Abstract
Aims
We investigated the correlation between the red cell distribution width (RDW) and RDW-to-platelet ratio (RPR) with the degree of inflammation and fibrosis in chronic hepatitis patients with different etiologies and in native and transplanted liver.
Methods
Between 2010 and 2013, patients from the MedStar Washington Hospital Center and Georgetown University Hospital with chronic hepatitis B, chronic hepatitis C, alcoholic hepatitis, and primary biliary cirrhosis who had a biopsy of the liver done in this time period were included. The correlation among the RDW, RPR, and model for end-stage liver disease (MELD) score with the degree of liver inflammation, fibrosis, and cirrhosis in separate groups of native and transplanted liver was calculated.
Results
A total of 152 cases with native liver and 70 cases with transplanted liver were included. The majority of patients had hepatitis C in both groups. None of the investigated variables showed significant correlation with the degree of inflammation in either group. The strongest correlation with the degree of fibrosis in the native liver group was for the RPR with 0.51 (p < 0.001) and then the RDW and MELD with 0.34 (p < 0.001) and 0.31 (p < 0.001), respectively. In the transplanted liver group, none of the variables showed significant correlation with the degree of fibrosis. The receiver-operator curve showed that only the RDW and RPR in the native liver group, with areas under the curve of 0.770 and 0.684, respectively, have significantly positive association with the risk of cirrhosis. In the transplanted group, none of the predictors were associated with risk of cirrhosis. In the native liver group, a cutoff value of 0.088 in the RPR led to 82.7 % sensitivity and 61.0 % specificity to predict cirrhosis.
Conclusion
The RPR can be a strong predictor of the degree of fibrosis and cirrhosis in patients with chronic hepatitis and native liver. It shows higher accuracy compared to the RDW and MELD score. However, its use in predicting inflammation is limited.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Red cell distribution width (RDW), a measure of the variability in the size of circulating erythrocytes, is a routine component of the complete blood count. The RDW has been shown to be an independent marker of mortality in multiple cardiovascular diseases and interventions (such as percutaneous coronary interventions), renal, and infectious disease [1–4]. Recent studies show that RDW values are significantly increased in hepatitis B patients and RDW is an independent 3-month mortality risk predictor in this population [5–7]. Other studies have shown that the RDW-to-platelet ratio (RPR) can be a predictor of significant fibrosis and cirrhosis in patients with chronic hepatitis B, and it was hypothesized that the high RDW due to anemia and the low platelet count due to cirrhosis may explain this finding [8]. However, there are no studies to investigate the role of the RDW or RPR in other chronic hepatitis types and also in transplanted liver.
There are several noninvasive methods using laboratory tests to predict the severity of chronic liver disease, and one of the most widely used ones is the model for end-stage liver disease (MELD) [9]. It was originally used to predict death within 3 months of surgery in patients after the transjugular intrahepatic portosystemic shunt (TIPS) and was subsequently found to be helpful in determining prognosis and prioritizing receiving a liver transplant [10, 11]. Given the low cost and ease of measuring these blood indices, finding a correlation with these variables can decrease the need for performing liver biopsy in chronic hepatitis and transplanted patients. Therefore, we attempted to investigate the correlation between RDW and RPR in comparison to inflammation and fibrosis detected by biopsy in patients with chronic hepatitis B (CHB), chronic hepatitis C (CHC), primary biliary cirrhosis (PBC), and alcoholic hepatitis. We also studied these correlations in patients who had previously undergone orthotopic liver transplantation. In addition, we compared these methods with the MELD score to better understand the usefulness of these indices.
Materials and methods
We included the patients from the MedStar Washington Hospital Center and MedStar Georgetown University Hospital between the years 2010–2013 with the initial diagnosis of chronic hepatitis B, chronic hepatitis C, alcoholic hepatitis, and primary biliary cirrhosis who had a biopsy of the liver done in this time period. For all subjects, demographic data were obtained. We retrieved the pathology reports for the liver biopsy and values for the RDW, platelet count, international normalized ratio (INR), creatinine, and bilirubin, measured within a week of performing the biopsy. The RDW and platelet count were measured by Sysmex XE-5000, INR by Stago-Compact Max, and creatinine and bilirubin by Siemens Vista-1500. Then we calculated the MELD score and RPR for each patient. The MELD score was calculated using the web site calculator (http://www.mayoclinic.org/gi-rst/mayomodel7.html). Patients with hepatocellular carcinoma were excluded from the study.
Ethics statement
This study was reviewed and approved by the Institutional Review Board of MesdStar Health Research Institute.
Histological assessment of the liver
Liver inflammation was determined by the Batts-Ludwig 5-point scale [12]: grade 0: no or minimal inflammation; grade 1: portal inflammation or lobular inflammation without necrosis; grade 2: mild periportal inflammation and piecemeal necrosis or focal hepatocellular necrosis; grade 3: moderate periportal inflammation and piecemeal necrosis or severe focal cell damage; grade 4: severe periportal inflammation and piecemeal necrosis or bridging necrosis.
Degree of fibrosis was retrieved from the pathology reports evaluated by the Batts-Ludwig 5-point scale [12]: stage 0: no fibrosis; stage 1: enlarged fibrotic portal tracts; stage 2: periportal fibrosis or portal-to-portal septa, without architectural distortion; stage 3: bridging fibrosis with architectural distortion and no obvious cirrhosis; stage 4: cirrhosis.
Statistical analysis
Descriptive statistics for baseline characteristics were performed by Fisher’s exact test for categorical variables and Wilcoxon rank-sum test for continuous variables. The Spearman rank correlation test was used to detect a monotonic trend in the laboratory results with an increase in the severity level of inflammation or fibrosis. Patients with native liver or transplanted liver were analyzed separately. To obtain the best predictor of the risk of cirrhosis from the laboratory data, we developed logistic regression models with using the RDW, RPR, or MELD score, respectively, as a predictor. The odds ratio with the associated 95 % confidence interval for each predictor was estimated. The performance of discrimination for each model was evaluated by the receiver-operating characteristic (ROC) curve analysis. We estimated the area under the ROC curve (AUC) of each model with the associated 95 % confidence interval. In addition, the ROC contrast test [13] was performed to compare the difference in AUC between each model. Finally, we used Youden’s index [14], defined as sensitivity + specificity − 1, to determine the cutoff value for the optimal combination of sensitivity and specificity. Data analysis was performed with the statistical software package SAS™ 9.3 (SAS Institute, Cary, NC, USA).
Results
During the study period there were 152 cases with native liver and 70 with transplanted liver. The majority of patients in both groups were African-American. Chronic hepatitis C was the dominant type of hepatitis in both groups. Most patients with native liver had grade 1 inflammation and stage 4 fibrosis, and grade 2 inflammation and stage 2 fibrosis were the most prevalent in the transplanted liver group. The RDW and MELD score did not show a significant difference between the two groups, but the RPR was significantly lower in the native liver group (Table 1).
None of the investigated variables showed significant correlation with the degree of inflammation in the native or transplanted liver groups. The strongest correlation with the degree of fibrosis in the native liver group was for RPR with 0.51 (p < 0.001) and then RDW and MELD with 0.34 (p < 0.001) and 0.31 (p < 0.001), respectively. In the transplanted liver group none of the variables showed a significant correlation with the degree of fibrosis (Table 2).
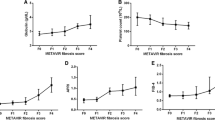
Analyses from logistic regression models indicate that only RDW and RPR in the native liver group showed a significantly positive association with the risk of cirrhosis (Table 3). One unit increase in RDW led to an 18.4 % increase in the odds of cirrhosis. For every 0.1 unit increase in RPR, the odds of having cirrhosis increased by a factor of 3.76. For the ROC analysis (Fig. 1), the highest AUC was the RPR model with 0.770 followed by the RDW (0.684) and MELD (0.613) in the native liver group. The confidence interval of AUC for each model did not contain 0.5, indicating a significant difference from random guessing. The ROC contrast test shows a significant difference in AUC between the RPR and MELD, but not between the RPR and RDW. In the transplanted liver group, all three predictors as continuous variables were not significantly associated with the risk of cirrhosis (Table 3). For the measures of discriminative ability, the RPR model had the highest AUC with 0.693, followed by the MELD model (0.688). Both AUCs were significantly greater than 0.5 and did not show a significant difference from each other (p = 0.892). The confidence interval of the AUC for the RDW model contained 0.5; hence, this model did not show significant discriminative ability (Fig. 2).
After determining the optimal cutoff by Youden’s index, the RPR had the highest positive predictive value (PPV) and negative predictive value (NPP) in both groups (Table 3).
In the native liver group, a cutoff value of 0.088 in the RPR led to 82.7 % sensitivity and 61.0 % specificity to predict the event of cirrhosis. In the transplanted liver group, using a cutoff value of 0.174 could reach 75 % sensitivity and 75.8 % specificity.
Discussion
The aim of this study was to test the usefulness of a simple and inexpensive approach to predict inflammation and fibrosis in native and transplanted liver in patients with chronic hepatitis, using easily available hematological CBC parameters. RDW reflects the variability in circulating RBC size and is based on the width of the RBC volume distribution curve. Higher values indicate greater variability [15]. RDW may reflect a nutritional deficiency, chronic inflammation, or bone marrow depression [16, 17]. These conditions are common in patients with liver disease, correlate with the severity of the disease, and are related to worse prognosis [18]. Another situation that may result in an increase in RDW is hemolytic anemia, which is commonly present in patients with chronic liver disease and cirrhosis [19]. Thrombocytopenia is also a known complication of chronic liver disease and cirrhosis, and the platelet count has been used in different predictive models for liver fibrosis and cirrhosis [8].
In the study by Lou et al. [5] and Karagoz et al. [6], RDW values were significantly increased in hepatitis B patients, and the elevation was correlated with the severity of the disease. RDW was also shown to be an independent predicting factor for 3-month mortality in these patients. Our study showed in a patient population comprising different hepatitis types, with the majority being hepatitis C patients, RDW has a statistically significant correlation with the degree of fibrosis in native liver. This correlation was slightly stronger than the correlation between the MELD score and liver fibrosis. However, the correlation between the RDW and degree of inflammation in native liver was not significant. RDW was not significantly correlated with either inflammation or fibrosis in the transplanted liver group. This may be related to either the smaller sample size in this group or significantly lower fibrosis in the transplanted liver group compared to the native liver group.
A study by Chen et al. [8] showed that in patients with chronic hepatitis B, RPR is an accurate tool for predicting significant fibrosis and cirrhosis. In their study, the AUC for predicting severe fibrosis and cirrhosis was 0.882 and 0.885, respectively. Our study showed that the RPR was significantly correlated with the degree of fibrosis in native liver. This correlation was the strongest compared to the RDW and MELD score. Similar to the MELD score and RDW, RPR failed to show a significant correlation with inflammation in native liver, which may be attributable to the lower fibrosis level in the transplanted liver group or its smaller sample size.
The RPR also showed the highest area under the curve (AUC) in the receiver-operating characteristic (0.770) and highest positive and negative predictive values when compared to the RDW and MELD score for predicting cirrhosis in native liver. This is concordant with the results of the study by Chen et al. [8] that showed RPR could be a useful and accurate tool for predicting cirrhosis and severe fibrosis in chronic hepatitis B patients. However, our study had a sample size of different hepatitis categories with a majority of patients with chronic hepatitis C. This shows that the RPR can be a useful tool to predict the degree of fibrosis and cirrhosis in other forms of chronic hepatitis as well. None of the tested variables could significantly predict cirrhosis in the transplanted liver. This may be attributable to the very small number of patients with cirrhosis in the transplanted liver group.
The mechanism of association between RDW and liver fibrosis is not well understood. A recent study by Lippi et al. [20] showed RDW has a strong and graded correlation with the degree of inflammatory markers, which was independent of ferritin, age, sex, and other hematological variables. Another prospective study showed that RDW elevation might be an indicator of inflammatory stress and impaired iron mobilization [21]. Iron overload and inflammation may subsequently contribute to the hepatic fibrosis [22]. The role of platelets in the progression of fibrosis is also not clear. In a recent study by Knight et al. [23] it was shown that platelets alleviate liver fibrosis through the decreased expression of the principal profibrogenic cytokine TGF-b and the increased expression of matrix metalloproteinases. This suggests a negative correlation between platelets and liver fibrosis [8].
The current study has several limitations. The patients were retrospectively enrolled in the study. In addition, due to the lack of data, we did not investigate the possible causes that may affect RDW values, such as iron or vitamin B12 deficiency. We also did not include the data regarding the antiviral therapy for these patients, and the possible effect of antiviral medications on blood indices were not studied.
In conclusion, the current study shows that the RPR can be a useful predictor of the degree of fibrosis and cirrhosis in patients with chronic hepatitis and native liver. Because RDW and platelet values are easily available at no additional cost to the routine complete blood cell counts and are highly reproducible, it may serve as an important biomarker and potentially reduce the need for liver biopsy in this patient population. Further studies are needed to validate this index in different types of hepatitis. Studies with a larger sample size of transplanted liver patients are also warranted to study this index in this patient population.
References
Zalawadiya SK, Veeranna V, Niraj A, Pradhan J, Afonso L. Red cell distribution width and risk of coronary heart disease events. Am J Cardiol 2010;106:988–993
Patel KV, Ferrucci L, Ershler WB, Longo DL, Guralnik JM. Red blood cell distribution width and the risk of death in middle-aged and older adults. Arch Intern Med 2009;169:515–523
Horne BD. A changing focus on the red cell distribution width: why does it predict mortality and other adverse medical outcomes? Cardiology 2012;122:213–215
Bojakowski K, Dzabic M, Kurzejamska E, Styczynski G, Andziak P, et al. A high red blood cell distribution width predicts failure of arteriovenous fistula. PLoS One 2012;7:e36482
Lou Y, Wang M, Mao W. Clinical usefulness of measuring red blood cell distribution width in patients with hepatitis B. PLoS One 2012;7:e37644
Karagoz E, Ulcay A, Tanoglu A, Kara M, Turhan V, et al. Clinical usefulness of mean platelet volume and red blood cell distribution width to platelet ratio for predicting the severity of hepatic fibrosis in chronic hepatitis B virus patients. Eur J Gastroenterol Hepatol 2014;26:1320–1324
Huang R, Yang C, Wu K, Cao S, Liu Y, et al. Red cell distribution width as a potential index to assess the severity of hepatitis B virus-related liver diseases. Hepatol Res 2014;44:E464–E470
Chen B, Ye B, Zhang J, Ying L, Chen Y. RDW to platelet ratio: a novel noninvasive index for predicting hepatic fibrosis and cirrhosis in chronic hepatitis B. PLoS One 2013;8:e68780
Malinchoc M, Kamath PS, Gordon FD, Peine CJ, Rank J, et al. A model to predict poor survival in patients undergoing transjugular intrahepatic portosystemic shunts. Hepatology 2000;31:864–871
Kamath PS, Wiesner RH, Malinchoc M, Kremers W, Therneau TM, et al. A model to predict survival in patients with end-stage liver disease. Hepatology 2001;33:464–470
Kamath PS, Kim WR, Advanced Liver Disease Study G. The model for end-stage liver disease (MELD). Hepatology. 2007;45:797–805
Batts KP, Ludwig J. Chronic hepatitis. An update on terminology and reporting. Am J Surg Pathol 1995;19:1409–1417
DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics 1988;44:837–845
Youden WJ. Index for rating diagnostic tests. Cancer 1950;3:32–35
Huo TI, Wu JC, Lin HC, Lee FY, Hou MC, et al. Evaluation of the increase in model for end-stage liver disease (DeltaMELD) score over time as a prognostic predictor in patients with advanced cirrhosis: risk factor analysis and comparison with initial MELD and Child-Turcotte-Pugh score. J Hepatol 2005;42:826–832
Karnad A, Poskitt TR. The automated complete blood cell count. Use of the red blood cell volume distribution width and mean platelet volume in evaluating anemia and thrombocytopenia. Arch Intern Med 1985;145:1270–1272
Thompson WG, Meola T, Lipkin M Jr, Freedman ML. Red cell distribution width, mean corpuscular volume, and transferrin saturation in the diagnosis of iron deficiency. Arch Intern Med 1988;148:2128–2130
Evans TC, Jehle D. The red blood cell distribution width. J Emerg Med 1991;9(Suppl 1):71–74
McHutchison JG, Manns MP, Longo DL. Definition and management of anemia in patients infected with hepatitis C virus. Liver Int 2006;26:389–398
Lippi G, Targher G, Montagnana M, Salvagno GL, Zoppini G, et al. Relation between red blood cell distribution width and inflammatory biomarkers in a large cohort of unselected outpatients. Arch Pathol Lab Med 2009;133:628–632
Allen LA, Felker GM, Mehra MR, Chiong JR, Dunlap SH, et al. Validation and potential mechanisms of red cell distribution width as a prognostic marker in heart failure. J Card Fail 2010;16:230–238
Coursaget P, Buisson Y, N’Gawara MN, Van Cuyck-Gandre H, Roue R. Role of hepatitis E virus in sporadic cases of acute and fulminant hepatitis in an endemic area (Chad). Am J Trop Med Hyg 1998;58:330–334
Knight V, Tchongue J, Lourensz D, Tipping P, Sievert W. Protease-activated receptor 2 promotes experimental liver fibrosis in mice and activates human hepatic stellate cells. Hepatology 2012;55:879–887
Acknowledgements
This project was funded in part by federal funds (grant no. UL1TR000101, previously UL1RR031975) from the National Center for Advancing Translational Sciences (NCATS), National Institutes of Health (NIH), through the Clinical and Translational Science Awards Program (CTSA), a trademark of DHHS, part of the Roadmap Initiative, “Re-Engineering the Clinical Research Enterprise.”
Compliance with Ethical Requirements and Conflict of interest
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008 (5). This study was reviewed and approved by the Institutional Review Board of MesdStar Health Research Institute. Amir Taefi, Chun-Chih Huang, Kirthi Kolli, Suzan Ebrahimi, and Mitesh Patel declare that they have no conflict of interests.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Taefi, A., Huang, CC., Kolli, K. et al. Red cell distribution width to platelet ratio, a useful indicator of liver fibrosis in chronic hepatitis patients. Hepatol Int 9, 454–460 (2015). https://doi.org/10.1007/s12072-015-9638-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12072-015-9638-9