Abstract
Significant number of patients diagnosed with chronic rhino sinusitis often tend to have a final diagnosis of fungal sinusitis. We wanted to find out (a) The incidence of patients with fungal sinusitis in those patients who were initially diagnosed as chronic rhinosinusitis. (b) The presentation of fungal sinusitis patients who were initially diagnosed as CRS. Retrospective chart review of 242 patients diagnosed as CRS from May 2006 to April 2009. The various symptoms and signs of those diagnosed initially as CRS, who were then diagnosed as fungal sinusitis were tabulated. Radiological and serological investigations were then analyzed. The microbiology of various species that were cultured in those identified as fungal sinusitis were also presented. Out of 242 patients diagnosed with CRS, 67 patients had clinical and radiological evidence of fungal sinusitis but only 24 of these patients had fungal organisms identified. Majority of them were Aspergillus fumigatus. Clinical suspicion of fungal sinusitis should be made in those patients presenting with CRS with the following signs and symptoms of nasal obstruction, discharge and polyps. Most of those fungus were Aspergillus fumigatus and responded well to treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Fungal infection of the nose and paranasal sinuses was thought to be an uncommon condition and was diagnosed rarely. But it is not like that. Even diagnosis was made in immunocompetent individuals. With the advent of nasal endoscope and CT scan and the tendency of the surgeons to subject all the removed tissues for biopsy and also the pathologist doing special fungal stains in suspected material, a high percentage of positive report for fungal infection has been noticed.
Knowledge of the fungal organism is important in directing appropriate anti fungal therapy. Aspergillosis is the commonest fungal infection of the nose and paranasal sinuses and seven pathogenic species have been described. Of these, Aspergillus fumigatus (90%) is the most common fungal pathogen followed by Aspergillus niger and Aspergillus flavus. Mucormycosis, Candidiasis may also occur. Maxillary sinuses are commonly involved [1].
Materials and Methods
The clinical material consisted of total number of 242 patients came to ENT department of MGMCRI between May 2006 and April 2009 with features suggestive of chronic sinusitis. Based on clinical and radiological parameters, 67 cases were diagnosed to have mycotic infections. In these cases, postoperatively after HPE examination, 24 cases were confirmed to have mycotic infection.
The diagnosis of fungal infection was based on:
-
Detailed history and clinical assessment was noted from each patient on admission and the data entered in the proforma,
-
Plain X-ray nose and paranasal sinuses (water’s view),
-
CT scan nose and paranasal sinuses (Axial and coronal view),
-
Diagnostic nasal endoscopy,
-
Microscopic examination of material (i.e) sinus mucosa and nasal polyp in wet mount KOH preparation,
-
Histopatholgical examination of biopsy material with special stain,
-
Fungal culture in Sabouraud’s dextrose agar (Fig. 1).
Observations and Results
The findings are based on the study of 242 cases of chronic rhino sinusitis with or without polyps. Of these 105 patients had undergone FESS. Of these, 67 cases were diagnosed to be of fungal etiology based on clinical and radiological parameters. All the specimens were submitted for histopathological examination for fungal stains and fungal culture. Of theses, 24 cases were confirmed to be fungal etiology. The patients evaluations and observations were as follows:
-
1.
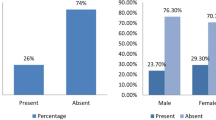
Age/Sex ratio––Out of 67 cases diagnosed to have fungal sinus disease, 35 patients were male and 32 were female patients. The sex ratio being equal, age varied from 14–63 years. The majority of patients belonged to the age group of third decade.
-
2.
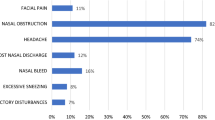
Mode of presentation––23 patients presented with feature of chronic sinusitis. 42 patients presented with polyp. (Bilateral–32, Right–6, Left–4). Two patients presented with unilateral nasal polyp and proptosis and of these, one were poorly controlled diabetic (Chart 1). Of these 67 patients, 15 were diagnosed to have atopy based on skin prick tests and fungal mass was found in eight cases, diagnosed by nasal endoscopy.
-
3.
Endoscopic findings––Pre-op nasal endoscopy revealed bilateral multiple ethmoidal polyps in 32 patients, unilateral polyp in 12 cases, purulent nasal discharge in the middle meatus in 13 patients and dried black crusts in one case. The remaining patients had osteo-meatal complex obstruction due to deviated nasal septum, concho bullosa etc.
-
4.
Radiological findings––Pre-op CT scan was taken in all suspected cases. Homogenous opacities were noted in 56%. Heterogenous opacities (Fig. 2) were seen in 32%. Mucosal thickening was observed in 10%. Heterogenous opacity with bone involvement was seen in 2% (Chart 2).
-
5.
Histopathological examination––Histopathological examination of the polyps and polypoidal mucosa was done in all 67 patients. HPE of the biopsy material with special (Lactophenol cotton blue) stain (Fig. 3) was positive for pathogenic fungi in 24 patients. Of these, culture was positive in all 24 patients.(A. fumigatus–16, A. flavus–3, Mucor–2, Candida–3) (Chart 3).
-
6.
Treatment––All the cases have undergone FESS. Aspergillus positive patients were given itraconazole 200 mg OD for one month. Mucormycosis patients were treated with systemic amphoterin–B (1.5–2 g). Postoperatively one patient with candidiasis was given local amphotericin-B (50 mg diluted in 20 ml of normal saline as nasal drops) for three months. Hepatic and renal functions were monitored in these patients.
Discussion
Fungal paranasal sinus disease is not as rare a disease as previously assumed. A dramatic increase in the number and diversity of reported has observed over the past two decades.
Over the last two decades, it has become clear that it is important to classify fungal rhinosinusitis to accurately predict prognosis and optimize effective therapy. This classification is based on immunological relationship of the fungus to the host [2]. There are two basic type of fungal disease: invasive and non invasive. These may be further subdivided into five distinct entities as illustrated below.
Host defense | Immunocompromised | Immunocompetent | Atopic |
|---|---|---|---|
Fungal form | 1. Invasive | 2. Granulomaous | 5. AFRS |
3. Saprophytic | |||
4. Fungal Ball |
Aspergillosis was one of the first fungal diseases of man or animals recognized. The name aspergillus had been coined by the florantine botanist Micheli in his “Nova Plantarum Genera” of 1729. The Aspergillum (Latin “to sprinkle”) referred to a perforated globe used to sprinkle holy water during religious ceremonies.
The term “Aspergillosis” was first utilized by Fresenius in 1850 in his work on a fungus infection of the air sac of a bird the bustard from the Frankfurt zoo. He named the isolate Aspergillus fumigates. Human infection was recognized by Bennett in 1842. The first case of Aspergillosis of the nose and the para nasal sinuses was reported by Schubert in 1885.
The exact pathophysiology of allergic fungal sinusitis remains a matter of controversial. Current data suggest that the etiology of the disease may be a mucosal hypersensitivity, directed against fungal antigens deposited on sinus mucosa (i.e.) immunologic hypersensitivity rather than infection.
According to Katzenstein et al. [3], the diagnostic feature of AFRS is “Allergicmucin”––a pale eosinophilic or basophilic mucoid material in which are found eosinophils, sloughed epithelial cells, cellular debris and charcot leyden as well as other crystals, associated with sinus bone remodeling and erosion.
Bent and Kuhn’s [4] Criteria for the Diagnosis of AFRS
Major Criteria
-
1.
Type I hypersensitivity
-
2.
Nasal polyposis
-
3.
Characteristics CT scan findings
-
4.
Presence of eosinophilic mucus
-
5.
Positive fungal smear
Minor Criteria
-
1.
Young individuals
-
2.
Co-existence asthma
-
3.
Unilateral predominance
-
4.
Radiographic bone erosion
-
5.
Fungal culture
-
6.
Charcot leyden crystals
-
7.
Serum eosinophilia.
Kupferberg et al. [5] refined the endoscopic follow up into a staging system, which allows closer control of the mucosal response to medical management (i.e.) oral steroids.
Stage | Endoscopic finding |
|---|---|
0 | No mucosal edema or alleric mucin |
1 | Mucosal edema with or without allergic mucin |
2 | Polypoidal edema with or without allergic mucin |
3 | Sinus polyps with fungal debris or allergic mucin. |
In addition to absolute increase in the morbidity rate, apparently favoured by use of antibiotics and predisposing factors such as diabetics, tumours, reduced physical resistance etc. It is certainly the improved diagnostic methods that account for the increase in the number of cases diagnosed.
Aspergillus is a common endogenous contaminant of the upper respiratory tract [6]. However, bacterial sinusitis may trigger its growth and proliferation. Aspergillus fumigates is the common organism in fungal sinusitis. In 1972, 37 cases had been reported with 17 by a single author [7]. Clinical signs and symptoms are non specific at first.
Fungal ball or mycetoma typically appears on CT scan as a heterogenous opacity often associated with microcalcification and even with metal dense spots. Heterogenous opacity was seen in 32% of my patients. CT scan evidence of sinus expansion with central areas of irregular heterogenous opacity should have suspicion of allergic fungal sinusitis. This is due to fungus having high affinity towards metallic salts (ca, mg). MR imaging, however is superior to CT in delineating intra cranial extent of disease [8, 9].
In my study of 67 patients, 23 patients presented history of chronic sinusitis, 32 patients presented with bilateral ethmoidal polyps, 10 patients presented with unilateral nasal polyp and 2 patients presented with mucormycosis.
The benefit of antifungal therapy in AFRS remains unproven, although sinus irrigation with antifungal agents has been proposed as a potential allergic fungal sinusitis treatment method. A reason study on treatment AFRS with post-op immunotherapy with specific fungal antigens demonstrate a dramatic reduction in mucosal edema and polyp formation, markedly lessened corticosteroids requirement and improved quality of life in AFRS patients as compared with a similar group not receiving such immunotherapy.
Interesting feature of the fulminant invasive aspergillosis is its variation in biological behavior in different geographical settings. Invasive aspergillosis is a disease of immunosuppressed, very ill patients in the west, while it is fairly common in parts of India, middle east and sudan to see invasion of skull base and orbit in perfectly healthy immunocompetent subjects.
Mucormycosis affects immunosuppressed patients and more than 75% of the cases involve patients suffering diabetics [10]. In my study, I have seen two cases of mucormycosis, one presented with diabetic ketoacidosis and other also a diabetic. Aggressive surgical debridement was done followed by systemic antifungal therapy were given.
Until today, the method of choice of invasive or fulminant aspergillosis and mucormycosis of the PNS is complete removal of affected structures. In cases of incomplete removal, post operative antimycotic drug treatment should be given. The colour of the mucosa is noted carefully, and any pale or grey areas may represent the earliest sign of tissue infarction caused by fungal invasion of blood vessels. Decreased pain reception is easily detected by touching the areas of suspicious mucosa with a metal suction tip or the wooden end of a cotton tipped applicator which indicates increasing mucosal necrosis.
In our study, all aspergillus infections occurred in immunocompetent patients and patients who had mucormycosis were poorly controlled diabetics.
Conclusion
The incidence of sinonasal mycotic infection is about 10% of chronic rhinosinusitis. The commonest age group is third decade and sex ratio is equal. Clinical suspicion of fungal sinusitis should be made in those patients presenting with CRS with the following signs and symptoms of nasal obstruction, discharge and polyps. CT scan, DNE and histopathological examination of all sinus specimens have made the diagnosis much more easier. All aspergillus infections were observed in immunocompetent patients and mucormycosis in immunocompromised patients. Endoscopic sinus surgery followed by antifungal therapy plays a major role in the treatment of fungal sinusitis. Because of the recent increase in fungal infection of nose and paranasal sinuses, otorhinolaryngolgists must keep fungal infection in mind in their daily practice.
References
Millar JW, Johnston A, Lamb D (1981) Allergic aspergillosis of the maxillary sinuses (abstract). Thorax 36:710
Ence BK, Gourely DS, Jorgensen NL et al (1990) Allergic fungal sinusitis. Am J Rhinol 4:169–178
Katzenstein AA, Sale SR, Greenberger PA (1983) Allergic aspergillus sinusitis, a newly recognized form of Sinusitis. J Allergy Clin Immunol 72:89–93
Bent JP, Kuhn FA (1994) The diagnosis of allergic fungal sinusitis. Otolaryngol Head Neck Surg 111:580–588
Kupferberg SB, Bent JP, Kuhn FA (1997) Prognosis for allergic fungal sinusitis. Otolaryngol Head Neck Surg 117:35–41
Allphin AL, Strauss M (1991) Allergic fungal sinusitis, problems in diagnosis and treatment. Laryngoscope 101:815–820
Romeet JL, Newman RK (1982) Aspergillosis of the nose and paranasal sinuses. Laryngoscope 92:764–766
Gillespie MB, O’ Malley BW, Francis HW (1998) An approach to fulminant invasive fungal rhinosinusitis in the immunocompromised host. Arch Otolaryngol Head Neck Surg 124:520–526
Silverman CS, Mancuso AA (1998) Periantral soft-tissue infiltration and its relevance to the early detection of invasive fungal sinusitis: CT and MR findings. Am J Neuroradiol 19:321–325
Pillsbury HCC, Fischer ND (1977) Rhinocerebral mucormycosis. Arch Otolaryngol Head Neck Surg 103:600–604
Acknowledgments
I thank Dr.T.M.Karthikeyan, Assistant Professor, Department of pathology, and Dr.S.Umadevi, Assistant Professor, Department of Microbiology, MGMC& RI for their help.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Karthikeyan, P., Nirmal Coumare, V. Incidence and Presentation of Fungal Sinusitis in Patient Diagnosed with Chronic Rhinosinusitis. Indian J Otolaryngol Head Neck Surg 62, 381–385 (2010). https://doi.org/10.1007/s12070-010-0062-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-010-0062-0