectinib (RO5424802/CH5424802, Alecensa, Chugai-Roche) whose aim is to enhance ALK inhibition and overcome resistance mechanisms [30].
Ceritinib
Ceritinib is an oral, ATP-competitive, small-molecule ALK inhibitor. It has a similar mechanism of action to crizotinib, but it is 20 times more potent against ALK. It does not inhibit the MET kinase while it is effective—to a lesser extent—against the IGF-1 receptor, the insulin receptor (InsR), and ROS1 [47]. The drug was approved by FDA in April 2014 for the treatment of patients with metastatic ALK-positive NSCLC who had disease progression after receiving crizotinib or are intolerant of it.
The accelerated approval was based on the very promising results of the ASCEND-1 trial before they were even published [48, 49]. It is a phase I trial that determined initially the maximum tolerated dose (MTD) of ceritinib at 750 mg daily. The study was later expanded with the addition of a larger number of patients who had either already received crizotinib or not. In the first group, the ORR was 56% and the PFS was 6.9 months, while in the second group, the outcomes were 58% and 10.4 months, respectively [50]. The updated data of ASCEND-1 were recently published and the PFS was 18.4 months for crizotinib-naïve patients [51]. Similar successful results were also described in phase II trials. In ASCEND-2, ceritinib was administered to patients who had already been treated with chemotherapy and had been resistant to crizotinib [52], while in ASCEND-3, ceritinib was given as first-line treatment [53]. In 2018, two phase III trials will be complete and their results are expected with great interest: ASCEND-4 compares ceritinib with chemotherapy (pemetrexed plus platinum) as first-line treatment and ASCEND-5 compares the same drugs in patients whose disease progressed after chemotherapy and crizotinib [54] (Table 1).
Even if ceritinib was especially developed to tackle the mechanisms of resistance to crizotinib, it confirmed the rule of targeted therapies: resistance arose not only in cell lines, but also in patients that received it. The first discovered mechanisms were the secondary mutations G1202R and F1174V/C. In one patient, both G1202R and F1174V/C were found at the same time proving the heterogeneity in the development of resistance [55]. Other identified mutations are the G1123S [56], C1156Y, 1151Tins, and L1152R [40] (Table 2). As for copy number gain, the other ALK dominant mechanism of resistance to crizotinib, it has not been confirmed for ceritinib [31].
On the contrary, secondary mutations were not detected in other preclinical studies. The most likely responsible resistance mechanism is the activation of alternative signaling pathways and, in particular, the NRG1–HER3–EGFR axis. Neuregulin-1 (NRG1), which is a ligand for HER3 and activates the EGFR pathway, was found to be increased in ceritinib-resistant cell lines [57]. Finally, the overexpression of P-glycoprotein seems to be associated with poor response to ceritinib therapy [58].
Alectinib
Alectinib is an oral, selective ALK inhibitor, 10 times more potent than crizotinib [59]. It is also effective against the leukocyte receptor tyrosine (LTK) and cyclin G-associated kinases (GAK), but not against IGF-1, InsR and ROS1, like ceritinib [6]. FDA granted Breakthrough Therapy Designation (BTD) to alectinib in June 2013 and finally approved it in December 2015 for patients with advanced ALK-rearranged NSCLC who had progressed on crizotinib [60]. Japan was the first country to approve the drug in July 2014 after the results of the phase I/II AF-001JP trial, which included only Japanese patients who had not received previous treatment [61]. The maximum tolerated dose was determined at 300 mg during the first part of the study. Then, in the second part, alectinib was administered at the same dosage and the ORR was 93.5% [62], while the 2-year PFS was 76% [63]. Two phase II trials that followed studied the safety and efficacy of the drug at a daily dose of 600 mg in crizotinib-resistant patients, without comparing it with any other treatment. NP28673 recruited patients from all over the world, while NP28761 included patients only from North America. The ORR was 49.2 and 47.8%, while the PFS was 11.2 and 7.5 months, respectively [64, 65] (Table 1).
With regard to secondary mutations, they contribute to the development of resistance to alectinib as well. V1180L was identified in preclinical models and I1171T in a patient. They both affect the binding between the drug and the ALK fusion protein [66]. I1171S [67] and G1202R [68] have also been detected (Table 2). Furthermore, the amplification of the MET gene is a potential mechanism of resistance, as was found in an in vitro study with the activation of the Hepatocyte Growth Factor (HGF)–MET pathway [42] and in the rebiopsy of an alectinib-resistant patient [69]. The phase II ALRIGHT trial has been designed based on these data and will gather information on whether crizotinib can be administered to alectinib-refractory patients as it inhibits both ALK and MET kinases [70]. Like in ceritinib-resistant patients, the NRG1–HER3–EGFR axis affects the sensitivity to alectinib [57]. Finally, we should mention that a case of transformation to SCLC after treatment with alectinib has been reported [71].
Strategies to overcome resistance
Judging from the above, it becomes clear that almost all patients with ALK-rearranged NSCLC, who are treated with ALK inhibitors, have disease progression after a certain period of time, as they become resistant to these drugs. In some of them, there is only an increase in the size of their lesions with no further deterioration of their symptoms [72]. In the case of crizotinib, there is evidence that the continuation of the same treatment beyond progression could be beneficial [73]. This approach has been withdrawn after the development of the second-generation ALK inhibitors, especially in patients with rapid progression [74].
As for ceritinib, the very good response of the crizotinib-refractory patients led to administering the drug as second-line treatment in this group, unless there are secondary identified mutations that are responsible for resistance to ceritinib [49, 54]. The phase I–II AF-002JG study had similar results when it examined the other approved second-generation ALK inhibitor. Alectinib was administered to 47 patients who had developed resistance to crizotinib at a dose of 600 mg twice daily, which resulted in an ORR of 55% [75]. There is also an ongoing phase III trial, ALEX, which compares crizotinib with alectinib as a first-line treatment in ALK-positive NSCLC [26].
The disease progression only in CNS is a type of acquired resistance and different strategies have been tested to overcome it. One of them was the dose escalation of crizotinib as it does not cross the blood–brain barrier sufficiently, but that did not lead to a better outcome [76]. The second-generation ALK inhibitors seem to have higher penetration and response. In the ASCEND-1 and ASCEND-2 trials, patients with brain metastases that were resistant to crizotinib and received ceritinib had an intracranial RR at 35.7 and 39.4%, respectively [77]. ASCEND-7 is still ongoing to evaluate the safety and efficacy of ceritinib in patients with ALK-rearranged NSCLC and CNS disease [26]. With regard to alectinib, the analysis of the NP28761 and NP28673 trials showed a 22% CRR in patients with brain metastases [78], while in AF-002JG, the RR was 52% [75]. These results, in combination with the small number of secondary mutations causing resistance, make alectinib a very attractive option as a first-line treatment. Dose escalation of the drug has been used as an effort to increase response in CNS, but this hypothesis needs more trials to confirm it [79]. We should also mention the case of leptomeningeal metastases (LM), a rare form of CNS involvement. Alectinib has been reported to have good results in patients with ALK-positive NSCLC and LM after progression on both crizotinib and ceritinib [80]. Finally, another potential way to accomplish higher intracranial concentration of ALK inhibitors is to co-administer them along with an inhibitor of the P-glycoprotein (P-gp), a transporter of the blood–brain barrier [81]. According to preclinical models, alectinib is not transported to the brain via the P-gp and, probably, this is why it has better accumulation and response in CNS [17].
Regarding the oligoprogression only in CNS, there is also the option of focal treatments, such as radiotherapy (whole-brain radiotherapy-WBRT or stereotactic radiosurgery-SRS) and local ablative therapy (LAT), alone or in combination with ALK inhibitors. A recent multi-institutional study showed that patients with ALK-rearranged NSCLC and brain metastases had prolonged survival when they received radiotherapy along with ALK TKIs [82]. In another study of a single institution, it was described that LAT and continuation of crizotinib offered more than 6 months of additional disease control [83]. However, more trials are necessary to clarify the role of local therapies.
Brigatinib (AP26113, Ariad) is another second-generation ALK inhibitor that is being researched as a way to overcome resistance to the previously described drugs. It is an oral inhibitor of EGFR, ALK and ROS1, and is effective against the EGFR T790M and ALK L1196M, C1156Y, G1202R, S1206Y, 1151Tins, D1203N, F1174C [84] mutations (Table 2). In the phase I–II NCT01449461 trial, patients with ALK-rearranged NSCLC received brigatinib and the results of the ORR were the following: 100% for those who had not received any other treatment, 69% for those who were crizotinib-refractory and 37% for the patients with brain metastases. Furthermore, we should mention the ongoing phase II NCT02094573 ALTA trial for patients with resistance to crizotinib who are given brigatinib as second-line treatment [26, 85], and the phase II NCT02706626 trial that will soon recruit patients to receive the drug after progression on other second-generation ALK inhibitors [26, 86] (Table 1). On August 30, 2016, the pharmaceutical company that developed brigatinib completed its rolling submission of the New Drug Application (NDA) to the FDA to get an accelerated approval.
Furthermore, many thirrd-generation ALK inhibitors are in early stages of development and are especially designed to be more effective in CNS as well as against the secondary mutations that cause resistance to other TKIs. The most important of these are PF-06463922 (lorlatinib, Pfizer), Χ-396 (Xcovery), X-376, RXDX-101(entrectinib), ASP3026, TSR-011, CEP-37440, and CEP-28122 [32, 87,88,89] (Tables 2, 3). A case of a patient, who was resistant to crizotinib because of the C1156Y mutation and received lorlatinib, is worth mentioning. When he had disease progression, he developed another mutation, the L1198F, which made him sensitive, again, to crizotinib [90]. This case report is very interesting, but needs to be proved by more clinical data.
The activation of bypass tracks is a common mechanism of resistance to ALK inhibitors. For this reason, it could be a potential target in lung cancer treatment. There are some ongoing preclinical trials whose purpose is to inhibit ALK and the EGFR, ΚΙΤ, IGF-1R pathways at the same time [31, 91, 92]. The 90-kDa heat shock protein (HSP90) inhibitors also seem to be very promising. HSP90 is a molecular chaperone that contributes to the correct formation and stability of proteins. Its inhibition leads to abnormal function of these proteins, including ALK, as well as lack of activation of many oncogenic pathways [28]. IPI-504 (retaspimycin hydrochloride), STA-9090 (ganetespib), AT13387 (onalespib) and AUY922 are inhibitors of this kind, which are used alone or in combination with ALK TKIs in ongoing trials (NCT01579994, NCT01712217, NCT01772797) [32].
Discussion and future perspectives
The discovery of the ALK rearrangement and its oncogenic role, as well as the discovery of the EGFR mutations, revolutionized the NSCLC treatment. In patients that carry the translocation, standard chemotherapy was replaced by targeted therapies and, in particular, by crizotinib that significantly increased the RR and the PFS of this group. Despite the initial enthusiastic results of all trials on crizotinib, two limitations became soon clear: the development of resistance within the first year of treatment and the poor response in CNS where metastases occur very often in ALK-positive NSCLC. The most common mechanisms of resistance are secondary mutations and activation of alternative signaling pathways. The development of novel inhibitors was the next logical step and two of them, ceritinib and alectinib, have been approved for the treatment of ALK-rearranged NSCLC. Unfortunately, the resistance is inevitable even after these drugs; so different third-generation inhibitors are under investigation.
A question that needs to be answered about these new agents is in what sequence they should be administered, so that the highest clinical benefit is obtained. Doctors face the following dilemma, namely, whether to use second-generation inhibitors only after progression on crizotinib so as to overcome the acquired resistance or to administer them from the start to achieve higher responses. The superiority of crizotinib compared with chemotherapy as a first-line treatment has been described in the PROFILE 1014 trial. Similar studies should be done on the other drugs as well. When complete, ASCEND-4 will offer some answers with regard to ceritinib, but we have not yet seen a similar trial on alectinib. The head-to-head comparison of the different inhibitors is also very important and there are two ongoing trials of this kind: ALEX, which compares crizotinib with alectinib, and ALTA-1L between crizotinib and brigatinib, which is now recruiting patients [26]. Their results are expected with anticipation. As for crizotinib and ceritinib, there has been only a recently reported study that compared data from previous trials after adjusting the characteristics of the patients and showed an association of ceritinib with better PFS [93]. The evaluation of the ALK TKIs should also be focused on their efficacy in CNS to determine the appropriate therapy for brain metastases. Alectinib seems to have the best outcomes as it achieves a sufficient intracranial concentration.
Beyond targeted therapies, there is another field in Medical Oncology that has been rapidly growing over the last years: immunotherapy. Nivolumab and pembrolizumab have been approved for the treatment of patients with metastatic NSCLC, while ipilimumab is evaluated in a phase III study. The combination of an ALK inhibitor with immune checkpoint inhibition might be an effective treatment for ALK-positive NSCLC. There are three ongoing trials that combine ceritinib with nivolumab (NCT02393625), crizotinib with pembrolizumab (NCT02511184), and crizotinib with ipilimumab (NCT01998126) [26].
Therefore, it is very obvious how important rebiopsy is when a patient with ALK-rearranged NSCLC develops disease progression. There needs to be a comparison with the initial diagnosis to detect any secondary mutations or overexpressed products of other activated pathways. This is the only approach that will help us understand the mechanisms of resistance, choose the right treatment, and increase the response and survival of our patients.
References
Siegel R, Miller K, Jemal A. Cancer statistics. CA Cancer J Clin. 2016;66:7–30.
Siegel RL, Miller KD, Jemal A. Cancer statistics 2016. Ca Cancer J Clin. 2016;66:7–30.
Ettinger D, Wood D, Akerley W, Bazhenova L, Borghaei H, Camidge DR et al. Non-small-cell lung cancer, Version 6.2015. Featured updates to the NCCN guidelines. JNCCN. 2015;13(5):517–21.
Candarella S, Johnson B. The impact of genomic changes on treatment of lung cancer. Am J Respir Crit Care Med. 2013;188(7):770–5.
Awad M, Shaw AT. ALK inhibitors in non-small-cell lung cancer: crizotinib and beyond. Clin Adv Hematol Oncol. 2014;12(7):429–39.
Sullivan I, Planchard D. Treatment modalities for advanced ALK-rearranged non-small-cell lung cancer. Future Oncol. 2016. doi:10.2217/fon.16.15.
Van der Wekken AJ, Saber A, Hiltermann TJN, Kok K, Van den Berg A, Groen HJM. Resistance mechanisms after tyrosine kinase inhibitors afatinib and crizotinib in non-small cell lung cancer, a review of the literature. Crit Rev Oncol/Hematol. 2016. doi:10.1016/j.critrevonc.2016.01.024.
Lovly C, Shaw AT. Molecular pathways: resistance to kinase inhibitors and implications for therapeutic strategies. Clin Cancer Res. 2014;20(9):2249–56.
Bayliss R, Choi J, Fennell DA, Fry AM, Richards MW. Molecular mechanisms that underpin EML4-ALK driven cancers and their response to targeted drugs. Cell. 2016;73:1209–24.
Morris SW, Kirstein MN, Valentine MB, Dittmer KG, Shapiro DN, Saltman DL, et al. Fusion of a kinase gene, ALK, to a nucleolar protein gene, NPM, in non-Hodgkin’s lymphoma. Science. 1994;263:1281–4.
Shaw AT, Solomon B. Targeting anaplastic lymphoma kinase in lung cancer. Clin Cancer Res. 2011. doi:10.1158/1078-0432.
Webb T, Slavish J, George RE, Look AT, Xue L, Jiang Q, et al. Anaplastic lymphoma kinase: role in cancer pathogenesis and small-molecule inhibitor development for therapy. Expert Rev Anticancer Ther. 2009;9(3):331–56.
Soda M, Choi YL, Enomoto M, Takada S, Yamashita Y, Ishikawa S, et al. Identification of the transforming EML4-ALK fusion gene in non-small-cell lung cancer. Nature. 2007;448:561–6.
Gerber D, Minna J. ALK inhibition for non-small-cell lung cancer: from discovery to therapy in record time. Cancer Cell. 2010. doi:10.1016/j.ccr.2010.11.033.
Shaw AT, Yeap BY, Mino-Kenudson M, Digumarthy SR, Costa DB, Heist RS, et al. Clinical features and outcome of patients with non-small-cell lung cancer who harbor EML4-ALK. J Clin Oncol. 2009;27:4247–53.
Lindeman NI, Cagle PT, Beasley MB, Chitale DA, Dacic S, Giaccone G, et al. Molecular testing guideline for selection of lung cancer patients for EGFR and ALK tyrosine kinase inhibitors: guideline from the College of American Pathologists, International Association for the Study of Lung Cancer, and Association for Molecular Pathology. J Thorac Oncol. 2013;8:823–59.
Toyokawa G, Seto T, Takenoyama M, Ichinose Y. Insights into brain metastasis in patients with ALK+ lung cancer: is the brain truly a sanctuary? Cancer Metastasis Rev. 2015;34:797–805.
Rangachari D, Yamaguchi N, VanderLaan PA, Folch E, Mahadevan A, Floyd SR, et al. Brain metastases in patients with EGFR-mutated or ALK-rearranged non-small cell lung cancers. Lung Cancer. 2015;88(1):108–11.
Christensen JG, Zou HY, Arango ME, Li Q, Lee JH, McDonnell SR, et al. Cytoreductive antitumor activity of PF-2341066, a novel inhibitor of anaplastic lymphoma kinase and c-Met, in experimental models of anaplastic large-cell lymphoma. Mol Cancer Ther. 2007;6(12):3314–22.
Kwak EL, Bang YJ, Camidge DR, Shaw AT, Solomon B, Maki RG, et al. Anaplastic lymphoma kinase inhibition in non-small-cell lung cancer. N Engl J Med. 2010;363:1693–703.
Camidge DR, Bang YJ, Kwak EL, Iafrate AJ, Varella-Garcia M, Fox SB, et al. Activity and safety of crizotinib in patients with ALK-positive non-small-cell lung cancer: updated results from a phase I study. Lancet Oncol. 2012;13(10):1011–9.
Crino L, Kim DW, Riely GJ, Janne PA, Blackhall FH, Camidge DR, et al. Initial phase 2 results with crizotinib in advanced ALK-positive non-small-cell lung cancer (NSCLC): PROFILE 1005. J Clin Oncol. 2011;29:7514.
Ou SHI, Bartlett CH, Mino-Kenudson M, Cui J, Iafrate AJ. Crizotinib for the treatment of ALK-rearranged non-small-cell lung cancer: a success story to usher in the second decade of molecular targeted therapy in oncology. Oncologist. 2012;17:1351–75.
Shaw AT, Kim DW, Nakagawa K, Seto T, Crino L, Ahn MJ, et al. Crizotinib versus chemotherapy in advanced ALK-positive lung cancer. N Engl J Med. 2013;368:2385–94.
Solomon B, Mok T, Kim DW, Wu YL, Nakagawa K, Mekhail T, et al. First-line crizotinib versus chemotherapy in ALK-positive lung cancer. N Engl J Med. 2014;371:2167–77.
Clinicaltrials.gov.
Morgensztern D, Campo MJ, Dahlberg SE, Doebele RC, Garon E, Gerber DE, et al. Molecularly targeted therapies in non-small-cell lung cancer annual update 2014. J Thorac Oncol. 2015;10:S1–63.
Ye M, Zhang X, Li N, Zhang Y, Jing P, Chang N, et al. ALK and ROS1 as targeted therapy paradigms and clinical implications to overcome crizotinib resistance. Oncotarget. 2016;7(11):12289–304.
Choi YL, Soda M, Yamashita Y, Toshihide U, Takashima J, Nakajima T, et al. EML4-ALK mutations in lung cancer that confer resistance to ALK inhibitors. N Engl J Med. 2010;363:1734–9.
Camidge DR, Doebele RC. Treating ALK-positive lung cancer- early success and future challenges. Nat Rev Clin Oncol. 2012;9(5):267–77.
Toyokawa G, Seto T. Updated evidence on the mechanisms of resistance to ALK inhibitors and strategies to overcome such resistance: clinical and preclinical data. Oncol Res Treat. 2015;38:291–8.
Sullivan I, Planchard D. ALK inhibitors in non-small-cell lung cancer: the latest evidence and developments. Ther Adv Med Oncol. 2016;8(1):32–47.
Costa DB, Kobayashi S, Pandya SS, Yeo WL, Shen Z, Tan W, et al. CSF concentration of the anaplastic lymphoma kinase inhibitor crizotinib. J Clin Oncol. 2011;29:e443–5.
Rolfo C, Passiglia F, Castiglia M, Raez LE, Germonpre P, Gil-Bazo I, et al. ALK and crizotinib: after the honeymoon…what else? Resistance mechanisms and new therapies to overcome it. Transl Lung Cancer Res. 2014;3(4):250–61.
Steuer C, Ramalingam S. ALK positive non-small cell lung cancer, mechanisms of resistance and emerging treatment options. Cancer. 2014;120:2392–402.
Sasaki T, Koivunen J, Ogino A, Yanagita M, Nikiforow S, Zheng W, et al. A novel ALK secondary mutation and EGFR signaling cause resistance to ALK kinase inhibitors. Cancer Res. 2011;71:6051–60.
Katayama R, Shaw AT, Khan TM, Mino-Kenudson M, Solomon B, Halmos B, et al. Mechanisms of acquired Crizotinib resistance in ALK-rearranged lung cancers. Sci Transl Med. 2012;4:120ra17.
Doebele RC, Pilling AB, Aisner DL, Kutateladze TG, Le AT, Weickhardt AJ, et al. Mechanisms of resistance to crizotinib in patients with ALK gene rearranged non-small cell lung cancer. Clin Cancer Res. 2012;18:1472–82.
Sasaki T, Okuda K, Zheng W, Butrynski J, Capelletti M, Wang L, et al. The neuroblastoma associated F1174L mutation causes resistance to an ALK kinase inhibitor in ALK translocated cancers. Am Assoc Cancer Res. 2010. doi:10.1158/0008-5472.CAN-10-2956.
Heuckmann JM, Holzel M, Sos ML, Heynck S, Balke-Want H, Koker M, et al. ALK mutations conferring differential resistance to structurally diverse ALK inhibitors. Clin Cancer Res. 2011;17(23):7394–401.
Maione P, Sacco PC, Sgambato A, Casaluce F, Rossi A, Gridelli C. overcoming resistance to targeted therapies in NSCLC: current approaches and clinical application. Ther Adv Med Oncol. 2015;7(5):263–73.
Isozaki H, Takigawa N, Kiura K. Mechanisms of acquired resistance to ALK inhibitors and the rationale for treating ALK-positive lung cancer. Cancers. 2015;7:763–83.
Yamaguchi N, Lucena-Araujo AR, Nakayama S, Figueiredo-Pontes L, Gonzalez DA, Yasuda H, et al. Dual ALK and EGFR inhibition targets a mechanism of acquired resistance to the TKI crizotinib in ALK rearranged lung cancer. Lung Cancer. 2014;83(1):37–43.
Awad M, Katayama R, McTigue M, Liu W, Deng YL, Brooun A, et al. Acquired resistance to crizotinib from a mutation in CD74-ROS1. N Engl J Med. 2013. doi:10.1056/NEJMoa1215530.
Tanizaki J, Okamoto I, Okabe T. Activation of HER family signaling as a mechanism of acquired resistance to ALK inhibitors in EML4-ALK-positive non-small cell lung cancer. Clin Cancer Res. 2012. doi:10.1158/1078-0432.
Cha YJ, Cho BC, Kim HR, Lee HJ, Shim HS. A case of ALK-rearranged adenocarcinoma with small cell carcinoma-like transformation and resistance to crizotinib. J Thorac Oncol. 2015;11(5):e55–8.
Nix N, Brown K. Ceritinib for ALK-rearrangement-positive non-small-cell lung cancer. J Adv Pract Oncol. 2015;6:156–60.
Raedler L. Zykadia (ceritinib) approved for patients with crizotinib-resistant ALK-positive non-small cell lung cancer. Am Health Drug Benef. 2015;8:163–6.
Khozin S, Blumenthal GM, Zhang L, Tang S, Brower M, Fox E, et al. FDA approval: ceritinib for the treatment of metastatic anaplastic lymphoma kinase-positive non-small cell lung cancer. Am Assoc Cancer Res. 2015. doi:10.1158/1078-0432.CCR-14-3157.
Shaw AT, Kim DW, Mehra R, Tan DSW, Felip E, Chow LQM, et al. Ceritinib in ALK-rearranged non-small-cell lung cancer. N Engl J Med. 2014;370:1189–97.
Kim DW, Mehra R, Tan DSW, Felip E, Chow LQM, Camidge R, et al. Activity and safety of ceritinib in patients with ALK-rearranged non-small-cell lung cancer (ASCEND-1): updated results from the multicentre, open-label, phase 1 trial. Lancet Oncol. 2016;17(4):452–63.
Mok T, Spiegel D, Felip E, deMarinis F, Ahn MJ, Groen HJM, et al. ASCEND-2: a single-arm, open-label, multicenter phase II study of ceritinib in adult patients with ALK-rearranged(ALK+) non-small cell lung cancer previously treated with chemotherapy and crizotinib. J Clin Oncol. 2015;33:8059.
Felip E, Orlov S, Park K, Yu CJ, Tsai CM, Nishio M, et al. ASCEND-3: a single-arm, open-label, multicenter phase II study of ceritinib ALKi-naïve adult patients with ALK-rearranged (ALK+) non-small cell lung cancer. J Clin Oncol. 2015;33:8060.
El-Osta H, Shackelford R. Personalized treatment options for ALK-positive metastatic non-small-cell lung cancer: potential role for ceritinib. Pharmacogen Pers Med. 2015;8:145–54.
Friboulet L, Li N, Katayama R, Lee CC, Gainor JF, Crystal AS, et al. The ALK inhibitor ceritinib overcomes crizotinib resistance in non-small-cell lung cancer. Cancer Discov. 2014;4:662–73.
Toyokawa G, Inamasu E, Shimamatsu S, Yoshida T, Nosaki K, Hirai F, et al. Identification of a novel ALK G1123S mutation in a patient with ALK rearranged NSCLC exhibiting resistance to ceritinib. J Thorac Oncol. 2015;10(7):55–7.
Dong X, Fernandez-Salas E, Li E, Wang S. Elucidation of resistance mechanisms to second-generation ALK inhibitors alectinib and ceritinib in non-small-cell lung cancer cells. Neoplasia. 2016;18(3):162–71.
Katayama R, Sakashita T, Yanagitani N, Ninomiya H, Horiike A, Friboulet L, et al. P-glycoprotein mediates ceritinib resistance in anaplastic lymphoma kinase-rearranged non-small-cell lung cancer. EBioMedicine. 2016;3:54–66.
Iragavarapu C, Mustafa M, Akinleye A, Furqan M, Mittal V, Cang S, et al. Novel ALK inhibitors in clinical use and development. J Hematol Oncol. 2015;8:17.
Larkins E, Blumenthal GM, Chen H, He K, Agarwal R, Gieser G, et al. FDA approval: alectinib for the treatment of metastatic ALK positive non-small cell lung cancer following crizotinib. Clin Cancer Res. 2016. doi:10.1158/1078-0432.CCR-16-1293.
Lovly C. Combating acquired resistance to tyrosine kinase inhibitors in lung cancer. Am Soc Clin Oncol Educ Book. 2015;e165–e173. doi:10.14694/EdBook_AM.2015.35.e165.
Seto T, Kiura K, Nishio M, Nakagawa K, Maemondo M, Inoue A, et al. Alectinib for patients with ALK-rearranged advanced non-small-cell lung cancer (AF 001JP study): a single-arm, open-label, phase 1-2 study. Lancet Oncol. 2013;14:590–8.
Tamura T, Seto T, Nakagawa K, Maemondo M, Inoue A, Hida T, et al. Updated data of a phase 1-2 study (AF001JP) of alectinib, a CNS-penetrant, highly selective ALK inhibitor in ALK-rearranged advanced NSCLC. Radiat Oncol. 2014;90:S6.
Ou SHI, Ahn JS, De Petris L, Govindan R, Yang JCH, Hughes B, et al. Alectinib in crizotinib-refractory ALK-rearranged non-small-cell lung cancer: a phase II global study. J Clin Oncol. 2015;33:1–8.
Shaw AT, Gandhi L, Gadgeel S, Riely GJ, Cetnar J, West H, et al. Alectinib in ALK-positive, crizotinib-resistant, non-small-cell lung cancer: a single-group, multicentre, phase 2 trial. Lancet Oncol. 2015;17(2):234–42.
Katayama R, Friboulet L, Koike S, Lockerman EL, Khan TM, Gainor JF, et al. Two novel ALK mutations mediate acquired resistance to the next generation ALK inhibitor alectinib. Clin Cancer Res. 2014. doi:10.1158/1078-0432.CCR-14-1511.
Ou SH, Milliken JC, Azada MC, Miller VA, Ali SM, Klempner SJ. ALK, F1174V mutation confers sensitivity while ALK I1171 mutation confers resistance to alectinib. The importance of serial biopsy post progression. Lung Cancer. 2016;91:70–2.
Ou SHI, Azada M, Hsiang DJ, Herman JM, Kain TS, Siwak-Tapp C, et al. Next-generation sequencing reveals a novel NSCLC ALK F1174V mutation and confirms ALK G1202R mutation confers high-level resistance to Alectinib in ALK-rearranged NSCLC patients who progressed on crizotinib. J Thorac Oncol. 2014;9:549–53.
Toyokawa G, Seto T, Takenoyama M, Ichinose Y. Crizotinib can overcome acquired resistance to CH5424802. Is amplification of the MET gene a key factor? J Thorac Oncol. 2014;9(3):e27–8.
Isozaki H, Hotta K, Ichihara E, Takigawa N, Ohashi K, Kubo T, et al. Protocol design for the bench to bed trial in alectinib-refractory non-small-cell lung cancer patients harboring the EML4-ALK fusion gene (ALRIGHT/OLCSG1405). Clin Lung Cancer. 2016. doi:10.1016/j.cllc.2016.05.005.
Fujita S, Masago K, Katakami N, Yatabe Y. Transformation to SCLC after treatment with the ALK inhibitor alectinib. J Thorac Oncol. 2016;11(6):e67–72.
Romanidou O, Landi L, Cappuzzo F, Califano R. Overcoming resistance to first/second generation EGFR TKIs and ALK inhibitors in oncogene-addicted advanced non-small cell lung cancer. Ther Adv Med Oncol. 2016;8:176–87.
Ou SHI, Janne PA, Bartlett CH, Tang Y, Kim DW, Otterson GA, et al. Clinical benefit of continuing ALK inhibition with crizotinib beyond initial disease progression in patients with advanced ALK-positive NSCLC. Ann Oncol. 2014;25(2):415–22.
Peters S. Emerging options after progression during crizotinib therapy. J Clin Oncol. 2015. doi:10.1200/JCO.2015.65.1406.
Gadgeel SM, Gandhi L, Riely GJ, Chiappori AA, West HL, Azada MC, et al. Safety and activity of Alectinib against systemic disease and brain metastases in patients with Crizotinib-resistant ALK-rearranged non-small-cell lung cancer (AF 002JG): results from the dose finding portion of a phase 1–2 study. Lancet Oncol. 2014;15:1119–28.
Kim YH, Ozasa H, Nagai H, Sakamori Y, Yoshida H, Yagi Y, et al. High-dose crizotinib for brain metastases refractory to standard-dose crizotinib. J Thorac Oncol. 2013;8(9):85–6.
Felip E, Crino L, Kim DW, Spigel DR, Nishio M, Mok T, et al. Whole body and intracranial efficacy of ceritinib in patients with crizotinib pretreated, ALK-rearranged non-small-cell lung cancer and baseline brain metastases. Results from ASCEND-1 and ASCEND-2 trials. J Thorac Oncol. 2016;11:S57–166.
Ou SH, Shaw AT, Govindan R, Socinski M, Camidge R, De Petris L, et al. Pooled analysis of CNS response to alectinib in two studies of pre-treated ALK+ NSCLC. 16th WCLC-IACLC. 2015.
Gainor JF, Chi AS, Logan J, Hu R, Oh KS, Brastianos PK, et al. Alectinib dose escalation reinduces central nervous system responses in patients with anaplastic lymphoma kinase-positive NSCLC relapsing on standard dose alectinib. J Thorac Oncol. 2015;11(2):256–60.
Gainor J, Sherman CA, Willoughby K, Logan J, Kennedy E, Brastianos PK, et al. Alectinib salvages CNS relapses in ALK-positive lung cancer patients previously treated with crizotinib and ceritinib. J Thorac Oncol. 2015;10(2):232–6.
Tang SC, Nguyen LN, Sparidans RW, Wagenaar E, Beijnen JH, Shinkel AH. Increased oral availability and brain accumulation of the ALK inhibitor crizotinib by coadministration of the P-glycoprotein (ABCB1) and breast cancer resistance protein (ABCG2) inhibitor elacridar. Int J Cancer. 2014;134:1484–94.
Johung KL, Yeh N, Desai NB, Williams TM, Lautenshlaeger T, Arvold ND, et al. Extended survival and prognostic factors for patients with ALK-rearranged non-small-cell lung cancer and brain metastasis. J Clin Oncol. 2015;34(2):123–9.
Weickhardt AJ, Scheier B, Burke JM, Gan G, Lu X, Bunn PA, et al. Local ablative therapy of oligoprogessive disease prolongs disease control by tyrosine kinase inhibitors in oncogene-addicted non-small-cell lung cancer. J Thorac Oncol. 2012;7(12):1807–14.
Squillace RM, Anjum R, Miller D, Vodala S, Moran L, Wang F, et al. AP 26113 possesses pan-inhibitory activity versus crizotinib-resistant ALK mutants and oncogenic ROS1 fusions. Cancer Res. 2013;73:5655.
Wu J, Savooji J, Liu D. Second- and third-generation ALK inhibitors for non-small cell lung cancer. J Hematol Oncol. 2016;9:19.
Facchinetti F, Tiseo M, Di Maio M, Graziano P, Bria E, Rossi G, et al. Tackling ALK in non-small cell lung cancer: the role of novel inhibitors. Transl Lung Cancer Res. 2016;5(3):301–21.
Liao BC, Lin CC, Shih JY, Yang JCH. Treating patients with ALK-positive non-small-cell lung cancer: latest evidence and management strategy. Ther Adv Med Oncol. 2015;7(5):274–90.
Li T, LoRusso P, Maitland ML, Ou SHI, Bahceci E, Ball HA, et al. First-in-human, open-label dose escalation and dose expansion study of the safety, pharmacokinetics, and antitumor effects of an oral ALK inhibitor ASP3026 in patients with advanced solid tumors. J Hematol Oncol. 2016;9:23.
Reckamp KL, Infante JR, Blumenschein GR, Wakelee HA, Carter CA, Gockerman JP, et al. Phase I/II trial of X-396, a novel anaplastic lymphoma kinase inhibitor, in patients with ALK+ non-small-cell lung cancer. J Thorac Oncol. 2016;11(2):S36–7.
Shaw AT, Friboulet L, Leshchiner I, Gainor JF, Bergqvist S, Brooun A, et al. Resensitization to crizotinib by the lorlatinib ALK resistance mutation L1198F. N Engl J Med. 2015. doi:10.1056/NEJMoa1508887.
Wang W, Jiang X, Song Z, Zhang Y. Patients harboring EGFR mutation after primary resistance to crizotinib and response to EGFR-TKI. OncoTargets Ther. 2016;9:211–5.
Lovly CM, Mc Donald NT, Chen H, Ortiz-Cuaran S, Heukamp LC, Yan Y, et al. Rationale for co-targeting IGF-1R and ALK in ALK fusion positive lung cancer. Nat Med. 2014;20(9):1027–34.
Tan DSW, Araujo A, Zhang J, Signorovitch J, Zhou ZY, Cai X, et al. Comparative efficacy of ceritinib and crizotinib as initial ALK-targeted therapies in previously treated advanced NSCLC: an adjusted comparison with external controls. J Thorac Oncol. 2016;11(9):1550–7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Research involving human participants and/or animals
This article does not contain any studies with human participants or animals performed by any of the authors.
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Drizou, M., Kotteas, E.A. & Syrigos, N. Treating patients with ALK-rearranged non-small-cell lung cancer: mechanisms of resistance and strategies to overcome it. Clin Transl Oncol 19, 658–666 (2017). https://doi.org/10.1007/s12094-016-1605-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12094-016-1605-y