Abstract
Objectives
To investigate the effect of external beam radiotherapy (EBRT) for head and neck cancer (HNC) the intimal–medial thickness (IMT) and the lumen of the carotid artery.
Methods
Patients with HNC and an indication for EBRT were enrolled. A carotid artery color Doppler examination was performed before and 6 and 12 months after EBRT.
Results
From 2008 to 2011, 50 patients were enrolled. The mean carotid IMT was 0.9 vs. 1.02 mm before and 6 months after EBRT, respectively (p = 0.0001). The common carotid artery lumen was narrowed without statistical significance, 6 months after EBRT (p = 0.3). 1 year from EBRT, the IMT increase and the lumen reduction were statistically significant (p = 0.001, p = 0.01, respectively). Neurological events (stroke or TIA) were not observed.
Conclusions
Our data showed a significant IMT increase 6 months from EBRT without a corresponding narrowing of the common carotid lumen while a significant increase 12 months after EBRT.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
External beam radiotherapy (EBRT) could produce damage to the carotid arteries because of endothelial alteration, periadventitial fibrosis, and obliteration of the vasa vasorum [1–6]. Patients who received EBRT to the head and neck area have a higher incidence of significant extracranial carotid artery stenosis [1–5].
Carotid plaque morphology has been shown to be an important factor to cause stroke; the risk of stroke for irradiated patients can be caused from the radiation-induced accelerated atherosclerotic process [6]. The relative contribution of wall fibrosis and intimal–medial thickness and its effect on luminal diameters is also unclear. Carotid stenosis develops some years after irradiation, and the efficacy of early intervention in asymptomatic patients is not defined. The natural history of asymptomatic carotid stenosis in these patients with head and neck tumors is unknown, and the treatment recommendations are uncertain due to the limited published data and the patients’ life expectancy.
Nevertheless, with modern therapies and knowledge [7, 8], the head and neck cancer long-term survivors increased and may benefit from stroke prevention procedures. Therefore, patients who would receive much more benefit from carotid plaque studies are those who have a long history of neck irradiation and an established degree of stenosis in their arteries.
The aim of this observational study was to investigate the effect of EBRT for head and neck cancer, on the intimal–medial thickness (IMT) and the diameter of the carotid artery.
Patients and methods
Patients
Patients aged more than 18, with histological proven head and neck cancer, receiving EBRT, were enrolled. From January 2008 to December 2011, a screening program for carotid stenosis was offered from the cardiology and radiotherapy department of our Institution, to all the irradiated patients with head and neck cancer.
External beam radiotherapy
Patients’ immobilization was obtained using a thermoplastic mask in supine position. A treatment planning CT (2.5 mm slice thickness) was acquired in the treatment position. All three-dimensional conformal EBRT treatments planning were performed with Treatment planning system eclipse 8.6 (Varian Medical System, Palo Alto, CA).
Total doses for the clinical target volumes (CTV) were as follows: 66–70 Gy to the macroscopic disease; 60 Gy to the high-risk microscopic disease clinical target volume; 50 Gy to the microscopic low-risk disease. Each CTV was expanded by 5 mm to the corresponding planning target volume.
Ultrasound examination
All patients underwent a carotid artery color flow Doppler examination in our vascular laboratory by Hitachi CVX 7.5 MHz. The color Doppler exams were performed before beginning EBRT and 6, 12 and 18 months after the end of EBRT.
The percent stenosis of the common carotid (CCA) and internal carotid (ICA) arteries were recorded using standard criteria based on peak systolic velocity and end diastolic velocity as well as ICA/CCA ratio.
Intimal–medial thickness measurement
A longitudinal view of the common and internal carotid artery was obtained separately using the duplex scanner and, stored and captured as described above.
The intimal–medial thickness (IMT) was determined by the far-wall measurements taken at the common carotid artery away from the atherosclerotic plaque and averaged over three readings on a magnified image. The maximal intimal–medial thickness of the far-wall and the minimal vessel lumen of the common carotid artery were determined.
Statistical analysis
The IMT and the common and internal carotid artery lumen values were calculated for all patients and evaluated by the Wilcoxon test. A value less than 0.05 was defined as significant.
Results
Patients
Fifty patients were enrolled in this study (Table 1): 41 men and 9 female with a median age of 65 years; 80 % of patients were smokers and drinkers. The major comorbidities were hypertension and diabetes, which were pharmacologically controlled.
Carotid arteries
One hundred carotid arteries were evaluated; considering that the arteries are in radiotherapy field for the neck irradiation, median dose was 62 Gy (range 50–70 Gy).
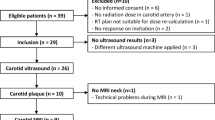
Table 2 represents the wall parameters for the evaluated patients. The mean carotid IMT value was 0.9 vs. 1.02 mm before and 6 months after EBRT, respectively (p = 0.0001). All patients were evaluated after 6 months from EBRT, and the common carotid arteries lumen was narrowed, but without statistical significance: its mean value was 6.43 vs. 6.27 mm, before and after EBRT, respectively (p = 0.3). As shown in Fig. 1, 30 patients had a follow-up more than 12 months, but only 15 patients (30 carotid arteries) were evaluated (5 refused, 7 patients died and 3 patients were lost at follow-up): the increase in IMT and the reduction of lumen were significant at 12 months from EBRT (0.81 vs. 1.06 mm, p = 0.001 and 6.65 vs. 6.2 mm, p = 0.01, respectively).
Only six patients (12 carotid arteries) were evaluated 18 months after EBRT and both IMT and lumen diameter were statistically different from those before EBRT (0.8 vs. 1.1 mm, p = 0.01 and 6.98 vs. 6.15 mm, p = 0.02, respectively).
Neurological events such as stroke or transient ischemic attack were not observed and patients are still followed up.
Discussion
Radiotherapy is frequently used as a curative treatment for head and neck malignancies. Radiation-induced toxicity has been described: radiation is an independent risk factor for cerebrovascular disease in cancer patients, due to the increasing risk of accelerated atherosclerosis and stenosis of the common and internal carotid arteries [1–5]. The mechanism of irradiation-induced carotid stenosis was a combination of direct vessel wall damage, intimal proliferation, necrosis of the media, periadventitial fibrosis, and accelerated atherosclerosis.
In arterioles, radiotherapy could produce myointimal proliferation, necrosis, and replacement with collagen and the lipid deposits [6].
Moreover, the increased risk of ischemic stroke after head and neck EBRT in patients under 60, has been documented with a relative risk of 5.6 compared with population rates [9].
Significant extracranial carotid artery disease was found in nasopharyngeal cancer patients who developed ischemic stroke post irradiation, patients are at risk of delayed diffuse atherosclerosis but they may develop carotid occlusion: a multifactorial origin of the lesions is the most probable cause of the neurologic events [10]. Experimental studies performed by Stewart et al. [11] showed that radiation leads to the formation of inflammatory vulnerable plaques, which are prone to rapture, causing a fatal stroke. Vascular lesions can cause neurologic events in irradiated patients, thus affecting quality of life and survival. This risk can last for more than 15 years, therefore a subclinical marker of vascular damage is warranted.
Cheng et al. [2] showed on 240 patients treated with head and neck irradiation that carotid stenosis (>70 %) occurred significantly in 12 % of patients. Another study on 290 patients (192 patients in RT group and 98 patients in control group), showed that radiotherapy increases the risk of carotid arteries stenosis >50 and >70 % (p = 0.001; p = 0.002, respectively) [4].
Thus, the aim of this analysis was to evaluate carotid arteries, in terms of IMT and reduction of lumen, in patients treated with EBRT of the neck. Our data are consistent with the other published data [1–5, 12], observing a significant reduction in diameter and an increase of intimal–medial thickness at 12 and 18 months after EBRT. The data published investigated the effect of EBRT on the morphology of atherosclerotic plaques and the intimal–medial thickness of the carotid artery between patients treated with EBRT and non irradiated controls. We have no control group in our study, but considering that the Los Angeles atherosclerosis study showed a mean IMT increase value of 0.0143 ± 0.0017 mm per year in normal sedentary patients aged 40–60 [13], we observed an IMT increase in our irradiated patients (mean increase: 0.1 mm at 6 months and 0.25 mm at 12 months).
In a prospective study involving 36 patients, Muzaffar [14] showed that EBRT significantly increases the carotid IMT during the first year after irradiation. Our data showed that IMT increases statistically at 18 months after EBRT compared with that at the first year (p = 0.01); this trend was observed also in patients controlled after 24 months, but they were only four.
Moreover, the common carotid IMT was associated with atherosclerosis and also with myocardial infarction and stroke, and there are many reports about the incidence rate of stroke after irradiation of head and neck [4, 15–18]. Elerding et al. [16] did not report a significantly different stroke incidence about RT group patients and controls (p = 0.39). Cheng et al. [2, 17] showed that 67 % of irradiate patients with carotid stenosis >70 %, experienced a stroke, while another study reported only 1 % of patients had a stroke [4]. Another study reported a low incidence of stroke after EBRT, underlining the important role of the routine screening for this setting of patients [18]. In our analysis no pathological–clinical events were observed, so, the clinical meaning of the IMT increase remains uncertain and only a longer follow-up will clarify whether it is a precursor of clinical neurologic events. Data from our observational study do not suggest that early evaluation of carotid arteries is useful to detect subclinical changes that may predict clinical events. It seems more reasonable to suggest evaluation after 1 year from EBRT.
Conclusion
Finally, despite the limitation of this study (sample size and lack of control group), our data showed that EBRT for head and neck cancer produces a thickening of the IMT with a significant reduction in carotid artery lumen at 12 and 18 months from irradiation.
At the moment, the relationship between radiotherapy and stroke or TIA is unknown and needs to be ascertained by the routine cardiologic and carotid artery follow-up of irradiated patients, starting at 1 year from EBRT. Further studies are necessary to define the dose constraints for the carotid arteries to prevent the side effects, as it happened for other organs at risk [19, 20].
References
Carmody BJ, Arora S, Avena R, Curry KM, Simpkins J, Cosby K, et al. Accelerated carotid artery disease after high-dose head and neck radiotherapy: is there a role for routine carotid duplex surveillance? J Vasc Surg. 1999;30:1045–51.
Cheng SW, Wu LL, Ting AC, Lau H, Lam LK, Wei WI. Irradiation-induced extracranial carotid stenosis in patients with head and neck malignancies. Am J Surg. 1999;178:323–8.
Cheng SWK, Ting ACW, Wu LLH. Accelerated progression of carotid stenosis in patients with previous external neck irradiation. J Vasc Surg. 2004;39:409–15.
Chang YJ, Chang TC, Lee TC, Ryu SJ. Predictors of carotid artery stenosis after radiotherapy for head and neck cancers. J Vasc Surg. 2009;50:280–5.
Cheng SWK, Ting ACW, Wu LLH. Ultrasonic analysis of plaque characteristics and intimal–medial thickness in radiation-induced atherosclerosis carotid artery. Eur J Endovasc Surg. 2002;24:499–504.
Fajardo LF. Is the pathology of radiation injury different in small vs large blood vessel? Cardiovasc Radiat Med. 1999;1:108–10.
Pedicini P, Caivano R, Jereczek-Fossa BA, Strigari L, Vischioni B, Alterio D, et al. Modelling the correlation between EGFr expression and tumour cell radiosensitivity, and combined treatments of radiation and monoclonal antibody EGFr inhibitors. Theor Biol Med Model. 2012;9:37.
Bonner JA, Harari PM, Giralt J, Cohen RB, Jones CU, Sur RK, et al. Radiotherapy plus cetuximab for locoregionally advanced head and neck cancer: 5-year survival data from a phase III randomised trial, and relation between cetuximab-induced rash and survival. Lancet Oncol. 2010;11:21–8.
Dorresteijn LDA, Kappelle AC, Boogerd W, Klokman WJ, Balm AJ, Keus RB, et al. Increased risk of ischemic stroke after radiotherapy on the neck in patients younger than 60 years. J Clin Oncol. 2002;20:282–8.
Li CS, Schminke U. Tan TY Extracranial carotid artery disease in nasopharyngeal carcinoma patients with post-irradiation ischemic stroke. Clin Neurol Neurosurg. 2010;112:865–8.
Stewart FA, Hoving S, Russel NS. Vascular damage as an underlying mechanism of cardiac and cerebral toxicity in irradiated cancer patients. Radiation Res. 2010;174:865–9.
Gianicolo ME, Gianicolo EA, Tramacere F, Andrenassi MG, Portaluri M. Effects of external irradiation of the neck region on intima media thickness of the common carotid artery. Cardiovasc Ultrasound. 2010;8:8.
Nordstrom CK, Dwyer KM, Merz NB, Shircore A, Dwyer JH. Leisure time physical activity and early atherosclerosis: the Los Angeles atherosclerosis study. Am J Med. 2003;115:19–25.
Muzzafar K, Collins SL, Labropoulos N, Baker WH. A prospective study of the effects of irradiation on the carotid artery. Laryngoscope. 2000;111:1811–4.
O’leary DH, Polak JF, Kronmal RA, Manolio TA, Burke GL, Wolfson SK. Carotid-artery intima and media thickness as a risk factor for myocardial infarction and stroke in older adults. N Engl J Med. 1999;340:14–22.
Elerding SC, Fernandez RN, Grotta JC, Lindberg RD, Causay LC, McMurtrey MJ. Carotid artery disease following external cervical irradiation. Ann Surg. 1981;194:609–15.
Cheng SW, Ting AC, Lam LK, Wei WI. Carotid stenosis after radiotherapy for nasopharyngeal carcinoma. Act Otolaryngol Head Neck Surg. 2000;126:517–21.
Lam WW, Leung SF, So NM, Wong KS, Liu KH, Ku PK, et al. Incidence of carotid stenosis in nasopharyngeal carcinoma patients after radiotherapy. Cancer. 2001;92:2357–63.
Fiorentino A, Cozzolino M, Caivano R, Pedicini P, Chiumento C, Oliviero C, et al. Cone-beam computed tomography dose monitoring during intensity-modulated radiotherapy in head and neck cancer: parotid glands. Clin Transl Oncol. 2012;. doi:10.1007/s1209401209464.
Fiorentino A, Caivano R, Metallo V, Chiumento C, Cozzolino M, Califano G, et al. Parotid gland volumetric changes during intensity-modulated radiotherapy in head and neck cancer. Br J Radiol. 2012;85:1415–9.
Conflict of interst
The authors declared no conflict of interests.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Faruolo, M., Fiorentino, A., Gallucci, G. et al. Intimal–medial thickness and carotid arteries lumen in irradiated patients for head and neck cancer: preliminary data of an observational study. Clin Transl Oncol 15, 861–864 (2013). https://doi.org/10.1007/s12094-013-1023-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12094-013-1023-3