Abstract
Objectives
To study the carotid artery plaque composition and its volume changes in a group of patients at baseline and 2 years after head and neck radiation therapy treatment (HNXRT).
Methods
In this retrospective study, 62 patients (41 males; mean age 63 years; range 52–81) who underwent HNXRT and 40 patients (24 males; mean age 65) who underwent surgical resection of neoplasm and did not undergo HNXRT were assessed, with 2-year follow-up. The carotid artery plaque volumes, as well as the volume of the sub-components (fatty-mixed-calcified), were semiautomatically quantified. Mann-Whitney and Wilcoxon tests were used to test the hypothesis.
Results
In the HNXRT group, there was a statistically significant increase in the total volume of the carotid artery plaques (from 533 to 746 mm3; p = 0.001), in the fatty plaques (103 vs. 202 mm3; p = 0.001) and mixed plaque component volume (328 vs. 419 mm3; p = 0.034). A statistically significant variation (from 21.8 % to 27.6 %) in the percentage of the fatty tissue was found.
Conclusions
Results
of this preliminary study suggest that HNXRT promotes increased carotid artery plaque volume, particularly the fatty plaque component.
Key Points
• HNXRT increases carotid plaque volume.
• Plaque volume increase is mainly due to increase.in fatty plaque component
• Patients who undergo HNXRT have a progression of carotid artery disease.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The first association between radiation and vascular injury was observed in 1899 [1], and since its first histological description, several researches have tried to identify the effects of radiation on the vessels [2, 3]. Studies have shown that radiation-induced vasculopathy is a cause of ischemic stroke in patients who have undergone head and neck radiation therapy (HNXRT) for the treatment of malignancy [4–6].
In the past, chronic radiation vasculopathy was quite uncommon, as patients would often die from their pathology before the condition manifested itself [7, 8]. Today, however, thanks to improvements in head and neck cancer treatment, a significant number of patients are now “outliving” their malignancies, with increased presentation of the long-term effects of treatment, such as radiation-induced vasculopathy [9].
The degree of carotid artery stenosis is considered the most important parameter associated with the risk of cerebrovascular events, and for this reason, studies investigating radiation-induced carotid vasculopathy have used this parameter as an endpoint to assess vascular damage [10, 11]. However, in the neurovascular field, new evidence has demonstrated that in addition to the degree of luminal stenosis, certain plaque-related parameters are significant contributors to the risk of cerebrovascular events [12–15]. In particular, the volume and composition of the carotid artery plaque seem to be significantly related to increased vulnerability and risk of rupture [16, 17].
The purpose of this longitudinal study was to evaluate variations in carotid artery plaque composition and volume using multi-detector-row computed tomography (MDCT) in a group of patients before and two years after HNXRT.
Materials and methods
Study design and patient population
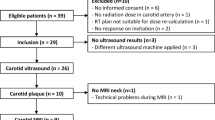
Institutional review board approval was obtained for this retrospective single-centre longitudinal study. Since it was a retrospective study, informed consent of the patients was waived. All patients who underwent HNXRT from January 2007 to January 2011 and had a 2-year follow-up were included in this study (with an allowed time range of ± 2 weeks). Inclusion criteria were the presence of MDCT before and 2 years after HNXRT. Patients for whom imaging or artefact scores were low (scores of 1 or 2) were excluded from the analysis.
Sixty-two patients (41 males and 21 females; mean age 64 years; age range 52–81 years) fulfilled the inclusion criteria for the study. From each patient chart, the following data were collected: age, sex, primary tumour, timing of RT, cerebrovascular risk factors (smoking, hypertension, diabetes mellitus [DM], and dyslipidaemia). The study also considered the occurrence of cerebrovascular symptoms.
Essential hypertension was defined as diastolic blood pressure (DBP) that twice exceeded 95 mmHg or that was treated with blood pressure-lowering drugs. Diabetes was indicated by abnormal fasting plasma glucose levels (>7.9 mmol/l) or the current use of insulin or an oral hypoglycaemic agent. Dyslipidaemia was defined as abnormal fasting plasma cholesterol (low-density lipoprotein cholesterol) levels (fasting cholesterol > 6.5 mmol/l) or the current use of lipid-lowering agents. Cigarette smoking status was scored positive when the patient was currently smoking or had quit smoking less than 2 years before the last follow-up.
Data obtained were compared with a population of 40 subjects who underwent surgical resection of neoplasm of the neck that did not require HNXRT and who underwent follow-up MDCT after 2 years. We included only patients who underwent surgical therapy alone (no chemotherapy or HNXRT). We also excluded patients who developed other neoplasms during the 2-year follow-up.
Classification of cerebrovascular symptoms
Vascular risk factors and coexisting comorbidities and treatment known before stroke or transient ischemic attack (TIA) are systematically recorded at our institution, and the Trial of Org 10172 in Acute Stroke Treatment (TOAST) criteria were used to classify the causes of stroke [18]. The criterion for stroke was the presence of a fixed neurologic deficit lasting for more than 24 hours whereas, TIA was considered when symptoms lasted for less than 24 hours. Subarachnoid and intra-cerebral haemorrhages were excluded. For each case, the clinical diagnosis was based on a neurologic examination and was confirmed with CT.
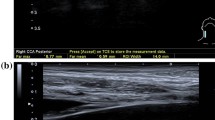
MDCT technique
All patients underwent MDCT of the head and neck with a 16-detector row CT system (Brilliance, Philips Medical Systems, Eindhoven, Netherlands). A non-enhanced image was acquired, followed by a contrast-material phase. In the head and neck cancer analysis, the region of interest (ROI) trigger threshold was placed into the aortic arch, and the monitor scanning started 6 s after the beginning of i.v. administration of 80–130 ml of pre-warmed contrast medium (Ultravist 370; Bayer AG, Leverkusen, Germany) into the median cubital vein (flow rate of 2.5 ml/s). The trigger threshold was set at + 80 Hounsfield units (HU) above the baseline. Sixty seconds after the threshold was reached, the venous phase started. CT technical parameters were as follows: matrix 512 × 512, field of view 14–19 cm; slice thickness 0.6 mm, interval 0.3 mm, 180–220 mAs; 120–140 kV. A C-filter algorithm of reconstruction was applied.
Volume of plaque and its components
In this study, we measured the volume of carotid artery plaque as well as that of its subcomponents. For semi-automatic quantification of the different plaque components in CT images, the polymeasure plug-in for the software package ImageJ (Rasband, WS, ImageJ, U. S. National Institutes of Health, Bethesda, MD, USA, http://imagej.nih.gov/ij/, 1997–2014) was used [19, 20]. With this software, it is possible to first delineate the inner and outer wall boundaries of the vessel, and then to calculate the volume of the plaque and its subcomponents based on the specific region of interest. Following this, the total number of voxels and the number of voxels of different ranges of HU values within these ROIs is calculated. The following voxel thresholds were used to classify different components of plaque: lipids, < 60 HU; fibrous tissue, 60–130 HU; and calcium tissue, > 130 HU [21, 22].
Evaluation of carotid image quality and artefacts
Evaluation of image quality and artefacts was performed by two radiologists with 9 and 12 years of experience in neurovascular imaging. The readers were blinded to patients’ symptoms, and were asked to assess overall image quality on a five-point scale, where 5 corresponded to excellent quality and 1 represented unacceptable image quality. Values 1 and 2 included cases in which the carotid artery wall did not show a well-defined cleavage plan with nearby structures. In these cases, it was not possible to clearly observe the outer carotid artery wall, thus making it impossible to correctly trace the plaque’s profile.
The readers were also asked to assess the impact of image artefacts on a five-point scale. On this scale, 5 corresponded to the complete absence of imaging artefacts; 4 represented mild artefacts, not interfering with diagnostic decision-making; 3 represented moderate artefacts, slightly interfering with diagnostic-decision making; 2 represented pronounced artefacts, interfering with diagnostic decision-making (though it was still possible to arrive at a diagnosis); and 1 designated a situation in which artefacts completely hindered diagnostic decision-making. Patients with image quality scores of 1 and 2 and image artefact scores of 1 and 2 were excluded from the evaluation.
Statistical analysis
The normality of each continuous variable group was tested using the Kolmogorov–Smirnov Z test. Continuous data were described as the mean value ± SD. Mann–Whitney and Wilcoxon tests were used when normality was rejected, whereas student t tests for paired and unpaired groups were applied when normality was accepted. Inter-observer agreement was calculated using the Cohen weighted kappa test. Values of 0–0.2 were considered poor agreement; 0.21–0.4, fair agreement; 0.41–0.6, moderate agreement; 0.61–0.8, substantial agreement; and 0.81–1.0, almost perfect or perfect agreement. A p value < 0.05 was considered to indicate statistical significance, and all values were calculated using a two-tailed significance level. R software (www.r-project.org) was employed for statistical analyses.
Results
General results
No patients were excluded for suboptimal image quality or artefacts. Among the 102 patients, the average image quality score was 4.24 (range 3–5) and the average artefact score was 4.65 (range 3–5). Inter-rater agreement between the two radiologists was analysed using Cohen’s kappa, and we found kappa values of 0.756 and 0.814 for image quality and image artefacts, respectively. Demographic and clinical characteristics are given in the Table 1. At baseline analysis (before HNXRT or surgery), no statistically significant differences were found for cardiovascular risk factors or in plaque and subcomponent volume. In the HNXRT subgroup, there were four cases of cerebrovascular events, whereas in the surgical subgroup, we encountered two cerebrovascular events.
Plaque volume analysis
The plaque volumes (total and subcomponents; Figs. 1 and 2) are summarized in Table 2, and the subcomponent percentages are given in Table 3. By performing Wilcoxon analysis before and after therapy we found that in the group of patients who underwent HNXRT (Table 4), there was a statistically significant increase in the total carotid artery plaque volume (from 533 to 746 mm3; p = 0.001) and also a statistically significant increase in fatty component volume (103 vs. 202 mm3; p = 0.001) and mixed component volume (328 vs. 419 mm3; p = 0.034). No statistically significant difference was found in the volume of calcified tissue. In analysing the variation among percentages of the three components, we found that only the lipid component showed a statistically significant variation (21.8–27.6 %).
Panels a–b: MDCT axial image of a 64-year-old male patient before (a) and 2 years after (b) surgery. Volumetric analysis in the right carotid artery (white arrow) is visible, and the different colours represent the lipid, mixed, and calcified tissues (yellow = lipid; red = mixed; blue = calcified; green = opacified lumen). In the small panel, 200 % magnification of the carotid is shown (white arrowhead). Panels c–d: MDCT axial image of a 69-year-old male patient before (c) and 2 years after (d) HNXRT. The same colour code is applied for the lipid, mixed, and calcified tissues (yellow = lipid; red = mixed; blue = calcified; green = opacified lumen)
Box-plot analysis of the variation of plaque components (fatty–mixed–calcified). Panel a: volume analysis before and after HNXRT. Panel b: volume analysis after surgery. Panel c: percentage variation of plaque components before and after HNXRT. Panel d: percentage variation of plaque components before and after surgery
In the group of patients who underwent only surgical therapy (Table 4), no statistically significant variation was found in total plaque volume (463 vs. 527 mm3) or in absolute percentage of the plaque subcomponents, whereas there was a statistically significant variation in the volume of the calcium component, with a significant increase (114 vs. 153 mm3).
Degree of stenosis
We also assessed the variation in degree of stenosis. In the HNXRT group, There was a strong statistically significant increase in the degree of stenosis (from 40.2 % to 49.5 %; p = 0.001). A statistically significant difference was also found in patients treated with surgery (37.9 % vs. 40.8 %; p = 0.0214).
Discussion
Previously published papers have demonstrated that radiation therapy (RT) negatively affects the vascular system by promoting atherosclerosis [9, 23, 24]. Small arteries are generally considered the most vulnerable vessels with regard to endothelial cell injury. Damage in the medium and large arteries (external diameters >100 and >500 μm, respectively) [25] occurs less frequently, and two different types of lesions have been described: acute rupture and chronic vasculopathy [26]. Vessel rupture nowadays is rare [27].
Researchers have observed that chronic vasculopathy is indicative of accelerated atherosclerotic disease in vessels close to organs targeted for RT [9]. Previous studies have demonstrated increased carotid artery stenosis in patients treated with HNXRT, which is of clinical significance [28]. In the past, however, arterial damage was quantified by evaluating the degree of carotid artery stenosis [10, 11, 23, 28–30]. In fact, this was considered the most important parameter for classifying the risk of carotid-related cerebrovascular events [31, 32]. However, several imaging and pathological studies have recently demonstrated that the degree of carotid artery stenosis is only one of the parameters related to the risk of plaque rupture, and that the composition and volume of the plaque play a critical role in its vulnerability or stability [12, 16, 17, 20, 29].
In this study, we compared the HNXRT group with subjects who underwent only surgery, while ensuring that they had similar cardiovascular risk factors (Table 1). In patients treated with HNXRT, there were four cases of cerebrovascular events, and in the cohort of patients treated with the surgical approach alone, two cerebrovascular events occurred; these numbers are too small to draw any conclusions, and the control cohort was smaller than the HNXRT cohort. The occurrence of cerebrovascular events after HNXRT is a well-recognized consequence of carotid artery wall damage [30, 31] and the prevalence found in our study is similar to that in the literature. We would note, however, that the group undergoing RT tended to have more markers associated with vascular disease such as smoking, dyslipidaemia and pretreatment plaque size; while these differences individually are not significant, in combination, they may influence the progression of atherosclerosis.
The main focus of this longitudinal study was the assessment of the volume and composition of plaque, and we found some intriguing results. First, in patients treated with HNXRT, there was a statistically significant increase in plaque volume after 2 years (from 533 to 746 mm3; p = 0.001), whereas no statistically significant difference was found in the group of patients treated with surgery alone (463 vs. 527 mm3). These findings support the hypothesis of increased plaque vulnerability after HNXRT, as some authors have suggested that the volume of plaque is a stronger indicator of cerebrovascular risk via the degree of stenosis [20].
However, in our opinion, the most interesting finding of this study is the difference in behaviour among the plaque components. In the HNXRT group, there was a strong statistically significant increase in the fatty component volume (103 vs. 202 mm3; p = 0.001) and also an increase, albeit more subtle, in the mixed component volume (328 vs. 419 mm3; p = 0.034). In the analysis of variations in percentages among the three components, only the fatty component showed a statistically significant variation (from 21.8 % to 27.6 %). These results suggest that radiation treatment promotes specific routes of atherosclerosis that increase the plaque lipid pool; in MDCT, the fatty plaques identify the lipid-rich necrotic core and frequently intra-plaque haemorrhages as well as macrophages and inflammatory cells [32, 33]. Previous studies have demonstrated that the fatty component is significantly associated with the risk of cerebrovascular events. A key observation in our study was that among the group of patients who underwent only surgery, one component—i.e. calcified tissue—showed a statistically significant increase (114 vs. 153 mm3), while no variations in the percentage of the subcomponents were found.
With regard to the degree of stenosis, in the group of patients who underwent HNXRT, we found a strong statistically significant increase in the degree of stenosis (from 40.2 % to 49.5 %; p = 0.001), and a statistically significant difference was also present in patients treated with surgery (37.9 % vs. 40.8 %; p = 0.0214).
We acknowledge that there were limitations to our study. First, this was a retrospective evaluation, and a prospective longitudinal study is needed to validate our observations. However, we think that our data was not biased, since the methodology was homogeneous. Second, our findings are based on a relatively small group of patients, and our data need to be confirmed in larger studies in other populations at risk, and should be considered as preliminary results.
Conclusions
The results of this preliminary study suggest that HNXRT is associated with an increase in the volume of carotid artery plaque, and particularly of the fatty component. Moreover, we found that HNXRT was also associated with an increase in absolute lipid percentage of plaque.
References
Gassmann A (1899) Zur histologie der rontgenulcera. Fortschritte Gebiete Röntgenstrahlen Nuklearmedizin Ergänzungsband 2:199–207
Dorresteijn LD, Kappelle AC, Boogerd W, Klokman WJ, Balm AJ, Keus RB, van Leeuwen FE, Bartelink H (2002) Increased risk of ischemic stroke after radiotherapy on the neck in patients younger than 60 years. J Clin Oncol 20:282–288
Silverberg GD, Britt RH, Goffinet DR (1978) Radiation-induced carotid artery disease. Cancer 41:130–137
Haynes JC, Machtay M, Weber RS, Weinstein GS, Chalian AA, Rosenthal DI (2002) Relative risk of stroke in head and neck carcinoma patients treated with external cervical irradiation. Laryngoscope 112:1883–1887
Kang JH, Kwon SU, Kim JS (2002) Radiation-induced angiopathy in acute stroke patients. J Stroke Cerebrovasc Dis 11:315–319
Abayomi OK (2004) Neck irradiation, carotid injury and its consequences. Oral Oncol 40:872–878
Brant-Zawadzki M, Anderson M, DeArmond SJ, Conley FK, Jahnke RW (1980) Radiation-induced large intracranial vessel occlusive vasculopathy. AJR Am J Roentgenol 134:51–55
Zidar N, Ferluga D, Hvala A, Popović M, Soba E (1997) Contribution to the pathogenesis of radiation-induced injury to large arteries. J Laryngol Otol 111:988–990
Jordan LC, Duffner PK (2009) Early-onset stroke and cerebrovascular disease in adult survivors of childhood cancer. Neurology 73:1816–1817
Dorth JA, Patel PR, Broadwater G, Brizel DM (2014) Incidence and risk factors of significant carotid artery stenosis in asymptomatic survivors of head and neck cancer after radiotherapy. Head Neck 36:215–219
Greco A, Gallo A, De Virgilio A, Marinelli C, Macri GF, Fusconi M, Pagliuca G, de Vincentiis M (2012) Carotid stenosis after adjuvant cervical radiotherapy in patients with head and neck cancers: a prospective controlled study. Clin Otolaryngol 37:376–381
Truijman MT, Kooi ME, van Dijk AC, de Rotte AA, van der Kolk AG, Liem MI, Schreuder FH, Boersma E, Mess WH, van Oostenbrugge RJ, Koudstaal PJ, Kappelle LJ, Nederkoorn PJ, Nederveen AJ, Hendrikse J, van der Steen AF, Daemen MJ, van der Lugt A (2013) Plaque At RISK (PARISK): prospective multicenter study to improve diagnosis of high-risk carotid plaques. Int J Stroke. doi:10.1111/ijs.12167
Saba L, Mallarini G (2009) Fissured fibrous cap of vulnerable carotid plaques and symptomaticity: are they correlated? Preliminary results by using multi-detector-row CT angiography. Cerebrovasc Dis 27(4):322–327
Homburg PJ, Rozie S, van Gils MJ, Jansen T, de Weert TT, Dippel DW, van der Lugt A (2010) Atherosclerotic plaque ulceration in the symptomatic internal carotid artery is associated with nonlacunar ischemic stroke. Stroke 41:1151–1156
Saba L, Anzidei M, Marincola BC, Piga M, Raz E, Bassareo PP, Napoli A, Mannelli L, Catalano C, Wintermark M (2013) Imaging of the Carotid Artery Vulnerable Plaque. Cardiovasc Intervent Radiol. 2013.
van Gils MJ, Bodde MC, Cremers LG, Dippel DW, van der Lugt A (2013) Determinants of calcification growth in atherosclerotic carotid arteries; a serial multi-detector CT angiography study. Atherosclerosis 227:95–99
Saba L, Montisci R, Sanfilippo R, Mallarini G (2009) Multidetector row CT of the brain and carotid artery: a correlative analysis. Clin Radiol 64:767–778
Fure B, Wyller TB, Thommessen B (2005) TOAST criteria applied in acute ischemic stroke. Acta Neurol Scand 112:254–258
Saba L, Raz E, Anzidei M, Francone M, Piga M (2013) Differences in plaque morphology and correlation of stenosis at the carotid artery bifurcation and the carotid siphon. AJR Am J Roentgenol 201:1108–1114
Saba L, Sanfilippo R, Sannia S, Anzidei M, Montisci R, Mallarini G, Suri JS (2012) Association between carotid artery plaque volume, composition, and ulceration: a retrospective assessment with MDCT. AJR Am J Roentgenol 199:151–156
de Weert TT, Ouhlous M, Zondervan PE, Hendriks JM, Dippel DW, van Sambeek MR, van der Lugt A (2005) In vitro characterization of atherosclerotic carotid plaque with multidetector computed tomography and histopathological correlation. Eur Radiol 15:1906–1914
de Weert TT, de Monyé C, Meijering E, Booij R, Niessen WJ, Dippel DW, van der Lugt A (2008) Assessment of atherosclerotic carotid plaque volume with multidetector computed tomography angiography. Int J Cardiovasc Imaging 24:751–759
Wethal T, Nedregaard B, Andersen R, Fosså A, Lund MB, Günther A, Kvaløy S, Fosså SD, Kjekshus J (2014) Atherosclerotic lesions in lymphoma survivors treated with radiotherapy. Radiother Oncol 110:448–454
Sattler MG, Vroomen PC, Sluiter WJ, Schers HJ, van den Berg G, Langendijk JA, Wolffenbuttel BH, van den Bergh AC, van Beek AP (2013) Incidence, causative mechanisms, and anatomic localization of stroke in pituitary adenoma patients treated with postoperative radiation therapy versus surgery alone. Int J Radiat Oncol Biol Phys 87:53–59
Fajardo LF (1999) Is the pathology of radiation injury different in small vs large blood vessels? Cardiovasc Radiat Med 1:108–110
Plummer C, Henderson RD, O'Sullivan JD, Read SJ (2011) Ischemic stroke and transient ischemic attack after head and neck radiotherapy: a review. Stroke 42:2410–2418
Rockman CB, Riles TS, Fisher FS, Adelman MA, Lamparello PJ (1996) The surgical management of carotid artery stenosis in patients with previous neck irradiation. Am J Surg 172:191–195
Steele SR, Martin MJ, Mullenix PS, Crawford JV, Cuadrado DS, Andersen CA (2004) Focused high-risk population screening for carotid arterial stenosis after radiation therapy for head and neck cancer. Am J Surg 187:594–598
Xu D, Hippe DS, Underhill HR, Oikawa-Wakayama M, Dong L, Yamada K, Yuan C, Hatsukami TS (2014) Prediction of high-risk plaque development and plaque progression with the carotid atherosclerosis score. JACC Cardiovasc Imaging 7:366–373
Hong JC, Kruser TJ, Gondi V, Mohindra P, Cannon DM, Harari PM, Bentzen SM (2013) Risk of cerebrovascular events in elderly patients after radiation therapy versus surgery for early-stage glottic cancer. Int J Radiat Oncol Biol Phys 87:290–296
Huang YS, Lee CC, Chang TS, Ho HC, Su YC, Hung SK, Lee MS, Chou P, Chang YH, Lee CC (2011) Increased risk of stroke in young head and neck cancer patients treated with radiotherapy or chemotherapy. Oral Oncol 7:1092–1097
Wintermark M, Jawadi SS, Rapp JH, Tihan T, Tong E, Glidden DV, Abedin S, Schaeffer S, Acevedo-Bolton G, Boudignon B, Orwoll B, Pan X, Saloner D (2008) High-resolution CT imaging of carotid artery atherosclerotic plaques. AJNR Am J Neuroradiol 29:875–882
van Gils MJ, Vukadinovic D, van Dijk AC, Dippel DW, Niessen WJ, van der Lugt A (2012) Carotid atherosclerotic plaque progression and change in plaque composition over time: a 5-year follow-up study using serial CT angiography. AJNR Am J Neuroradiol 33:1267–1273
Acknowledgments
The scientific guarantor of this publication is Luca Saba. The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article. The authors state that this work has not received any funding. No complex statistical methods were necessary for this paper. Institutional review board approval was obtained. Written informed consent was waived by the institutional review board. . No study subjects or cohorts have been previously reported. Methodology: retrospective, observational, performed at one institution.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Anzidei, M., Suri, J.S., Saba, L. et al. Longitudinal assessment of carotid atherosclerosis after Radiation Therapy using Computed Tomography: A case control Study. Eur Radiol 26, 72–78 (2016). https://doi.org/10.1007/s00330-015-3753-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-015-3753-9