Abstract
Traumatic brain injuries (TBI) manifest into post-traumatic stress disorders such as anxiety comorbid with gut ailments. The perturbations in gut microbial communities are often linked to intestinal and neuropsychological disorders. We have previously reported anxiety and abnormalities in gut function in mild TBI (MTBI)-exposed rats. The current study demonstrates the changes in gut microbiome of MTBI-exposed animals and discusses its implications in intestinal health and behaviours. The rats were subjected to repeated MTBI (rMTBI) and microbial composition in jejunum was examined after 6 h, 48 h and 30 days of rMTBI. Significant reduction in bacterial diversity was observed in the rMTBI-exposed animals at all the time points. Principal coordinate analysis based on weighted UniFrac distances indicated substantial differences in gut microbial diversity and abundances in rMTBI-exposed animals as compared to that in healthy controls. The abundance of Proteobacteria increased dramatically with reciprocal decrease in Firmicutes after rMTBI. At the genus level, Helicobacter, Lactobacillus, Campylobacter, and Streptococcus were found to be differentially abundant in the jejunum of rMTBI-exposed rats as compared to sham controls indicating profound dysbiosis from the healthy state. Furthermore, substantial depletion in butyrate-producing bacterial communities was observed in rMTBI-exposed animals. These results suggest that the traumatic stress alters the gut microbiome with possible implications in gut health and neuropsychopathology.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
The advent of recent high-throughput sequencing technologies led to gain deeper insights into the understanding of various host–microbe interactions. On similar lines, studies on gut microbiota have attracted considerable attention in recent years, with a special emphasis on its impact on multiple aspects of host physiology. Gut microbiome plays an integral role in host metabolism, homeostasis maintenance, nutrition, and immune function (Tremaroli and Bäckhed 2012; Round and Mazmanian 2009). These microbes synthesize vitamins, amino acids, and metabolites such as short-chain fatty acids (SCFA; Bull and Plummer 2014). Therefore, characterization of the gut microbial communities holds paramount importance in understanding the host–microbe interplay in health and disease. Recently, a growing body of evidence linked perturbations in the gut microbiome to various metabolic and comorbid neuropsychiatric disorders such as autism, depression, schizophrenia, obesity, type 2 diabetes mellitus, rheumatoid arthritis, etc. (Grochowska et al. 2018; Shreiner et al. 2015).
The bacteria associated with the human host are reported to be of the same order as the count of human cells (Sender et al. 2016). The consortium of bacteria colonising the gut play a crucial role in regulating the gut–brain axis; hence it is also referred as gut–microbiome–brain axis (Cenit et al. 2017). The comorbidity of stress-induced neuropsychiatric disorders and gastroenteric ailment implicate the importance of bidirectional communication between the gut–brain axis in pathophysiology of stress (Carabotti et al. 2015). Disruption of the gut–microbiome–brain axis is recently reported in diseases such as irritable bowel syndrome (IBS), autism spectrum disorders, Parkinson’s disease and disorders of mood, anxiety and chronic pain (Mayer et al. 2015). Specifically, alterations in gut microbiome have been associated to dysregulation of microglial activity, blood–brain barrier disruption along with impairment of neuropsychiatric activities leading to anxiety, abnormal behaviour and cognition (Logsdon et al. 2018; Cenit et al. 2017).
Tannock and Savage in 1974, have suggested that neuropsychological stress induced dysregulation of the hypothalamic–pituitary axis can influence gut microbiota (Tannock and Savage 1974). Traumatic brain injuries (TBI) including concussions result in psychological and physiological disturbances in the clinical population (Karr et al. 2014). The TBI is commonly found comorbid with abnormalities in gut functions such as gut motility, permeability, and inflammation (Mayer 2000; Drossman 2011). Gastrointestinal dysfunction is one of the most common, but neglected consequences of TBI (Kharrazian 2015; Zhu et al. 2018). Abnormalities in gut motility and mucosal alterations are frequently observed in TBI patients that can lead to ulceration and inflammation (Kao et al. 1998; Hang et al. 2003). According to a recent survey, 85% of TBI are characterized as MTBI graded on Glasgow Coma scale (Li et al. 2016). Usually the symptoms of MTBI resolve within 3 weeks of trauma; however, a few patients experience post-concussion syndrome (McInnes et al. 2017).
Weight drop on closed head induces MTBI in rodents and cause anxiety, depression and cognitive deficits similar to post concussion syndrome (Meyer et al. 2012; Mychasiuk et al. 2014; Zohar et al. 2003; Sagarkar et al. 2017a). Our previous studies showed that the repeated MTBI (rMTBI) induces anxiety-like behaviour in rats and decreases gut motility, specifically in the jejunal part of the gut (Sagarkar et al. 2017a, b). However, the perturbation in the microbial population colonizing the jejunum post-MTBI remains mostly unknown. The current study is aimed to investigate the changes in the microbial communities in jejunal mucosa post-MTBI, which may further help in understanding the microbial contribution to the imbalance in the gut–brain axis after physical traumatic stress. In this study, the rats were subjected to rMTBI at immediate and protracted time points, and changes in their gut microbiota composition were tracked. The changes in microbial communities at different levels of their classification and diversities are discussed in view of gut–brain pathophysiology post-rMTBI as previously reported (Sagarkar et al. 2017a, b, 2019).
2 Materials and methods
2.1 Animal experiments
Adult (75–90 days old) male Wistar rats weighing 200–225 g were housed under controlled light (12 h of light, followed by 12 h of darkness) and temperature (25 ± 2 °C) conditions. All protocols employed in the present study were carried out in accordance with National Institutes of Health (NIH), USA Guidelines under the strict compliance with Institutional Animal Ethics Committee (IAEC), Savitribai Phule Pune University, Pune, India. Food and water were provided ad libitum during the course of the study.
2.2 rMTBI experiments
The closed-head weight drop paradigm was used to simulate MTBI in rats as described previously (Sagarkar et al. 2017a, b). Briefly, the trauma simulator has a hollow guide tube (100 cm) with an inner diameter of 15 mm and a cylindrical metal weight of approximately 200 g that results in a contact area of 5–7 mm2 on the skull surface. The rats were mildly sedated using diethyl ether and placed on a platform made of aluminium foil. The weight was dropped on the intact skull, from the height of 30 cm by releasing the key. The drop was made at the intersection of lines connecting ears and eyes from opposite sides of the skull to ensure uniform impact on the head. The animals from trauma-induced group were subjected to 5 impacts with a recovery time of 48 h between each injury. The sham control (n=2; C1MTBI and C2MTBI) animals were not subjected to head trauma but underwent the rest of the procedures, including anaesthesia. The animals were allowed to recover from anaesthesia (2–3 h) and righting reflex, beam walking tests were performed. Animals from each of the three MTBI groups (n=2 per group) were decapitated at different time points; i.e. 6 h (6h1MTBI, 6h2MTBI), 48 h (48h1MTBI, 48h2MTBI) and 30 days (30d1MTBI, 30d2MTBI) post-trauma under deep anaesthesia induced by intraperitoneal (IP) injection of thiopentone sodium (60 mg/kg, Neon Laboratories Ltd, Mumbai). Before sacrificing, animals were deprived of food for 6 h to empty portions of the gastrointestinal tract. Rat jejunum samples were carefully dissected from the rest of the small intestine and stored at −80 °C until further use. The jejunums were thawed at room temperature; the jejunal mucosa was collected by scrapping the internal lining after longitudinally cutting the jejunum in aseptic conditions. The animal experimental paradigm is summarized in figure 1.
2.3 Sample processing and DNA extraction
DNA was isolated from jejunum scrapings of animals using Fast DNA spin kit for faeces (6570-200, MP bio, USA) as per manufacturer’s instructions. Further, the qualitative and quantitative analysis was performed using Nanodrop 2000C spectrophotometer (Thermo Scientific, USA) (supplementary table 1).
2.4 Amplicon sequencing and bioinformatics analysis
The amplicon libraries were prepared using the Nextera XT index Kit as per 16S amplicon library preparation protocol by Illumina Inc. Amplification of the V3–V4 region of the 16S rRNA gene was carried out and PCR products were resolved on 1.2% agarose gel. The amplicons with the Illumina adaptors were amplified using i5 and i7 primers as per standard Illumina protocol. The amplicon library was purified by 1X AMPure XP beads and quantified by Qubit fluorometer. The amplified libraries were analysed on 4200 Agilent Tape Station system (Agilent Technologies) as per the manufacturer’s instructions. The samples were sequenced using Illumina MiSeq with 2*300 paired-end chemistry that generates at least 0.1 million reads per sample. The primers used for V3–V4 hypervariable region amplification are as follows: Forward primer 5′ GCCTACGGGNGGCWGCAG 3′ and reverse primer 3′ ACTACHVGGGTATCTAATCC 5′. After sequencing, the quality of raw paired-end reads was checked by FASTQC tool (Andrews 2010) and pre-processing of sequences (primers and barcodes trimming) was performed using Cutadapt (Martin 2011). Trimmed sequences were assembled by PEAR with default parameters (Zhang et al. 2014). Microbiome_helper package was used for pre-processing of the data such as trimming, chimera removal and conversion of Fastq to Fasta files (Comeau et al. 2017). The pre-processed Fasta sequences were merged into a single Fasta file using QIIME v1.8 (Quantitative Insights Into Microbial Ecology) (http://qiime.org/) (Caporaso et al. 2010). Sequence reads were assigned to operational taxonomic units (OTUs) by using a reference-based OTU picking approach with Greengenes database (DeSantis et al. 2006). The OTU picking was performed using UCLUST method with a similarity threshold of 97% (Kopylova et al. 2016). The RDP naïve Bayesian classifier (version rdp_classifier_2.10.1) (Wang et al. 2007) was used for taxonomic assignment. Using QIIME pipeline, alpha and beta diversity analysis was performed. Alpha diversity indices, i.e., ACE, Chao1, Simpson, Shannon index and Goods coverage were estimated using QIIME pipeline. Data normalization was carried out at 99,138 reads per sample, at the lowest sequence count. Beta diversity was also calculated within the QIIME pipeline using weighted and unweighted UniFrac distances (Lozupone et al. 2011). From these estimates, jackknifed Principal Co-ordinates (PC) were computed to compress dimensionality into three-dimensional principal coordinate analysis (PCoA) plots. Further statistical analysis was performed using in-house R scripts and R package. The raw reads have been deposited in the sequence read archive (SRA) and are available under the BioProject ID PRJNA51195.
3 Results
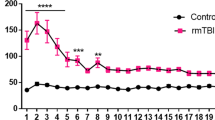
High-throughput sequencing resulted in generation of approximately 3 million raw reads from eight samples with average 368,869 ± 50,449 reads per sample. After assembly of paired-end reads, 2.3 million reads were retained from all the samples. Finally, 1,362,785 high-quality sequences were used for taxonomic assignment resulting in 2005 operational taxonomic units (OTUs) in all samples (supplementary table 2). Good’s coverage for all the control and trauma samples was found to be 0.998 ± 0.001 (mean ± SD) indicating that the majority of the bacterial diversity was captured in all the samples. Alpha diversity measures such as Chao1, observed and Shannon indicated significant diversity reduction in rMTBI samples as compared to sham controls (table 1; figure 2). A linear decrement in diversity was observed with increase in days post-rMTBI implying that rMTBI decreases bacterial diversity in a time-dependent manner. A similar observation was made using rarefaction curve which represents number of OTUs as a function of number of sequences in the samples (supplementary figure 1). Species richness was also found to be higher in control samples as compared to rMTBI samples with lowest species richness post 30 days (figure 3).
Box plot of alpha diversity measures viz. Observed species, Chao1 and Shannon index in trauma and control samples. 30 days, 48 h, 6 h represents time points after MTBI. Observed species, Chao1 and Shannon index showed substantial differences in microbial diversity between trauma and control samples.
Beta diversity analysis using PCoA ordination plots based on weighted and unweighted UniFrac metrics considering all the OTUs demonstrated that samples from control and rMTBI groups segregated into distinct clusters based on their abundances and presence/absence of OTUs (figure 4). Control samples formed a separate cluster showing less interindividual variation between the samples. However, rMTBI samples showed higher interindividual variations. Analysis suggests immediate changes in the gut microbiota after rMTBI (6 h) and the perturbation with reduction in bacterial diversity was persistent until 30 days.
Principal coordinate analysis (PCoA) based on weighted UniFrac metrics among trauma and control samples. Proportion of variance explained by each axis is denoted in the corresponding axis labels. Each circle (designated by the color) represents control and trauma group and labels represent sample IDs.
A total of 15 bacterial phyla were detected in all the samples. Bacterial phyla Proteobacteria (57.2%), Firmicutes (33.4%), Tenericutes (4.43%) and Fusobacteria (2.3%) were most abundant in rMTBI samples and constituted for 97% of the total microbiome in rMTBI group. Similarly, Firmicutes (64.1%), Proteobacteria (27.8%), Bacteroidetes (3.1%), TM7 (2.1%) and Actinobacteria (1.2%) were most abundant in sham controls and constituted for 98.4% of the total microbiome (supplementary table 3). The relative abundances of top 10 phyla and top 30 genera across all samples were calculated and the results are represented in figure 5a and b respectively. Figure 5a indicates waxing and waning of abundance of Proteobacteria and Firmicutes in rMTBI samples respectively, as compared to controls. A total of 11 genera were detected in MTBI samples and 10 genera were detected in control samples with relative abundance above 1% (supplementary table 4). Moreover, the most abundant genus in rMTBI exposed animals was Helicobacter (29.2%) followed by Lactobacillus (21.7%) and Campylobacter (17.7%), while in controls the most abundant genus was Lactobacillus (40.3%) followed by Helicobacter (11.5%) and Streptococcus (9.8%) (figure 5b). We observed a gradual increase in relative abundance of genus Helicobacter (29.2% ± 4.9) in trauma samples from 6 h to 30 days, but decrease in abundance of the genus Lactobacillus was independent of time post-trauma (21.7% ± 12.3). Overall, a substantial reduction in the relative abundance of Lactobacillus followed by Streptococcus and an increase in the abundance of the Helicobacter and Campylobacter was observed in the rMTBI group.
A hierarchical clustering using ward method was employed to analyse the clustering between the rMTBI groups with microbial abundance at phylum (figure 6a) and family level (figure 6b). The hierarchical clustering showed clear separation between rMTBI and control samples, but no clear separation was observed within distinct rMTBI groups, i.e. 6 h-MTBI, 48 h-MTBI, and 30 days-MTBI. Firmicutes, Actinobacteria, and TM7 were found to be abundant in control rats, whereas Proteobacteria was abundant in rMTBI-exposed rats (figure 6a). At family level, Campylobacteraceae and Helicobacteraceae were most abundant in rMTBI-exposed rats, especially post 30 days of rMTBI. On the contrary, these bacterial families were least abundant in the jejunum of control rats. Similarly, families such as Actinomycetaceae, Erysipelotrichaceae, and Lachnospiraceae were abundant in control samples as compared to rMTBI samples (figure 6b). Discriminant Analysis was conducted to find the biomarkers associated with trauma (figure 7). The linear discriminant analysis predicted Campylobacteraceae, Helicobacteraceae, Mycoplasmataceae, and Aerococcaceae as the biomarkers of trauma.
(a) Hierarchical clustering and heatmap visualization at phylum level using trauma and control group as experimental factors. Hierarchical clustering was based on ward linkage algorithm using Euclidean distance as a distance measure. Heatmap is used to show taxa abundance in a particular sample. (b) Hierarchical clustering and heatmap visualization at family level using trauma group at different time points and control group as experimental factors. Hierarchical clustering was based on ward linkage algorithm using Euclidean distance as a distance measure. Heatmap is used to show taxa abundance in a particular sample.
Uniqueness and divergence of jejunal microbial diversity in MTBI and control group was determined by Linear Discriminant Analysis (LDA) of effect size using LEFSe in MicrobiomeAnalyst. Blue colored bars denote taxa which were higher in MTBI group and pink colour denotes taxa which were higher in control groups.
Based on the previous literature, members of the families Lachnospiraceae and Ruminococcaceae (Vital et al. 2014), Veillonellaceae (Esquivel-Elizondo et al. 2017) and Erysipelotrichaceae (Pozuelo et al. 2015) are considered as potential butyrate producers. We conducted imputed analysis on our dataset which revealed the differential abundance of members of these families as shown in figure 8. Moreover, the relative abundance of butyrate-producing bacterial families was decreased in rMTBI samples. A sharp decline in relative abundance of Lachnospiraceae, Ruminococcaceae, and Erysipelotrichaceae was seen at 6 h post-rMTBI compared to control, and such a trend was persistent up to 30 days.
4 Discussion
Increasing evidences are showing that the intestinal microbiota contributes to the host physiology and maintains homeostasis. A plethora of studies relate the microbial communities to immunity mechanisms and inflammatory challenges in the intestine. Therefore, intestinal microbiota is linked to gut pathologies such as inflammatory bowel disease and cancer (Ayres et al. 2012; Dupont and Dupont 2011; Le Chatelier et al. 2013; Yoshimoto et al. 2013). Not only intestinal health but in recent years the perturbations in gut microbiota have been implicated in neurodevelopmental and neurobehavioral disorders such as depression, anxiety, and autism (Hsiao et al. 2013; Kang et al. 2013). The present study characterizes the alterations in microbial communities in jejunal mucosa of the rMTBI-induced rats using high-throughput targeted amplicon sequencing of the 16S rRNA gene. Although this study is based on a small cohort size, which is one of the shortcomings of our findings, the results for the first time link rMTBI to perturbations in microbial communities in jejunum as early as 6 h post-trauma, and it persisted through 48 h and continued until 30 days. Whereas rMTBI induced the increase in phylum Proteobacteria, owing to rise in the abundance of Helicobacter and Campylobacter; levels of Firmicutes declined persistently from 6 h to 30 days post-trauma as compared to healthy controls.
Recently, Nicholson and colleagues detailed the effect of moderate TBI on the faecal microbiota composition and reduction in bacterial alpha diversity post-TBI, similar to what we have observed in the jejunal microbiota. Controlled cortical impact model, wherein the animals underwent craniotomy, was employed in their study (Nicholson et al. 2018); whereas we have applied a closed-head injury paradigm. In yet another study, dramatic changes are reported in the caecal microbiota in response to TBI in mice (Houlden et al. 2016). These changes were observed post 72 h of stroke in mice; similar to that found in trauma patients (Howard et al. 2017). We have noticed the changes in microbiome in jejunum as early as 6 h which persisted until 48 h and 30 days time points. In mice, the norepinephrine release in the gut as a consequence to TBI was suggested as causal to the perturbation in caecal microbiome (Houlden et al. 2016). In this connection, the findings by Singh and colleagues are noteworthy in which brain injuries due to a stroke caused gut microbial dysbiosis and reduced gastrointestinal motility in mice (Singh et al. 2016). Using the same rMTBI model as in this study, we have previously reported the slowing in gut motility at the level of jejunum in rats at identical time points of 48 h and 30 days (Sagarkar et al. 2017b). These observations suggest the concurrence between microbial dysbiosis and gut motility. However, bacterial communities belonging to Bacteroidetes phylum was overcrowded in faeces after the stroke (Singh et al. 2016). On the contrary, we have observed the increased abundance of Proteobacteria in the jejunum of rMTBI-exposed rats. The discrepancies in observations in these two studies could be related to (1) species differences (mice versus rats), (2) injury paradigm (stroke versus rMTBI), and (3) microbial sample (faeces versus jejunual mucosa). A recent study elucidated the link between TBI and gut bacterial dysbiosis in mice (Treangen et al. 2018). Although they have observed an elevation of Eubacterium and Marvinbryantia post brain injury, Helicobacter and Campylobacter dominated in our trauma groups. Again, these variations could be ascribed to different experimental protocols and models. Proteobacteria are known to be associated with inflammation and dysbiosis (Bäckhed et al. 2012). With the increase in Proteobacteria in the gut of rMTBI-exposed rats, intriguing would be to examine the inflammatory changes therein, in addition to reductions in gut motility as reported earlier (Sagarkar et al. 2017b).
In the similar model of rMBTI in rats, we have observed the deficits in learning and memory (Sagarkar et al. 2019) and expression of anxiety-like behaviours as measured by light dark box (LDB) exploration test (Sagarkar et al. 2017a), comorbid with reduced gastrointestinal motility (Sagarkar et al. 2017b) at 48 h which persisted until 30 days. The TBI has been shown to induce alterations in inflammatory responses (Chen et al. 2008), contractility (Olsen et al. 2013), motility (Smith 2013) and permeability (Bansal et al. 2009) in the gut. Clinically, severe TBI has also been reported to be comorbid with food intolerance due to reduced gastrointestinal motility and absorption (Kao et al. 1998; Tan et al. 2011). A growing body of evidence also associates gut dysbiosis with neuropsychiatric ailments (Bansal et al. 2009; Dinan and Cryan 2017; Evrensel and Ceylan 2015). Several studies have associated stress and imbalance of hypothalamic-pituitary axis with short term as well as long term modulations in the gut microbial composition (Cryan and Dinan 2012). Exposure to early life stressor such as maternal separation caused persistent alterations in the composition of faecal microbiota of adult rats (O’Mahony et al. 2009). In addition, germ-free mice exhibited elevated anxiety like-behaviours as compared to gnotobiotic mice, which were alleviated by monocolonization with Blautia coccoides (Nishino et al. 2013). On the contrary, reduction in the anxiety-like behaviours of germ-free mice as accessed by LDB and elevated plus maze (EPM) tests were also reported in three independent studies (Clarke et al. 2013; Heijtz et al. 2011; Neufeld et al. 2010). In view of the above, the gut microbial changes in rMTBI-exposed rats are expected to be causal to the intestinal pathologies such as motility and inflammation, and the psychological manifestations of the rMTBI. Therefore, future studies are warranted to discern the specific microbial communities linked to rMTBI-induced imbalance of gut–brain axis and molecular mechanisms therein. For example, the expression of brain-derived neurotrophic factor (BDNF), key synaptic plasticity regulating neuropeptide and NMDA receptor subunit 2A (NR2A) was decreased in the cortex and hippocampus of germ-free mice (Sudo et al. 2004). Moreover, infection of gut pathogen (T. muris) also reduced BDNF mRNA expression in the hippocampus precipitating into anxiety-like behaviours which were restored by Bifidobacterium longum administration (Bercik et al. 2010). On similar lines, we have previously reported the reduction in the BDNF levels in the amygdala of rMTBI-induced rats at 48 h and 30 days post-trauma. While on one hand the gut microbiome is linked with the BDNF expression and anxiety levels in mice (Sudo et al. 2004; Bercik et al. 2010); on the other hand, we have observed the trauma-induced changes in gut microbiome and BDNF expression in amygdala coincident with anxiety-like behaviours (Sagarkar et al. 2017a). Therefore, it may be speculated that the healthy microbial communities in jejunum might confer a neuroprotective role via regulation of neuropeptides such as BDNF; the imbalance of which may be implicated in trauma-induced neuropsychiatric behaviours.
Proteobacteria have been listed previously as a marker of gut microbial dysbiosis (Shin et al. 2015). According to the spatial distribution of the bacteria in the gut, the Helicobacter are predominantly housed in stomach (Andersson et al. 2008) with an extremely low abundance in the small intestine and colon (Jandhyala et al. 2015). However, rMTBI increased the abundance of the Proteobacteria in the jejunum suggesting bacterial translocation from adjoining areas of intestine. The notion is further supported by the increased abundance of Helicobacter and Campylobacter after trauma. While Campylobacter has been shown to be elevated in the fecal and intestinal samples of patients with Crohn’s disease (Man et al. 2009), Helicobacter levels were found to be elevated in duodenal ulcers and gastric cancer (Sheh and Fox 2013). On the contrary, Helicobacter are proposed to have a protective role in intestinal bowel disease (Papamichael et al. 2014; Bartels et al. 2015). Therefore, the proposed model of rMTBI can be further utilized to draw the causal potential of these bacterial communities in traumatic stress-induced intestinal ailments including inflammation.
We have noticed the depletion of butyrate-producing communities in the gut of trauma-induced rats, which were abundant in control animals. The healthy gut is believed to harbour butyrate producers, mostly belonging to Clostridium cluster IV and XIVa (Barcenilla et al. 2000; Rivière et al. 2016). Jejunum is known for its ability to absorb small molecules like butyrate and other SCFAs from the food (Schmitt et al. 1976). Butyrate is known for its effects as a histone deacetylase (HDAC) inhibitor (Bourassa et al. 2016). Previous studies have elucidated the action of microbiota-derived butyrate in HDAC inhibition in intestine (Furusawa et al. 2013; Waldecker et al. 2008). Inhibition of HDACs in brain by molecules such as butyrate, valproic acid, and trichostatin A has been linked to reduction in anxiety and fear (Whittle and Singewald 2014). Therefore, the reductions in butyrate-producing microbial communities might be suggested to be causal to increased anxiety levels and reduced gut motility in rMTBI-induced rats (Sagarkar et al. 2017a). Previous studies in rat and human support the potential of Bifidobacteria (a butyrate producer) and other probiotics in treating neurological ailments (Messaoudi et al. 2011). Recently, a study elaborated on the neuroprotective effects of Clostridium butyricum (a butyrate producer) in alleviating the impact of TBI, when trauma mice were treated intragastrically with the mentioned bacterium (Li et al. 2018). Hence, using the faecal microbiota transplantation (FMT) in rMTBI-induced rats, future studies could discern the contribution of butyrate-producing bacterial communities in maintaining the healthy homeostasis in gut-microbiome-brain axis.
In conclusion, the results of the present study potentially relate rMTBI-induced microbial changes in jejunum to the comorbid conditions of gut dysfunction and neuropsychiatric readouts. However, additional studies involving molecular and cognitive phenotyping are required to establish a causal link between trauma, behaviour and microbial perturbations. The depletion of butyrate-producing bacteria after the trauma may alter the epigenome in the specific areas of the brain relevant to emotional behaviours such as amygdala. These observations further offer a plausible explanation for the persistent anxiety-like behaviours comorbid with reduced gut motility. The rMTBI model used in the present study, therefore, may prove useful in investigating the relevance of gut psychobiome in stress-induced neuropathologies.
4.1 Study limitation
The current study was carried out using only two samples per group which remains as a limitation of the study. Although the results show profound changes in the microbial composition in the jejunum of rMTBI-induced rats as compared to control rats, the degree of statistical significance cannot be provided in view of a limited number of samples. Although non-significant, a slight reduction in body weights of rMTBI-induced rats at the 30 days time point was observed. Therefore, the possibility may not be excluded that the reduced gut motility and consequent changes in feeding habits might underlie the profound differences in microbiome post-rMTBI. Future studies are warranted to scrutinize the relevance of gut microbiome changes in rMTBI-induced neuropsychiatric and intestinal ailments or vice versa to draw causal relationships between consequences.
References
Andersson AF, Lindberg M, Jakobsson H, Bäckhed F, Nyrén P and Engstrand L 2008 Comparative analysis of human gut microbiota by barcoded pyrosequencing. PloS One 3 e2836
Andrews S 2010 FastQC: a quality control tool for high throughput sequence data. http://www.bioinformatics.babraham.ac.uk/projects/fastqc/. Accessed 28 Nov 2017
Ayres JS, Trinidad NJ and Vance RE 2012 Lethal inflammasome activation by a multidrug-resistant pathobiont upon antibiotic disruption of the microbiota. Nat. Med. 18 799–806
Bäckhed F, Fraser CM, Ringel Y, Sanders ME, Sartor RB, Sherman PM, Versalovic J, Young V and Finlay BB 2012 Defining a healthy human gut microbiome: current concepts, future directions, and clinical applications. Cell Host Microbe 12 611–622
Bansal V, Costantini T, Kroll L, Peterson C, Loomis W, Eliceiri B, Baird A, Wolf P and Coimbra R 2009 Traumatic brain injury and intestinal dysfunction: uncovering the neuro-enteric axis. J. Neurotrauma 26 1353–1359
Barcenilla A, Pryde SE, Martin JC, Duncan SH, Stewart CS, Henderson C and Flint HJ 2000 Phylogenetic relationships of butyrate-producing bacteria from the human gut. Appl. Environ. Microbiol. 66 1654–1661
Bartels LE, Jepsen P, Christensen LA, Gerdes LU, Vilstrup H and Dahlerup JF 2015 Diagnosis of Helicobacter pylori infection is associated with lower prevalence and subsequent incidence of Crohn’s disease. J. Crohns Colitis 10 443–448
Bercik P, Verdu EF, Foster JA, Macri J, Potter M, Huang X, Malinowski P, Jackson W, Blennerhassett P, Neufeld KA and Lu J 2010 Chronic gastrointestinal inflammation induces anxiety-like behavior and alters central nervous system biochemistry in mice. Gastroenterology 139 2102–2112
Bourassa MW, Alim I, Bultman SJ and Ratan RR 2016 Butyrate, neuroepigenetics and the gut microbiome: can a high fiber diet improve brain health? Neurosci. Lett. 625 56–63
Bull MJ and Plummer NT 2014 Part 1: The Human Gut Microbiome in Health and Disease. Integr. Med. (Encinitas) 13 17–22
Caporaso JG, Kuczynski J, Stombaugh J, Bittinger K, Bushman FD, Costello EK, Fierer N, Pena AG, Goodrich JK, Gordon JI and Huttley GA 2010 QIIME allows analysis of high-throughput community sequencing data. Nat. Methods 7 335
Carabotti M, Scirocco A, Maselli MA and Severi C 2015 The gut–brain axis: interactions between enteric microbiota, central and enteric nervous systems. Ann. Gastroenterol. 28 203
Cenit MC, Sanz Y and Codoñer-Franch P 2017 Influence of gut microbiota on neuropsychiatric disorders. World J. Gastroenterol. 23 5486
Chen GH, Wu DP, Sun AN, Yang MZ, Wang Y, Tang XW, Chang HR, Feng YF and Zhu ZL 2008 Experimental study on IL-2-and IL-15 application in allogeneic hematopoietic stem cell transplantation. Zhonghua Xue Ye Xue Za Zhi 29 526–530
Clarke G, Grenham S, Scully P, Fitzgerald P, Moloney RD, Shanahan F, Dinan TG and Cryan JF 2013 The microbiome–gut–brain axis during early life regulates the hippocampal serotonergic system in a sex-dependent manner. Mol. Psychiatry 18 666
Comeau AM, Douglas GM and Langille MGI 2017 Microbiome Helper: a Custom and Streamlined Workflow for Microbiome Research. MSystems 2 1–11
Cryan JF and Dinan TG 2012 Mind-altering microorganisms: the impact of the gut microbiota on brain and behaviour. Nat. Rev. Neurosci. 13 701
DeSantis TZ, Hugenholtz P, Larsen N, Rojas M, Brodie EL, Keller K, Huber T, Dalevi D, Hu P and Andersen GL 2006 Greengenes, a chimera-checked 16S rRNA gene database and workbench compatible with ARB. Appl. Environ. Microbiol. 72 5069–5072
Dinan TG and Cryan JF 2017 Brain-gut-microbiota axis—Mood, metabolism and behavior. Nat. Rev. Gastroenterol. Hepatol. 14 69–70
Drossman DA 2011 Abuse, trauma, and GI illness: Is there a link and quest. Am. J. Gastroenterol. 106 14–25.
Dupont AW and Dupont HL 2011 The intestinal microbiota and chronic disorders of the gut. Nat. Rev. Gastroenterol. Hepatol. 8 523–531
Esquivel-Elizondo S, Ilhan ZE, García-Peña EI and Krajmalnik-Brown R 2017 Insights into butyrate production in a controlled fermentation system via gene predictions. mSystems 2 e00051–17
Evrensel A and Ceylan ME 2015 The gut–brain axis: the missing link in depression. Clin. Psychopharmacol. Neurosci. 13 239–244
Furusawa Y, Obata Y, Fukuda S, Endo TA, Nakato G, Takahashi D, Nakanishi Y, Uetake C, Kato K, Kato T and Takahashi M 2013 Commensal microbe-derived butyrate induces the differentiation of colonic regulatory T cells. Nature 504 446
Grochowska M, Wojnar M and Radkowski M 2018 The gut microbiota in neuropsychiatric disorders. Acta Neurobiol. Exp. 78 69–81
Hang CH, Shi JX, Li JS, Wu W and Yin HX 2003 Alterations of intestinal mucosa structure and barrier function following traumatic brain injury in rats. World J. Gastroenterol. 9 2776
Heijtz RD, Wang S, Anuar F, Qian Y, Björkholm B, Samuelsson A, Hibberd ML, Forssberg H and Pettersson S 2011 Normal gut microbiota modulates brain development and behavior. Proc. Natl. Acad. Sci. USA 108 3047–3052
Houlden A, Goldrick M, Brough D, Vizi ES, Lénárt N, Martinecz B, Roberts IS and Denes A 2016 Brain injury induces specific changes in the caecal microbiota of mice via altered autonomic activity and mucoprotein production. Brain Behav. Immun. 57 10–20
Howard BM, Kornblith LZ, Christie SA, Conroy AS, Nelson MF, Campion EM, Callcut RA, Calfee CS, Lamere BJ, Fadrosh DW and Lynch S 2017 Characterizing the gut microbiome in trauma: significant changes in microbial diversity occur early after severe injury. J. Trauma Acute Care 2 e000108
Hsiao EY, McBride SW, Hsien S, Sharon G, Hyde ER, McCue T, Codelli JA, Chow J, Reisman SE, Petrosino JF and Patterson PH 2013 Microbiota modulate behavioral and physiological abnormalities associated with neurodevelopmental disorders. Cell 155 1451–1463
Jandhyala SM, Talukdar R, Subramanyam C, Vuyyuru H, Sasikala M and Reddy DN 2015 Role of the normal gut microbiota. World J. Gastroenterol. 21 8787
Kang DW, Park JG, Ilhan ZE, Wallstrom G, LaBaer J, Adams JB and Krajmalnik-Brown R 2013 Reduced incidence of Prevotella and other fermenters in intestinal microflora of autistic children. PloS One 8 e68322
Kao CH, ChangLai SP, Chieng PU and Yen TC 1998 Gastric emptying in head-injured patients. Am. J. Gastroenterol. 93 1108
Karr JE, Areshenkoff CN and Garcia-Barrera MA 2014 The neuropsychological outcomes of concussion: a systematic review of meta-analyses on the cognitive sequelae of mild traumatic brain injury. Neuropsychology 28 321–336
Kharrazian D 2015 Traumatic Brain Injury and the Effect on the Brain-Gut Axis. Altern. Ther. Health Med. 21 28–32
Kopylova E, Navas-Molina JA, Mercier C, Xu ZZ, Mahé F, He Y, Zhou HW, Rognes T, Caporaso JG and Knight R 2016 Open-source sequence clustering methods improve the state of the art. Msystems 1 e00003–15
Le Chatelier E, Nielsen T, Qin J, Prifti E, Hildebrand F, Falony G, Almeida M, Arumugam M, Batto JM, Kennedy S and Leonard P 2013 Richness of human gut microbiome correlates with metabolic markers. Nature 500 541
Li M, Zhao Z, Yu G and Zhang J 2016 Epidemiology of Traumatic Brain Injury over the World: A Systematic Review. Austin Neurol. Neurosci. 1 1007
Li H, Sun J, Du J, Wang F, Fang R, Yu C, Xiong J, Chen W, Lu Z and Liu J 2018 Clostridium butyricum exerts a neuroprotective effect in a mouse model of traumatic brain injury via the gut–brain axis. Neurogastroenterol Motil. 30 e13260
Logsdon AF, Erickson MA, Rhea EM, Salameh TS and Banks WA 2018 Gut reactions: How the blood-brain barrier connects the microbiome and the brain. Exp. Biol. Med. (Maywood) 243 159–165
Lozupone C, Lladser ME, Knights D, Stombaugh J and Knight R 2011 UniFrac: An effective distance metric for microbial community comparison. ISME J. 5 169–172
Man SM, Zhang L, Day AS, Leach ST, Lemberg DA and Mitchell H 2009 Campylobacter concisus and other Campylobacter species in children with newly diagnosed Crohn’s disease. Inflamm. Bowel Dis. 16 1008–1016
Martin M 2011 Cutadapt removes adapter sequences from high-throughput sequencing reads. EMBnet J. 17 10
Mayer EA 2000 The neurobiology of stress and gastrointestinal disease. Gut 47 861–869.
Mayer EA, Tillisch K and Gupta A 2015 Gut/brain axis and the microbiota. J. Clin. Invest. 125 926–938
McInnes K, Friesen CL, MacKenzie DE, Westwood DA and Boe SG 2017 Mild Traumatic Brain Injury (mTBI) and chronic cognitive impairment: A scoping review. PLoS One 12 e0174847
Messaoudi M, Lalonde R, Violle N, Javelot H, Desor D, Nejdi A, Bisson JF, Rougeot C, Pichelin M, Cazaubiel M and Cazaubiel JM 2011 Assessment of psychotropic-like properties of a probiotic formulation (Lactobacillus helveticus R0052 and Bifidobacterium longum R0175) in rats and human subjects. Br. J. Nutr. 105 755–764
Meyer DL, Davies DR, Barr JL, Manzerra P and Forster GL 2012 Mild traumatic brain injury in the rat alters neuronal number in the limbic system and increases conditioned fear and anxiety-like behaviors. Exp. Neurol. 235 574–587
Mychasiuk R, Farran A, Angoa-Perez M, Briggs D, Kuhn D and Esser MJ 2014 A novel model of mild traumatic brain injury for juvenile rats. J. Vis. Exp. 94 e51820
Neufeld KM, Kang N, Bienenstock J and Foster JA 2010 Reduced anxiety-like behavior and central neurochemical change in germ-free mice. Neurogastroenterol. Motil. 23 255–264
Nicholson SE, Watts LT, Burmeister DM, Merrill D, Scroggins S, Zou Y, Lai Z, Grandhi R, et al. 2018 Moderate traumatic brain injury alters the gastrointestinal microbiome in a time-dependent manner. Shock https://doi.org/10.1097/shk.0000000000001211
Nishino R, Mikami K, Takahashi H, Tomonaga S, Furuse M, Hiramoto T, Aiba Y, Koga Y and Sudo N 2013 Commensal microbiota modulate murine behaviors in a strictly contamination-free environment confirmed by culture-based methods. Neurogastroenterol. Motil. 25 521–528
Olsen AB, Hetz RA, Xue H, Aroom KR, Bhattarai D, Johnson E, Bedi S, Cox Jr CS and Uray K 2013 Effects of traumatic brain injury on intestinal contractility. Neurogastroenterol. Motil. 25 593-463
O’Mahony SM, Marchesi JR, Scully P, Codling C, Ceolho AM, Quigley EM, Cryan JF and Dinan TG 2009 Early life stress alters behavior, immunity, and microbiota in rats: implications for irritable bowel syndrome and psychiatric illnesses. Biol. Psychiatry 65 263–267
Papamichael K, Konstantopoulos P and Mantzaris GJ 2014 Helicobacter pylori infection and inflammatory bowel disease: is there a link? World J. Gastroenterol. 20 6374
Pozuelo M, Panda S, Santiago A, Mendez S, Accarino A, Santos J, Guarner F, Azpiroz F and Manichanh C 2015 Reduction of butyrate- and methane-producing microorganisms in patients with Irritable Bowel Syndrome. Sci. Rep. 5 12693
Rivière A, Selak M, Lantin D, Leroy F and De Vuyst L 2016 Bifidobacteria and butyrate-producing colon bacteria: importance and strategies for their stimulation in the human gut. Front. Microbiol. 7 979
Round JL and Mazmanian SK 2009 The gut microbiota shapes intestinal immune responses during health and disease. Nature Rev. Immunol. 9 313–323
Sagarkar S, Balasubramanian N, Mishra S, Choudhary AG, Kokare DM and Sakharkar AJ 2019 Repeated mild traumatic brain injury causes persistent changes in histone deacetylase function in hippocampus: Implications in learning and memory deficits in rats. Brain Res. 1711 183–192.
Sagarkar S, Bhamburkar T, Shelkar G, Choudhary A, Kokare DM and Sakharkar AJ 2017a Minimal traumatic brain injury causes persistent changes in DNA methylation at BDNF gene promoters in rat amygdala: a possible role in anxiety-like behaviors. Neurobiol. Dis. 106 101–109
Sagarkar S, Mahajan S, Choudhary AG, Borkar CD, Kokare DM and Sakharkar AJ 2017b Traumatic stress-induced persistent changes in DNA methylation regulate neuropeptide Y expression in rat jejunum. Neurogastroenterol. Motil. 29 e13074
Schmitt MG, Soergel KH and Wood CM 1976 Absorption of short chain fatty acids from the human jejunum. Gastroenterology 70 211–215
Sender R, Fuchs S and Milo R 2016 Revised Estimates for the Number of Human and Bacteria Cells in the Body. PLoS Biol 14 e1002533
Sheh A and Fox JG 2013 The role of the gastrointestinal microbiome in Helicobacter pylori pathogenesis. Gut microbes 4 505–531
Shin NR, Whon TW and Bae JW 2015 Proteobacteria: microbial signature of dysbiosis in gut microbiota. Trends Biotechnol. 33 496–503
Shreiner AB, Kao JY and Young VB 2015 The gut microbiome in health and in disease. Curr. Opin. Gastroenterol. 31 69–75
Singh V, Roth S, Llovera G, Sadler R, Garzetti D, Stecher B, Dichgans M and Liesz A 2016 Microbiota dysbiosis controls the neuroinflammatory response after stroke. J. Neurosci. 36 7428–7440
Smith K 2013 TBI affects intestinal motility Nat. Rev. Gastroenterol. Hepatol. 10 260
Sudo N, Chida Y, Aiba Y, Sonoda J, Oyama N, Yu XN, Kubo C and Koga Y 2004 Postnatal microbial colonization programs the hypothalamic–pituitary–adrenal system for stress response in mice. J. Physiol. 558 263–275
Tan M, Zhu JC and Yin HH 2011 Enteral nutrition in patients with severe traumatic brain injury: reasons for intolerance and medical management. Br. J. Neurosurg. 25 2–8
Tannock GW and Savage DC 1974 Influences of dietary and environmental stress on microbial populations in the murine gastrointestinal tract. Infect. Immun. 9 591–598
Treangen TJ, Wagner J, Burns MP and Villapol S 2018 Traumatic brain injury in mice induces acute bacterial dysbiosis within the fecal microbiome. Front. Immunol. 9 2757
Tremaroli V and Bäckhed F 2012 Functional interactions between the gut microbiota and host metabolism. Nature 489 242–249
Vital M, Howe AC and Tiedje JM 2014 Revealing the bacterial butyrate synthesis pathways by analyzing (meta)genomic data. MBio 5 e00889
Waldecker M, Kautenburger T, Daumann H, Busch C and Schrenk D 2008 Inhibition of histone-deacetylase activity by short-chain fatty acids and some polyphenol metabolites formed in the colon. J. Nutr. Biochem. 19 587–593
Wang Q, Garrity GM, Tiedje JM and Cole JR 2007 Naïve Bayesian classifier for rapid assignment of rRNA sequences into the new bacterial taxonomy. Appl. Environ. Microbiol. 73 5261–5267
Whittle N and Singewald N 2014 HDAC inhibitors as cognitive enhancers in fear, anxiety and trauma therapy: where do we stand? Biochem. Soc. Trans. 42 569–581
Yoshimoto S, Loo TM, Atarashi K, Kanda H, Sato S, Oyadomari S, Iwakura Y, Oshima K, Morita H, Hattori M, Honda K, Ishikawa Y, Hara E and Ohtani N 2013 Obesity-induced gut microbial metabolite promotes liver cancer through senescence secretome. Nature 499 97–101
Zhang J, Kobert K, Flouri T and Stamatakis A 2014 PEAR: A fast and accurate Illumina Paired-End reAd mergeR. Bioinformatics 30 614–620
Zohar O, Schreiber S, Getslev V, Schwartz JP, Mullins PG and Pick CG 2003 Closed-head minimal traumatic brain injury produces long-term cognitive deficits in mice. Neuroscience 118 949–955
Zhu C, Grandhi R, Patterson T and Nicholson S 2018 A Review of traumatic brain injury and the gut microbiome: insights into novel mechanisms of secondary brain injury and promising targets for neuroprotection. Brain Sci. 8 113
Acknowledgements
This work was supported by the grants from the University Grants Commission, Government of India (UGC, GOI; F.4-5/151-FRP/2014/BSR); Science and Engineering Research Board (SERB, GOI, EMR/2017/000621); Council for Scientific and Industrial Research (CSIR, GOI, 37(1718)/18/EMR-II); University Research Grant Scheme, Savitribai Phule Pune University (SPPU) and DST-PURSE, SPPU to AJS. AJS also acknowledges funds received through the Department Research and Development Program (DRDP), Department of Biotechnology, Savitribai Phule Pune University. NB thanks UGC-GOI for the award of Junior Research Fellowship (File No. 2061330923).
Author information
Authors and Affiliations
Corresponding authors
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Matharu, D., Dhotre, D., Balasubramanian, N. et al. Repeated mild traumatic brain injury affects microbial diversity in rat jejunum. J Biosci 44, 120 (2019). https://doi.org/10.1007/s12038-019-9940-0
Published:
DOI: https://doi.org/10.1007/s12038-019-9940-0