Abstract
Non-alcoholic fatty liver disease (NAFLD) is the most common liver disease which may progress to non-alcoholic steatohepatitis. The prevalence of sarcopenia, which is the loss of muscle mass and strength, is increasing in the aging society. Recent studies reported the relationship between NAFLD and sarcopenia. The skeletal muscle is the primary organ for glucose disposal. Loss of muscle mass can cause insulin resistance, which is an important risk factor for NAFLD. Moreover, obesity, chronic low-grade inflammation, vitamin D deficiency, physical inactivity, hepatokines, and myokines might be involved in the pathophysiologic mechanism of sarcopenia and NAFLD. Although most of the previous studies have demonstrated the positive correlation between sarcopenia and NAFLD, the difference in diagnostic methods of sarcopenia and NAFLD leads to difficulties in interpretation and application. This review discusses the concept and diagnosis of sarcopenia and NAFLD, common pathophysiology, and clinical studies linking sarcopenia to NAFLD. The presentation of the association between sarcopenia and NAFLD may provide an opportunity to prevent the deterioration of fatty liver disease.
Graphic abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sarcopenia is an age-related decrease in muscle mass with progressive loss of muscle strength and physical performance. It is associated with metabolic impairment, falls, disability, hospitalization, and mortality in the elderly [1]. Besides aging, sarcopenia can occur earlier in life secondary to various causes, including unhealthy diet, physical inactivity, and chronic diseases [2]. The skeletal muscle is the primary organ of insulin-mediated glucose disposal, decreased muscle mass has a pivotal role in insulin resistance (IR) and metabolic syndrome [3].
Non-alcoholic fatty liver disease (NAFLD) is the most common liver disease worldwide, with a prevalence of 25.2% globally, 24% in the USA, and 27% in Asia [4]. The prevalence of NAFLD is gradually increasing, and the prevalence of NAFLD and non-alcoholic steatohepatitis (NASH) would increase by 21% and 63%, respectively, from 2015 to 2030. Moreover, NAFLD affecting 10–20% of the general pediatric population, the prevalence of NAFLD will rise more rapidly [5]. NAFLD can progress from simple steatosis to NASH and can be accompanied by liver cirrhosis, and liver failure [6]. NAFLD is associated with IR, type 2 diabetes mellitus (T2DM), cardiovascular disease, and significantly higher mortality than in the general population [7].
The main pathophysiology of sarcopenia is associated with insulin resistance, which plays a major role in the development of NAFLD. The prevalence of sarcopenia is higher in patients affected by NAFLD and correlates with the severity of fatty liver disease. In a recent meta-analysis, the risk of NAFLD and NAFLD-related fibrosis was higher in subjects with sarcopenia than in subjects without sarcopenia (29% and 57%, respectively) [8]. Loss of muscle mass is associated with decreased survival, increase in the length of hospitalization, and mortality in patients with cirrhosis [9]. Moreover, muscle function is related to NAFLD and vice versa. To clearly elucidate the interaction between sarcopenia and NAFLD, it is important to clarify definition and diagnosis. In this review, we described the definition and diagnostic methods of NAFLD and sarcopenia, then summarize the results of recent clinical studies and suggest possible pathological mechanisms. Furthermore, the role of hepatokines and myokines in the crosstalk between skeletal muscle and liver is introduced.
NAFLD
NAFLD is a spectrum of liver diseases encompassing non-alcoholic fatty liver (NAFL), NASH, fibrosis, and cirrhosis in the absence of excessive alcohol consumption (> 20 g/day for Female and > 30 g/day for male). NAFL is defined as ≥ 5% of steatosis without hepatocellular injury. NASH is defined as steatosis with hepatocellular damage with or without hepatic fibrosis. NAFLD is closely related to visceral obesity, IR, T2DM, hypertension, and dyslipidemia; and has been regarded as a hepatic manifestation of metabolic syndrome [10]. Hepatic steatosis development is regulated by increased free fatty acids (FFA) from the adipose tissue or dietary intake, hepatic de novo lipogenesis, impaired fatty acid oxidation, and decreased liver secretion [11]. The mechanism of liver injury in NAFLD is currently thought to be a “multiple hit process” involving IR, oxidative stress, apoptosis, and adipokines [12]. A sedentary lifestyle with a high-caloric diet, excess saturated fat, refined carbohydrate, and high fructose intake have been associated with obesity and NAFLD [13].
Liver biopsy is regarded as the gold standard for diagnosing NAFLD. However, ultrasonography is recommended as the first-line imaging modality in a clinical setting as it is easily accessible and relatively accurate in diagnosing hepatic steatosis compared to histology (sensitivity of 85% and specificity of 94%) [14]. A controlled attenuation parameter is a promising tool for non-invasive detection of hepatic steatosis along with liver stiffness [15]. It is measured by vibration-controlled transient elastography with FibroScan® and is comparable with biopsy-diagnosed steatosis (sensitivity of 69% and specificity of 82%). 1H-magnetic resonance spectroscopy is a safe and non-invasive alternative for quantification of hepatic fat content that offers good reproducibility [16]. Besides imaging modalities, risk factor models, such as SteatoTest, fatty liver index, NAFLD liver fat score, hepatic steatosis index, and Framingham steatosis index, can also be used for estimation of hepatic steatosis. In case of NASH, liver biopsy remained the most specific test to define the characteristics and severity of the liver disease. The NAFLD fibrosis score, fibrosis-4 index, enhanced liver fibrosis test, and Fibrotest can be used to define fibrosis using a non-invasive method [17].
Sarcopenia
Definition and diagnosis of sarcopenia
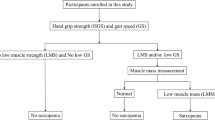
Sarcopenia was first described in 1989, and is derived from the Greek words “sarx” meaning flesh and “penia” meaning loss [18]. Sarcopenia is defined as appendicular skeletal muscle mass (ASM) divided by height in square meters (ASM/height2) less than two standard deviations (SD) below the mean for young reference group [19]. ASM/height2 is the most commonly used method adopted by the European Working Group on Sarcopenia in Older People (EWGSOP), International Working Group on Sarcopenia, and Asian Working Group for Sarcopenia (AWGS) guidelines [1, 20, 21]. This operational method has a significant correlation with physical disability [19]. However, this is highly correlated with body mass index (BMI), the current index for obesity, which considers thin people as sarcopenic and underestimates sarcopenia in overweight or obese people. In 2002, the weight-adjusted muscle mass index was developed [22]. This index was modified as ASM/weight and is wildly used in investigating the relationship between sarcopenia and metabolic diseases, such as metabolic syndrome, NAFLD, and diabetes [23]. In 2010, EWGSOP proposed an operational clinical definition and consensus on the diagnostic criteria [20]. The working definition of sarcopenia was required to consider muscle mass, strength, and physical performance for the first time. Based on the EWGSOP guidelines, AWGS published a sarcopenia consensus report for Asians containing an algorithm for the diagnosis and unique cutoff points of each parameter [21]. Recently, the Foundation for the National Institutes of Health (FNIH) Sarcopenia Project published a consensus definition of sarcopenia using a database from nine large observational studies with more than 25,000 participants. Since obesity influences the relationship between lean mass and muscle strength, FNIH created an alternative, the skeletal muscle index (SMI), which is defined as ASM/BMI [24]. We found that ASM/BMI-defined sarcopenia is more closely related to IR index, visceral obesity, and metabolic syndrome than other muscle mass indices in the Korean population [25]. There is no current unified definition for sarcopenia because of different clinical implications according to the consensus on sarcopenia.
In 2018, EWGSOP2 updated the sarcopenia definition and care strategy [2]. In these guidelines, muscle strength is the principal parameter of sarcopenia. After low muscle strength is detected, low muscle quantity or quality confirms sarcopenia. Additionally, FNIH and AWGS considered muscle strength in the first place for diagnosing sarcopenia. Based on the new consensus and research data, incorporating muscle strength/physical performance along with low muscle mass in defining sarcopenia is crucial in elucidating the association between sarcopenia and NAFLD.
Sarcopenia is primarily associated with aging in elderly people, but it can be due to secondary causes. EWGSOP2 suggests the concept of secondary sarcopenia, which is caused by loss of muscle mass and function secondary to malignancy, organ failure, physical inactivity, and inadequate energy intake [2]. In addition, the AWGS consensus suggests screening of sarcopenia not only in the elderly, but also in people with specific clinical conditions, such as the presence of recent functional decline or impairment, unintentional weight loss, depression or cognitive disorder, repeated falls, malnutrition, and chronic conditions (chronic heart failure, diabetes mellitus, chronic kidney disease, and other chronic wasting conditions) [21].
Assessment of sarcopenia
Muscle mass can be measured as total body skeletal muscle mass, ASM, and cross-sectional area of a specific body site or muscle group. Dual-energy X-ray absorptiometry is the most commonly used method for muscle measurement in sarcopenia. Body impedance analysis (BIA) has been widely used as an alternative method, because it is non-invasive and easily accessible, cost-effective, and has radiation-free characteristics. However, BIA is less validated and easily altered based on temperature, humidity, and water contents. Hence, diagnostic accuracy has not been fully established. Computed tomography and magnetic resonance imaging have been considered as the gold standards for evaluation of body composition [26]. The psoas, paraspinal, and abdominal muscles in the third lumbar vertebra region are the most common muscles used for estimating muscle mass indices [27]. In addition, ultrasonography may measure muscle mass and quality. The handgrip strength is considered as a reliable and convenient method to measure muscle strength [28]. Grip strength is a predictor of strength in other body compartments, the length of hospital stay, functional limitations, quality of life, and death [29]. Likewise, the chair rise test can be used to measure the strength and endurance of leg muscles. Physical performance can be assessed using gait speed, short physical performance battery (SPPB), and Timed Up and Go test [20]. Gait speed is commonly adopted in the EWGSOP, AWGS, and FNIH guidelines.
Prevention and treatment approaches to sarcopenia
There are no approved pharmacological interventions for sarcopenia. The main strategy for prevention and treatment of sarcopenia is lifestyle intervention, such as exercise and nutrition. Resistance training improves physical strength and muscle mass by increasing type II muscle fiber size and satellite muscle recruitment. Aerobic exercise remodels myofibers and improves cardiorespiratory fitness. Besides lifestyle intervention, proper nutritional support (protein, essential amino acid, β-hydroxy-β-methylbutyrate, Vit. D, creatinine, etc.) is crucial in sarcopenia; and the benefit of exercise is potentiated with nutritional support. In Japanese sarcopenic female, exercise with amino acid supplementation enhanced muscle strength, muscle mass, and walking speed [30]. In addition, a calorie restriction regimen with exercise may be a good option for the treatment of obese sarcopenic subjects [31]. In light of the close relationship between obesity and NAFLD, calorie restriction with exercise might be the efficient strategy to interrupt for the vicious cycle of sarcopenia and NAFLD.
Clinical studies
Clinical studies on the association between sarcopenia and NAFLD/NASH are summarized in Table 1. Most studies were conducted in Asia [32,33,34,35,36,37,38,39,40,41,42] and only four studies [43,44,45,46] were analyzed from other continents. Currently, most studies show a positive relationship between sarcopenia and NAFLD.
In 2014, we investigated the relationship between sarcopenia and NAFLD from the Korean Sarcopenic Obesity Study [32]. Subjects with low muscle mass had an increased risk of NAFLD after adjusting for IR and inflammation. SMI had reverse association with HOMA-IR, hs-CRP, triglycerides, and total body fat. Moreover, subjects with the lowest quartile of SMI value had a higher risk of NAFLD even after adjusting for potential confounding factors. Another subsequent study showed a positive relationship between sarcopenia and NAFLD regardless of obesity or IR [33]. Furthermore, they presented that sarcopenic subjects with NAFLD had a higher risk of advanced fibrosis than normal subjects, independent of obesity, IR, or liver enzyme levels [34]. A 1% increment in SMI could decrease the risk of NAFLD by 20% in men with T2DM [36], and the grip strength was inversely related to NAFLD [40].
The association of sarcopenia and NAFLD is closely related to the severity of the advanced fatty liver disease. One study from Korea showed that the prevalence of sarcopenia gradually increased from control to NAFLD and NASH groups [8.7%, 17.9%, and 35.0%, respectively (p < 0.001)] [37]. Furthermore, sarcopenic subjects with NAFLD had increased risk of NASH (OR 2.30; 95% CI 1.08–4.93) and significant fibrosis (OR 2.05; 95% CI 1.01–4.16) independent of obesity and IR. Another two studies support the relationship between sarcopenia and severity of NASH and liver fibrosis in Caucasians [44, 45]. Although most previous studies have demonstrated a consistently positive association between sarcopenia and NAFLD, two studies revealed a heterogeneous association. One study showed different associations between sarcopenia and NAFLD based on the criteria used for diagnosing sarcopenia [46], whereas another study reported no relationship between NAFLD and sarcopenia when sarcopenia was defined by muscle mass, muscle strength, and gait speed [41].
Since most studies were conducted using a cross-sectional design, the causal relationship between sarcopenia and NAFLD cannot be determined. Recently, in a 7-year follow-up, longitudinal cohort study including 15,567 subjects, which consisted of 12,624 subjects without NAFLD and 2943 subjects with NAFLD, showed that 14.8% of baseline non-NAFLD subjects developed NAFLD, and subjects with the highest tertile of SMI at baseline had decreased risk of NAFLD (adjusted hazard ratio [AHR], 0.44; 95% CI, 0.38–0.51) [38]. Furthermore, a positive association in baseline SMI and the resolution of existing baseline NAFLD was noted. Interestingly, the study evaluated the association between the change in SMI in a year and NAFLD. The highest tertile of change in SMI showed a significantly decreased incidence of NAFLD (AHR 0.69; 95% CI 0.59–0.82) and resolution of baseline NAFLD (AHR 4.17; 95% CI 1.90–6.17) even after adjusting the baseline SMI. It was suggested that maintaining or increasing skeletal muscle mass could be a therapeutic option for NAFLD.
Pathophysiology
The possible mechanisms of interaction between NAFLD and sarcopenia are IR, obesity, chronic low-grade inflammation, physical inactivity, hepatokines, and myokines (Fig. 1, Table 2). The potential pathophysiological mechanisms are listed below.
Insulin resistance
IR is the main pathologic mechanism of sarcopenia and NAFLD. It is caused by fat tissue infiltration in the skeletal muscle and increased circulating FFA from excessive body fat [3, 47]. Insulin activates the mammalian target of rapamycin and enhances signaling to its downstream effectors 4E-binding protein 1 and ribosomal S6 kinase 1, which results in maintenance of muscle mass and plays a role in skeletal muscle anabolism [48]. Skeletal muscle IR leads to increased muscle degradation with decreased mitochondrial content, function and oxidative capacity [49]. Therefore, IR can be one of the pivotal mechanisms causing sarcopenia. We found that T2DM was independently associated with sarcopenia, leading to metabolic disorders and physical disability in older adults with T2DM [50]. Furthermore, reduced muscle mass may aggravate IR.
Skeletal muscle acts as the primary organ for whole-body glucose homeostasis by expression of insulin-dependent transporter GLUT-4 [51]. Decreased insulin sensitivity impairs glucose uptake and insulin stimulated glycogen synthesis [3]. Excess glucose is converted to triacylglycerol in the liver, causing NAFLD, which can be attributed to hepatic IR [52]. Moreover, obesity induces an increased flux of FFA, increased hepatic diacylglycerol concentration, and translocation of protein kinase-Cε (PKCε) to the plasma membrane, which inhibits tyrosine phosphorylation of receptor substrate (IRS)-1 and IRS-2, phosphoinositide 3-kinases activation, and hepatic insulin signaling [53]. Hence, both hepatic IR and peripheral IR can be pathologic mechanism for NAFLD. Hepatic steatosis is related more to skeletal IR than hepatic IR in patients with NAFLD, supporting the pivotal role of skeletal muscle IR in the development of NAFLD [54].
Obesity
Obesity is an important cause of the increasing global burden of metabolic and cardiovascular morbidity and mortality. The coexistence of sarcopenia and obesity is defined as sarcopenic obesity (SO). A reciprocal interaction between excess visceral fat and sarcopenia aggravates loss of muscle mass. In a longitudinal study, we revealed that visceral obesity was independently associated with future loss of skeletal muscle [55]. Adipose tissue–muscle–liver interplay causes NAFLD and accelerates liver fibrosis (Fig. 2). Especially, obesity-induced excess of FFA which results in liver damage and injury. Injured liver stimulates Kupffer cells and recruits monocyte-derived macrophages to accelerate the progression from NAFLD to NASH [56]. In addition, increased visceral adipose tissue promotes chronic inflammation by secreting inflammatory cytokines such as interleukin-6 (IL-6), tumor necrosis factor-α (TNF-α), plasminogen activator inhibitor-1, leptin, and other adipokines [57]. Leptin, the first adipocyte-secreted hormone, regulates appetite, energy metabolism, and body weight. However, hyperleptinemia can promote IR, hepatic inflammation, and fibrosis [58]. In the meta-analysis including 33 studies, circulating leptin levels were higher in NAFLD subjects than those in normal subjects, and leptin levels were positively correlated with NAFLD severity [59]. Another study demonstrated that ASM was independently and negatively correlated with the leptin level regardless of body fat mass [60]. Additionally, leptin upregulates proinflammatory cytokines and reduces the anabolic effect of insulin-like growth factor-1 (IGF-1) [61]. Moreover, visceral obesity itself strongly suppresses secretion of growth hormone (GH) by hyperinsulinemia, increases FFA and somatostatin tone, and reduces ghrelin. Impaired GH/IGF-1 axis could be associated with SO and ectopic fat deposition in the liver [62]. Adipocyte fatty acid-binding protein (A-FABP) can play a role in obesity-induced IR and inflammation. Serum A-FABP levels are negatively correlated with SMI (ASM/weight) independent of confounding factors [63]. In a cross-sectional study, A-FABP independently predicted the incidence of inflammation and fibrosis in NAFLD, even after adjusting the homeostasis model assessment-estimated insulin resistance (HOMA-IR) and visceral fat [64].
Vitamin D
Vit. D is the hormone involved in calcium homeostasis, bone metabolism, and muscle growth. It is known as a potent mediator of IR, metabolic syndrome, NAFLD, and sarcopenia. This vitamin exerts its effect via the vitamin D receptor (VDR) expressed in various human cells including the skeletal muscle [65]. Vit. D deficiency reduces VDR expression, increases reactive oxygen species generation, and causes mitochondrial function disruption, leading to skeletal muscle atrophy [66]. Whole-body VDR knockout mice showed skeletal muscle dysfunction and abnormal development. In a 3-year longitudinal aging study, lower 25-OH Vit. D and higher parathyroid hormone levels increased the risk of sarcopenia in elderly people [67]. Subjects with 25-OH Vit. D < 25 nmol/L were 2.57 (95% confidence interval [CI], 1.40–4.70, based on grip strength) times and 2.14 (95% CI 0.73–6.33, based on muscle mass) times more likely to experience sarcopenia. Furthermore, Vit. D regulates oxidative stress, inflammation, hepatocyte apoptosis, and fibrosis in the liver [68]. In a cross-sectional study in East China, 84.6% of male with NAFLD were diagnosed with Vit. D deficiency and subjects with decreased Vit. D levels had a 54% increased risk of NAFLD after adjusting confounding factors [69]. In a meta-analysis including 17 cross-sectional and case–control studies, NAFLD patients had decreased serum Vit. D levels and had a 26% increased risk of Vit. D deficiency (odds ratio [OR], 1.26; 95% CI 1.17–1.35) [70]. However, it is controversial whether or not Vit. D deficiency is related to the histologic feature of NAFLD [71, 72].
Chronic low-grade inflammation
Obesity induces increased levels of circulating inflammatory cytokines, including TNF-α, IL-6, and C-reactive protein (CRP), which cause chronic low-grade inflammation. TNF-α stimulates reactive oxygen species production and causes oxidative stress and mitochondrial dysfunction [73]. It inactivates the AMP-activated protein kinase (AMPK) pathway, which leads to the development of NAFLD. The serum TNF-α level was higher in patients with simple steatosis and steatohepatitis than in healthy subjects [74]. IL-6 has an important role in the development of NASH and systemic inflammation; IL-6 levels were correlated with the degree of inflammation and fibrosis in the liver [75]. The above-mentioned inflammatory cytokines have a negative association with the skeletal muscle. In the Health ABC study, elevated TNF-α and IL-6 levels were correlated with low muscle mass and reduced muscle strength in aged male and Female [76]. In a 10-year longitudinal study, plasma TNF-α and IL-6 concentrations could predict the frailty and mortality in older subjects [77]. We demonstrated that subjects with sarcopenia had increased high-sensitivity C-reactive protein (hs-CRP) levels than subjects without sarcopenia. Moreover, hs-CRP levels had a negative correlation with SMI and liver attenuation index (p < 0.001) suggesting that inflammation may be an important causative factor of sarcopenia and NAFLD [32].
Hepatokines
Hepatokines are autocrine, paracrine, and endocrine proteins secreted by hepatocytes that can mediate metabolic disorders. These include adropin, angiopoietin-like protein 4, sex hormone-binding globulin, fetuin-A and -B, retinol-binding protein 4, selenoprotein P, fibroblast growth factor (FGF)-21, leukocyte cell-derived chemotaxin 2 (LECT2), and hepassocin (HPS) [11]. In 2005, FGF-21 was first identified as a novel metabolic regulator. FGF-21 potentiates clearance of systemic glucose and lipids and improves insulin sensitivity, adiponectin action, mitochondrial function, thermogenesis, and energy expenditure. The improvement is correlated with a reduction in triglyceride and diacylglycerol levels and PKC translocation in the liver and skeletal muscle [78]. Infusion of FGF-21 in mouse model caused improvements in both hepatic and peripheral insulin sensitivity and had a beneficial effect on obesity, diabetes, and fatty liver disease [78, 79]. LECT2 is a novel hepatokine that mediates obesity and skeletal muscle IR [80]. Deletion of LECT2 in mice improved IR by phosphorylation of c-Jun N-terminal kinase (JNK) pathway in the skeletal muscle. The results of our study showed that the circulating LECT2 levels were higher in patients with NAFLD than in those without NAFLD [81]. Furthermore, LECT2 was positively associated with obesity, lipid profiles, hs-CRP, and liver aminotransferase levels. Hepatocyte-derived fibrinogen-related protein (HPS) is a protein involved in hepatic regeneration [82]. HPS can mediate IR and T2DM. Plasma HPS concentrations were upregulated in NAFLD by inducing hepatic steatosis through the extracellular signal-regulated kinase 1/2-dependent pathway [83]. Furthermore, HPS was independently correlated with fasting plasma glucose level, IR, impaired fasting glucose, impaired glucose tolerance, and newly detected diabetes in human [84]. In a recent study, increased HPS levels in hepatocytes caused IR in the skeletal muscle through epidermal growth factor receptor/JNK pathway [85].
Myokines
The skeletal muscle is an endocrine organ secreting myokines that regulate systemic metabolism. Irisin is a myokine which stimulates uncoupling protein-1, browning of adipose tissue and improves glucose intolerance and energy expenditure [86]. In the experimental models, irisin, in an AMPK-dependent manner, improves hepatic steatosis and glucose metabolism. In biopsy-proven NAFLD subjects, irisin levels were similar in NAFL and NASH; however, they were positively associated with the presence of portal inflammation [87]. Irisin levels were inversely related to hepatic triglyceride levels in 296 obese Chinese subjects [88]. These metabolic effects may be related to sarcopenia, but previous studies have shown contradicting results. We observed that circulating irisin levels were not different in subjects with sarcopenia compared with the controls using two different irisin enzyme-linked immunosorbent assay kits [89]. However, another study showed that irisin levels were positively correlated with ASM/height2 and hand grip strength [90]. Myostatin, a member of the transforming growth factor superfamily, is predominantly released by the skeletal muscle and has a negative effect on the skeletal muscle [91]. Blocking myostatin increases muscle mass, improves insulin sensitivity and protects hepatic steatosis in mice [92].
Physical inactivity
Physical inactivity causes loss of muscle mass and excess positive energy balance aggravates obesity. Consequently, sarcopenia and NAFLD can be provoked and aggravated by chronic inflammation, IR, and oxidative stress. Exercise can increase muscle insulin sensitization, promote muscle protein synthesis, and myokine secretion. Physical activity reduces the risk of developing sarcopenia (OR 0.45; 95% CI 0.37–0.55) as revealed in a meta-analysis [93]. Exercise can improve metabolic health independent of weight loss [94]. After a 4-week aerobic cycling exercise, the hepatic triglyceride concentration was observed to be decreased by 21%.
Areas for future study
Several studies have investigated the role of genetics in the field of sarcopenia and NAFLD. The most extensively studied polymorphisms in sarcopenia are those of angiotensin converting enzyme (ACE) gene I/D, α-actinin-3 (ACTN3), and myostatin (MSTN) [95]. In a recent study in UK, variation in the human leukocyte antigen complex and non-coding single nucleotide polymorphisms was associated with sarcopenia [96]. However, whether the influence of genetic variations is direct or specific to muscle phenotypes or strength is controversial. In NAFLD, genetic variability in patatin-like phospholipase domain-containing protein 3 (PNPLA3), transmembrane 6 superfamily 2 human gene (TM6SF2), membrane-bound O-acyltransferase domain-containing protein 7 (MBOAT7), and glucokinase regulatory protein (GCKR) genes was validated as a modifier [97]. Interestingly, there have been several studies that NAFLD/NASH and insulin resistance has been associated with genetic variation, such as PNPLA3. PNPLA3 I148 M variant is associated with high liver fat, but not with insulin sensitivity [98]. However, PNPLA3 I148 M allele was associated with insulin resistance in severely obese individuals [99]. Sarcopenia and NAFLD share common pathophysiology. Further studies on the elucidation of genetic aspects that mediates sarcopenia and NAFLD are needed.
Summary and conclusion
An increasing body of evidence indicates that sarcopenia may play a role in NAFLD, not only in the pathogenesis but also severity and prognosis. The underlying mechanisms for the pathophysiology of NAFLD are IR, obesity, low-grade inflammation, Vit. D deficiency, physical inactivity, hepatokines, and myokines. Interventions such as weight reduction, exercise, Vit. D supplementation, myostatin inhibitor administration, and insulin sensitizer therapy can be utilized to ameliorate the loss of muscle mass and improve hepatic steatosis (Fig. 3). High fructose diet is a well-known risk factor for NAFLD. The high fructose intake increases uric acid level thereby inducing insulin resistance and oxidative stress [100]. Thus, changing diet habit may be helpful in the management of sarcopenia as well as NAFLD. Aging and underlying diseases can contribute to the incidence of sarcopenia; NAFLD may be a risk factor for sarcopenia. Therefore, it is currently unclear if sarcopenia contributes to NAFLD or vice versa. Sarcopenia is a progressive loss of skeletal muscle mass, strength, and physical performance. Recent consensus suggests muscle function as a primary determinant in addressing sarcopenia. Considering the clinical studies demonstrating the association of low muscle mass and NAFLD, further mechanistic studies on the effect of low muscle function/performance on NAFLD are necessary.
References
Fielding RA, Vellas B, Evans WJ, Bhasin S, Morley JE, Newman AB, et al. Sarcopenia: an undiagnosed condition in older adults. Current consensus definition: prevalence, etiology, and consequences. International working group on sarcopenia. J Am Med Dir Assoc. 2011;12:249–56.
Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyère O, Cederholm T, et al. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing. 2019;48:16–31.
DeFronzo RA, Tripathy D. Skeletal muscle insulin resistance is the primary defect in type 2 diabetes. Diabetes Care. 2009;32(Suppl 2):S157–63.
Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M. Global epidemiology of nonalcoholic fatty liver disease-Meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016;64:73–84.
Temple JL, Cordero P, Li J, Nguyen V, Oben JA. A guide to non-alcoholic fatty liver disease in childhood and adolescence. Int J Mol Sci. 2016;17:947.
Estes C, Razavi H, Loomba R, Younossi Z, Sanyal AJ. Modeling the epidemic of nonalcoholic fatty liver disease demonstrates an exponential increase in burden of disease. Hepatology. 2018;67:123–33.
Calzadilla Bertot L, Adams LA. The natural course of non-alcoholic fatty liver disease. Int J Mol Sci. 2016;17:774.
Pan X, Han Y, Zou T, Zhu G, Xu K, Zheng J, et al. Sarcopenia contributes to the progression of nonalcoholic fatty liver disease- related fibrosis: a meta-analysis. Dig Dis. 2018;36:427–36.
Kim G, Kang SH, Kim MY, Baik SK. Prognostic value of sarcopenia in patients with liver cirrhosis: a systematic review and meta-analysis. PLoS One. 2017;12:e0186990.
Marchesini G, Marzocchi R. Metabolic syndrome and NASH. Clin Liver Dis. 2007;11(105–117):ix.
Meex RCR, Watt MJ. Hepatokines: linking nonalcoholic fatty liver disease and insulin resistance. Nat Rev Endocrinol. 2017;13:509–20.
Kim CH, Younossi ZM. Nonalcoholic fatty liver disease: a manifestation of the metabolic syndrome. Cleve Clin J Med. 2008;75:721–8.
European Association for the Study of the Liver (EASL) European Association for the Study of Diabetes (EASD), European Association for the Study of Obesity (EASO). EASL-EASD-EASO clinical practice guidelines for the management of non-alcoholic fatty liver disease. J Hepatol. 2016;64:1388–402.
Hernaez R, Lazo M, Bonekamp S, Kamel I, Brancati FL, Guallar E, et al. Diagnostic accuracy and reliability of ultrasonography for the detection of fatty liver: a meta-analysis. Hepatology. 2011;54:1082–90.
Karlas T, Petroff D, Sasso M, Fan JG, Mi YQ, de Ledinghen V, et al. Individual patient data meta-analysis of controlled attenuation parameter (CAP) technology for assessing steatosis. J Hepatol. 2017;66:1022–30.
Szczepaniak LS, Nurenberg P, Leonard D, Browning JD, Reingold JS, Grundy S, et al. Magnetic resonance spectroscopy to measure hepatic triglyceride content: prevalence of hepatic steatosis in the general population. Am J Physiol Endocrinol Metab. 2005;288:E462–8.
Stefan N, Häring HU, Cusi K. Non-alcoholic fatty liver disease: causes, diagnosis, cardiometabolic consequences, and treatment strategies. Lancet Diabetes Endocrinol. 2019;7:313–24.
Rosenberg IH. Summary comments. Am J Clin Nutr. 1989;50:1231–3.
Baumgartner RN, Koehler KM, Gallagher D, Romero L, Heymsfield SB, Ross RR, et al. Epidemiology of sarcopenia among the elderly in New Mexico. Am J Epidemiol. 1998;147:755–63.
Cruz-Jentoft AJ, Baeyens JP, Bauer JM, Boirie Y, Cederholm T, Landi F, et al. Sarcopenia: European consensus on definition and diagnosis: report of the European working group on sarcopenia in older people. Age Ageing. 2010;39:412–23.
Chen LK, Liu LK, Woo J, Assantachai P, Auyeung TW, Bahyah KS, et al. Sarcopenia in Asia: consensus report of the Asian Working Group for Sarcopenia. J Am Med Dir Assoc. 2014;15:95–101.
Janssen I, Heymsfield SB, Ross R. Low relative skeletal muscle mass (sarcopenia) in older persons is associated with functional impairment and physical disability. J Am Geriatr Soc. 2002;50:889–96.
Lim S, Kim JH, Yoon JW, Kang SM, Choi SH, Park YJ, et al. Sarcopenic obesity: prevalence and association with metabolic syndrome in the Korean longitudinal study on health and aging (KLoSHA). Diabetes Care. 2010;33:1652–4.
Studenski SA, Peters KW, Alley DE, Cawthon PM, McLean RR, Harris TB, et al. The FNIH sarcopenia project: rationale, study description, conference recommendations, and final estimates. J Gerontol A Biol Sci Med Sci. 2014;69:547–58.
Kim TN, Park MS, Lee EJ, Chung HS, Yoo HJ, Kang HJ, et al. Comparisons of three different methods for defining sarcopenia: an aspect of cardiometabolic risk. Sci Rep. 2017;7:6491.
Heymsfield SB. Development of imaging methods to assess adiposity and metabolism. Int J Obes (Lond). 2008;32(Suppl 7):S76–82.
Prado CM, Lieffers JR, McCargar LJ, Reiman T, Sawyer MB, Martin L, et al. Prevalence and clinical implications of sarcopenic obesity in patients with solid tumours of the respiratory and gastrointestinal tracts: a population-based study. Lancet Oncol. 2008;9:629–35.
Roberts HC, Denison HJ, Martin HJ, Patel HP, Syddall H, Cooper C, et al. A review of the measurement of grip strength in clinical and epidemiological studies: towards a standardised approach. Age Ageing. 2011;40:423–9.
Leong DP, Teo KK, Rangarajan S, Lopez-Jaramillo P, Avezum A Jr, Orlandini A, et al. Prognostic value of grip strength: findings from the prospective urban rural epidemiology (PURE) study. Lancet. 2015;386:266–73.
Kim HK, Suzuki T, Saito K, Yoshida H, Kobayashi H, Kato H, et al. Effects of Exercise and amino acid supplementation on body composition and physical function in community-dwelling elderly japanese sarcopenic women: a randomized controlled trial. J Am Geriatr Soc. 2012;60:16–23.
Villareal DT, Aguirre L, Gurney AB, Waters DL, Sinacore DR, Colombo E, et al. Aerobic or Resistance exercise, or both, in dieting obese older adults. N Engl J Med. 2017;376:1943–55.
Hong HC, Hwang SY, Choi HY, Yoo HJ, Seo JA, Kim SG, et al. Relationship between sarcopenia and nonalcoholic fatty liver disease: the Korean Sarcopenic Obesity Study. Hepatology. 2014;59:1772–8.
Lee YH, Jung KS, Kim SU, Yoon HJ, Yun YJ, Lee BW, et al. Sarcopaenia is associated with NAFLD independently of obesity and insulin resistance: Nationwide surveys (KNHANES 2008–2011). J Hepatol. 2015;63:486–93.
Lee YH, Kim SU, Song K, Park JY, Kim DY, Ahn SH, et al. Sarcopenia is associated with significant liver fibrosis independently of obesity and insulin resistance in nonalcoholic fatty liver disease: Nationwide surveys (KNHANES 2008–2011). Hepatology. 2016;63:776–86.
Kim HY, Kim CW, Park CH, Choi JY, Han K, Merchant AT, et al. Low skeletal muscle mass is associated with non-alcoholic fatty liver disease in Korean adults: the Fifth Korea national health and nutrition examination survey. Hepatobiliary Pancreat Dis Int. 2016;15:39–47.
Hashimoto Y, Osaka T, Fukuda T, Tanaka M, Yamazaki M, Fukui M. The relationship between hepatic steatosis and skeletal muscle mass index in men with type 2 diabetes. Endocr J. 2016;63:877–84.
Koo BK, Kim D, Joo SK, Kim JH, Chang MS, Kim BG, et al. Sarcopenia is an independent risk factor for non-alcoholic steatohepatitis and significant fibrosis. J Hepatol. 2017;66:123–31.
Kim G, Lee SE, Lee YB, Jun JE, Ahn J, Bae JC, et al. Relationship between relative skeletal muscle mass and nonalcoholic fatty liver disease: a 7-year longitudinal study. Hepatology. 2018;68:1755–68.
Lee MJ, Kim EH, Bae SJ, Kim GA, Park SW, Choe J, et al. Age-related decrease in skeletal muscle mass is an independent risk factor for incident nonalcoholic fatty liver disease: a 10-year retrospective cohort study. Gut Liver. 2019;13:67–76.
Meng G, Wu H, Fang L, Li C, Yu F, Zhang Q, et al. Relationship between grip strength and newly diagnosed nonalcoholic fatty liver disease in a large-scale adult population. Sci Rep. 2016;6:33255.
Zhai Y, Xiao Q, Miao J. The relationship between NAFLD and sarcopenia in elderly patients. Can J Gastroenterol Hepatol. 2018;2018:5016091.
Kang MK, Park JG, Lee HJ, Kim MC. Association of low skeletal muscle mass with advanced liver fibrosis in patients with non-alcoholic fatty liver disease. J Gastroenterol Hepatol. 2019;34:1633–40.
Issa D, Alkhouri N, Tsien C, Shah S, Lopez R, McCullough A, et al. Presence of sarcopenia (muscle wasting) in patients with nonalcoholic steatohepatitis. Hepatology. 2014;60:428–9.
Petta S, Ciminnisi S, Di Marco V, Cabibi D, Camma C, Licata A, et al. Sarcopenia is associated with severe liver fibrosis in patients with non-alcoholic fatty liver disease. Aliment Pharmacol Ther. 2017;45:510–8.
Wijarnpreecha K, Kim D, Raymond P, Scribani M, Ahmed A. Associations between sarcopenia and nonalcoholic fatty liver disease and advanced fibrosis in the USA. Eur J Gastroenterol Hepatol. 2019;31:1121–8.
Peng TC, Wu LW, Chen WL, Liaw FY, Chang YW, Kao TW. Nonalcoholic fatty liver disease and sarcopenia in a Western population (NHANES III): the importance of sarcopenia definition. Clin Nutr. 2019;38:422–8.
Reaven GM. Banting lecture 1988. Role of insulin resistance in human disease. Diabetes. 1988;37:1595–607.
Fujita S, Rasmussen BB, Cadenas JG, Drummond MJ, Glynn EL, Sattler FR, et al. Aerobic exercise overcomes the age-related insulin resistance of muscle protein metabolism by improving endothelial function and Akt/mammalian target of rapamycin signaling. Diabetes. 2007;56:1615–22.
Turcotte LP, Fisher JS. Skeletal muscle insulin resistance: roles of fatty acid metabolism and exercise. Phys Ther. 2008;88:1279–96.
Kim TN, Park MS, Yang SJ, Yoo HJ, Kang HJ, Song W, et al. Prevalence and determinant factors of sarcopenia in patients with type 2 diabetes: the Korean Sarcopenic Obesity Study (KSOS). Diabetes Care. 2010;33:1497–9.
Huang S, Czech MP. The GLUT4 glucose transporter. Cell Metab. 2007;5:237–52.
Petersen KF, Dufour S, Savage DB, Bilz S, Solomon G, Yonemitsu S, et al. The role of skeletal muscle insulin resistance in the pathogenesis of the metabolic syndrome. Proc Natl Acad Sci USA. 2007;104:12587–94.
Perry RJ, Samuel VT, Petersen KF, Shulman GI. The role of hepatic lipids in hepatic insulin resistance and type 2 diabetes. Nature. 2014;510:84–91.
Kato K-I, Takeshita Y, Misu H, Zen Y, Kaneko S, Takamura T. Liver steatosis is associated with insulin resistance in skeletal muscle rather than in the liver in Japanese patients with non-alcoholic fatty liver disease. J Diabetes Investig. 2015;6:158–63.
Kim TN, Park MS, Ryu JY, Choi HY, Hong HC, Yoo HJ, et al. Impact of visceral fat on skeletal muscle mass and vice versa in a prospective cohort study: the Korean Sarcopenic Obesity Study (KSOS). PLoS One. 2014;9:e115407.
Cha JY, Kim DH, Chun KH. The role of hepatic macrophages in nonalcoholic fatty liver disease and nonalcoholic steatohepatitis. Lab Anim Res. 2018;34:133–9.
Ahima RS, Flier JS. Adipose tissue as an endocrine organ. Trends Endocrinol Metab. 2000;11:327–32.
Polyzos SA, Kountouras J, Zavos C, Deretzi G. The potential adverse role of leptin resistance in nonalcoholic fatty liver disease: a hypothesis based on critical review of the literature. J Clin Gastroenterol. 2011;45:50–4.
Polyzos SA, Aronis KN, Kountouras J, Raptis DD, Vasiloglou MF, Mantzoros CS. Circulating leptin in non-alcoholic fatty liver disease: a systematic review and meta-analysis. Diabetologia. 2016;59:30–43.
Waters DL, Qualls CR, Dorin RI, Veldhuis JD, Baumgartner RN. Altered growth hormone, cortisol, and leptin secretion in healthy elderly persons with sarcopenia and mixed body composition phenotypes. J Gerontol A Biol Sci Med Sci. 2008;63:536–41.
Stanley TL, Grinspoon SK. Effects of growth hormone-releasing hormone on visceral fat, metabolic, and cardiovascular indices in human studies. Growth Horm IGF Res. 2015;25:59–65.
Poggiogalle E, Lubrano C, Gnessi L, Mariani S, Lenzi A, Donini LM. Fatty liver index associates with relative sarcopenia and GH/IGF-1 status in obese subjects. PLoS One. 2016;11:e0145811.
Kim TN, Won JC, Kim YJ, Lee EJ, Kim MK, Park MS, et al. Serum adipocyte fatty acid-binding protein levels are independently associated with sarcopenic obesity. Diabetes Res Clin Pract. 2013;101:210–7.
Milner KL, van der Poorten D, Xu A, Bugianesi E, Kench JG, Lam KS, et al. Adipocyte fatty acid binding protein levels relate to inflammation and fibrosis in nonalcoholic fatty liver disease. Hepatology. 2009;49:1926–34.
Girgis CM, Clifton-Bligh RJ, Hamrick MW, Holick MF, Gunton JE. The roles of vitamin D in skeletal muscle: form, function, and metabolism. Endocr Rev. 2013;34:33–83.
Dzik KP, Kaczor JJ. Mechanisms of vitamin D on skeletal muscle function: oxidative stress, energy metabolism and anabolic state. Eur J Appl Physiol. 2019;119:825–39.
Visser M, Deeg DJ, Lips P. Longitudinal Aging study amsterdam. low vitamin D and high parathyroid hormone levels as determinants of loss of muscle strength and muscle mass (sarcopenia): the longitudinal aging study amsterdam. J Clin Endocrinol Metab. 2003;88:5766–72.
Abramovitch S, Dahan-Bachar L, Sharvit E, Weisman Y, Ben Tov A, Brazowski E, et al. Vitamin D inhibits proliferation and profibrotic marker expression in hepatic stellate cells and decreases thioacetamide-induced liver fibrosis in rats. Gut. 2011;60:1728–37.
Zhai HL, Wang NJ, Han B, Li Q, Chen Y, Zhu CF, et al. Low vitamin D levels and non-alcoholic fatty liver disease, evidence for their independent association in men in East China: a cross-sectional study (Survey on Prevalence in East China for Metabolic Diseases and Risk Factors (SPECT-China)). Br J Nutr. 2016;115:1352–9.
Eliades M, Spyrou E, Agrawal N, Lazo M, Brancati FL, Potter JJ, et al. Meta-analysis: vitamin D and non-alcoholic fatty liver disease. Aliment Pharmacol Ther. 2013;38:246–54.
Nelson JE, Roth CL, Wilson LA, Yates KP, Aouizerat B, Morgan-Stevenson V, et al. Vitamin D Deficiency is associated with increased risk of non-alcoholic steatohepatitis in adults with non-alcoholic fatty liver Disease: possible role for MAPK and NF-kappaB? Am J Gastroenterol. 2016;111:852–63.
Patel YA, Henao R, Moylan CA, Guy CD, Piercy DL, Diehl AM, et al. Vitamin D is not associated with severity in NAFLD: results of a paired clinical and gene expression profile analysis. Am J Gastroenterol. 2016;111:1591–8.
Engin A. Non-alcoholic fatty liver disease. Adv Exp Med Biol. 2017;960:443–67.
Hui JM, Hodge A, Farrell GC, Kench JG, Kriketos A, George J. Beyond insulin resistance in NASH: TNF-alpha or adiponectin? Hepatology. 2004;40:46–54.
Wieckowska A, Papouchado BG, Li Z, Lopez R, Zein NN, Feldstein AE. Increased hepatic and circulating interleukin-6 levels in human nonalcoholic steatohepatitis. Am J Gastroenterol. 2008;103:1372–9.
Visser M, Pahor M, Taaffe DR, Goodpaster BH, Simonsick EM, Newman AB, et al. Relationship of interleukin-6 and tumor necrosis factor-alpha with muscle mass and muscle strength in elderly men and women: the Health ABC Study. J Gerontol A Biol Sci Med Sci. 2002;57:M326–32.
Baylis D, Bartlett DB, Syddall HE, Ntani G, Gale CR, Cooper C, et al. Immune-endocrine biomarkers as predictors of frailty and mortality: a 10-year longitudinal study in community-dwelling older people. Age (Dordr). 2013;35:963–71.
Camporez JP, Jornayvaz FR, Petersen MC, Pesta D, Guigni BA, Serr J, et al. Cellular mechanisms by which FGF21 improves insulin sensitivity in male mice. Endocrinology. 2013;154:3099–109.
Xu J, Lloyd DJ, Hale C, Stanislaus S, Chen M, Sivits G, et al. Fibroblast growth factor 21 reverses hepatic steatosis, increases energy expenditure, and improves insulin sensitivity in diet-induced obese mice. Diabetes. 2009;58:250–9.
Lan F, Misu H, Chikamoto K, Takayama H, Kikuchi A, Mohri K, et al. LECT2 functions as a hepatokine that links obesity to skeletal muscle insulin resistance. Diabetes. 2014;63:1649–64.
Yoo HJ, Hwang SY, Choi JH, Lee HJ, Chung HS, Seo JA, et al. Association of leukocyte cell-derived chemotaxin 2 (LECT2) with NAFLD, metabolic syndrome, and atherosclerosis. PLoS One. 2017;12:e0174717.
Hara H, Uchida S, Yoshimura H, Aoki M, Toyoda Y, Sakai Y, et al. Isolation and characterization of a novel liver-specific gene, hepassocin, upregulated during liver regeneration. Biochim Biophys Acta. 2000;1492:31–44.
Wu HT, Lu FH, Ou HY, Su YC, Hung HC, Wu JS, et al. The role of hepassocin in the development of non-alcoholic fatty liver disease. J Hepatol. 2013;59:1065–72.
Wu HT, Ou HY, Hung HC, Su YC, Lu FH, Wu JS, et al. A novel hepatokine, HFREP1, plays a crucial role in the development of insulin resistance and type 2 diabetes. Diabetologia. 2016;59:1732–42.
Jung TW, Chung YH, Kim HC, Abd El-Aty AM, Jeong JH. Hyperlipidemia-induced hepassocin in the liver contributes to insulin resistance in skeletal muscle. Mol Cell Endocrinol. 2018;470:26–33.
Boström P, Wu J, Jedrychowski MP, Korde A, Ye L, Lo JC, et al. A PGC1-alpha-dependent myokine that drives brown-fat-like development of white fat and thermogenesis. Nature. 2012;481:463–8.
Polyzos SA, Kountouras J, Anastasilakis AD, Geladari EV, Mantzoros CS. Irisin in patients with nonalcoholic fatty liver disease. Metabolism. 2014;63:207–17.
Zhang HJ, Zhang XF, Ma ZM, Pan LL, Chen Z, Han HW, et al. Irisin is inversely associated with intrahepatic triglyceride contents in obese adults. J Hepatol. 2013;59:557–62.
Choi HY, Kim S, Park JW, Lee NS, Hwang SY, Huh JY, et al. Implication of circulating irisin levels with brown adipose tissue and sarcopenia in humans. J Clin Endocrinol Metab. 2014;99:2778–85.
Chang JS, Kim TH, Nguyen TT, Park KS, Kim N, Kong ID. Circulating irisin levels as a predictive biomarker for sarcopenia: a cross-sectional community-based study. Geriatr Gerontol Int. 2017;17:2266–73.
Elkina Y, von Haehling S, Anker SD, Springer J. The role of myostatin in muscle wasting: an overview. J Cachexia Sarcopenia Muscle. 2011;2:143–51.
Wilkes JJ, Lloyd DJ, Gekakis N. Loss-of-function mutation in myostatin reduces tumor necrosis factor alpha production and protects liver against obesity-induced insulin resistance. Diabetes. 2009;58:1133–43.
Steffl M, Bohannon RW, Sontakova L, Tufano JJ, Shiells K, Holmerova I. Relationship between sarcopenia and physical activity in older people: a systematic review and meta-analysis. Clin Interv Aging. 2017;12:835–45.
Johnson NA, Sachinwalla T, Walton DW, Smith K, Armstrong A, Thompson MW, et al. Aerobic exercise training reduces hepatic and visceral lipids in obese individuals without weight loss. Hepatology. 2009;50:1105–12.
Garatachea N, Lucía A. Genes and the ageing muscle: a review on genetic association studies. Age. 2013;35:207–33.
Jones G, Pilling LC, Kuo CL, Kuchel G, Ferrucci L, Melzer D. Sarcopenia and variation in the human leukocyte antigen complex. J Gerontol A Biol Sci Med Sci. 2019. https://doi.org/10.1093/gerona/glz042.
Eslam M, Valenti L, Romeo S. Genetics and epigenetics of NAFLD and NASH: clinical impact. J Hepatol. 2018;68:268–79.
Franko A, Merkel D, Kovarova M, Hoene M, Jaghutriz BA, Heni M, et al. Dissociation of fatty liver and insulin resistance in I148 M PNPLA3 carriers: differences in diacylglycerol (DAG) FA18:1 lipid species as a possible explanation. Nutrients. 2018;10:1314.
Palmer CN, Maglio C, Pirazzi C, Burza MA, Adiels M, Burch L, et al. Paradoxical lower serum triglyceride levels and higher type 2 diabetes mellitus susceptibility in obese individuals with the PNPLA3 148 M variant. PLoS One. 2012;7:e39362.
Jegatheesan P, De Bandt J-P. Fructose and NAFLD: the multifaceted aspects of fructose metabolism. Nutrients. 2017;9:230.
Acknowledgements
This work was supported in part by a grant of Korea University.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Jung A. Kim and Kyung Mook Choi have no conflicts of interest to disclose.
Ethical approval
This article does not contain any studies with human or animal subjects.
Informed consent
Informed consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kim, J.A., Choi, K.M. Sarcopenia and fatty liver disease. Hepatol Int 13, 674–687 (2019). https://doi.org/10.1007/s12072-019-09996-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12072-019-09996-7